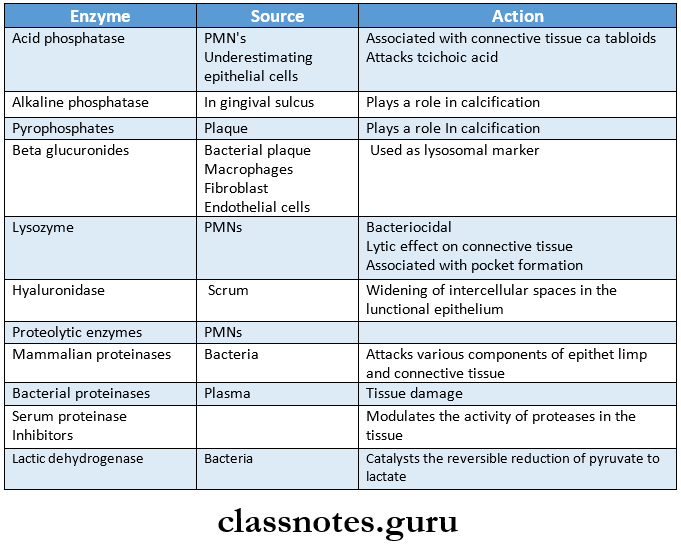
Question 1. Enzymes in the gingiva.
Answer:
Question 2. Cells of Periodontal Ligaments.
Answer:
1. Synthetic Cells:
Osteoblasts:
- Covers the periodontal surface of the alveolar bone
- It actively synthesizes ribosomes
- Contains a largely open nucleus containing prominent nucleoli
Read And Learn More: Periodontics Question and Answers
2. Fibroblasts, spindle-shaped cells:
- Most prominent cell
- Synthesizes chondroitin sulfates, heparin sulfate, and hyaluronan sulfate
- Synthesizes connective tissue matrix
Fibroblasts, spindle-shaped cells Produces:
- Collagen fibers
- Reticulin fibers
- Oxytalan fibers
- Elastin fibers
1. Cementoblast:
- Seen lining cementum
- Lay down cementum
2. Resorptive cells:
- Osteoclast:
- Multinucleated giant cell
- Lies adjacent to the bone
- Undergoes resorption of bone
- Formed by monocytes
- Fibroblast:
- Contain fragments of collagen
- These undergoes digestion
- Results in resorption of bone
- Cementoclast:
- Located in Howships Lacunae
- Causes resorption of cementum
3. Progenitor cells:
- Formed in the basal cell layer
- Basal cells have the ability to divide
- One of the divided cells migrates to the superficial layer and the other remains as a progenitor cell
4. Epithelial cell rests of Malassez:
- Remnants of Hertwig’s epithelial root sheath
- Present near and parallel to root surfaces Attached to one another by desmosomes
- During disease conditions, they undergo proliferation
- Persists as a network strand, island, or tubule
- Exhibits tonofilaments
5. Mast Cell:
- Small, round, or oval cell
- Contains cytoplasmic granules
- Contains heparin and histamine
- During an inflammatory response, these releases of histamine cause antigen-antibody formation
6. Macrophages:
- Capable of phagocytosis
Question 3. Functions of Periodontal ligament.
Answer:
1. Physical Functions of Periodontal ligament:
- Provide soft tissue casing
- Protect nerves and vessels from injury
- Transmit occlusal forces to the bone
- By stretching of oblique fibers of PDL
- Transmits tensional force to the bone
- Results in bone formation
- Attaches tooth to the bone
- Maintains architecture of gingival tissue
- Shock absorbent
2. Formative and Remodelling function:
- Synthesis and resorption of cementum, PDL, and al-alveolar bone
- Old cells and fibers are replaced by a new one
3. Nutritional and Sensory function:
- Nutrition – Through blood supply
- Sensory – Transmits sensation of touch, pressure, and pain to CNS
Neural Transmission Functions of Periodontal ligament :
- Apical area – Ruffini
- Apex Pressure and vibration endings
- Mid root – Meissners corpuscles
Question 5. Define alveolar bone and describe its composition.
