Chronic And Granulomatous Inflammation Important Notes
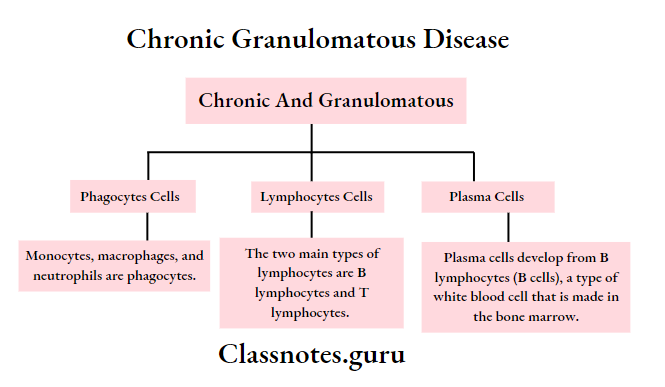
1. Chronic inflammatory lesions are infiltrated by mononuclear inflammatory cells like phagocytes, lymphocytes, and plasma cells
- Macrophages comprise the most important cells in chronic inflammation
- Chronic granulomatous inflammation is characterized by the formation of granulomas which are tiny circumscribed lesions composed predominantly of a collection of modified macrophages called epitheloid cells and are rimmed at the periphery by lymphoid cells
2. Giant cells
- They are multinucleated cells derived from monocytes or macrophages
- The nuclei may be arranged
- In horseshoe pattern
- Clustered at two poles – Langhans giant cells
- Present centrally – foreign body giant cells
- Langhans giant cells occur mostly in granulomas
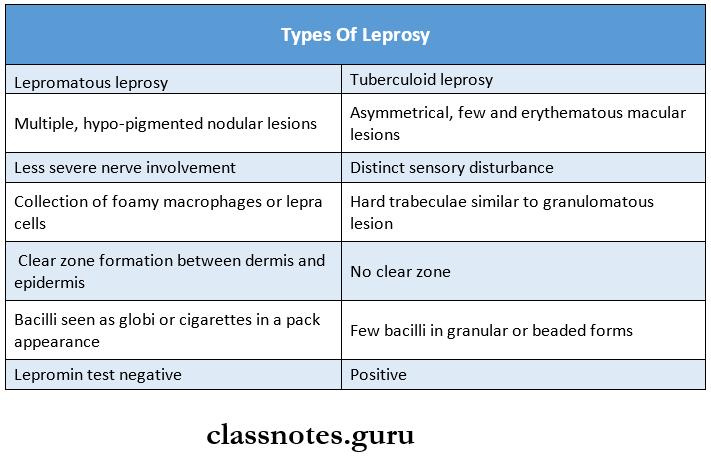
3. Types of leprosy
4. Lepromin test
- It involves intradermal injection of lepromin an antigenic extract of M.leprae
- It is used for classifying leprosy on the basis of immune response
- It reveals delayed hypersensitivity reactions in patients of tuberculoid leprosy
- Patients with lepromatous leprosy are negative for the test
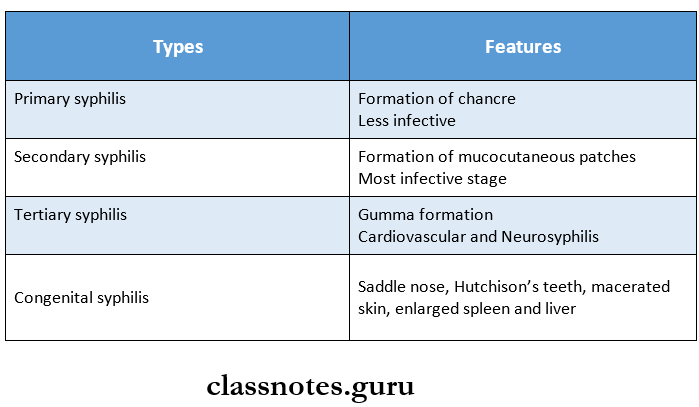
5. Types of syphilis
6. Types of tuberculosis
- Primary tuberculosis/ Ghons complex/ Childhood tuberculosis
- Secondary tuberculosis/ Post-primary reinfection/ Chronic tuberculosis
7. Fate of primary tuberculosis
- The lesions commonly do not progress but instead, heal by fibrosis and in time undergo calcification and even ossification
- Continuous to grow and the caseous material is disseminated through bronchi to other parts of the same lung or opposite lung
- Bacilli may enter the circulation through erosion in the blood vessel and spread to other tissues and organs resulting in military tuberculosis
- Healed lesions of primary tuberculosis may get reactivated and cause progressive second tuberculosis
Read And Learn More: Pathology Question And Answers
8. Fate of secondary tuberculosis
- Lesions may heal with fibrous scarring and calcification
- Lesions may coalesce and produce progressive secondary pulmonary tuberculosis along with
- Fibrocaseous tuberculosis
- Tuberculous caseous pneumonia
- Military tuberculosis
9. Ghon’s complex
- It consists of three components
- Pulmonary component
- Lesion of the lung is the primary focus
- It is 1-2 cm solitary area of tuberculous pneumonia located peripherally under a patch of pleurisy
- Lymphatic vessel component
- Lymph node component
- This consists of hilar and tracheobronchial lymph nodes in the area drained.
