General Surgery Miscellaneous Important Notes
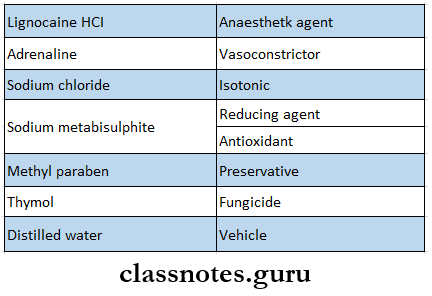
Composition of Local Anaesthesia
General surgery miscellaneous question and answers
General Surgery Miscellaneous Short Essays
Question 1. Local anaesthesia
Answer:
Local Anaesthesia Definition: It is loss of sensation in a circumscribed area of the body characterized by depression or excitation of nerve endings and inhibition of the conduction process of peripheral nerve
Local Anaesthesia Composition:
- Local anesthetic- ester or amide
- Vasoconstrictor- Epinephrine
- Antioxidant- Sodium metabisulphite
- Preservative- Methyl paraben
- Fungicide-Thymol
- Salt- sodium chloride
- Vehicle- Distilled water or Ringers lactate solution
Local Anaesthesia Ideal Properties:
- Nonirritant
- No permanent damage to nerve
- Low systemic toxicity
- Effective
- Short onset of action
- Long-lasting effect
- Potent
- Free of allergens
- Stable and biocompatible
- Able to sterilize it
Question 2. Complications of local anesthesia
Answer:
Local Anaesthesia Complications:
1. Needle Breakage:
- Due To Sudden Movement Of The Patient
- Narrow gauge needle
- Broken needle
- Bonded needle
- Local Anaesthesia Management:
- Radiograph to locate it
- Expose the site and remove it
2. Facial Nerve Paralysis:
- Facial Nerve Paralysis Causes: Insertion of needle into the parotid capsule
- Facial Nerve Paralysis Management:
- Self-curing
- Eye can be protected with the help of an eye pad
- Paraesthesia:
- Paraesthesia Cause: Injury to the nerve
- Paraesthesia Management: Self-recovery by regeneration of nerve
Important general surgery questions with answers
Read And Learn More: General Surgery Question and Answers
3. Trismus:
- Trismus Cause: Trauma to medial pterygoid muscle, Contaminated needle
- Trismus Management:
- Analgesic
- Muscle relaxants
- Mot fomentation
- Physiotherapy
4. Pain On Injection:
- Pain On Injection Cause: Blunt needle, Broader gauge needle
- Pain On Injection Management: Use of short, narrow-gauge needle
5. Burning On Injection:
- Burning On Injection Cause:
- An acidic solution of LA
- Contaminated needle
- Burning On Injection Management:
- Isotonic solution by addition of bicarbonate
- Use of disposable needle
6. Soft Tissue Injury:
- Soft Tissue Injury Cause: Due to being unaware of numbness of lips patient tries to do lip-biting
- Management:
- Explain to the patient about the numbness
- Use of lifeguards in children
- Soft Tissue Injury Hematoma:
- Hematoma Cause: Injury to blood vessels
- Hematoma Management:
- Assure of proper anatomy of landmarks and nerve
- Massage the area
- Antibiotics
- Hot fomentation
7. Infection:
- Local Anaesthesia Infection Causes: Contaminated needle
- Local Anaesthesia Infection Management:
- Use of disposable needle
- Antibiotics
- Drainage of space involved
- Physiotherapy
8. Necrosis Of Tissues Causes :
- Seen in palatal injection
- This region is tightly bound to the underlying bone
- Thus excessive pressure is required for the insertion of the needle
- This leads to the blanching of the area
- Vasoconstriction and localized necrosis
9. Edema Causes:
- Injury to nerve
- Contaminated needle
10. Edema Management:
