Periapical Radiolucency And Radiopacity Important Notes
- Multilocular radiolucencies – 3 types
- Soap bubble:- Individual compartments are circular, large and overlapped
- Honeycomb:- Individual compartments are small, numerous, and equally spaced.
- Angular:- Individual compartments are angular in shape
- Common lesions showing multilocular radiolucency:
- Ameloblastoma
- Odontogenic keratocyst
- Odontogenic myxoma
- Central giant cell granuloma
- Central hemangioma
- Aneurysmal bone cyst
- Cherubism
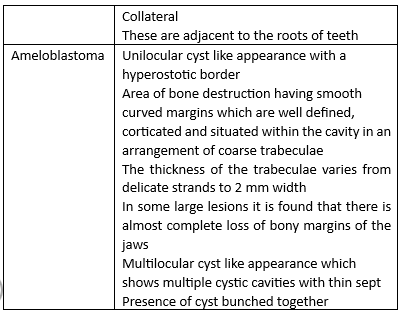
- Ameloblastoma:
- Soap bubble or honeycombed appearance
- Most common in 3rd molar – ramus area
- Nothing is seen in the advancing end of the tumor
- Root resorption and displacement of adjacent teeth are seen
- Rarely causes perforation
- Odontogenic Keratocyst:
- Soap bubble appearance
- No expansion of cortical plates, because the lesion grows anterior-posteriorly
- Odontogenic myxoma:
- Exclusively seen in jaws, only in tooth-bearing portions
- Angular or tennis racket or honeycomb appearance
- May be found in association with impacted tooth
Periapical radiolucency differential diagnosis
Periapical Radiolucency And Radiopacity Long Essays
Question 1. Enumerate periapical radiolucencies and opacities. How would you diagnose systemic diseases with periapical changes in radiographs?
Answer.
Periapical Radiolucencies:
- True periapical radiolucencies
- Pulpoperiapical Radiolucencies:
- Periapical granuloma:
- Radicular cyst
- Periapical scar
- Chronic and acute dentoalveolar abscess:
- Surgical defect
- Osteomyelitis
- Pulpoperiapical disease
- Dentigerous Cyst
- Periapical Cementosseous Dysplasis:
- Periodontal Disease
- Traumatic Bone Cyst
- Non radicular Cyst
- Malignant Tumors
- Pulpoperiapical Radiolucencies:
- Rarities:
- Ameloblastoma
- Aneurysmal bone cyst
- Cementifying and ossifying fibroma
- Cementoblastoma – early stage
- Giant cell granuloma
- Leukemia
Read And Learn More: Oral Radiology Question and Answers
Periapical Radiopacities:
- True Periapical Radiopacities:
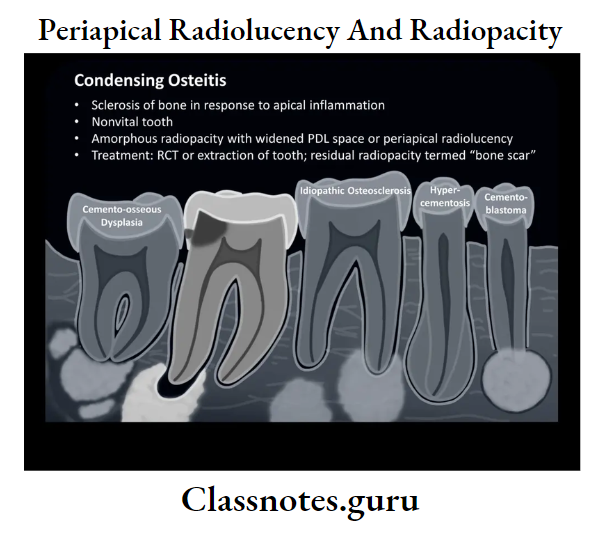
- Condensing or sclerosing osteitis
- Periapical idiopathic osteosclerosis
- Periapical or focal cement osseous dysplasia
- Unerupted succedaneous teeth
- Foreign bodies
- Hypercementosis
- Rarities
- Calcifying odontogenic cyst
- Cementoossifying fibroma
- Chondroma
- Hematoma
- Mature cementoblastoma
- Osteogenic sarcoma
- False Periapical Radiopacities:
- Anatomic structures
- Impacted teeth
- Tori, exostosis
- Retained root tips
- Foreign bodies
- Mucosal cyst of the maxillary sinus
- Ectopic calcification
- Rarities
- Calcified acne lesions
- Calcified hematoma
- Calcifying odontogenic cyst
- Squamous cell carcinoma
- Tonsilloliths
Periapical radiopacity differential diagnosis
Systemic Diseases With Periapical Changes:
- Hyperparathyroidism:
- There is a loss of lamina dura
- Depending on the duration and severity, loss of lamina dura may occur around one tooth or all remaining teeth
- Loss may be complete or partial
- It results in a tapered appearance of the root
- Hypoparathyroidism:
- Reveals dental enamel hypoplasia
- External root resorption
- Delayed eruption
- Root dilaceration
- Hyperpituitarism:
- Hypercementosis present over roots of posterior teeth
- Hypopituitarism:
- Third molar buds are completely absent
- Hyperthyroidism:
- Excessive bone resorption is seen
- Hypothyroidism:
- Show periodontal disease, loss of teeth, and external root resorption
- Diabetes mellitus:
- Presence of bone loss due to more prone to periodontal diseases
- Results in focal sclerosing osteomyelitis or dry socket
- Cushing’s syndrome:
- Teeth may erupt prematurely
- Partial loss of lamina dura may occur
- Osteoporosis:
- Thinning of the inferior mandibular cortex
- Reduction in the number of trabeculae
- Rickets:
- Enamel hypoplasia
- Involves both unerupted and erupted teeth
- Lamina dura and cortical boundary of tooth follicles may be thin or missing
- Renal Osteodystrophy:
- Hypoplasia and hypo calcification of teeth
- Results in loss of enamel
- Lamina dura may be absent or less apparent
- Hypophosphatemic rickets:
- Teeth are poorly formed with thin enamel caps large pulp chambers and root canals
- Presence of periapical and periodontal abscesses
- Subsequent pulp necrosis may be present
- Lamina dura may become sparse
- Cortical boundaries around tooth crypts may be thin or absent
- Hypophosphatasia:
- Both primary and permanent teeth have thin enamel layers large pulp chambers and root canals
- Osteopetrosis:
- Teeth are poorly calcified
- Ankylosis is seen
- Lamina dura and cortical borders may appear thicker than normal
- Systemic sclerosis:
- Increase in width of periodontal ligament spaces around teeth
- Both anterior and posterior teeth are affected
- Sickle cell anemia:
- Thinning of cortical plates
- Thalassemia:
- Thinning of cortical borders
- Enlargement of marrow spaces
- Trabeculae are large and coarse
- Lamina dura is thin and the roots of teeth may be short
Causes of periapical radiolucent lesions
Question 2. Describe differential diagnosis of radiolucencies on the coronal part of teeth
Answer.
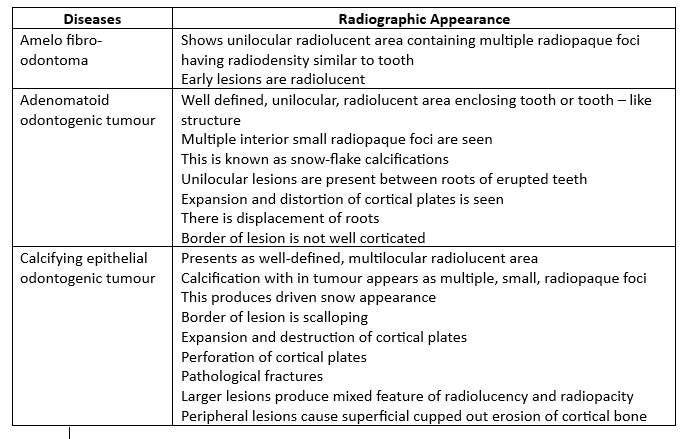
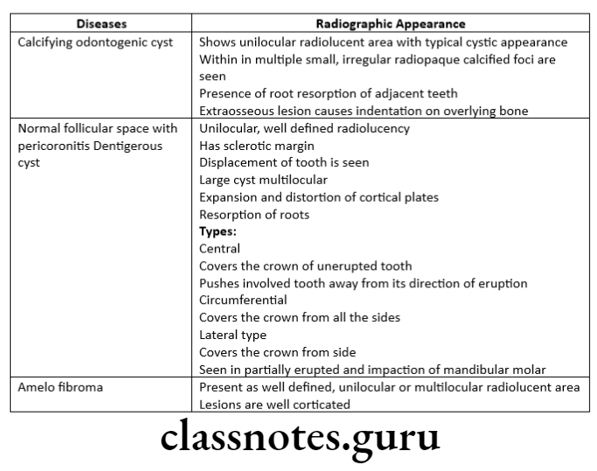
Pericoronal Radiolucencies:
With radiopaque flecks
- Ameloblastic fibro – odontoma
- Adenomatoid odontogenic tumor
- Calcifying epithelial odontogenic tumor
- Calcifying odontogenic cyst
Without radiopaque flecks
- Normal follicular space
- Osteitis with pericoronitis
- Dentigerous cyst
- Ameloblastic fibroma
Question 3. Describe the differential diagnosis of radiolucent lesions in the posterior part of the body of the mandible.
