Question 1. Oral manifestations of diphtheria
Answer:
Oral Manifestations Of Diphtheria
- Diphtheria is an infectious disease caused by Corynebacterium Diphtheriae
- Oral Manifestations Of Diphtheria is characterized by local exudative inflammation of the upper respiratory tract and usually with the formation of pseudomembrane at the level of the nasopharynx
- Oral manifestations
- Sore throat
- Formation of thick, fibrinous, greyish-green pseudomembrane on tonsils, larynx, pharynx
- Exudation in tonsillar area
- Hoarseness of voice
- Paralysis of the soft palate
- Dysphagia
- Dysphonia
- Cervical Lymphadenopathy
- Formation of thick, fibrinous, greyish-green pseudomembrane on tonsils, larynx, pharynx
- Sore throat
Infectious Diseases Short Notes
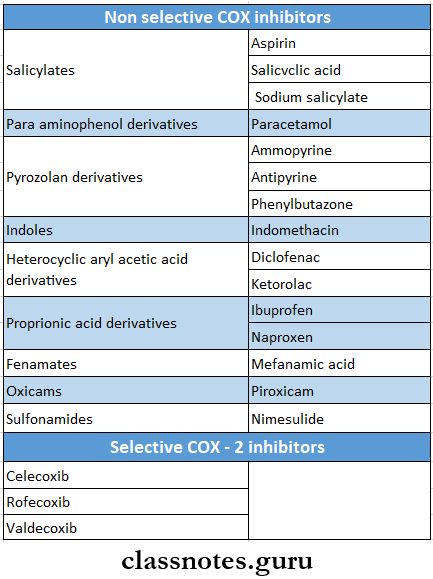
Question 2. NSAIDs
Answer:
NSAIDs Classification
Question 3. Oral manifestations of AIDS
Answer:
Oral Manifestations Of AIDS
- Bacterial infections
- Tuberculosis
- M. avium complex
- Salmonellosis
- Viral infection
- Herpes simplex
- Varicella zoster
- Epstein Barr virus
- Mycotic infections
- Pneumocystis pneumonia
- Candidiasis
- Aspergillosis
- Cryptococcosis
- Parasitic infection
- Toxoplasmosis
- Cryptosporidiosis
- Malignancies
- Kaposi’s sarcoma
- B cell lymphoma
Read And Learn More: General Medicine Question and Answers
Question 4. Human immunodeficiency virus (HIV)- post-exposure prophylaxis
Answer:
Human Immunodeficiency Virus (HIV)- Post-Exposure Prophylaxis
- Following exposure, postexposure prophylaxis may be required depending upon the category of exposure and HIV status of the exposure source
- Drugs used are:
- Zidovudine 300 mg BD
- Lamivudine 150 mg BD
- Protease inhibitors
- Lopinavir 400 mg BD or 800 md OD
- Ritonovir 100 mg BD or 200 mg OD
- Drugs are started within the first 72 hours
- It should be continued for 4 weeks
- The injured site on the wound should be thoroughly washed with soap and water
- Antiseptics are also used
Short essays on communicable diseases
Question 5. Gonorrhoea
Answer:
Gonorrhoea Definition:
- Gonorrhoea is a communicable sexually transmitted disease of humans
Etiology:
- Etiology is caused by Neisseria gonorrhoea
Gonorrhoea Clinical Features:
- In males
- Dysuria
- Increased frequency of micturition
- Purulent discharge per urethra
- Oedema of the penis
- Erythema of the urethral meatus with purulent discharge
- In females
- Dysuria
- Vaginal discharge
- Abnormal menstrual bleeding
- Rectal discomfort
- In homosexuals
- Asymptomatic
- In children
- Conjunctivae
- Involvement of the pharynx or the respiratory tract
Gonorrhoea Complications:
- Acute epididymitis
- Prostatitis
- Periurethral abscess or fistula
- Salpingitis
- Bartholin’s abscess
- Premature birth
- Arthritis
- Bacteraemia
- Perihepatitis
Gonorrhoea Treatment:
- For uncomplicated gonorrhea
- 2.4 g of procaine penicillin IM + 1 g of oral probenecid or
- Oral amoxicillin 2-3 g + Oral probenecid 1 g or
- Cotrimoxazole (400+80 mg) 8 tablets orally
- In penicillin-resistant gonorrhea
- Ciprofloxacin-250-500 mg orally single dose or
- Cefotaxime- 0.5-1 g IM as single dose or
- Cefixime- 400 mg orally as a single dose or
- Ceftriaxone-250 mg IM as single dose
- In gonorrhea with complications
- Aqueous crystalline penicillin G-10 million units 4 daily for 5 days
- Ciprofloxacin 500 mg twice daily for 5 days