- These affected lymph nodes are matted and show caseation necrosis
- Pulmonary component
Chronic And Granulomatous Inflammation Long Essays
Question 1. Describe briefly the serological diagnosis of syphilis.
Answer:
1. Microscopy:
- It is useful in primary and secondary syphilis
- Direct fluorescent antibody test is used for T. pal¬lidum
- In this method, acetone fixed smear is subjected to fluorescently tagged anti-T, pallidum antiserum
2. Serological tests:
- Tests for antibodies reacting with cardiolipin anti¬gen
- Standard tests for syphilis
- Wassermann test
- It is a complement fixation test
- Serological tests Method:
- The patient’s serum is inactivated by heating at 56° C for 30 minutes
- Incubated with cardiolipin antigen and guinea pig antigen at 37° C for 1 hour
- The indicator is added to detect the presence or absence of a complement
- Serological tests Interpretation:
- If hemolysis does not occur, it indicates that the complement is utilized
- This is positive Wassmann’s reaction
- If hemolysis takes place, it indicates the complement is not been utilized in the primary reaction but utilized by the indicator system
- Serological tests Method:
- It is a complement fixation test
- Kahn test
- It is a tube flocculation test
- Kahn test Method:
- 0.15 ml of inactivated serum is taken in three test tubes containing 0.05, 0.025, and 0.0125 ml of freshly prepared antigen dilution
- Tubes are shaken on Kahn’s shaken and examined
- Kahn test Interpretation:
- The negative test shows uniform opalescence
- A positive test shows floccules
- Kahn test Method:
- It is a tube flocculation test
- VDRL test
- In this test, the inactivated serum is mixed with cardiolipin antigen on a special slide and rotated for 4 minutes
- Uniform distribution of crystals in the drop indicates the serum is non reacting
- The formation of clumps indicates it is reactive
- Wassermann test
- Standard tests for syphilis
- Tests for antibodies reacting with group-specific treponemal antigen
- Reiter protein complement fixation test
- In this method, lipopolysaccharide protein complex antigen derived from the cultivable Reiter’s stain is used
- It is less sensitive
- Reiter protein complement fixation test
- Tests for specific antibodies to pathogenic treponema
- Treponema pallidum immobilization test
- It employs live T. pallidum
- The test serum is mixed with actively motile Nichol’s strain of T. pallidum and incubated anaerobically
- If antibodies are present, the treponemas are immobilized
- Fluorescent treponemal antibody absorption
- Test serum is preabsorbed with an extract of nonpathogenic treponemas to remove group-specific antigens
- It detects IgM and IgG
- It is the earliest test to become positive
- Microhaemagglutination test for treponema pallidum
- T. pallidum antigen is coated onto the surface of red cells
- Tanned sheep RBCs are sensitized with an extract of T. pallidum
- When these sensitized erythrocytes are mixed with the patient’s serum containing anti¬bodies, the erythrocytes clump together
- Enzyme immunoassay
- They have been developed using T. pallidum antigens and are available commercially
- Treponema pallidum immobilization test
Question 2. Define granuloma. What are the causes and pathology of granuloma?
