Haemorrhage Shock And Blood Transfusion Long Essays
Question 1. Classify shock. Describe the pathophysiology, clinical features and management of shocks.
Answer:
Shock:
- Shock is a condition in which circulation fails to meet the nutritional needs of the cells and fails to remove the metabolic waste products.
- It is characterised by hypoperfusion and severe dysfunction of vital organs.
Shock Classification:
- Haematogenic or hypovolaemic shock.
- Occurs due to loss of blood, plasma or body water and electrolytes.
- Caused by haemorrhage, vomiting, diarrhoea, dehydration, etc.
- Traumatic shock.
- Caused by major fractures, crush injuries, burns, extensive soft tissue injuries and intraabdominal injuries.
- Neurogenic shock.
- Caused by paraplegia, quadriplegia, trauma to the spinal cord and spinal anaesthesia.
- Cardiogenic shock.
- Caused by injury to the heart, myocardial infarction or congestive cardiac failure.
- Septic shock.
- Occurs due to gram-negative septicaemia.
- Miscellaneous types – includes:
- Anaphylactic shock.
Physiology: It can be described as 2 processes.
- Reduced effective circulating volume.
- May result in either.
- By actual loss of blood volume or
- By decreased cardiac output.
- May result in either.
- Tissue anoxia.
Haemorrhage shock and blood transfusion long essay
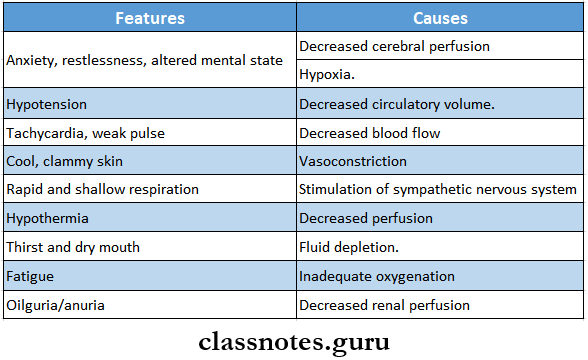
Shock Clinical features:
Management: AIMS:
- To increase cardiac output.
- To improve tissue perfusion to vital organs.
Shock Treatment:
- Maintenance.
- Maintain a patent airway and oxygen.
- Head position – At a low position with the face turned to one side
- Control of haemorrhage.
- Done by elevation, compression bandages or by ligation of blood vessels.
- Extracellular fluid replacement.
- Nonsugar, nonprotein crystalloid is preferred.
- Normal saline or Ringer’s lactate should be started first.
- Correct acid-base disturbance.
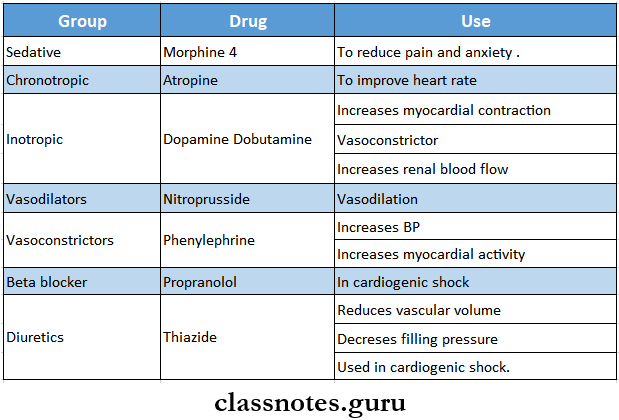
- Drugs.
Long essay on types of shock and management
Question 2. Describe the pathophysiology, clinical features and treatment of septic shock.
Answer:
Septic Shock:
- Septic shock is caused by to release of endotoxin in blood, mostly by Gram-negative organisms.
- Occurs in cases of severe septicaemia, peritonitis or meningitis.
- Pathophysiology.
Read And Learn More: General Surgery Question and Answers
Presence of gram-positive and gram-negative organisms
↓
Local inflammation occurs
↓
Release of endotoxins from the organism
↓
Activation of neutrophils, monocytes & macrophages.
↓
Release of inflammatory mediators.
↓
Cellular chemotaxis.
↓
Endothelial injury
↓
Activation of the coagulation cascade
↓
Massive fluid loss
↓
Septic shock
Septic Shock Clinical Features:
- Initially, chills and fever above 100 °C occur.
Septic Shock Types:
- Early warm shock.
- There is cutaneous vasodilation.
- Body temperature increases
- Cutaneous vasodilatation occurs.
- Arterial blood pressure falls.
- Cardiac output increases.
- Skin remains warm, pink and well-perfused.
- Pulse rate increases
- Late cold shock.
- There is increased vascular permeability
- Cardiac output is decreasing.