- Ceftriaxone 1 g 4 daily for 5 days
Question 6. Chickenpox
Answer:
Chickenpox
- Chickenpox is caused by Varicella zoster virus
- Chickenpox rarely occurs a second time
- The virus enters the mucosa of the upper respiratory tract and spreads by droplets from the throat
Chickenpox Clinical Features:
- Chickenpox involves young children and adults
- The incubation period is 14-21 days
- Malaise
- Low-grade fever followed by a rash
- Rash is macula papular
- Heals by scabs formation
Chickenpox Sites Involved:
- Skin lesions- over trunk and face then spread to peripheral parts of the body
- Mucosal lesions- affects the mucosa of the pharynx and vagina
Chickenpox Complications:
- Superinfection of skin due to frequent scratching
- Encephalitis
- Cerebellar ataxia
- Myocarditis
- Osteomyelitis
- Septic arthritis
- Septicaemia
- Hepatitis
- Pneumonia
Infectious Diseases Short Answer Questions
Question 7. Herpes simplex
Answer:
Herpes simplex
- Herpes simplex is a DNA virus o It belongs to the herpesviridae family.
- Man is the only natural host.
- Herpes simplex virus has two types as follows.
- Herpes simplex type 1 – is usually associated with oral and ocular lesions.
- Herpes simplex type 2 – is usually associated with genital infections.
- Lesions caused by herpes simplex depend on the site of infection, age, and immune status of the individual as follows:
- Cutaneous infections: These include:
- Fever
- Blisters on the cheeks, chins around the mouth, (or) on the forehand
- Napkin rash on the buttocks of children, – Herpetic with low in medical professionals.
- Eczema herpeticum:
- The generalized herpetic eruption is seen in children suffering from eczema.
- Mucosal lesions:
- Acute gingivostomatitis
- Recurrent herpes labialis.
- Ophthalmic lesions:
- Keratoconjunctivitis
- Follicular conjunctivitis.
- Visceral lesions:
- Nervous system:
- HSV meningitis,
- Sacral autonomic dysfunction.
- Genital lesions:
- Infection of cervix, vagina, vulva (females)
- Congenital lesions:
- Subclinical or localized infection of skin mouth or eyes.
- Besides primary infections, herpes viruses may present as latent infection, reactivation, and recrudescence.
Question 8. Herpes labialis
Answer:
Herpes Labialis
- Herpes labialis occurs in patients with no prior infection with Herpes Simplex Virus-1
Herpes Labialis Clinical Features:
- Age- children and young adults
- Incubation period-5-7 days
- Prodromal generalized symptoms
- Fever
- Malaise
- Headache
- Nausea, vomiting
- Painful mouth
- Sore throat
- Irritability
- Excessive drooling of saliva
- Lack of tactile sensation
- Cervical lymphadenopathy
- Later symptoms
- Numerous vesicle formations over keratinized mucosa
- Vesicles are thin-walled
- They contain clear fluid
- They rupture leaving multiple, small, punctuate shallow painful ulcers of 2-6 mm
- Ulcers are surrounded by a red ring of inflammation
- Ulcers may become secondarily infected
- Healing starts in about 3 days and is completed within 7-14 days
Herpes Labialis Treatment:
- To prevent secondary infection- antibiotics are used
- To control fever- Antipyretics are given
Question 9. Mumps
Answer:
Mumps
- Mumps is an acute viral infectious disease characterized by unilateral (or) bilateral nonsuppurative enlargement of the salivary glands usually the parotid gland.