- Subsidies on their own
- Avoid application of hot fomentation
- Application of cold fomentation
- As it acts as a vasoconstrictor and analgesic
11. Post-anesthetic lesions
- Ulcers
- Allergic reactions
Post-Anesthetic Lesions Causes:
- Trauma
- Allergy to LA agent
Common general surgery viva questions
Systemic Complications Local Anaesthesia :
Overdose:
- Overdose Causes:
- Excessive dose of LA
- Systemic disorders of metabolism
- Overdose Features
- Nausea
- Vomiting
- Diplopia
- Tremors
- Acidosis
- Respiratory distress
- Chest pain
- Bradycardia
- Hypotension
- Dizziness
- Overdose Management:
- Reassure the patient
- Maintain patient’s airway
- Intubate if necessary
- Cardiac life support given
- 4 fluids and vasopressors given for hypotension
- Hypersensitivity:
- Hypersensitivity Causes:
- Allergy to LA
- Allergy to the preservative used
- Hypersensitivity Features:
- Pruritis
- Utricaria
- Dyspnoea
- Wheezing
- Nausea, vomiting
- Erythema
- Hypersensitivity Management:
- Stop the procedure
- Mild allergy-corticosteroids
- Severe allergy- epinephrine 1:1000 of 0.3-0. ml SC
- If symptoms continue 5 ml of 1:10000 epi nephrite given 4
- Hypersensitivity Causes:
Question 3. FNAC
Answer:
FNAC Method:
- 23-26 gauge needle is inserted into the tissues
- Aspirate the needle
- Cystic fluid is collected in it
- Examine the fluid
FNAC Indication:
- Cystic cavity
- OKC
General surgery FAQs for students
Question 4. Anaphylaxis
Answer:
Anaphylaxis Features:
- Severe dyspnoea
- Hoarseness of voice
- Hypotension
- Nausea
- Cyanosis
- Abdominal cramps
- Tachycardia
- Bronchospasm
- Chest tightness
Anaphylaxis Management:
- The upright position of the patient
- Elevate the legs
- Basic life support
- Administer adrenaline 1:1000 0.3 mg IM
- Administer oxygen
- Recovery of patient
- Give antihistamine IM
- Continue basic life support
- Transfer the patient to the hospital
Question 5. Oral submucous fibrosis
Answer:
Oral Submucous Fibrosis
- Oral Submucous Fibrosis is a pre-cancerous condition
- It is characterized by juxta epithelial inflammatory reaction in the oral mucosa followed by a fibro elastic transformation of the lamina propria loading to mucosal atrophy, rigidity, and trismus
Oral Submucous Fibrosis Etiology:
- Consumption of red chilies
- Consumption of areca nuts
- Nutritional deficiencies
- Immunological factors
- Genetic factors
Oral Submucous Fibrosis Features:
- Burning sensation
- Difficulty in mastication
- Referred pain in the ear
- Depapillation of longue
- Restricted movement of floor of mouth
- Shrunken uvula
- Fibrous bands
- Restricted mouth opening
- Stiffness of buccal mucosa
Oral Submucous Fibrosis Management:
- Quit the habit
- Antioxidant- Oxyacc-1 capsule/ day
- Multivitamin therapy
- Steroid- Betnovate 0.12%
- Tumeric application
- Intralesional injection of Hyaluronidase-1500 U
- Physiotherapy
- Splitting of fibrous bands
- Laser
General surgery exam questions and answers
Question 6. Mechanism of action of LA
Answer:
Mechanism Of Action Of LA
- Displacement of calcium ions from sodium channel receptor site which permits
- The binding of LA molecule to this site produces
- Blockade of the sodium channel and a