Answer.
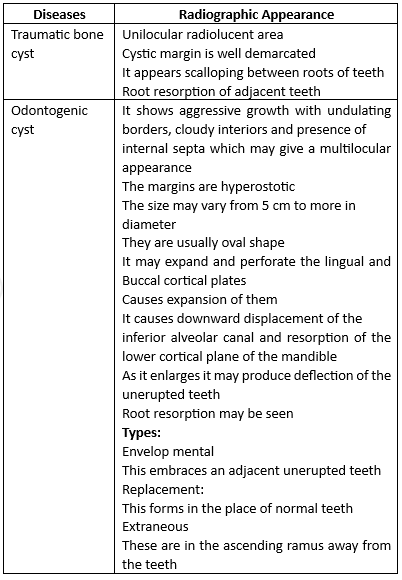
Radiolucent Lesions In the Posterior Part Of The Body Of the Mandible:
- Traumatic bone cyst
- Odontogenic keratocyst
- Ameloblastoma
- Cherubism
- Odontogenic myxoma
- Aneurysmal bone cyst
- Central hemangioma
Causes of periapical radiopaque lesions
Question 4. Discuss the differential diagnosis of periapical radiolucencies.
Answer.
True periapical radiolucencise:
- Pulpoperiapical Radiolucencies:
- Periapical granuloma:
- The lesion has well-circumscribed radiolucency
- It is somewhat rounded surrounding the apex of the tooth
- This may have thin radiopaque borders
- The involved may show deep restorations, extensive caries, fractures, or narrower pulp canals
- Its size is less than 2.5 cm in diameter
- Radicular cyst:
- It appears as a round or pear-shaped radiolucency at the apex of a nonvital tooth
- The radiolucency is more than 1.5 cm, but less than 3 cm in diameter, with a well defined hyperostotic borders
- The margins are smooth, well-defined, well-etched and continuous
- A radiopaque line of corticated bone is seen surrounding it
- The radiopaque border is continuous with lamina dura
- It may cause resorption of the roots
- The adjacent teeth are displaced
- There may be Buccal expansion
- There may be displacement of the antrum
- Periapical scar:
- A well-circumscribed radiolucency, that is smaller than granuloma and cyst
- The scar is constant in size
- Chronic and acute dentoalveolar abscess:
- The radiolucency may vary in size from small to quite large
- The initial lesion may even cause expansion of the jaws
- The margins may vary from well-defined to poorly defined-borders
- The involved tooth may show deep restorations, caries, narrowed pulp canals
- The roots may even show resorption
- Surgical defect:
- The radiolucency is usually rounded
- It is smooth-contoured
- It has well-defined borders
- It usually doesn’t measure more than 1 cm in diameter
- The radiolucency usually decreases in size
- Osteomyelitis:
- The density of the Involved bone is decreased
- Loss of sharpness of trabeculae
- Outline becomes blurred
- Gradually solitary or multiple radiolucent areas may be seen on the radiograph representing enlarged trabeculae spaces
- Saucer saucer-shaped area of destruction with irregular margins with teeth and some supporting bone is seen
- Inflammatory exudates may lift the periosteum, which is seen as a radiopaque line adjacent to and almost parallel or slightly convex to the surface
- There is a loss of continuity of lamina dura
- Pulpoperiapical disease:
- These appear as gray shadows that may be dome-shaped in the maxillary floor or a gray radiopacity that appears as a cap over the adjacent root
- The margin is usually smooth contoured and distinct
- Periapical granuloma:
- Dentigerous Cyst:
- It appears as well defined radiolucent lesion with a hyperostotic border associated with the crown of unerupted teeth
- It is usually unilocular
- It may envelop the crown symmetrically or may expand laterally
- The associated tooth may be displaced
- The outline of the larger cyst may expand from the ramus into the coronoid process or the condyle
- There may be resorption of the adjacent teeth
- Types:
- Central
- The crown is enveloped symmetrically
- Lateral
- Cyst results from the dilatation of the follicle on one aspect of the crown
- Circumferential
- This entire tooth is surrounded by the cyst
- Central
- Periapical Cementosseous Dysplasia:
- In the early stage, it occurs as radiolucencies that are usually somewhat rounded
- They have well-defined borders
- They are associated with vital pulp
- The lesions may be solitary or multiple
- They exceed 1 cm in diameter
- Periodontal Disease:
- Radiolucency is caused by advanced bone loss
- The entire bony support is lost
- The tooth may appear as floating in the radiolucency
- Traumatic Bone Cyst:
- The lesion exceeds size efficient to cause expansion of the cortical plates
