Viral Infections Important Notes
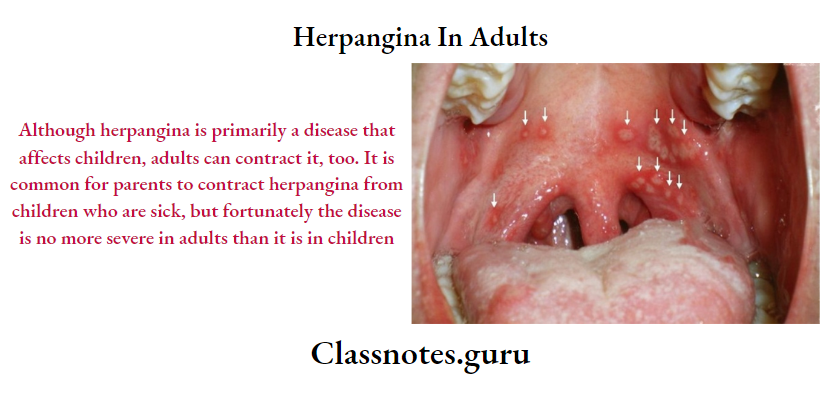
1. Herpangina
- Caused by coxsackie virus
- The prodromal phase consists of fever, chills, anorexia, sore throat, and dysphagia
- Oral lesions start as punctuate macules and quickly evolve into papules and vesicles on the posterior pharynx, tonsils, faucial pillars, and soft palate
2. Herpes Zoster
Common sites involved are the areas innervated by spinal cord segments D3 to L2 and the ophthalmic branch of the trigeminal nerve
3. Measles
- It is an acute, contagious, hepatotropic viral infection
- Characterized by fever, malaise, Koplik’s spots, cough, maculopapular rash
- Koplik spots are prodromal and disappear after the onset of the rash
- They usually occur on the buccal mucosa as small, irregular bluish-white flecks surrounded by a red margin
- Histologically it shows multinucleated giant cells
Viral Infections Long Essays
Question 1. Define vesicle. Write pathogenesis, clinical features, investigations, and management of primary herpetic infection.
Answer:
Vesicle:
Vesicles are elevated blisters containing clear fluid that are under 1 cm in diameter
Read And Learn More: Oral Medicine Question and Answers
Primary Herpetic Infection
- Pathogenesis: Herpes simplex virus infects skin and neurons of the dorsal root ganglia
Primary Herpetic Infection Clinical Features:
Primary Herpetic Infection Oral Manifestations:
- Site involved
- Gingiva
- Hard palate
- Dorsum of tongue
- Lips
- Vermillion border
- Perioral skin
- Nasopharynx
- Reddening of the oral mucosa
- Formation of numerous small, dome-shaped, or pin-head type vesicle
- Size-2-3 mm in diameter
- Vesicles contain clear fluid and rupture to form ulcers
- Ulcers are multiple, small, circular, punctuate, shallow, and painful
Primary Herpetic Infection Treatment:
- Fluid administration
- Acetaminophen- to reduce fever
- Topical anesthesia- to decrease oral pain
- Have red margins and yellowish or greyish floor
- Small ulcers fuse to form diffuse, large, whitish ulcers
- They are surrounded by a red halo
- Gingival margins are red, swollen, and painful and have punched-out erosions
- Difficulty in taking food
- Difficulty in mastication
- Difficulty in swallowing
- Numerous vesicle formations over the tonsillar area and posterior pharynx
Primary Herpetic Infection Investigations:
- Lesions show features of epithelial hyperplasia with acanthosis and hyperkeratosis
- Superficial epithelial cells show dense aggregates of nuclear chromatin
- Minor atypical changes include basal cell hyperchromatic and an increased number of mitoses
Primary Herpetic Infection Treatment:
- Fluid administration
- Acetaminophen- to reduce fever
- Topical anesthesia- to reduce oral pain
- Acyclovir- to reduce symptoms of infection
Viral Infections Short Essays
Question 1. Herpangina.
Answer:
Herpangina Clinical Features:
- Age – Young children of the aged group 3 to 10 years
- Incubation period – 2 – 10 days
- Site – Commonly occurs over posterior pharynx, tonsil, faucial pillars, and soft palate
Herpangina Prodromal Symptoms:
- Fever, chills
- Headache
- Anorexia, vomiting
- Abdominal pain
- Sore throat, dysphagia
Herpangina Ulceration:
- The lesion initially appears as a punctuate macule
- This turns into papules and vesicles
- Within 24 – 48 hours, vesicles rupture to form a 1-2 mm ulcer
- They show a grey base
- They generally heal without treatment
Herpangina Differential Diagnosis:
1. Primary Herpes Simplex Infection: Herpangina occurs in epidemic
2. Herpes Zoster: Segmental distribution of vesicles occurs
Herpangina Treatment – Only palliative treatment is done
Question 2. Infectious Mononucleosis.