- Decrease in sodium conductance, which leads to
- Depression of rate of electrical depolarization
- Failure to achieve the threshold potential level along with a
- Lack of development of propagated action potential which is called
- Conduction blockade
Question 7. Mandibular nerve block
Answer:
Mandibular Nerve Block
- Nerves Anaesthesized: inferior alveolar nerve and its branches
- Areas To Be Anesthetized: mandibular teeth and its supporting tissues
Mandibular Nerve Block Landmarks:
- Mucobuccal fold
- Anterior border of coronoid process
- Coronoid notch
- Pterygomandibular raphe
- Retromolar pad
- Retromolar triangle
- External oblique ridge
Mandibular Nerve Block Technique:
- Position the patient in a semi-reclined position
- Move your index finger over the mesiobuccal fold up to the external oblique ridge
- Move it up and down to obtain depression
- This is a coronoid notch
- Retract the cheek
- Support the mandible
- Insert 1 5/8 inch 25 gauge needle from the lingual side
- Aspirate and Slowly deposit the solution
Positive Aspiration: 10-15%
Question 8. Paget’s disease of bone
Answer:
Paget’s Disease Of Bone
Paget’s Disease Of Bone is bone disorder characterized by an excessive uncoordinated phase of bone resorption and subsequent deposition of bone in the same area
Paget’s Disease Of Bone Clinical Features
- Age-old people are usually affected
- Sex – common in males
- Site – Weight-Bearing Areas
- Skull
- Pelvis
- Sternum
- In jaws, common in the maxilla than in the mandible
- Presentation
- Pain is always present
- Bilateral swelling
- Waddling gait
- Involvement of facial bone causes leontiasis ossa
- Headache
- Enlargement of skull
Paget’s Disease Of Bone Radiological Features
- Haphazardly arranged radiolucent and radiopaque areas representing new bone deposition and resorption in the involved area
- This gives cotton wool appearance
- In jaw, it shows
- Prognathic mandible
- Hypercementosis
- Obliteration of periodontal ligament space
- Root resorption
- Loss of lamina dura
Paget’s Disease Of Bone Complication: Osteosarcoma
General surgery question bank with answers
Question 9. Causes and complications of chronic otitis media
Answer:
Chronic Otitis Media Causes:
- Inflammation of the middle ear
- Resistant bacterial infection
- Risk factors
- Traumatic perforation of tympanic membrane
- Insertion of grommets
- Craniofacial abnormalities
Chronic Otitis Media Complications
- Meningitis
- Intracranial abscess
- Facial paralysis
- Conductive hearing loss
- Scarring of tympanic membrane
- White calcified plaques in tympanic membrane
Question 10. Causes of inflammation
Answer:
Causes Of Inflammation
- Infection
- Injury
- Autoimmune disorders
- Long-term exposure to irritants
- Contributing factors are
- Smoking
- Alcohol
- Stress
- Obesity
General Surgery Miscellaneous Short Answers
Question 1. Pain
Answer:
Pain
- Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage
- It is considered as part of the body’s defense system
Pain Management
- Acute pain- by analgesics and antibiotics
- Chronic pain
- Analgesics
- Sedatives
- Physiotherapy
Question 2. Adenoid
Answer:
Adenoid
- Adenoid is mass of soft tissue present behind the nasal cavity.