Answer:
- Granuloma: Granuloma is defined as circumscribed, tiny lesion, about 1 mm in diameter, composed predominantly of a collection of modified macrophages called epitheloid cells and rimmed at the periphery by lymphoid cells.
Besides the presence of epitheloid cells and lymphoid cells, granuloma have giant cells, necrosis, and fibrosis.
Granuloma Etiology:
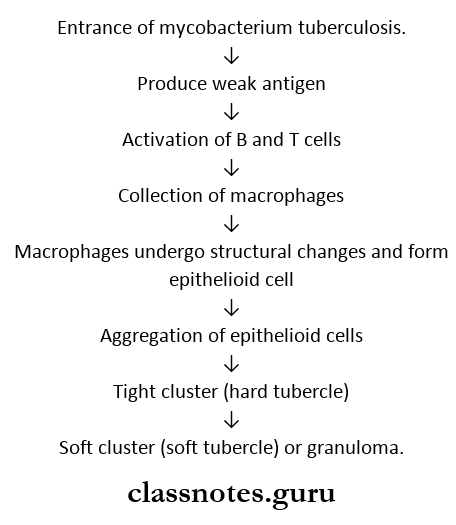
- Tuberculosis is an infection caused by a rod-shaped, non-spore-forming, aerobic bacterium called mycobac¬terium tuberculosis.
- The organism is spread by small airborne droplets generated by coughing, sneezing, and talking to a person with pulmonary/laryngeal tuberculosis.
- Introduction of M-tuberculosis into the lungs leads to infection of the respiratory system, however, they can spread to other organs such as the lymphatics, pleura, bones/joints, and meninges and cause extrapulmonary tu¬berculosis.
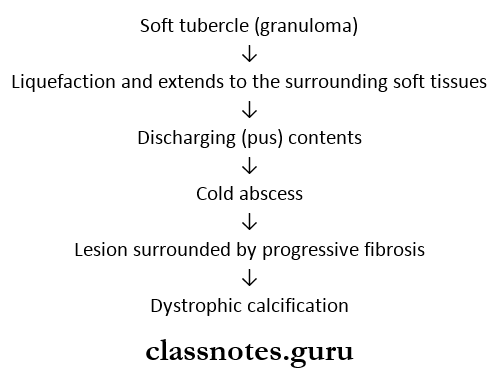
Evolution of tubercle:
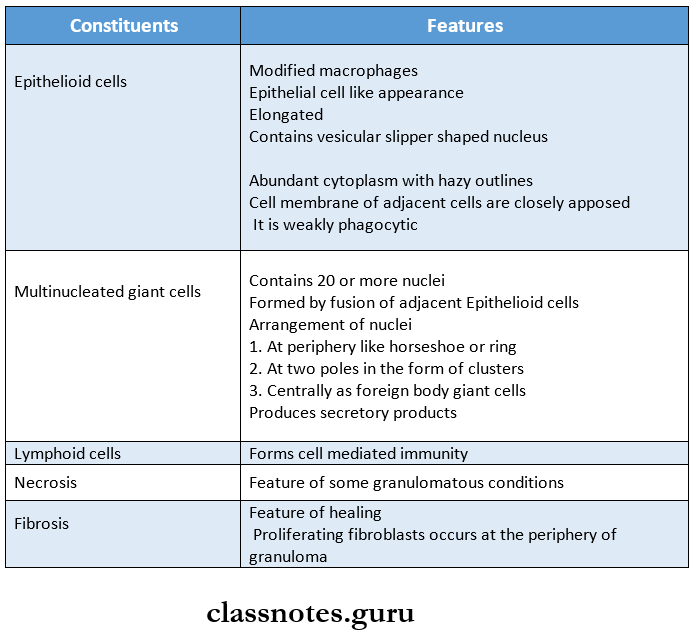
Constituents of granuloma:
- Epitheloid cells,
- Lymphoid cells,
- Giant cells,
- Necrosis,
- Fibrosis.