- This produces a bony hard bulge on the jaws
- The lamina dura is intact
- The radiolucency is well-defined
- It is round to oval in shape
- The lateral and inferior borders of the elongated variety have smooth, regular borders
- Non Radicular Cyst:
- The most common structures seen are incisive canal cysts, median mandibular cysts, and primordial cyst
- Malignant Tumors:
- It may be found as a single periapical radiolucency
- Expansion of the jaw occurs in advanced conditions
- The expansion has a smooth surface covered with a normal structure
- Rarities:
- Ameloblastoma
- Aneurysmal bone cyst
- Cementifying and ossifying fibroma
- Cementoblastoma – early stage
- Giant cell granuloma
- Leukemia
Radiographic interpretation of periapical lesions
Periapical Radiolucency And Radiopacity Short Essays
Question 1. Differential diagnosis of periapical radiopacities.
Answer.
True Periapical Radiopacities:
- Condensing or sclerosingosteitis:
- The lesion is of variable size with margins that are well-defined or diffuse
- At the diffuse margins, the thickened trabeculae can be seen in continuation with the normal adjacent trabeculae
- The image is seen outside the lamina dura and periodontal spaces outlining the root
- Periapical idiopathic osteosclerosis:
- There may be solitary, multiple
- It may be unilateral or bilateral
- It may vary in size from 2 mm to cm in diameter
- May have a round or irregular shape
- The border may be distinct to indistinct, ragged, or blending with the adjacent bone
- Commonly seen in the mandible
- Sometimes deciduous molar roots are resorbed and replaced by sclerotic bone
- Peripheral or focal cement osseous dysplasia:
- It is predominantly round or oval with smoothly contoured borders
- It varies in diameter from 0.5 to 2 cm
- The mature lesion is uniformly dense
- It may have a thin radiolucent border
- The border may be vague
- Adjacent root shows hypercementosis
- Unerupted succedaneous teeth:
- The crowns of permanent teeth represent radiopacity
- Seen in patients under 12 or 13 years of age
- Foreign bodies:
- Radiopaque foreign bodies in the peri-apex is usually root canal-filling material
- Hypercementosis:
- The premolars are more often affected
- It may be confined to just a small region on the root producing a nodule or the whole root may be involved
- The altered shape of the root is apparent
- The root is surrounded by a normal periodontal ligament space and lamina dura
- On the anterior tooth, it may appear as a spherical mass of cementum attached to the root end
- Rarities:
- Calcifying odontogenic cyst
- Cementoossifying fibroma
- Chondroma
- Hamartoma
- Mature cementoblastoma
- Osteogenic sarcoma
False Periapical radiopacities:
- Anatomic structures:
- It includes the anterior nasal spine, malar process, external oblique ridge, mylohyoid ridge, mental protuberance, and hyoid bone
- Impacted teeth
- It may be situated directly at the apex of an erupted tooth
- Tori, exostosis,
- It may appear as a single or multiple lesion
- It is smoothly contoured, somewhat rounded, dense radiopaque masses
- These are not circumscribed by periodontal ligament and lamina dura
- Retained root tips
- They are projected over the apex of adjacent teeth
- The shape of the root, root canal, periodontal ligament, and lamina dura remain unaltered
- Foreign bodies
- Examples of such objects are metal fragments, zippers, hooks, jewelry, etc.
- Mucosal cyst of the maxillary sinus
- It appears relatively dense, dome-shaped mass with its base on the floor of the sinus
- Ectopic calcification
- It includes
- Sialoliths
- Rhinoliths
- Antroliths
- Calcified lymph nodes
- Phleboliths
- Anterial calcification
- Rarities:
- Calcified acne lesions
- Calcified hematoma
- Calcifying odontogenic cyst
- Squamous cell carcinoma
- Tonsilloliths
Periapical pathology radiographic features
Question 2. Differential diagnosis of multiple punched-out radiolucencies.
Answer.
