Intracellular Accumulations Important Notes
1. Endogenous pigments
- It includes lipofuscin, melanin, and certain derivatives of hemoglobin
- Lipofuscin is a yellowish-brown intracellular lipid pigment
- Found in
- Atrophied cells of old age so-called wear and tear pigment
- Myocardial fibres
- Hepatocytes
- Leydig cells of the testes
- Neurons of senile dementia
Intracellular Accumulations Long Essays
Question 1. Mention types of degeneration. Discuss pathogenesis and macroscopic appearance of fatty liver.
Answer:
Degeneration Types:
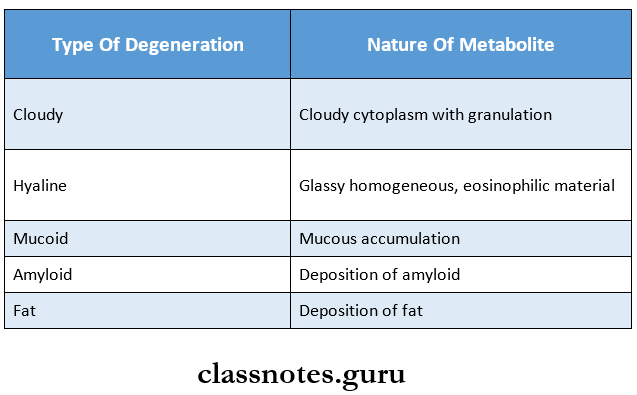
Fatty Liver Pathogenesis:
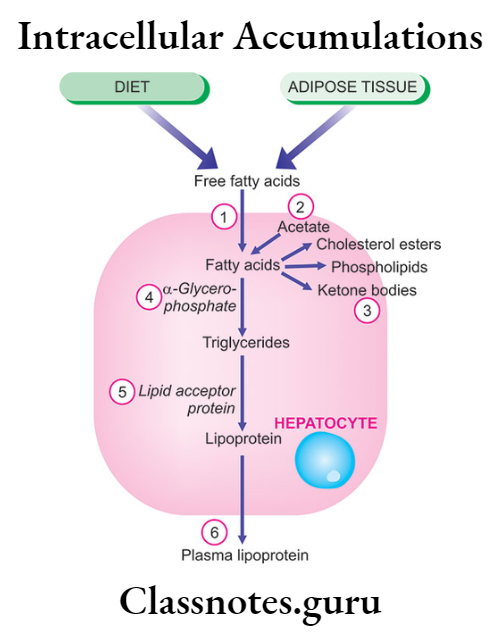
In fatty liver: Intracellular accumulation of triglycerides can occur due to defect at one/ more of the following 6 steps:
- Increased entry of fatty acids into the liver.
- Increased synthesis of fatty acids by the liver.
- Decreased conversion of fatty acids into ketone bodies resulting in increased esterification of fatty acids to triglycerides.
- Increased a-glycerophosphate causes increased esterification of fatty acids to triglycerides.
- Decreased synthesis of lipid acceptor protein resulting in decreased formation of lipoprotein from triglycerides.
- Block in the excretion of lipoprotein from the liver into plasma.
Read And Learn More: Pathology Question And Answers
Macroscopic Appearance of Fatty Liver:
1. Gross appearance
- Size- liver is enlarged
- Color-yellow
- Capsule- tense and glistening capsule
- Margins are rounded
2. Cut surface
- It bulges slightly
- Color varies from pale yellow to yellow
- The surface is greasy to the touch
Question 2. Define and classify degeneration. Discuss etiopathogenesis and pathology of fatty liver,
(or)
Mention types of degeneration. Discuss patho¬genesis and microscopic appearance of fatty liver
Answer:
Degeneration Definition:
- Degeneration is a process by which a tissue deteriorates, loses its functional activity, and may become con¬verted into or replaced by other kinds of tissue.