The fate of granuloma:
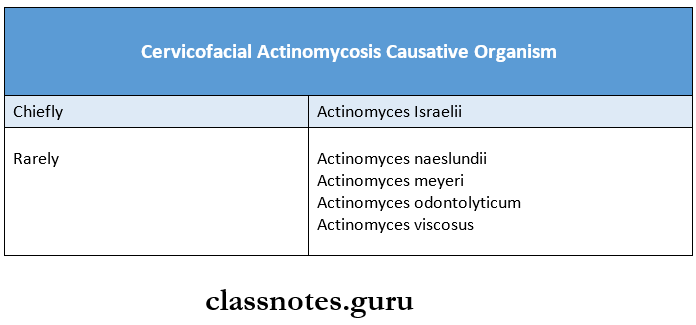
Question 3. Write briefly on cervicofacial actinomycosis.
Answer:
Cervicofacial actinomycosis is the commonest form of actinomycosis
Cervicofacial actinomycosis Causative Organism:
Site Involved:
- Cheek
- Submaxillary regions
Route of Infection:
- Tonsils
- Carious tooth
- Periodontal disease
- Trauma following tooth extraction
Cervicofacial actinomycosis Features:
- Initially, a firm swelling appears in the lower jaw
- Gradually, the mass breaks down
- This leads to abscesses and sinus formation
Cervicofacial actinomycosis Microscopic Features:
- The pus contains typical tiny yellow sulfur granules
- Abscess is present in the center of the lesion
- Periphery contains inflammatory cells, giant cells, and fibroblasts
- Radiating filaments demonstrating ray fungus, actino- myocytes appears in the center
- These filaments are hyaline, eosinophilic with club-like ends
- These demonstrate secreted immunoglobulins
Cervicofacial actinomycosis Complications:
- Spreading of infection into adjacent soft tissues
- Destruction of bone
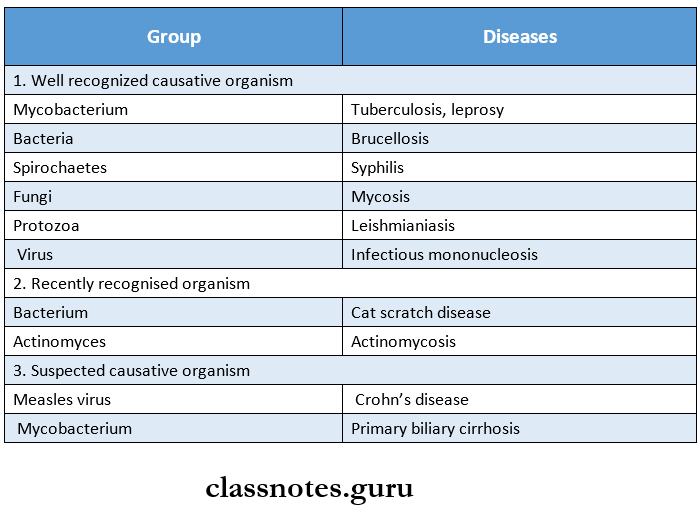
Question 4. Classify granuloma. Describe the etiopathogenesis and pathology of tuberculosis.
Answer:
Granuloma Classification:
Granulomatous diseases are grouped into three groups as follows:
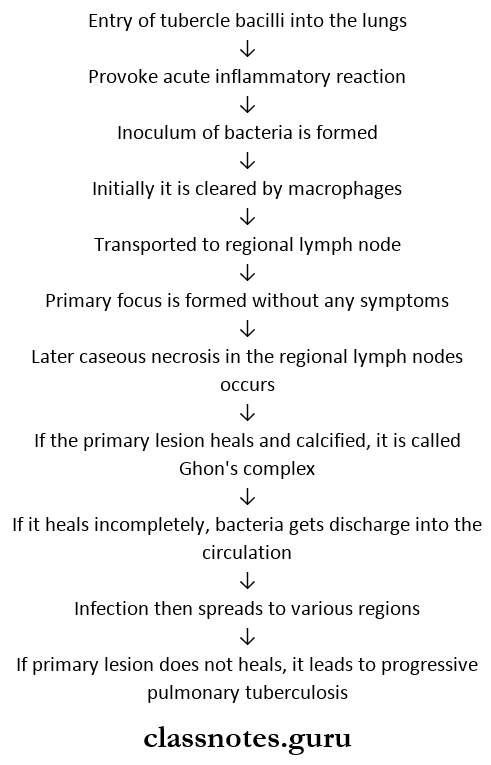
Tuberculosis Etiopathogenesis:
Tuberculosis Pathology:
1. Gross appearance
- The tuberculous cavity is spherical
- It has a thick fibrous wall
- Around the wall, foci of solidification are seen
- The wall is lined by yellowish, caseous, necrotic mate¬rial.
