Question 1. Hypercalcemia
Answer:
Hypercalcemia Causes:
- Conditions associated with hypercalcemia and increased PTH levels
- Hyperparathyroidism
- Chronic renal failure
- Conditions associated with hypercalcemia and low PTH levels
- Multiple myeloma
- Sarcoidosis
- Hyperthyroidism
- Thiazide diuretics
- Milk alkali syndrome
- Familial
Hypercalcemia Clinical Features
- Nausea, vomiting
- Pain in abdomen
- Dehydration
- Hypotension
Hypercalcemia Treatment:
- Avoid calcium-containing antacids
- Replacement of fluid and electrolytes by 4-6 l of normal saline
- To correct dehydration, hypotension, and calcium levels
- Forced diuresis by saline and diuretic frusemide given 4 to depress tubular reabsorption of calcium
- Drugs given include a generation bis- phosphonate ex: pamidronate given as a single 4 dose of 15-60 mg in normal saline
- Calcitonin is used in emergency state
- Cinacalcet is used orally in hypercalcemia crisis
Endocrine System Short Essay Questions
Question 2. Thyrotoxicosis
Answer:
Thyrotoxicosis
- Thyrotoxicosis is a clinically toxic manifestation due to excess thyroid hormones
Thyrotoxicosis Causes:
- Common causes
- Grave’s disease
- Toxic nodular goitre
- Multinodular
- Solitary nodule
- Less common causes
- Thyroiditis Drug-induced
- Factitious
- Iodine induced
- Rarely
- Pituitary or ectopic TSH
- Thyroid carcinoma
Thyrotoxicosis Clinical Features:
- Goitre
- Weight loss, vomiting, diarrhea
- Increased pulse rate, dyspnea, arrhythmia
- Nervousness, restlessness, tremors, muscular weakness
- Perspiration, clubbing, loss of hair, pre-tibial myxoedema
- Amenorrhea, abortions, infertility, loss of libido
- Lid lag, exophthalmos, diplopia, watering of eyes
- Fatigue, heat intolerance, polydipsia
Question 3. Calcium homeostasis
Answer:
Regulation Of Calcium/ Hemostasis:
- Calcium level is regulated by
Calcitriol
- Calcitriol is the active form of vitamin D
Calcium Homeostasis Mechanism:
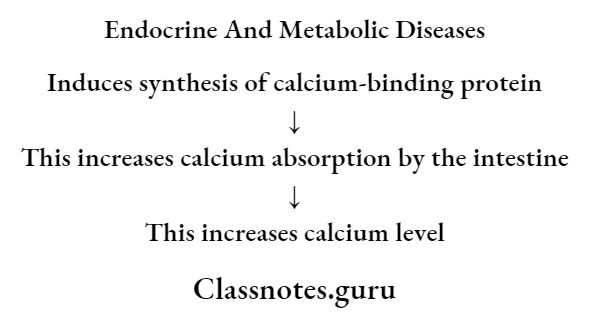
- Calcium homeostasis also promotes calcification and remodeling of bone.
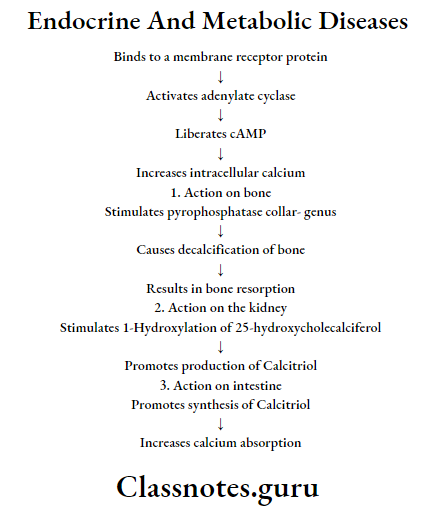
2. Parathyroid hormones
- Secreted by Parathyroid glands
Read And Learn More: General Medicine Question and Answers
Calcium Homeostasis Mechanism:
Question 4. Hypoglycemia-clinical features and management
Answer:
Hypoglycaemia
- Hypoglycaemia is defined as a fall in blood glucose concentration below 3.1 mmol/1
Hypoglycaemia Clinical Features:
- CVS symptoms
- Palpitation
- Tachycardia
- Anxiety
- Cardiac arrhythmias
- CNS symptoms
- Tremors
- Confusion
- Headache
- Tiredness
- Difficulty in concentration
- Slurred speech
- Drowsiness
- Convulsion
- Coma
- GIT symptoms
- Nausea
- Vomiting
- Dermatological symptoms
- Sweating
- Hypothermia
Hypoglycaemia Management:
- In unconscious patients
- Stop anti-diabetic medication
- Administer 50 ml of 50% intravenous glucose
- Intramuscular injection of 1 ml of glucagon
- Unconscious patients
- Oral glucose intake
- In severe cases
- 1 mg glucagon subcutaneously or intramuscularly and repeated if necessary after 10 minutes
Endocrine and metabolic disorders short answer
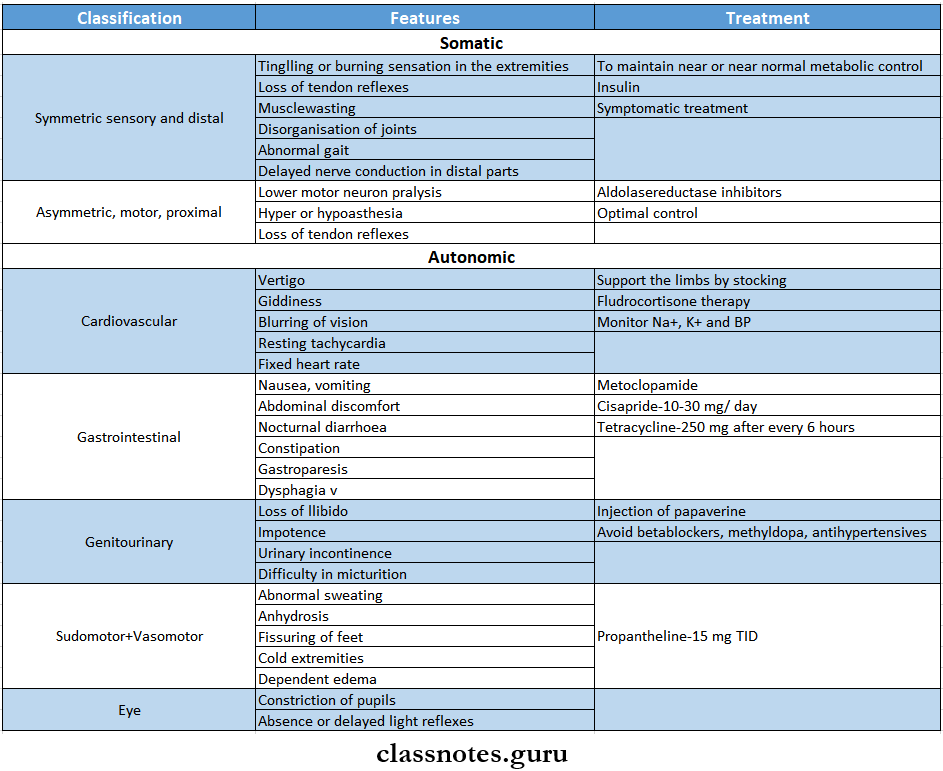
Question 5. Neurological complications of diabetes mellitus
Answer:
Neurological Complications Of Diabetes Mellitus
- Diabetes can involve any part of the nervous system except the brain