Answer:
Alveolar Bone is that portion of the maxilla and mandible that forms and supports the tooth socket
Alveolar Bone Composition:
Cells:
1. Osteoblast: Cuboidal cells
Osteoblast Contains:
- Rough endoplasmic reticulum
- Large Golgi apparatus
- Secretory vesicles
Osteoblast Functions:
- Synthesize osteoid, collage
- Regulate mineralization
Osteoblast Precursor: Progenitor cells
2. Osteoclasts: Multinucleated giant cells
Osteoclasts Precursor: blood-borne monocytes
Osteoclasts Functions: Resorptive cell, Secretes hydrolytic en-zymes
3. Osteocytes: These extend processes from lacunae to canaliculi
Osteocytes Function: Canaliculi bring oxygen and nutrients to osteocytes
4. Extracellular Matrix:
Extracellular Matrix Inorganic:
- Calcium, Hydroxyl
- Phosphate, Carbonate
- Citrate, Sodium
- Magnesium, Fluorine
Extracellular Matrix Organic:
- Osteocalcin
- Osteonectin
- BMP
- Proteoglycans
- Glycoproteins
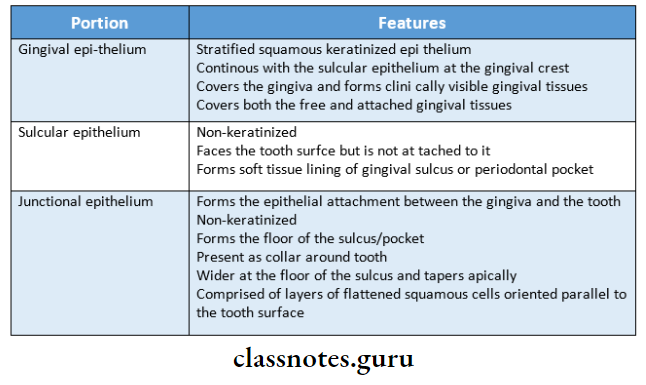
Question 6. Dentogingival junction.
Answer:
- The junctional epithelium and the gingival fibers are together considered a dentogingival unit
Dentogingival Junction:
- The Dentogingival Junction represents a unique anatomic feature concerned with the attachment of the gingiva to the tooth
- The Dentogingival Junction comprises an epithelial portion and a connective tissue portion
1. Epithelial portion It can be divided into
- Gingival epithelium
- Sulcular epithelium
- Junctional epithelium
2. The connective tissue component contains densely packed collagen fiber bundles.
- Dentogingival fibers
- Extends from cementum into free and at-attached gingiva
- Alveologingival fibres
- Extends from the alveolar crest into free and at-attached gingiva
- Circular fibers
- Wrap around the tooth
- Dentoperiosteal fibres
- Run from cementum, over the alveolar crest, and insert into the alveolar process
- Transseptal fibers
- Runs interdentally from cementum to one tooth to the adjacent tooth
Question 7. Sulcular Epithelium.
Answer:
- Sulcular epithelium is the epithelium lining the gingival sulcus
- Sulcular epithelium is a thin,non-keratinized stratified squamous epithelium without recipes
- Sulcular epithelium extends from the coronal limit of the junctional epithelium to the crest of the gingival margin
- Sulcular epithelium usually shows many cells with hydropic degeneration
- Sulcular epithelium lacks granulosum and corneum strata
- Enzymes present have a lower degree of activity
- Sulcular epithelium has the potential to keratinize if
- It is exposed to the oral cavity or
- The bacterial flora of the sulcus is totally eliminated
Sulcular Epithelium Importance:
- Sulcular epithelium may act as a semipermeable membrane through which injurious bacterial products pass into the gingival and tissue fluid from the gingiva seeps into the sulcus
Question 8. Fenestrations and Dehiscences.