- Lumen contains thrombosed blood vessels
2. Microscopic appearance
- Lesions consist of tuberculous granuloma with caseation necrosis
- The wall of the cavity shows eosinophilic, granular, caseous material
- The outer wall shows fibrosis
- Granulomas consist of epithelioid cells, Langhan’s giant cells, and lymphocytes.
Question 5. Write briefly about the etiopathogenesis of tuberculosis. Describe the complications of secondary pulmonary tuberculosis.
Answer:
Secondary pulmonary tuberculosis Complications:
- Localized, apical, secondary pulmonary tuberculosis may heal with fibrous scarring and calcification.
- Lesions may coalesce together to form a larger area of tuberculous pneumonia and produce progressive secondary pulmonary tuberculosis with the following pulmonary and extra-pulmonary involvements
1. Fibrocaseous tuberculosis:
- The tubercular cavity is spherical with a thick fibrous wall, lined by yellowish, caseous, necrotic material, and the lumen is transversed by thrombosed blood vessels.
- Microscopically, the wall of the cavity shows eosinophilic, granulancaseous material which may show foci of dystrophic calcification. Widespread coalesced tuberculous granulomas composed of epithelioid cells, Langerhan s giant cells, and peripheral mantle of lymphocytes having central caseous necrosis are seen the outer wall of the cavity showing fibrosis.
Fibrocaseous tuberculosis Complications:
- May produce hemoptysis
- Extending to the pleura produces bronchopleural fistula.
- Tubercular empyema
- Thickened pleura.
2. Tuberculosis caseous pneumonia:
- In an individual with a high degree of hypersensitiv¬ity, secondary pulmonary tuberculosis may spread to the rest of the lung, producing caseous pneumonia.
3. Systemic military tuberculosis:
- This is lymphohaematogenous spread to tuberculous infection from the primary focus/later stages of tuberculosis.
- Spread may occur to systemic organs/isolated organs.
- The spread is either by the entry of infection into the pulmonary vein producing disseminated/isolated organ lesions in different extrapulmonary sites (for example liver spleen, kidney) or into the pulmonary artery re¬stricting the development of military lesions within the lung.
- Military lesions are millet seed-size (1mm diameter), yellowish, firm areas without grossly visible caseation necrosis.
Question 6. List common examples of a granuloma, and describe the pathogenesis and effects of any one.