- Hypovolemia occurs.
Septic Shock Treatment:
- Removal of septic focus.
- Drainage of pus under anaesthesia.
- Closure of perforation.
- Resection of gangrene.
- Antibiotics.
- Administered after antibiotic sensitivity tests.
- Initial antibiotics are
- Cephalothin – 6 – 8 gm/day IV in 4 – 6 divided doses.
- Gentamicin – 5 mg/kg/day.
- Clindamycin
- Fluid replacement.
- Crystalloids such as isotonic saline as Ringer’s lactate, may be used.
- Blood transfusion – to maintain haemoglobin level at 10 mg%.
- Supportive care.
- Oxygenation.
- Mechanical ventilation.
- Endotracheal intubation.
- Steroids.
- Short-term, high-dose steroid therapy is used.
- An initial dose of 15 – 30 mg/ kg body weight of methylprednisolone is given.
- Same dose repeated within 4 hours.
- Vasoactive drugs.
- Vasodilators such as phenoxybenzamine are used along with fluid replacement.
- Inotropic agents such as isoproterenol are used to restore adequate circulation.
- It produces mild peripheral vasodilation.
- There is a slight fall in BP.
Blood transfusion long answer question
Question 3. Describe the pathophysiology, clinical features and management of haemorrhage or hypovolaemic shock.
Answer:
Haemorrhage shock/Hypovolaemic shock: Such shock occurs due to sudden loss of blood volume or loss of fluid from the vascular space.
Pathophysiology:
Haemorrhage
↓
Loss of blood
↓
Decreased filling of the right heart.
↓
Decreased filling of the pulmonary vasculature
↓
Decreased filling of the left atrium and ventricle
↓
Decrease in stroke volume.
↓
Drop in arterial blood pressure
Hypovolaemic Shock Clinical Features:
- Depending on the degree of blood loss it can be described into three types.
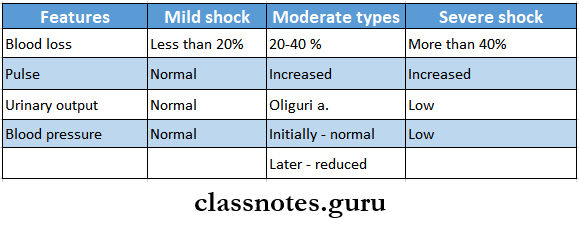
Hypovolaemic Shock Management:
- Resuscitation.
- Maintain airway with adequate ventilation and oxygenation.
- Lower the head with jaw support.
- Immediate control of bleeding.
- Raise the foot end of the bed.
- Use of compression bandages.
- Extracellular fluid replacement.
- Ringer’s lactate, Ringer’s acetate or normal saline supplemented with 1-2 ampules of sodium bicarbonate is used.
- 1000 – 2000 ml solution is given intravenously within 45 minutes.
- Blood transfusion was done if required.
Question 4. Describe neurogenic shock and its management.
Answer:
Neurogenic Shock Causes:
- Paraplegia.
- Quadriplegia.
- Trauma to spinal cord
- Spinal anaesthesia.
Pathophysiology:
Blockade of the sympathetic nervous system
↓
Loss of arterial and venous tone
↓
Peripheral pooling of blood.
↓
Decrease in cardiac filling
i
Decrease in stroke volume.
↓
Decrease in pulmonary blood volume.
↓
Decrease in cardiac output.
↓
Shock
Neurogenic Shock Clinical Features:
- Skin remains warm, pink and well-perfused.
- Urinary output – normal.
- Heart rate is rapid.
- Blood pressure – decreased
Neurogenic Shock Management:
- Elevation of the legs to correct peripheral pooling of blood.
- Fluid administration to increase cardiac output.
- Use of a vasoconstrictor drug.
- It increases BP and myocardial activity.
Classification and management of haemorrhage essay
Question 5. Classify haemorrhage and its management, and describe the causes and clinical features. How will you manage a case of primary haemorrhage after a dental extraction?.
Answer:
Haemorrhage: Haemorrhage is defined as the escape of blood from blood vessels.
Haemorrhage Classification:
- According To The Source:
- External haemorrhage.
- Seen externally.
- Internal haemorrhage.
- Not seen externally, it is hidden,
- Example: GIT bleeding.
- Arterial haemorrhage.
- It is a haemorrhage coming out of the artery.
- It is bright red in colour.
- Venous haemorrhage.
- It is a haemorrhage coming out of a vein.
- It is dark red in colour.
- Capillary haemorrhage.
- It is a haemorrhage coming out of a capillary
- It is bright red in color, and it oozes out
- External haemorrhage.
- According To The Time Of Appearance:
- Primary haemorrhage.