- Precipitating factors
- Poor glycaemic control
- Long control of diabetes
Pathological Changes:
- Axonal degeneration of myelinated and nonmyelinated fibers
- Patchy, segmental demyelination
- Vasculopathy
Question 6. Grave’s disease
Answer:
Grave’s Disease
- Grave’s disease is a diffuse goiter affecting the whole functioning thyroid tissue causing hypertrophy and hyperplasia due to abnormal thyroid stimulants
Grave’s Disease Clinical Features
- Grave’s Disease is a classical triad composed of
- Goitre
- Diffuse and symmetric enlargement of thyroid
- The gland surface is smooth
- Bruit is heard
- Thyrotoxicosis
- Excitability
- Restlessness
- Emotionally unstable
- Insomnia
- Muscle weakness
- Fatigue
- Myopathy
- Heat intolerance
- Increased sweating
- Weight loss
- Tachycardia
- Palpitation
- Increased cardiac output
- Gynaecomastia
- Increased libido
- Pretibial myxoedema
- Exophthalmos
- Protrusion of eyeballs
Grave’s Disease Treatment:
- Anti-thyroid drugs
- To restore the patient to the euthyroid state
- Radioactive iodine
- It destroys thyroid cells and reduces the mass of thyroid-functioning tissue
- Surgery
- Reduce active thyroid mass
Question 7. Acromegaly- clinical features and complications
Answer:
Acromegaly:
- Acromegaly occurs due to excess secretion of GH later in life after epiphyseal closure
Acromegaly Clinical Features:
- Thick bones-larger hands and feet
- Enlarged skull
- Increased intracranial pressure
- Headache
- Photophobia
- Visual disturbances
- Hepatomegaly
- Cardiomegaly
- Osteoporosis
- Arthralgia
- Excessive sweating
- Myalgia
- Bowing of legs
- Barrel shaped chest
Acromegaly Oral Manifestations:
- Enlarged mandible
- Class 3 malocclusion
- Macroglossia D Thick lips
- Proclamation of teeth
- Hypercementosis
- Large nose, ears, and prominent eyebrows
- Periodontitis
- Enlargement of maxillary air sinuses
Acromegaly Complications:
- High blood pressure (hypertension)
- Cardiovascular disease, particularly enlargement of the heart (Cardiomyopathy)
- Osteoarthritis
- Diabetes mellitus
- Precancerous growths (polyps) on the lining of your colon
- Sleep apnea is a condition in which breathing repeatedly stops and starts during sleep
- Carpal tunnel syndrome
- Reduced secretion of other pituitary hormones (hypopituitarism)
- Uterine fibroids, benign tumors in the uterus
- Spinal cord compression
- Vision loss
Short notes on endocrine disorders
Question 8. Addison’s disease
Answer:
Addison’s Disease
- Addison’s disease is due to progressive destruction of the three zones of the adrenal cortex and medulla with lymphatic infiltration
Addison’s Disease Clinical Features:
- Glucocorticoid insufficiency
- Weight loss
- Nausea and vomiting
- Malaise
- Weakness
- Anorexia
- Diarrhea
- Constipation
- Postural hypotension
- Hypoglycaemia
- Mineralocorticoid deficiency
- Hypotension
- Loss of androgens
- Reduction of pubic and axillary hair in females
- Increased ACTH secretion
- Pigmentation of exposed areas, pressure areas, mucous membranes, conjunctivae, and recently acquired scars
Question 9. Diabetes and surgery
Answer:
Diabetes And Surgery
- Patients with diabetes need to maintain very good oral hygiene as they are prone to odontogenic, periodontal, and other infections
- In well-controlled diabetics, dental procedures generally do not require any special precautions