Answer:
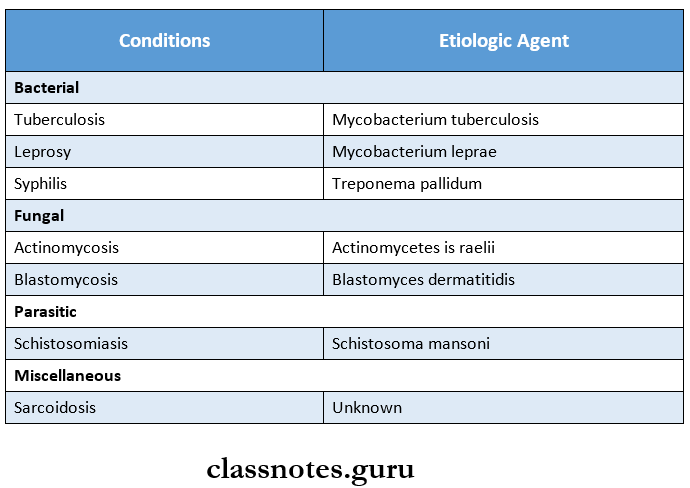
Common examples of granuloma:
1. Bacterial Tuberculosis,
- Leprosy,
- Syphilis,
- Granuloma inguinale,
- Brucellosis,
- Cat scratch disease,
- Taularemia,
- Glanders
2. Fungal
- Actinomycosis,
- Blastomycosis,
- Cryptococcosis,
- Cocci diomycosis
3. Parasitic
- Schistosomiasis
4. Miscellaneous
- Sarcoidosis,
- Crohn’s disease,
- Silicosis
- Berylliosis,
Effects of Tuberculosis:
- Productive cough
- Haemoptysis
- Pleural effusion
- Dyspnoea
- Orthopnea
- Fever
- Night sweats
- Fatigue
- Loss of weight
- Loss of appetite
- Pulmonary insufficiency
- Pulmonary hemorrhage
- Sepsis
- Secondary amyloidosis
Chronic And Granulomatous Inflammation Short Essays
Question 1. Classify leprosy. Describe the pathology of tuberculoid leprosy.
Answer:
Leprosy: Leprosy/Hansen’s disease is a slow communicable disease caused by mycobacterium lepra.
- It can be classified into 2 types based on the resistance offered as follows.
- Lepromatous leprosy (represents low resistance)
- Tuberculoid leprosy (represents high resistance)
- Leprosy is classified into 5 clinicopathologic groups (modified Ridley and Jopling’s classifica¬tion).
- TT – Tuberculoid polar
- BT – Borderline tuberculoid
- BB – Mid borderline (dimorphic)
- BL – Borderline lepromatous
- LL – Lepromatous polar.
Tuberculoid leprosy:
- Tuberculoid leprosy is characterized by asymmetrical skin lesions that are hypopigmented and erythematous macules.
- Nerve involvement is with the distinct sensory distribution.
- Histopathological features include hard tubercles similar to granulomatous lesions eroding the basal layer of the epidermis.
- Lepra bacilli are few and seen in destroyed nerves.
Question 2. Oral lesions of syphilis
Answer:
- Syphilis is a sexually transmitted disease caused by spirochaetes, treponema pallidum.
- Syphilis is divided into 3 stages depending upon the period after which the lesions appear and the type of lesions.
- They are primary, secondary, and tertiary.
- Oral lesions occur in secondary syphilis known as mucous patches, on the tongue, gingiva, etc. or as a split papule on lips, which are highly infectious.
- Tertiary/late syphilis/gumma is a granuloma with central necrosis, noninfectious, and is most common on the tongue and palate.
- Palatal perforation by ulcer after vigorous antibiotic use is known as the Herxheimer reaction.
- In congenital/prenatal syphilis, the most constant finding is relatively short roots of mandibular permanent 1st molars, short maxilla, Hutchinson triad (teeth, eye/ear involved), hypoplasia of incisors and molars i. e., notched incisors and mulberry molars.
- Treatment: Penicillin is the drug of choice.
Question 3. What is Ghon’s complex? Mention the lab diagnosis of tuberculosis.
Answer:
Mode of transmission:
- Usually direct by inhalation of air-borne organisms.
- By exposure to contaminated secretions of infected persons
- By drinking milk contaminated with Mycobacterium bovis.
- The most commonly involved tissues for the primary complex are the lung and hilar lymph nodes.
- Ghon’s complex in the lungs consists of 3 components as follows:
1. Pulmonary component:
- The lesion in the lung is primary focus) Ghon’s focus. It is a 1 – 14 cm solitary area of grey-white inflammatory consolidation.
- Tubercle bacilli either free/within phagocytes drain to the regional lymph nodes, which often caseate. This combination of parenchymal lesion and nodal involvement is referred to as Ghon’s complex.
2. Lymphatic vessels component:
- Lymphatics draining the lung lesions contain phagocytes containing bacilli and may develop beaded, military tubercles along the path of hilar lymph nodes.
3. Lymph node component:
- Consists of enlarged hilar and tracheobronchial lymph nodes in the area drained. The affected lymph nodes are matted and show caseation necrosis.