Multiple Myeloma:
- They are usually bilateral
- It is seen in the mandibular posterior region and ramus
- It arrears as a small rounded and discrete radiolucency having punched out appearance
- There may be numerous areas of bone destruction within the region of generalized radiolucency
- Some lesions have an oval and cystic shape
- It has well-defined margins
- The border may have a thin sclerotic rim
- It has well-defined margins
- The border may have a thin sclerotic rim
- The lesion may vary in size
- The teeth may appear too opaque
- The mandibular lesion may cause thinning of the cortical lower border
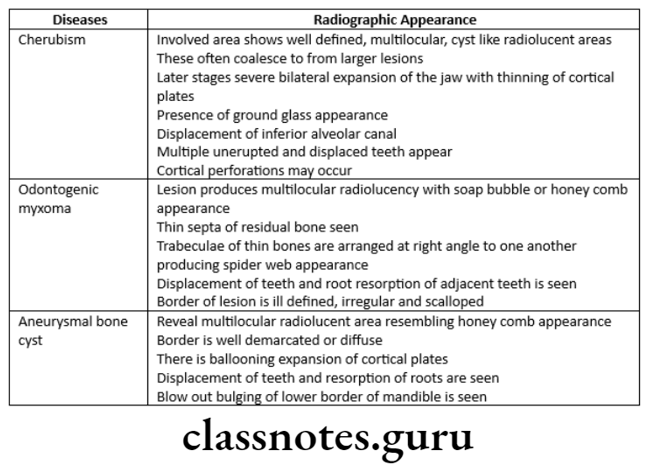
Cherubism
- It occurs bilaterally on rami
- The lesion grows slowly expanding but not perforating the cortex
- Usually, bony architecture returns to normal except for some that resemble ground glass appearance
Metastatic Carcinoma:
- It defined radiolucency
- It is seen in the mandible
- There may be multiple punched-out radiolucency when several nests of tumor cells are located close to each other
- There is a widening of PDL
- The cortical structures are destroyed
Periapical Radiolucency And Radiopacity Short Answers
Question 1. Periapical radiopacities.
Answer.
True Periapical Radiopacities:
- Condensing or sclerosing osteitis:
- At the diffuse margins, the thickened trabeculae can be seen in continuation with the normal adjacent trabeculae
- Periapical idiopathic osteosclerosis:
- May have a round or irregular shape
- The border may be distinct to indistinct, ragged, or blending with the adjacent bone
- Commonly seen in the mandible
- Periapical or focal cement osseous dysplasia:
- It is predominantly round or oval with smoothly contoured borders
- Unerupted succedaneous teeth:
- The crowns of permanent teeth represent radiopacity
- Seen in patients under 12 or 13 years of age
- Foreign bodies:
- Radiopaque foreign bodies in the periapex are usually root canal-filling material
- Hypercementosis:
- It may be confined to just a small region on the root producing a nodule or the whole root may be involved
- The altered shape of the root is apparent
- Rarities:
- Calcifying odontogenic cyst
- Cementoossifying fibroma
- Chondroma
- Hamartoma
- Mature cementoblastoma
- Osteogenic sarcoma
False periapical Radiopacities:
- Anatomic structures:
- It includes the anterior nasal spine, malar process, external oblique ridge, mylohyoid ridge, mental protuberance, and hyoid bone
- Impacted teeth:
- It may be situated directly at the apex of an erupted tooth
- Toxic, exostosis:
- It is smooth contoured, somewhat rounded, dense radiopaque masses
- Retained root tips:
- They are projected over the apex of adjacent teeth
- Foreign bodies:
- Examples of such objects are metal fragments, zippers, hooks, jewelry, etc.
- Mucosal cyst of the maxillary sinus:
- It appears relatively dense, dome-shaped mass with its base on the floor of the sinus
- Ectopic calcification:
- It includes
- Sialoliths
- Rhinoliths
- Antroliths
- Calcified lymph nodes
- Phleboliths
- Arterial calcification
- Rarities:
- Calcified acne lesions
- Calcified hematoma
- Calcifying odontogenic cyst
- Squamous cell carcinoma
- Tonsilloliths
Diagnosis of periapical radiolucency
Question 2. Radiographic features of cherubism
Answer.
Radiographic features of cherubism
- The involved area shows well-defined, multilocular, cyst-like radiolucent areas
- These often coalesce to form larger lesions
- Later stages cause severe bilateral expansion of the jaw with thinning of cortical plates
- Presence of ground-glass appearance
- Displacement of the inferior alveolar canal
- Multiple unerupted and displaced teeth appear
- Cortical perforations may occur