- Occurs at the time of injury.
- Reactionary haemorrhage.
- Occurs within 24 hours of injury.
- Secondary haemorrhage.
- Occurs after 7-14 days of injury.
- Primary haemorrhage.
Haemorrhage Management: To Stop Blood Loss.
- Rest.
- Use of sedatives and analgesics.
- Morphine is administered IM/IV.
- Inj. Pethidine is better than morphine.
- Position of the patient.
- The head end of the bed is raised in haemorrhage oc- curing after thyroidectomy.
- The foot end of the bed is raised in case of haemorrhage from varicose veins.
- Pressure and packing.
- Use of sterile gauze pieces and pressure bandage.
- At home, it can be done with clean linen cloth.
- Operative methods.
- Haemorrhage can be controlled by.
- Use of artery forceps.
- Ligation of blood vessels.
- Smaller vessels are coagulated with diathermy.
- Bigger vessels are sutured
- In case of oozing blood-following is used
- Oxycel or gelatine sponge.
- Gauze soaked in adrenaline (1:1000)
- Bone wax for bleeding occurring from the bone.
- Haemorrhage can be controlled by.
Haemorrhage Causes:
- Bleeding disorders.
- Low platelet count
- Anticoagulant medication.
- Broken or ruptured blood vessels.
- Severe trauma
- After surgery.
- After childbirth.
Haemorrhage Clinical Features:
- Blood loss
- Increased pulse rate
- Thready pulse
- Low blood pressure
- Pallor Restlessness
- Deep respiration
- Cold and calmmy extremities
- Empty veins
- Low urinary output.
Management Of Primary Haemorrhage:
1. Post-Extraction Bleeding.
Removal of clots with gauze
↓
Placement of gauze pad or tea bag over socket.
↓
Patient is instructed to bite over it for 1 hour
↓
Repeated 2-3 times.
↓
Prevent disruption of clot
2. If Bleeding Continues.
Anaesthetise the area
↓
Curette the socket
↓
Remove the existing clot and freshen the bone
↓
Irrigate with normal saline
↓
Place a local haemostatic agent into the socket
↓
Suture under gentle tension
Pathophysiology of shock long essay
Question 6. Describe the indications and complications of blood transfusion.
Answer:
Blood Transfusion: It is the process of transferring blood or blood-based products from one person into the circulatory system of another.
Blood Transfusion Indications:
- Acute haemorrhage – external or internal.
- Certain major operations, like a radical mastectomy.
- In deep burns.
- Preopera is lively in anaemic patients.
- Postoperatively in septicaemia.
- In anaemia.
- In severe malnutrition.
- In coagulation disorders like haemophilia.
- In the treatment of erythroblastosis foetal.
- During chemotherapy for malignant diseases.
Blood Transfusion Complications:
- Transfusion Reactions:
- Incompatibility
- Incompatibility Causes:
- Incompatible transfusion.
- Transfusion of hemolyzed blood.
- Transfusion of old blood.
- Incompatibility Clinical features:
- Fever, rigour.
- Headache.
- Nausea, vomiting.
- Pain in the loins.
- Tingling sensation in the extremities.
- The feeling of tightness in the chest
- Dyspnea.
- Diminished urinary output.
- Haemoglobinuria.
- Jaundice
- Incompatibility Treatment:
- Stop the transfusion immediately.
- Administration of 4 fluids.
- Alkalization of blood with 10 ml of isotonic solution of sodium lactate and simultaneously 10 ml of saturated solution of sodium bicarbonate 4.
- Use of 80 -120 mg furosemide IV to provoke diuresis.
- Antihistamine and hydrocortisone may be prescribed.
- Incompatibility Causes:
- Pyrexia Reactions.
- Pyrexia Causes:
- Lack of sterilisation
- Infected donor’s apparatus
- Infected blood transfusion,
- Rapid transfusion,
- Presence of sulphur compounds in rubber tubing.
- Pyrexia Clinical Features:
- Pyrexia.
- Rigour, chills.
- Restlessness.
- Headache.
- Increased pulse rate.
- Nausea and vomiting.
- Pyrexia Treatment:
- Stop the transfusion immediately.
- Cover the patient with a blanket.
- Antipyretic and antihistaminic drugs are injected.
- Pyrexia Causes:
- Allergic Reaction:
- Allergic Cause:
- Allergic reaction to plasma product
- Allergic Features:
- Mild tachycardia.
- Urticarial rash.
- Fever
- Dyspnea
- Circulatory collapse.
- Allergic Treatment:
- Stop transfusion
- Administer 10 mg of chlorpheniramine.
- Allergic Cause:
- Sensitization To Leucocytes And Platelets:
- Use of antipyretics, antihistamines and steroids.
