Oral Medicine Infections Important Notes
1. Burning Mouth Syndrome
- Shows clinically healthy oral mucosa
- A burning sensation of oral mucosa occurs
- Pain starts in the morning and aggravates during the day
Oral Medicine Infections Long Essays
Question 1. Classify ulcers of the oral cavity. Describe the etiology, clinical features, and management of recurrent aphthous stomatitis.
Answer:
Ulcers Of Oral Cavity Classification:
1. Ulcers Of Oral Cavity Classification Acute Multiple
- Herpes virus infection
- Primary herpes simplex virus infection
- Coxsackie virus infection
- Varicella-zoster virus infection
- Erythema multiform
2. Ulcers Of Oral Cavity Classification Recurrent Oral Ulcers
- Recurrent aphthous stomatitis
- Behcet’s syndrome
3. Ulcers Of Oral Cavity Classification Chronic Multiple Ulcers
- Pemphigus
- Subeplthellal Bullous dermatoses
4. Ulcers Of Oral Cavity Classification Single Ulcers
- Histoplasmosis
- Blastomycosis
- Mucormycosis
- It is a common disease characterized by the development of painful, recurrent, solitary ulceration of the oral mucosa
Read And Learn More: Oral Medicine Question and Answers
Ulcers Of Oral Cavity Classification Etiology:
- Immunological abnormalities:
- Due to T cell-mediated immunological abnormality
- Genetic predisposition
- Increased susceptibility to PAS
- Microbial organism
- Form L form of □hemolytic streptococci
- Systemic factors
- Nutritional deficiency
- Cyclic neutropenia
Ulcers Of Oral Cavity Classification:
- Minor Aphthae: the ulcers are less than 1 cm in diameter
- Major Aphthae: they are over 1 cm in diameter
- Herpetiform Ulcers: they are small ulcers throughout the mucosa
Ulcers Of Oral Cavity Clinical Features:
- Age and sex: common in women in the second and third decade of life
- Site: it occurs most commonly on buccal and lingual mucosa, tongue, soft palate, pharynx, and gingiva
- Prodromal symptoms:
- It begins with burning, itching, or stinging for 24-48 hours
- Next ulcer appears
- The ulcer gradually enlarges over the next 48-72 hours
- Later symptoms
- The lesion is typically painful
- It interferes with eating for several days
- It begins as a single or multiple superficial erosions covered by the gray membrane is surrounded by localized areas of erythema
- Lesions are round, symmetrical, and shallow
- Multiple lesions are present
- Minor aphthae:
- Size: 0.3-1 cm
- They heal without scar formation within 10-14 days
- Major aphthae
- Size: up to 5 cm in diameter
- They interfere with speech and eating
- The large portion may be covered with deep painful ulcers
- The lesions heal slowly and leave a scar
- Due to this, there is decreased mobility of the uvula and tongue
- Herpetiform ulcers
- Multiple small shallow ulcers often up to 100 in number
- It begins as small pinhead-size erosions that gradually enlarge in size
- Lesions are more painful
- It is present continuously for one to three years
- Patients get relief immediately with 2% tetracycline mouthwash
Ulcers Of Oral Cavity Classification Differential Diagnosis:
- BMMP and pemphigus: absence of vesicles
- Bedner’s aphthae: there is no aphthae
- Erythema multiforme: aphthae ulcers are uniform in distribution
Ulcers Of Oral Cavity Classification Management:
- Topical corticosteroid
- Triamcinolone acetonide: 3-4 times in a day
- Anesthetic cream
- Orobase should be given
- Tetracycline mouthwash:
- 250 mg/ml use four times daily for 5-7 days
- Nutritional supplements:
- Replacement therapy with vitamin B12, ferritin, folate, and iron
- Maintenance of oral hygiene
- Chlorhexidine mouthwash is given
Oral Medicine Infections Short Essays
Question 1. Stomatitis medicamentosa
Answer:
Stomatitis Medicamentosa
Stomatitis Medicamentosa is an allergic reaction associated with systemic drug intake.
Stomatitis Medicamentosa Etiology:
- Oral changes found with cutaneous reaction to drugs
- Mucosal alterations may result from the following:
- Myelosuppression
- Direct cytotoxic effect
- Xerostornic effects
- Alterations of oral microbial flora
Stomatitis Medicamentosa Clinical Features:
- Painful, erythematous, erosive, or ulcerative lesions
- Nonkeratinized locations are often affected initially
- Fixed forms of drug-associated eruptions are relatively uncommon intraorally
- The pseudomembranous necrotic surface may be noted
Stomatitis Medicamentosa Differential Diagnosis:
- Chemical or thermal burn
- Erosive lichen planus
- Pemphigus Vulgaris
- Mucous membrane (cicatricial) pemphigoid
- Erythema multiforme
- Acute herpetic gingivostomatitis
- Candidiasis
Stomatitis Medicamentosa Treatment:
- Identification and withdrawal of offending drug
- Symptomatic management including topical preparations
- Systemic corticosteroids if the mucosal reaction is not related to antineoplastic treatment
Question 2. Burning mouth syndrome.