Answer:
Infectious Mononucleosis Synonym – Glandular fever
- Infectious Mononucleosis is a benign acute infectious disease caused due to the Epstein-Barr virus, a herpes virus that infects the B- B-lymphocytes
Infectious Mononucleosis Clinical Features:
- Incubation period – 10 – 40 days
- Age-Young age
Infectious Mononucleosis Features:
- Sore throat
- Fever -101oF – 103oF
- Headache
- Photophobia
- Nausea, vomiting, diarrhea
- Erythematous macular rash
- Splenomegaly, hepatomegaly
- Lymphadenopathy
- Myalgia, arthralgia
- Depression and cognitive defect
Infectious Mononucleosis Oral Manifestations: Site affected – soft palate, labial and buccal mucosa
Infectious Mononucleosis Features:
- Petechiae over the soft palate
- Ulcerative gingivitis, periodontitis
- Stomatitis
- Inflamed and enlarged tonsils
- Tonsils are covered by pseudo-membrane
- Sore throat
- Dysphagia
- Bleeding occurs from the oro-nasopharyngeal region and the gingiva
Infectious Mononucleosis Complications:
- Airway obstruction.
- Splenic rupture
- Neurological involvement
- Hemolytic anemia
Infectious Mononucleosis Diagnosis:
- Positive Paul Bunnel test
- Increase in WBC count
Infectious Mononucleosis Management:
- For Oral Lesions
- Topical anesthetic agent
- Hydrogen peroxide rinses
- For Fever And Pain
- Antipyretics and Analgesics are prescribed
- To Control Infection
- Ganciclovir
- Alfa interferon
- To Avoid Complication
- Corticosteroids are indicated
Oral Medicine Viral Infections Short Answers
Question 1. Herpes labialis.
Answer:
Herpes Labialis
Herpes Labialis occurs in patients with no prior infection with HSV-1 (Herpes Simplex Virus-1)
Herpes Labialis Clinical Features:
- Age:
- It occurs in children and young adults
- Incubation period – 5 – 7 days
- Prodromal generalized symptoms
- Fever, malaise
- Headache
- Nausea, vomiting
- Painful mouth
- Sore throat
- Irritability
- Excessive drooling of saliva
- Lack of tactile sensation
- Cervical lymphadenopathy
- Later oral symptoms
- Numerous vesicle formations over the keratinized mucosa
- Vesicles are thin-walled
- They contain clear fluid
- They rupture leaving multiple, small, punctuate shallow painful ulcers of size 2-6 mm
- Ulcers are surrounded by a red ring of inflammation
- Ulcers may become secondarily infected
- Healing starts in about 3 days and is completed within 7-14 days
Herpes Labialis Treatment:
- To prevent secondary infection – Antibiotics are given
- To control fever – Antipyretics are given
Question 2. Post Herpetic Neuralgia.
Answer:
Post Herpetic Neuralgia
Post Herpetic Neuralgia is a complication of zoster infection
Post Herpetic Neuralgia Etiopathogenesis:
- Nerve injury
- Zoster virus attacks the peripheral nerve and leads to atrophy of dorsal horn cells in the spinal cord
- Infection
- Persistent infection of trigeminal ganglion
Post Herpetic Neuralgia Clinical Features:
- Age and Sex – Common in older women
- Presentation
- Skin rashes appear
- They are painful
- Pain continues for weeks and months, more than 6 months
- There may be paresthesia, hyperesthesia, and allodynia
- There is also the presence of a sensory deficit
Post Herpetic Neuralgia Management:
- Prevention: Use of live attenuated varicella-zoster vaccine
- Topical Therapy: Use of topical agents like lidocaine, capsaicin
- Drug Therapy: Use of Amitriptyline, Carbamazepine to minimize pain
- Surgery: Carried out at the level of peripheral nerve or dorsal root
- Steroid Therapy: Steroid injections are given to reduce the pain of the patient
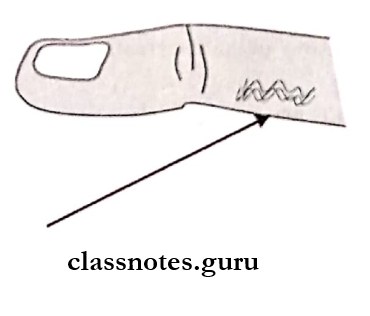
Question 3. Herpetic Whitlow.
Answer:
Herpetic Whitlow
- Herpetic Whitlow is caused by Herpes Simplex Virus
- Herpetic Whitlow is the infection of a finger by the virus through the break in the skin
- A dentist may experience it through contact with lesions of the mouth or saliva of patients who are asymptomatic carriers of HSV
- The lesions are usually preceded by prodromal symptoms of burning or tingling sensation
Oral Medicine Viral Infections Viva Voce
- Herpes simplex virus causes oral ulcerations in immunocompromised patients
- Herpes virus shows prodromal symptoms preceding local lesions
- Acyclovir controls herpes infections by inhibiting DNA replication in HSV-infected cells
- Skin eruptions found in rheumatic fever are known as erythema marginatum
- Varicella Zoster virus is the most common viral infection in older patients
- Lipschutz bodies are seen in primary herpetic stomatitis
- Strawberry tongue is seen in scarlet fever
- Koplik’s spots are a characteristic feature of measles
- Rubella is teratogenic virus
- Herpetic whitlow occurs in fingers
- In herpes simplex there is ballooning degeneration of inclusion bodies called Lipschutz bodies
- Herpes simplex is caused by herpes simplex virus type 1
- Herpangina is caused by the coxsackie virus
- Measles is caused by the rubella virus, paramyxovirus