Diagnosis of tuberculosis is made by the following tests
- Positive Mantoux skin test.
- Positive sputum for AFB.
- Complete haemogram (lymphocytosis and raised ESR)
- Chest X-ray (characteristic hilar nodules and other parenchymal changes)
- Fine needle aspiration cytology of an enlarged peripheral lymph node is quite helpful for confirmation of diagnosis.
Question 4. Primary tuberculosis.
Answer:
- Primary tuberculosis or Ghon’s complex is the infection of an individual who has not been previously infected/ immunized
- It consists of 3 components
- Pulmonary component
- It is a lesion in the lung
- It is 1-14 cm solitary area of grey-white inflammatory consolidation
- Tubercle bacilli either free/within phagocytes drain to the regional lymph nodes which often caseate
- This combination of parenchymal lesion and nodal in¬volvement is referred to as Ghon’s complex
- Lymphatic vessel component
- Lymphatics draining the lung lesions contain phagocytes containing bacilli and may develop beaded, mili¬tary tubercles along the path of hilar lymph nodes
- Lymph node component
- Consists of enlarged hilar and tracheobronchial lymph nodes in the area drained
- The affected lymph nodes are matted and show casea¬tion necrosis
Chronic And Granulomatous Inflammation Short Question And Answers
Question 1. Gumma
Answer:
- Syphilitic gumma is a lesion caused by tertiary syphilis
- It is a solitary, localized rubbery lesion with central necrosis seen in the original like liver, testis, bone and brain-associated scarring of hepatic parenchyma.
- Histologically, the structure of gumma shows the following:
- Central coagulative necrosis resembles caseation but is less destructive so that outlines of necrotic cells can still be seen.
- Surrounding zone of palisaded macrophages with lymphocytes, plasma cells, giant cells, and fibroblasts.
Question 2. Morphology of granuloma
Answer:
Granuloma consists of:
Question 3. Granulomatous inflammation
(or)
Chronic Granulomatous inflammation
Answer:
Granulomatous inflammation is a typical reaction to poorly digestible agents elicited by tuberculosis, lep¬rosy, fungal infections, etc.
Examples:
Question 4. Actinomycosis
Answer:
- Actinomycosis is a chronic suppurative disease caused by anaerobic bacteria, actinomycetes Israeli.
- The infection is always endogenous in origin. The or¬ganisms invade, proliferate and disseminate in favour¬able conditions.
- Based on the anatomical location of lesions, actinomycosis is of the following types:
- Cervico facial
- Thoracic
- Abdominal
- Pelvic.
- Of all the types, cervicofacial actinomycosis is the com¬monest from.
- Microscopically, in all the types:
- The inflammatory reaction is a granuloma with central suppuration.
- The Centre of each abscess contains a bacterial colony ‘sulfur granule’ characterized by radiating filaments.
- Bacterial strains reveal the organisms as nonacid, fast, gram-positive filaments.
Question 5. Primary complex
Answer:
- Primary complex/Ghon’s complex/childhood tubercu¬losis/ is the primary tuberculosis. Is the infection of an individual who has not been previously in- infected/immunized.
- It consists of 3 components:
- Pulmonary component
- Lymphatic vessel component
- Lymph node component
- The most commonly involved tissues for the primary complex are the lung and hilar lymph nodes.
- Tubercle bacilli, either free/within phagocytes drain the regional lymph nodes, which often caseate.
- This combination of parenchymal lesion and nodal in¬volvement is referred to as Ghon’s complex.
Question 6. Congenital syphilis
Answer:
Congenital syphilis’s Major features are:
- Hutchinson’s triad – which includes.
- Hutchinsons’s teeth – small, widely spaced, peg-shaped permanent teeth.
- Notched central incisors
- Intestinal keratitis with blindness and deafness from 8th cranial nerve injury.
- Saddle shaped nose
- Bony lesions like epiphysis and periostitis
- Mucocutaneous lesions of acquired secondary syphilis
- Diffuse fibrosis in the liver.
