Mycotic Infections Of Oral Cavity Important Notes
- Actinomycosis
- Causative organisms – A. israelii, A.naeslundh, A.bovis, A.odontolyticus, and A.viscosus
- Actinomycosis Types
- Cervicofacial
- Abdominal
- Pulmonary
- Actinomycosis Clinical features
- Overlying skin
- Dusky, red, or bluish-red
- Appears as a wooden indurated area of fibrosis
- Sinus contains pus which has sulphur granules
- Colonies produce the ray-fungus appearance
- Overlying skin
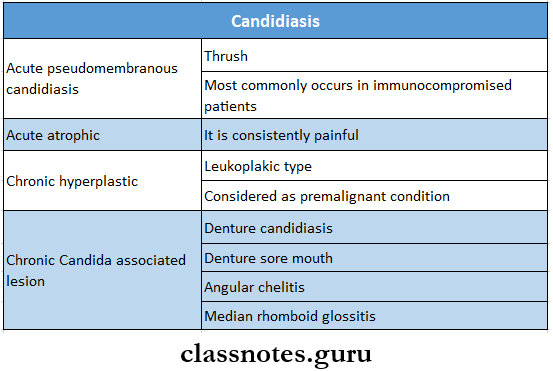
- Candidiasis
- Candidiasis Classification
- Acute
- Acute pseudomembranous candidiasis
- Acute atrophic candidiasis
- Chronic
- Chronic atrophic candidiasis
- Denture stomatitis
- Median rhomboid glossitis
- Angular cheilitis
- Chronic atrophic candidiasis
- ID reaction
- Chronic hyperplastic candidiasis
- Acute
- Chronic mucocutaneous candidiasis
- Familial CMC
- Localized CMC
- Diffused CMC
- Candidiasis endocrinopathy syndrome
- Candidiasis Clinical features
- Candidiasis Classification
Mycotic Infections Of Oral Cavity Long Essays
Question 1. Enumerate fungal Infections of the oral cavity. Write In detail about clinical features and Investigations of oral candidiasis
(or)
Describe the etiology, clinical features, and histopathology of oral candidiasis
Answer:
Fungal Infections Of The Oral Cavity:
- Candidiasis
- Coccidioidomycosis
- Histoplasmosis
- Cryptococcosis
- North American blastomycosis
- Mucormycosis
- Geotrichosis
- Phycomycosis
- Rhinosporidiosis
- Sporotrichosis
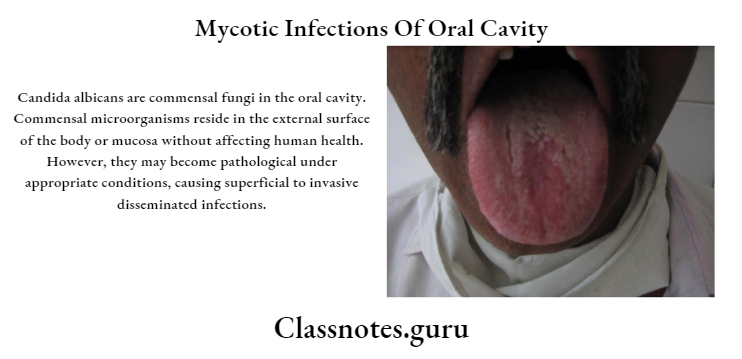
Oral Candidiasis:
- Candidiasis is the most common fungal infection of the oral cavity
Oral Candidiasis Etiology/Causative Organisms:
- Candidiasis is caused by
- Mainly Candida albicans
- Other species- C tropica C is, C.glabrala, C, Krusie, C.pseudotropicaiia
Read And Learn More: Oral Pathology Questions And Answers
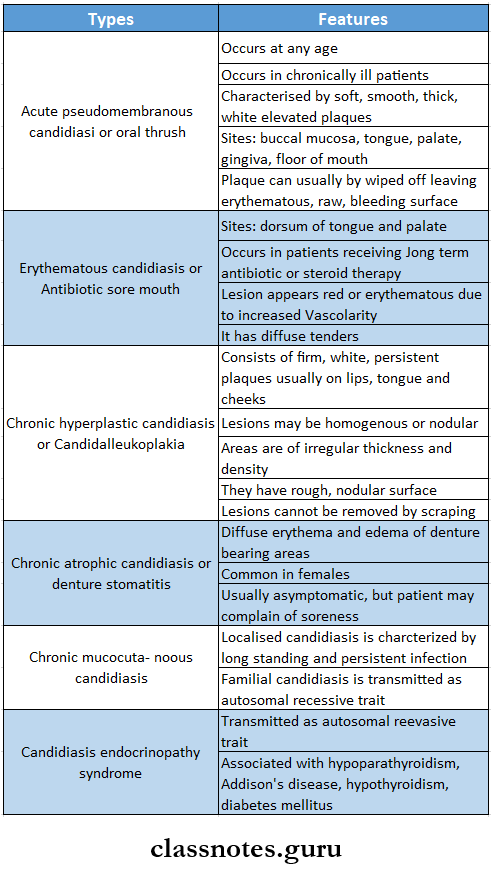
Oral Candidiasis Clinical Features:
- Candidiasis may range from mild superficial mucosal involvement to severe, fatal, disseminated form
Oral Candidiasis Investigations:
- Direct microscopy
- Gram-stained smears and KOH mounts from lesions are used
- They show budding Gram-positive yeast cells
- Culture- sabouraud’s dextrose agar media
- Media is inoculated and incubated at 25-37 degrees C for 24 hours
- Cream-colored smooth pasty colonies appear
- Identification
- Candida albicans can be identified by
- Germ tube test
- Chlamydospores
- Biochemical reactions
- albicans can be identified by the assimilation and fermentation of ssugarSerology
- OrOrganismsre identified by the precipitation test with a carbohydrate extract of group A antigens
Question 2. Write in detail about candidiasis concerning classification, histopathology, and management.