Fatty Liver:
- Fatty liver or steatosis is the intracellular accumulation of neutral fat within parenchymal cells
- It is common in the liver as it plays a central role in fat metabolism
Microscopic Appearance:
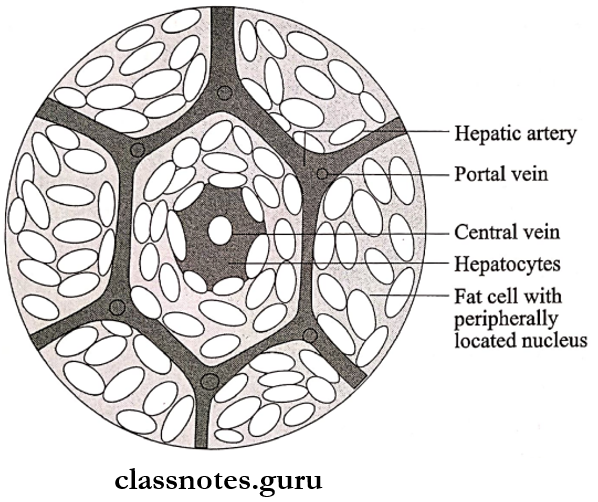
- The fatty liver shows numerous lipid vacuoles in the cytoplasm of hepatocytes
- It is seen as a clear area that may vary from minute droplets to an extension of the entire cytoplasm
1. Initially
- Vacuoles are small
- They are present around the nucleus
- Centrilobular hepatocytes are affected
2. Later
- Vacuoles enlarge
- They push the nucleus to the periphery of the cells
- Fat accumulation involves the entire lobule
- Occasionally adjacent cells containing fat may rupture producing fatty cysts
- Rarely, lymphogranuloma may appear consisting of a collection of microphones, lymphocytes, and multi-nucleate giant cells
Intracellular Accumulations Short Essays
Question 1. What is fatty liver? What are its causes?
Answer:
- Fatty change/steatosis is the intra-cellular accumula¬tion of neutral fat within parenchymal cells.
- It is especially common is the liver as it plays a central role in fat metabolism,
- It may occur in other non-fatty tissues like the heart, skeletal muscles, kidneys, and other organs.
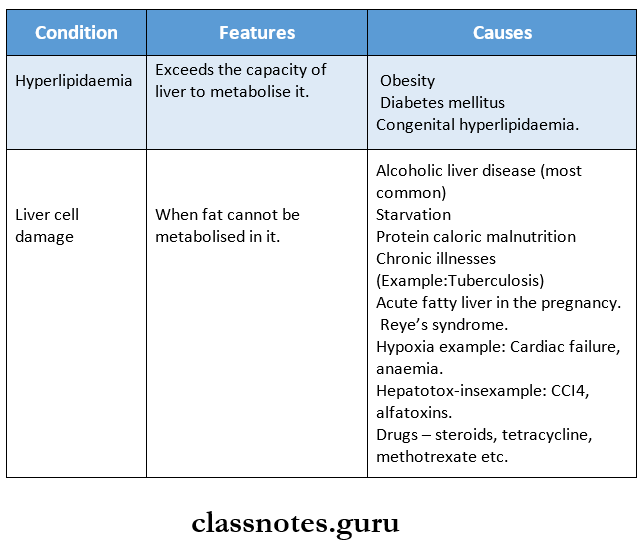
Fatty Liver Types:
- Fatty change may be
- Mild and reversible
- Severe and irreversible resulting in cell death.
Etiology: Fatty change in the liver results from.
Question 2. Wear and tear pigment
Answer:
- Lipofuscin is known as wear and tear pigment.
- Lipofuscin/lipochrome is a yellowish-brown intra-cellular lipid pigment.
- It is a hemoprotein-derived pigment
Site of Appearance:
- In atrophied cells of old age and Lence known as wear and tear pigment.
- It is seen in myocardial fibers, hepatocytes, Leydig cells of the testis, and neurons in senile dementia.
Significance:
- Lipofuscin represents the collection of indigestible material in the lysosomes after intra-cellular lipid peroxi¬dation and is therefore an example of residual bodies.
Microscopy:
- By light microscopy, the pigment is coarse, golden brown granular, and often.’ accumulates in the central part of the cells around the nuclei.
- In heart muscle, change is associated with wasting of the muscle and is commonly refered to as brown atrophy.