Question 7. Lepromatous leprosy
Answer:
- Leprosy caused by mycobacterium leprae is of 2 types of which lepromatous leprosy represents low resis¬tance and tuberculoid leprosy represents high resis¬tance.
- Lepromatous leprosy is characterized by multiple symmetrical skin lesions that are hypopigmented and erythematous maculopapular/nodular.
- Nerve involvement is present with less serve sensory distribution.
- Histopathology involves the collection of foamy macro¬phages/lepra cells in the dermis separated from the epidermis by a clear zone.
Question 8. Pathological lesions of syphilis
Answer:
- Primary chancre
- Regional lymphadenopathy
- Maculopapular rash
- Mucous patches
- Snail track ulcers
- Flat papules around the anus
- Tertiary gumma
- Meningitis
- Cranial nerve palsies
- Generalized paralysis of insane
Question 9. What is tuberculoid granuloma? Give three examples
Answer:
- Tuberculoid granuloma is defined as circumscribed, tiny lesion about 1 mm in diameter, composed predominantly of a collection of modified macrophages called epitheloid cells and rimmed at the periphery by lymphoid cells.
- It is caused by mycobacterium tuberculosis that has 5 pathogenic strains. Hominis, bovis, avian, murine, and cold-blooded vertebrate strains.
- Different organs may be affected by mycobacterium tuberculosis, which lung is the most common organ.
- Pulmonary tuberculosis
- Intestinal tuberculosis
- Hyperplastic caecal tuberculosis.
Question 13. Tuberculoid type of leprosy
Answer:
- Tuberculoid leprosy is characterized by asymmetrical skin lesions that are hypopigmented and erythematous macules.
- Nerve involvement is with the distinct sensory distribution.
- Histopathological features include hard tubercles similar to granulomatous lesions eroding the basal layer of the epidermis.
- Lepra bacilli are few and seen in destroyed nerves.
Question 14. Chancre
Answer:
- Chancre is a typical lesion of primary syphilis that appears on genitals/at extragenital sites in 2-4 weeks after exposure to infection.
- Initially, the lesion is a painless papule which ulcerates in the center so that the fully developed chancre is an indurated lesion with central ulceration accompanied by regional lymphadenitis.
- Chance heals without scarring, even in the absence of treatment
Question 15. Giant cells
Answer:
- In chronic inflammation, when the macrophages fail to deal with particles to be removed, they fuse together and form multinucleated giant cells.
- Giant cells are normally seen in cells like osteoclasts of bone, trophoblasts in the placenta, and megakaryocytes in bone marrow.
- Morphologically different cells are seen in chronic in¬flammation and tumors.
Giant cells in inflammation:
- Foreign body giant cells: Chronic infective granuloma, leprosy, and TS.
- Langerhans giant cells: Sarcoidosis and tuberculosis.
- Taunton’s giant cells: Xanthoma
- Aschoffs giant cells: Rheumatic nodules.
Giant cells in tumors:
- Anaplastic cancer giant cells: Seen in carcinoma of the liver and various soft-tissue sarcomas.
- Reed – Sternberg cells: Hodgkin’s lymphoma.
- Giant cells tumor of bone: Uniform distribution of os¬teoclastic giant cells spread in the stroma.
Question 16. Lepra reaction
Answer:
Lepra reaction/reactional leprosy:
- There may be of 2 types
- Type 1 (Reversal reactions),
- Type 2 (Erythema, nodosumleprosum)
Type 1: The polar forms of leprosy do not undergo any change in the clinical and histopathological picture.
Borderline groups are unstable and may move across the spectrum in either direction with upgrading/downgrading of the patient’s immune state.
1. Upgrading reaction:
- Characterized by increased cell-mediated immunity and occurs in patients of border¬line lepromatous (BL) type on treatment who up¬grade/shift towards tuberculoid type.
2. Downgrading reaction:
- Characterized by lowering of cellular immunity and is seen in borderline tuber¬culoid (BT) type who downgrade/shift towards lepromatous type.
Type 2: Occurs in lepromatous patients after treatment. It is characterized by tender cutaneous nodules, fever, iridocyclitis, synovitis, and lymph node involvement.