- Submandibular and sublingual glands are occasionally involved.
- Usually, children are affected. May also occur in adults.
- Also known as epidemic parotitis
Mumps Causative Organism:
- Organisms involved in paramyxovirus.
Mumps Route Of Infection:
- Infection is acquired by inhalation (or) direct contact or through the conjunctiva.
- The incubation period is 12 – 18 days.
Mumps Clinical Features:
- Unilateral (or) bilateral swelling of parotid glands.
- Fever, malaise
- Local pain and tender
- Involvement of extra parotid sites can cause more serious problems as follows.
- CNS involvement may lead to
- Meningitis,
- Meningoencephalitis
- Orchitis
- CNS involvement may lead to
Mumps Complications:
- Orchitis
- Oophoritis
- Arthritis
- Nephritis
- Pancreatitis
- Thyroiditis and myocarditis
Mumps Laboratory Diagnosis:
- Isolation of viruses from CSF, saline (or) urine.
- Serological tests with paired serum samples tested for the rise in the titer of antibodies by complement fixation test, ELISA, and haemagglutination tests.
- Serum amylase levare els elevated in both parotitis and acute pancreatitis.
Mumps Treatment:
- Treatment is conservative maintaining hydration. Prevention is using MMR vaccine
microbiology short notes on infections
Question 10. Diphtheria
Answer:
Diphtheria Clinical Features:
- It is insidious at the onset
- Moderate grade fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on the tonsils
- Swollen neck- Bull neck
- Tender lymphadenopathy
- Nasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Acute circulatory failure
- Myocarditis
- Nerve palsies
- Dysphagia
- Dysphonia
- Paraesthesia in the limbs
Diphtheria Management:
1. Antitoxin diphtheric serum (ADS)
- The dose varies from 20,000 to 1,00,000 units depending on {ho duration and severity of the disease
- In mild cases, a lesser dose may be used
2. Antibiotics
- Penicillin G-o.00,000 units every 12 hourly intravenously or
- Amoxycillin 500 mg S hourly for 7-10 days
- Patient allergic to penicillin
- Erythromycin- 500 mg 6 hourly or
- Azithromycin 500 mg daily or
- Riftamoicin 600 mg daily
3. Tradieostomy
Question 11. Three malarial parasites
Answer:
Three Malarial Parasites
- Malaria is a disease caused by four plasmodium speeds which are as follows:
- P. vivax
- P. Falciparum
- P. Malaria
- P. Ovale.
Question 12. Widal test
Answer:
Widal Test
- Widal Test is an agglutination test for detection of agglutinin H and O in patients with enteric fever
Widal test Procedure:
- Mix equal volumes of serial dilutions of the serum and H and O antigens
- Incubate in a water bath at 37 degrees C for 4 hours
- Read after overnight refrigeration at 4 degrees C
Widal test Result:
- A Titre upto 160 indicates enteric fever
Question 13. Chancre
Answer:
Chancre
- Chancre is a typical lesion of primary syphilis that appears on genitals/at extragenital sites in 2-4 weeks after exposure to infection.
- Initially, the lesion is a painless papule that ulcerates in the center so that the fully developed chancre is an indurated lesion with central ulceration accompanied by regional lymphadenitis.
- Chancre heals without scarring, even in the absence of treatment.