Answer:
Burning Mouth Syndrome
Burning sensation in the structures in contact with the dentures without any visible change in the mucosa
Burning Mouth Syndrome Features:
- Pain in the morning
- Dry mouth
- Persistent altered taste
- Generalized symptoms
Burning Mouth Syndrome Etiology:
- Irritation by ill-fitting dentures
- Constant masticatory activity
- Excessive friction on the mucosa
- Candidal infection
- Nutritional deficiency
- Xerostomia
- Medication
Burning Mouth Syndrome Management:
- Counseling
- Repair of ill-fitted dentures
Question 3. Allergic stomatitis.
Answer:
Allergic Stomatitis
Allergic Stomatitis occurs due to drug allergy
Allergic Stomatitis Clinical Features:
- Fever
- Arthralgia
- Inflammation
- Ulceration
- Vesicle formation
- Lymph node enlargement
- Erythematous skin
Allergic Stomatitis Oral Manifestations:
- Xerostomia
- Taste alteration
- Eating difficulty
- Vesicle bullae found on the mucosa
- The lesion has a diffuse distribution
- There may he ulceration and necrosis of the gingiva
- Severe periodontal problems may occur
- There may be erosion of teeth
- Bathing of teeth with corrosive substances can spread to the pharynx.
Allergic Stomatitis Differential Diagnosis:
- Recurrent herpes simplex infection – it occurs in groups,
- ANUG-punched out ulceration
- Erythema multiforme- skin lesions are present
Allergic Stomatitis Management:
- Discontinuation of the drug: stop the allergic drug.
- Use an alternative for it.
- Antihistaminic drug: to relieve the acute signs.
- Topical corticosteroid: to resolve localized reaction.
- Adrenaline
Question 4. Treatment of aphthous stomatitis.
Answer:
Treatment Of Aphthous Stomatitis
- Topical corticosteroid
- Triamcinolone acetonide: 3-4 times in a day
- Anesthetic cream
- Orobase should be given
- Tetracycline mouthwash:
- 250 mg/ml use four times daily for 5-7 days
- Nutritional supplements:
- Replacement therapy with vitamin B12, ferritin, folate, and iron
- Maintenance of oral hygiene
- Chlorhexidine mouthwash is given
Oral Medicine Infections Short Answers
Question 1. Major aphthous ulcers.
Answer:
Major Aphthae:
- Size: up to 5 cm in diameter
- They interfere with speech and eating
- The large portion may be covered with deep painful ulcers
- The lesions heal slowly and leave a scar
- Due to this there is decreased mobility of the uvula and tongue
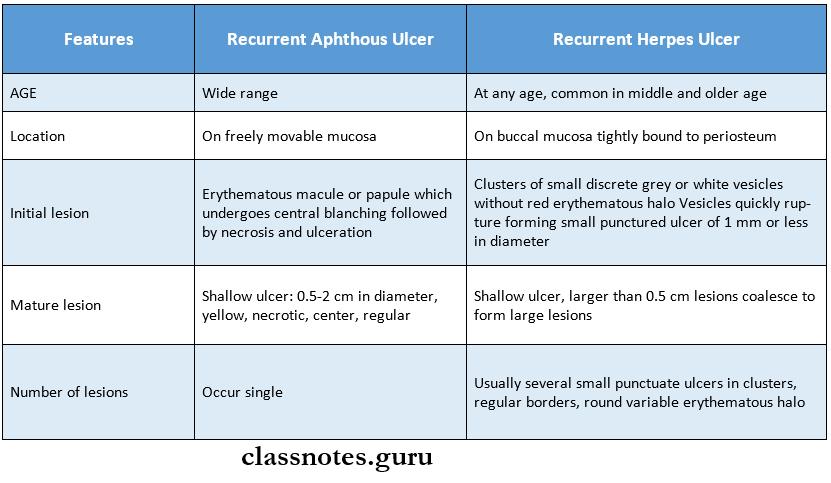
Question 2. Four differences between recurrent aphthous and recurrent herpes ulcers?
Answer:
Four Differences Between Recurrent Aphthous And Recurrent Herpes Ulcers
Oral Medicine Infections Viva Voce
- Chronic osteomyelitis shows a moth-eaten appearance