- Adenoid is part of immune system
- Adenoid is formed by lymphoid tissue.
- Adenoid is present at birth and disappears in adolescence.
Adenoid Causes:
- Bacterial infections
- Viral infections
- Pollutants
Adenoid Disorders:
- Adenoiditis
- Obstructive sleep apnoea
- Middle ear infections
Adenoid Treatment:
- Adenoidectomy
- Antibiotics to treat infection
General surgery short and long questions with answers
Question 3. Otitis media
Answer:
Otitis media
- In middle ear infections, the middle ear gets inflamed and is filled with fluid
- This is called Otitis media
Otitis Media Clinical Features:
- In Infants
- Irritability
- Pulling and stretching of the ear
- vomiting
- Drainage from ear
- Fever
- In Adults
- Earache
- Hearing problems
- Fever
- Pressure sensation in the ear
- Dizziness
- Nausea
- Vomiting
Question 4. Chemotherapy
Answer:
Chemotherapy
Chemotherapy refers to the use of chemicals in infectious diseases to destroy microorganisms without damaging the host tissues
Chemotherapy Drugs:
- Alkylating agents
- Antimetabolites
- Anthracyclines
- Plant alkaloids
- Topoisomerase inhibitors
- Anti-tumor agents
Chemotherapy Adverse Effects:
- Immunosuppression
- Myelosuppression
- Fatigue
- Gastrointestinal distress
- Nausea
- Vomiting
- Diarrheoa
- Apolecia
- Damage to specific organs
- Cardiotoxicity
- Hepatotoxicity
- Nephrotoxicity
- Ototoxicity
Question 5. Insulin
Answer:
Insulin
Insulin is stored in granules in the beta islet cells of the pancreas
Insulin Actions
- Stimulates uptake and metabolism of glucose in the peripheral tissues
- Inhibits lipolysis
- Facilitates amino acid uptake
Insulin Side Effects
- Hypoglycaemia
- Allergy
- Lipodystrophy
- Edema
Insulin Classification
- Conventional Insulins
- Short and long-lasting
- Intermediate-acting
- Long-acting
- Highly purified insulin
- Human insulin
- Insulin analogs
- Insulin mixtures
Previous year general surgery questions with solutions
Question 6. Penicillin
Answer:
Penicillin
β Lactum antibiotic Mechanism:
- Inhibit cell wall synthesis
- Inhibit transpeptidase thus inhibiting synthesis of peptidoglycan
Penicillin Classification:
- Natural- Penicillin G
- Semisynthetic
- Acid resistant – Penicillin V
- Penicillin resistant- Methicillin
- Aminopenicillin- Ampicillin
- Antipseudomonal penicillin- Carbenicillin
Penicillin Uses:
- Orodental infections
- Syphilis
- Gonorrhea
- Streptococcal infections
- Tetanus
- Prophylactic
- Gangrene
Penicillin Adverse Reaction:
- Hypersensitivity
- Anaphylaxis
- Local pain at the site of injection
- Suprainfection
- Farish Herxheimer reaction
Question 7. Antioxidant
Answer:
Antioxidant
Antioxidant is a molecule capable of inhibiting the oxidation of other molecules
Antioxidant Uses:
- Inhibit oxidation reactions
- Used as ingredients in dietary supplements
- Prevents cancer, coronary heart disease
- Industrial use as preservatives in food and cosmetics
- Prevents degradation of rubber and gasoline
Antioxidant Agents:
- Thiols
- Ascorbic acid
- Polyphenols
- Glutathione
- Superoxide dismutase
Question 8. Spinal anesthesia
Answer:
Spinal Anesthesia
- Local anesthetic solution is injected into the subarachnoid space between L2-3 or L3-4 below the end of the spinal cord