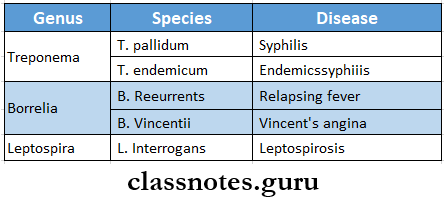
Question 14. Two spirochaetal diseases
Answer:
Two spirochaetal diseases
Short note on infectious diseases
Question 15. Oral manifestations of syphilis
Answer:
Oral manifestations of syphilis
- Syphilis is a sexually transmitted disease caused by spirochaetes, treponema pallidum.
- Syphilis is divided into 3 stages depending upon the period after which the lesions appear and the type of lesions.
- They are primary, secondary, and tertiary.
- Oral lesions occur in secondary syphilis known as mucous patches, on the tongue, gingiva, etc., or as a split papule on the lips, which are highly infectious.
- Tertiary/late syphilis/gumma is a granuloma with central necrosis, noninfectious, and is most common on the tongue and palate.
- Palatal perforation by ulcer after vigorous antibiotic use is known as the Herxheimer reaction.
- In congenital/prenatal syphilis, the most constant finding is relatively short roots of mandibular permanent 1st molars, short maxilla, Hutchinson triad (teeth, eye/ear involved), hypoplasia of incisors and molars i.e., notched incisors and mulberry molars.
- Treatment: Penicillin is the drug of choice.
Question 16. Congenital syphilis
Answer:
Congenital syphilis Major features are:
- Hutchinson’s triad includes.
- Hutchinson’s teeth-small, widely spaced, peg-shaped permanent teeth.
- Notched central incisors
- Intestinal keratitis with blindness and deafness from Stir cranial nerve injury.
- Saddle shaped nose
- Bony lesions like epiphysis and periostitis
- Mucocutaneous lesions of acquired secondary syphilis
- Diffuse fibrosis in the liver.
Question 17. VDRL test
Answer:
VDRL test
- VDRL test is an abbreviated form of the Venereal Disease Research Laboratory test
- VDRL test is the most widely used test for syphilis
- VDRL test is a simple arid rapid test
- VDRL test is a slide flocculation test
VDRL test Procedure:
- Cardiolipin antigen is freshly prepared
- A drop of this is added to a drop of inactivated patient’s serum on a slide
- Mix it by shaking
VDRL test Result:
- If floccules appear it indicates a positive test
Question 18. Prednisolone
Answer:
Prednisolone
- Prednisolone has potent glucocorticoid and mild mineralocorticoid activity
- Prednisolone is the most commonly used glucocorticoid
Prednisolone Uses:
- Replacement therapy
- Rheumatoid arthritis
- Osteoarthritis
- Acute gout
- Allergic diseases
- Bronchial asthma
- Collagen diseases
- Eye diseases
- Renal diseases
- Skin diseases
- GIT diseases
- Liver diseases
- Malignancies
- Organ transplantation
Prednisolone Adverse Effects:
- HPA axis suppression
- Cushing’s syndrome
- Hyperglycemia
- Susceptibility to infection is increased
- Osteoporosis
- Avascular necrosis
- Peptic ulceration
- Mental disturbances
- Cataract and glaucoma
- Delayed wound healing
Question 19. Metronidazole
Answer:
Metronidazole
- Metronidazole is a nitroimidazole
Metronidazole Mechanism of Action:
- Metronidazole is prodrug
- Susceptible micro-organisms reduce the nitro group of metronidazole by nitroreductase
- Convert it into a cytotoxic derivative
- It binds to DNA
- Inhibits protein synthesis
Metronidazole Uses:
- Anaerobic infection
- Amoebiasis
- Trichomonas vaginitis
- Giardiasis
- H.pylori infection
- Pseudomembranous colitis
- Draetmcwlosis
- Topical application
Metronidazole Adverse Reactions:
- Nausea, anorexia, abdominal pain, metallic taste in mouth
- Headache, dizziness
- Stomatitis, glossitis
- Furry tongue
- Insomnia, ataxia, vertigo
- Peripheral neuropathy
- Pruritis, urticaria, skin rashes
Question 20. Aminoglycosides
Answer:
Aminoglycosides
- Aminoglycosides are antibiotics with amino sugars in glycosidic linkages
Aminoglycosides Mechanism of Action:
- Penetrate bacterial cell membrane
- Bind to 30S ribosomes
- Inhibits bacterial protein synthesis
Aminoglycosides Uses:
- Tuberculosis
- Subacute bacterial endocarditis
- Plaque
- Tularemia
- Brucellosis
Aminoglycosides Adverse Effects:
- Ototoxicity
- Nephrotoxicity
- Neuromuscular blockade
Aminoglycosides Examples:
- Streptomycin
- Kanamycin
- Tobramycin
- Neomycin
- Gentamicin
- Netilmicin
Short questions in infectious diseases
Question 21. Chloramphenicol
Answer:
Chloramphenicol
- Chloramphenicol Is a broad spectrum and loll.