Answer:
Candidiasis Classification
- Acute
- Pseudomembranous candidiasis or oral thrush
- Atrophic
- Chronic
- Atrophic
- Hypertrophic
- Angular cheilitis
- Systemic
- Candidal endocarditis
- Candidal meningitis
- Candidalsepticaemia
- Mucocutaneous
- Localized
- Familial
- Syndrome associated
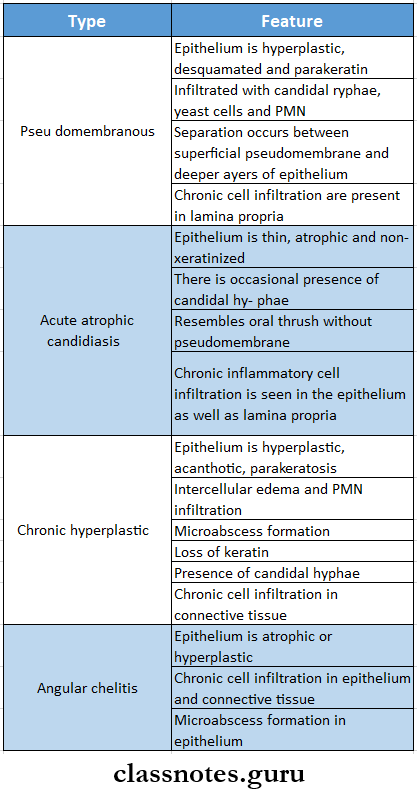
Candidiasis Histopathology
Candidiasis Management
- Removal of etiological factor
- Improvement of oral hygiene
- In conventional – topical and systemic administration of Nystatin
- In immunosuppressed patients – systemic administration of amphotericin B and fluconazole
Mycotic Infections Of Oral Cavity Short Essays
Question 1. Histoplasmosis
Answer:
Histoplasmosis
- Histoplasmosis is a generalized fungal infection caused by Histoplasma capsulatum
Histoplasmosis Clinical Features:
- Fever, malaise
- Headache
- Productive cough
- Hepatomegaly
- Splenomegaly
- Lymphadenopathy
- Anaemia, leukopenia
- Subcutaneous nodules
- Chest pain
- Weight loss
- Granulomatous, verrucous, or necrotic ulcers
Histoplasmosis Oral Manifestations:
- Nodular, ulcerative lesions on the buccal mucosa, gingiva, tongue, palate o, or lips
- Ulcers are covered by a non-specific grey membrane
- Regional lymphadenopathy
- Jaw swellings
- Oral lesions heal with scarring
Histoplasmosis Histopathology:
- Granulomas contain large number of macrophages, lymphocytes, plasma cells, multiple multi-nucleated giant cells
- Liquefaction necrosis and exudation at the margins
- Epithelial hyperplasia
- Microabscess formation
Histoplasmosis Treatment:
- In mild infections- ketoconazole
- In severe cases- amphotericin B
Question 3. Candida Albicans
Answer:
Candida Albicans
- Candida albicans is an ovoid or spherical budding yeast cells
- Size- 3-5 micrometers in diameter
- Candida Albicans is a normal inhabitant of skin, GIT, oral and vaginal cavities
- Candida Albicans causes candidiasis
- Lesions caused by it in include mucocutaneous lesions
- Skin and nail infections
- Systemic candidiasis
- Oral symptoms
Question 4. prPredisposingactors for candidiasis
Answer:
predisposing Factors For Candidiasis
- Diabetes
- Immunodeficiency
- Malignancy
- Prolonged administration of antibiotics
- Patients on immunosuppressive drugs and intravenous catheters
Question 5. Classification of oral candidiasis
Answer:
Primary Oral Candidiasis
- Acute forms
- Pseudomembranous
- Erythematous
- Chronic forms
- Hyperplastic
- Nodular
- Plaque like
- Erythematous
- Pseudomembranous
- Candida-associated lesions
- Denture stomatitis
- Angular cheilitis
- Median rhomboid glossitis
- Keratinized primary lesions superinfected with Candida
- Leukoplakia
- Lichen planus
- Lupus erythematosus
Secondary Oral Candidiasis
- Candidiasis endocrinopathy syndrome
Question 6. Identification of Candida albicans
Answer:
Identification Of Candida Albicans
- Germ tube test
- When incubated in human serum at 37 degrees, C.albicans form germ tubes within 2 hours
- This is called Rethe Ynolds braude phenomenon
- Chlamydospores
- Chlamydospores develop in cornmeal agar at 20 degrees
Question 7. Actinomycosis
Answer:
Actinomycosis
- Actinomycosis is a chronic granulomatous disease