- Incompatibility
- Transmission Of Diseases:
- Diseases transmitted are.
- Serum hepatitis
- AIDS
- Bacterial infections.
- Diseases transmitted are.
- Reactions Caused By Massive Transfusion:
- Acid-base imbalance – alkalosis.
- Hyperkalaemia.
- Citrate toxicity.
- Hypothermia.
- Failure of coagulation.
- Complications Of Over-Transfusion:
- Congestive cardiac failure occurs.
- Other Complications:
- Thrombophlebitis
- Air embolism.
Blood transfusion indications and complications essay
Question 7. Define shock. Describe the pathophysiology and classification of shock. Discuss management of hypovolaemic shock
Answer:
Shock Definition: Shock is a condition in which circulation fails to meet the nutritional needs of the cells and fails to remove the metabolic waste products
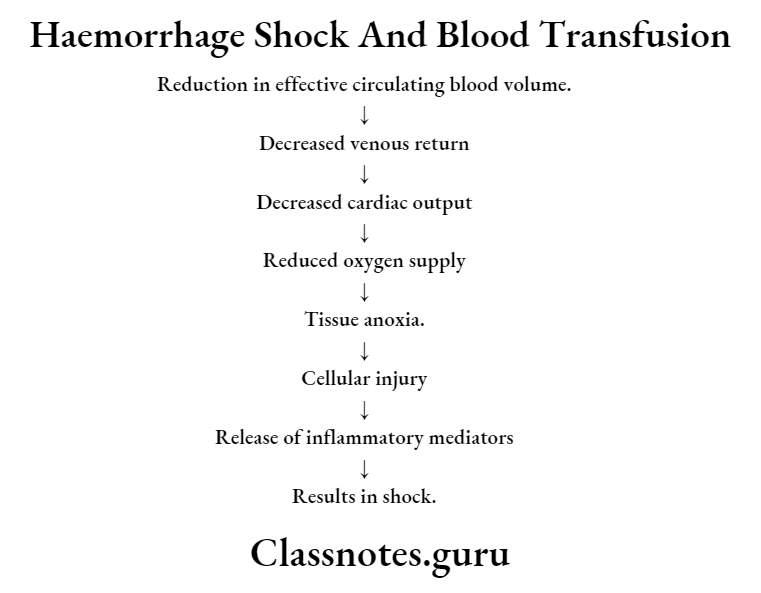
Pathophysiology
- Reduced effective volume
- It may result either
- By actual loss of blood volume or
- By decreased cardiac output
- It may result either
- Tissue anoxia
- Reduction in effective circulating blood volume
- Reduced venous return
- Decreased cardiac output
- Decreased oxygen supply
- Tissue anoxia
- Cellular injury
- Release of inflammatory mediators
- Results in shock
Shock Classification
- Haematogenic or hypovolaemic shock
- Traumatic shock
- Neurogenic shock
- Cardiogenic shock
- Septic shock
- Miscellaneous
- Anaphylactic shock
Management Of Hypovolemic Shock
- Resuscitation
- Maintain airway with adequate ventilation and oxygenation
- Lower the head with jaw support
- Immediate control of bleeding
- Raise the foot end of the bed
- Use of compression bandages
- Extracellular fluid replacement
- Ringer’s lactate, Ringer’s acetate or normal saline supplemented with 1-2 ampules of sodium bicarbonate is used
- 1000-2000 ml solution is given within 45 min intravenously
- Blood transfusion done if required
Principles of transfusion medicine long essay
Question 8. What are blood components? Write in detail about the indications, contraindications and complications of blood transfusion.
Answer:
Blood Components
- There are four main components of blood
- Plasma
- Red blood cells or erythrocytes
- White blood cells or leukocytes
- Platelets
Blood Transfusion
- Indications
- Acute haemorrhage
- Major surgery
- Deep burns
- Pre-operative and post-operative in anaemia
- In malnutrition
- In coagulation disorders
- In erythroblastosis fetalis
- During chemotherapy in malignant diseases
- Contraindications
- Infections
- Aortic stenosis
- Angina
- Significant cardiac or pulmonary disease
- Coronary heart disease
- Cyanotic heart disease
- Uncontrolled hypertension
- Complications
- Transfusion reactions
- Incompatibility
- Pyrexia reactions
- Allergic reactions.
- Transmission of diseases
- Reactions caused by massive transfusion
- Acid-base imbalance
- Hyperkalaemia
- Citrate toxicity
- Hypothermia
- Failure of coagulation
- Transfusion reactions
- Complications of over-transfusion
- Congestive cardiac failure
- Other complications
- Thrombophlebitis
- Air embolism