Chloramphenicol Mechanism of Action:
- It binds to 50S ribosome
- Inhibits transpeptidation reaction
- Inhibits protein synthesis
Chloramphenicol Uses:
- Typhoid lever
- Bacterial meningitis
- Anaerobic infections
- Rickettsial infection
- Kyo infections
Chloramphenicol Adverse Reactions:
- Gastrointestinal disturbances- nausea, vomiting, diarrhea
- Bone marrow depression
- Gray baby syndrome
- Hypersensitivity reactions
- Superinfection
Question 22. Malaria
Answer:
Malaria is a disease caused by four plasmodium species which are as follows:
- P. vivax
- P. Falciparum
- Malaria
- P. Ovale.
Malaria Life Cycle:
The malarial parasites pass their life cycle in two hosts.
- Man intermediate host [a sexual development
- Femalanopheles mosquito delinitive host [sexual development].
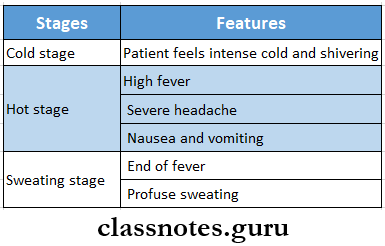
Malaria Clinical Features:
- Intermittent fever which is named malaria is caused by plasmodium
- It consists of
- Febrile paroxysm
- It comprises of three stages
- Anaemia
- Microcytic or normocytic hypochromic anemia develops
- Splenomegaly.
- The spleen becomes enlarged and palpable
- Black water fever and pernicious malaria are the most commonly seen complications in falciparum malaria.
- Febrile paroxysm
infectious disease short essay for mbbs
Question 23. Ludwig’s angina
Answer:
Ludwig’s angina
- Ludwig’s angina was described by Wilhelm Fredrich Von Ludwig in 1836
- Ludwig’s angina is rapidly spreading cellulitis involving simultaneously all three spaces i.e. Submandibular, sublingual, and submental spaces
Etiology:
- Odontogenic infection
- Traumatic injuries
- Infective condition
- Pathologic conditions
Ludwig’s angina Clinical Features:
- Generalised symptoms
- Dehydration
- Fever
- Dysphagia
- Dyspnoea
- Hoarseness of voice
- Stridor
- Extraoral features
- Brawny hard swelling
- Erythematous skin
- Local rise in temperature
- Drooling of saliva
- Respiratory distress
- Intraoral features
- Trismus
- Raised floor of mouth
- Airway obstruction
- Increased salivation
Ludwig’s angina Management:
- Airway maintenance
- Removal of the causative factor
- Administration of 4 fluids
- Antibiotics
- Penicillin G-2-4 million units TV 4-6 hourly
- Gentamycin-80 mg IM BD
- Metronidazole-400 mg 8 hourly
- Erythromycin-600 mg 6-8 hourly
- Amoxicillin-500 mg 6-8 hourly orally
- Surgical management