- Antibiotic coverage may be required
- In uncontrolled diabetics, infections and wound healing may be a problem even after minor procedures
- If major dental procedures or surgery is to be undertaken, prior control of diabetes by the physician is needed
- If the patient is on only oral antihyperglycemic drugs, he should start insulin
- Dental procedures may often reduce food intake and diabetics may go to hypoglycemia
- Dose adjustments may be required
Question 10. Gestational diabetes mellitus
Answer:
Gestational Diabetes Mellitus
- Gestational diabetes is defined as glucose intolerance that develops during pregnancy and usually cures after delivery
- Persons affected are
- Older women
- Obese/overweight women
- Women with a history of delivering large babies
- Women with a history of gestational diabetes
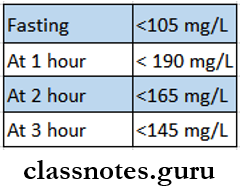
Gestational Diabetes Mellitus Diagnosis:
- All women during pregnane}7 should be screened based on random blood sugar tests in each trimester
- 50 mg oral glucose is administered and serum glucose is measured at 60 min
- If the glucose level is less than 140 mg, it is normal if not then the following step is taken
- 100 mg of glucose is administered and glucose in the fasting state is measured at 1,2 and 3 hours
- Deviation from normal levels indicates gestational diabetes
Normal Values:
Endocrine and metabolic disorders short answer
Question 11. Cushing’s syndrome
Answer:
Cushing’s Syndrome
- Cushing’s syndrome is caused by increased plasma glucocorticoid levels due to enhanced production of cortisol
Cushing’s Syndrome Clinical Features:
- Age- common in 3rd and 4th decades of life
- Females are more affected
- Obesity
- Truncal fullness
- Moon facies
- Buffalo hump
- Purple striae are seen on the abdomen
- Oligomenorrhoea and amenorrhoea
- Impotence in males
- Elevated blood pressure
- Muscle weakness
- Bone pain
- Decreased glucose tolerance
Cushing’s Syndrome Investigations:
- Screening test
- Determine free cortisol in urine
- Plasma ACTH measurement
- Plasma ACTH levels of more than 200-500 Pg per ml indicate Cushing’s syndrome
- Dexamethasone suppression test
- Plasma values above 5 microgram/100 ml suggest Cushing’s syndrome
Cushing’s Syndrome Treatment:
- Medical treatment
- Metyrapone- dose- 2-6 g per day in divided dose
- Aminoglutethimide-1-2 g per day
- Surgical treatment
- Pituitary irradiation
- Adrenalectomy
Question 12. Eye signs on thyrotoxicosis
Answer:
Eye Signs On Thyrotoxicosis
- Exophthalmos
- It means protrusion of the eyeball
- Spasm of the upper eyelid with lid retraction
- Proptosis with widening of the palpebral fissure
- Supraorbital and infraorbital swelling
- Congestion, edema, and chemosis of the conjunctiva
- Papilloedema
- Corneal ulceration
- External ophthalmoplegia
- Weakness of the extrinsic ocular muscles
- Other signs
- Von Giraffe’s sign
- When the patient is asked to look down, his upper eyelid fails to follow the rotation of the eyeball and thus lags behind
- Joffroy’s sign
- When the patient is asked to look upwards with the head fixed, there will be the absence of wrinkling on the forehead
- Moebius sign
- Failure of convergence of eyeballs
- Dalrymple’s sign
- Upper sclera is seen due to retraction of the upper eyelid
- Stellwag’s sign
- Absence of normal blinking
- Von Giraffe’s sign