Answer:
Fenestration:
- These are isolated areas in which the root surface is covered only by the periosteum and gingiva
- Marginal bone is intact
Dehiscence:
- Defect involving denudation of marginal bone
Etiology:
- Root prominence
- Malposition
- Teeth in labial version
Common location:
- Site – Facial bone
- Teeth involve – Anterior
Importance:
- Affect the outcome of surgical treatment
Question 9. Define and classify cementum. (or) Schroeder’s classification of cementum
Answer:
Cementum:
- It is a calcified avascular mesenchymal tissue that forms the outer covering of the anatomic root
Cementum Classification:
1. Acellular fibrillar cementum:
- Contains a mineralized ground substance
- Does not contain fibres or cells
Acellular fibrillar cementum Site: On enamel near CEJ
2. Acellular extrinsic fiber cementum:
- Contains Sharpey’s fibers
- Does not contain cells
Acellular extrinsic fiber cementum Site: Coronal half of root surface
3. Cellular mixed stratified cementum:
- Contains cells and fibres
Cellular mixed stratified cementum Site: Apical third of root, apices, and furcation areas
4. Cellular Intrinsic Fiber cementum:
- Contains fibers but not cells
Cellular Intrinsic Fiber cementum Site: Resorption lacunae
5. Intermediate Cementum:
Intermediate Cementum Site: Apical 1/3rd of root
Intermediate Cementum Function: Attaches cementum to dentin
- This is removed during root planning
Question 10. Junctional epithelium.
Answer:
- Junctional Epithelium is the tissue that joins to the tooth on one side and the oral sulcular epithelium and connective tissue on the other
- Junctional Epithelium forms the base of the sulcus
Junctional epithelium Attachment:
- Attach to the tooth surface
- By internal basal lamina
- Reinforced by the gingival fibers
- Consists of lamina dens and lamina lucida
- Attach to gingival connective tissue
- By external basal lamina
Junctional epithelium Features:
- Consists of non-keratinizing epithelium
- Thickness
- Early life- 3-4 layers
- Later- Increases
- Length- 0.25-1.35 mm
Junctional epithelium Structure:
- Consists of basal and suprabasal layer
- Zones present are
- Apical- germination
- Middle- adhesion
- Coronal-permeable
- Cells present are
- Basal cells- cuboidal/flattened
- Suprabasal cells
- Complex microvilli formation and interdigitation
- Presence of leukocytes and lymphocytes
- Desmosomes interconnect the cells
Question 11. Oxytalan fibers.
Answer:
- The periodontal ligament contains two immature forms of fibers
- Oxytalan fibers are xylan and cleaning fibers
- The xylan fibers run parallel to the root surface in a vertical direction and bend to attach to the cementum. in the cervical third of the root
- Oxytalan fibers are associated with blood vessels and nerves of the periodontal ligament
- Oxytalan fibers regulate the vascular flow
- An elastic meshwork in the periodontal ligament is composed of many elastic lamellae with peripheral oxy- talan fibers and cleaning fibers
- Oxytalan fibers develop de novo in the regenerated periodontal ligament
Question 12. Describe the mechanism by which ligament periodontal resists occlusal forces.
Answer:
1. Tensional theory:
- Tensional Theory states that the principal fibers of the periodontal ligament are major factors in supporting the tooth and transmitting forces to the underlying bone
- When a force is applied to the crown, the principal fibers first unfold and straighten and then transmit forces to the alveolar bone
- When the alveolar bone has reached its limit, the load is transmitted to the basal bone
2. Viscoelastic theory:
- Viscoelastic Theory states that the displacement of the tooth is controlled by fluid movements with fibers having only a secondary role
- When forces are transmitted to the tooth, the ex-intracellular fluid passes from the periodontal ligament into the marrow spaces of bone through fo- the lamina
3. Thixotropic theory:
- According to this theory, the periodontal ligament has rheological behavior of thixotropic gel
Question 13. Significance of width of attached gingiva
Answer:
- The width of the attached gingiva is the distance between the mucogingival junction and the projection on the external surface of the bottom of the gingival sulcus or periodontal pocket
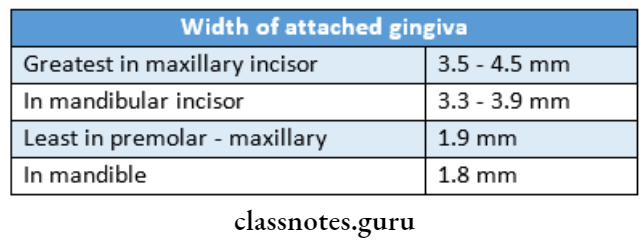
- The width of the attached gingiva increases with age 4 and in supra-erupted teeth
- On the lingual aspect of the mandible, the attached gingiva terminates at the junction of the lingual alveolar mucosa which is continuous with the mucous membrane lining the floor of the mouth