- The lower abdomen and lower limbs are anesthetized and paralyzed
Spinal Anesthesia Advantages
- Safe
- Affords good analgesic
- Muscle relaxant
- No loss of consciousness
Spinal Anesthesia Uses:
- Surgical procedures on the
- lower limb
- Pelvis
- Lower abdomen
- Obstetric procedures
- Cesarean section
Spinal Anesthesia Complications:
- Hypotension
- Bradycardia
- Respiratory paralysis
- Headache
- Cauda equine syndrome
- Sepsis
- Nausea
- Vomiting
Emergency surgery questions and answers
Question 9. Topical anaesthesia
(or)
Surface acting anaesthesia
Answer:
Topical Anaesthesia
Anesthesia of mucous membrane of the eye, nose, mouth, tracheobronchial tree, esophagus, and genitourinary tract can be produced by direct application of the anesthetic solution
Topical Anaesthesia Actions:
- Produces vasoconstriction
- Prolongs duration of action
- Anaesthesia is superficial
Topical Anaesthesia Agents Used:
- Tetracaine
- Lignocaine
- Phenylephrine
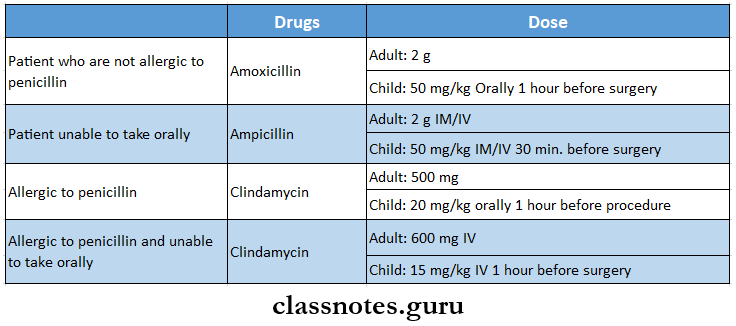
Question 10. Prophylactic antibiotics
Answer:
Prophylactic Antibiotics
Question 11. Drugs used in general anesthesia
Answer:
Drugs Used In General Anaesthesia
- Volatile Anaesthetics
- Ether
- Trichloroethylene
- Halothane
- Enflurane
- Isoflurane
- Sevoflurane
- Gaseous Anaesthetics
- Nitrous oxide
- Cyclopropane
- Intravenous Anaesthetics
- Thiopentone
- Methohexitone sodium
- Propanidid
- Ketamine
- Propofol
- Fentanyl
- Oxygen
Question 12. Signs of inflammation
Answer:
Signs Of Inflammation
- Rubor – redness
- Cause – vasodilatation in the area of inflammation
- Tumor – swelling
- Cause
- Increased local hydrostatic pressure
- Transudation of fluid into extracellular space
- Cause
- Calor – heat
- Cause – vasodilatation
- Dolor – pain
- Function Laesa – loss of function
Postoperative complications questions and answers
Question 13. Paronychia
Answer:
Paronychia
- Paronychia is a common hand infection
1s. Acute paronychia
- Occurs in the subcuticular area under eponychia
- Cause – mild injury to finger
- Causative organisms – staphylococcus aureus and streptococcus pyogenes
Paronychia Features
- Suppuration occurs
- It spreads around the skin margin and under the nail causing hanging or floating nail
- Severe throbbing pain and tenderness with pus under the nail root
- Nail is tender to touch
Paronychia Treatment
- Antibiotics
- Analgesics
- Drainage of pus
- Removal of the floating nail
Chronic Paronychia: Occurs due to fungal infection
Chronic Paronychia Features:
- Itching in the-nailbed
- Recurrent pain
- Discharge
Chronic Paronychia Treatment
- Long-term antifungal therapy
- Antibiotics
- Removal of nails in severe infection
Short answer questions in general surgery
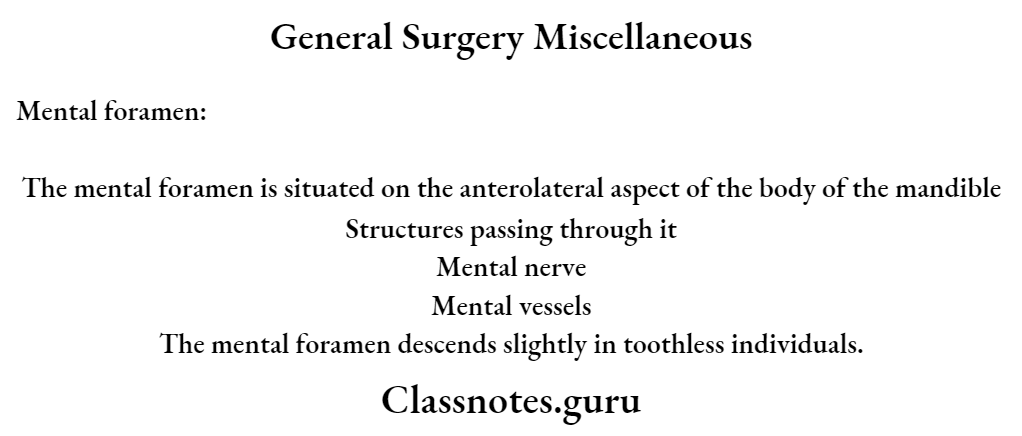
General Surgery Miscellaneous Viva Voce
- The primary site of action of the local anesthesia is nerve membrane
- Maxillary first molar is the most difficult tooth to Anaesthesize by infiltration alone
- Cocaine increases the vasoconstrictive action of adrenaline
- Succinylcholine prevents laryngospasm due to GA
- Most common cause of death occurring during GA administration is due to airway obstruction with improper ventilation.