Actinomycosis Causative Organisms:
- Chiefly- Actinomyces Israeli
- Rarely
- Actinomyces naeslundii
- Actinomyces meyeri
- Actinomyces odontolyticum
- Actinomyces viscosus
Actinomycosis Forms:
- Cervicofacial
- Thoracic
- Abdominal
- Pelvic
Actinomycosis Clinical Features:
- Multiple abscess formation
- Tissue destruction
- Fibrosis
- Multiple sinus formation
- Painless indurated swelling
- Gingivitis
- Periodontitis
Question 8. Cervicofacial Actinomycosis
Answer:
Cervicofacial Actinomycosis
- Cervicofacial Actinomycosis is the ommonest form of actinomycosis
Cervicofacial actinomycosis Sites Involved:
- Cheek
- Submaxillary regions
- Route of Infections:
- Tonsils
- Carious tooth
- Periodontal disease
- Trauma following tooth extraction
Cervicofacial Actinomycosis Clinical Features:
- Initially, a firm swelling appears in the lower jaw
- Gradually the mass breaks down
- This leads to abscesses and sinus formation
Cervicofacial actinomycosis Complications:
- Spreading of infection into adjacent soft tissues
- Destruction of bone
Question 9. Rhinosporidiosis
Answer:
Rhinosporidiosis
- Rhinosporidiosis is charoniconic granulomatous disease
Rhinosporidiasis Causative Organism:
- Rhinosporidium seeberi
Rhinosporidiosis Mode of Infection:
- Frequent contact with stagnant water
Rhinosporidiosis Clinical Features:
- Friable polyps
- The site involved nose, mouth, eyes
- Oropharyngeal lesions
- Appear as soft red polypoid growth and spreads to the pharynx and larynx
- Lesions contain mucoid discharge and are vascular
Question 10. Acute atrophic candidiasis
Answer:
Acute atrophic Candidiasis
- Acute atrophic Candidiasis occurs when the pseudomembranous covering of the oral thrush is lost
Acute Atrophic Candidiasis Features
- Site – dorsum of tongue and palate in patients receiving long-term antibiotics or steroid therapy
- Present as generalized red, painful peeling patches over the mucosa
- Causes tenderness, dysphagia, and a burning sensation
Acute Atrophic Candidiasis Histopathology
- The epithelium is thin, atrophic and non-keratinized
- There is occasional presence of candidal hyphae
- Resembles oral thrush without pseudomembrane
- Chronic inflammatory cell infiltration is seen in the epithelium as well as lamina propria
Question 11. Sulfur granules
Answer:
Sulfur Granules
- Sulfur Granules are features of actinomycosis
- In tissues affected by actinomycosis, there is a formation of numerous abscesses
- This abscess drains through discharging sinuses over the in
- The pus contains sulphur granules which contain colonies of actinomycosis
Mycotic Infections Of Oral Cavity Viva Sulfurphur granules in actinomycosis cocontainolonies of organisms of actinomycosis
- Lumpy jaw is a cervicofacial form of actinomycosis
- Chronic diagnosis of candidiasis is confirmed by the proliferation of inflamed pulp tissue
- Oral candidiasis is also known as Moniliasis or oral thrush
- Histoplasmosis is caused by Histoplasma capsulatum
- Candida albicans spherical budding yeast cell
- Cervicofacial is the common form norm of actinomycosis
- GeA germ tube test is used for the didentificationtion of Candida albican