- By electron microscopy, lipofuscin appears. J as integrally- ribosomal electron-dense granules in perinuclear location. Granules are composed of did-protein complexes.
Question 3. Hemosiderosis
Answer:
Hemosiderosis Definition:
- Excessive storage of hemosiderin is called he-mosiderosis
Hemosiderosis Causes:
- Increased breakdown of red cells
- Systemic overload of iron due to
- Primary causes
- Idiopathic
- Hereditary
- Secondary causes
- Thalassaemia
- Sideroblastic anemia
- Alcoholic cirrhosis
- Primary causes
Hemosiderosis Effects:
1. Localized hemosiderosis
- Black eye occurs due to bilirubin and biliverdin
- Brown induration in the lungs occurs due to small hemorrhages
2. Generalized hemosiderosis
- Parenchymatous deposition of hemosiderin in the liver, kidney, pancreas
- Reticuloendothelial deposition in the liver, spleen, and bone marrow
Intracellular Accumulations Short Question And Answers
Question 1. Melanin pigment
Answer:
- Melanin is an endogenous pigment
- Melanin is a brown-black, non-hemoglobin-derived pigment normally present in the hair, skin, choroid of the eye, meninges, and adrenal medulla.
Melanin pigment Synthesis:
- It is synthesized in the melanocytes and dendritic cells
Melanin pigment Storage:
- Stored in the form of cytoplasmic granules in the phagocytic cells called as melanophores.
Melanin pigment Disorders:
Various disorders of melanin pigmentation cause gen¬eralised and localized hyperpigmentation and hypopigmentation.
1. Generalised hyperpigmentation is seen during.
- Addison’s disease
- Chloasma
- Chronic arsenal poisoning.
2. Focal hyperpigmentation.
- Cafe-au-lait spots in Albright’s syndrome.
- Peutz-Jeghers syndrome.
- Melanosis coli.
- Melanotic tumors
- Dermatopathiclymphadentis.
3. Generalised hypopigmentation.
- Albinism
4. Localised hypopigmentation.
- Leukodema
- Vitiligo
- Acquire focal hypopigmentation.
Question 2. Exogenous pigment
Answer:
Exogenous pigments are the pigments introduced into the body from outside such as by inhalation, ingestion, or inoculation.
Inhaled pigments:
- The most commonly inhaled substances are carbon/coal, dust, silica/stone dust, iron oxide, asbestos, and various other organic substances.
- These substances may cause occupational lung disease called pneumoconiosis.
- Extensive deposition of particulate material over many years provides low-grade inflammation, fibrosis, and impaired respiratory function.
Ingested pigments:
- Chronic ingestion of certain metals may produce pigmentation. E^/Argyria, chronic lead poisoning, melanosis coli.
Injected pigments:
- Examples of injected pigments are prolonged use of ointments containing mercury, dirt left accidentally in a wound, and tattooing by pricking the skin with dyes.
- In it pigment is taken by the macrophages and lies permanently in the connective tissue
Question 3. Fatty degeneration/ fatty change
Answer:
- Fatty degeneration or fatty change is the intracellular accumulation of neutral fat within parenchymal cells
- It occurs in the cytosol and represents an absolute increase in the intracellular lipids
Fatty change Types:
- Depending upon the cause and amount of accumulation, fatty change can be
- Mild and reversible
- Severe and irreversible- Causing cell death
Question 4. Causes of Ketonuria.
Answer:
- Metabolic abnormalities – diabetes, renal glycosuria
- Dietary conditions – starvation, fasting, prolonged vomiting, anorexia
- Hyperthyroidism, fever, pregnancy, lactation
Question 5. Ketone bodies.
Answer:
- Ketone bodies are water-soluble molecules – acetone, acetoacetate, and beta-hydroxybutyrate
- They are produced by the liver from fatty acids during low food intake, starvation, prolonged intense exercise, alcoholism or untreated diabetes mellitus
- Ketone bodies are readily picked up by the extrahepatic tissues and converted into acetyl CoA which enters the citric acid cycle
- It is oxidized in mitochondria for energy
