Question 1. Describe the etiology, clinical features, and management of tetanus.
Answer:
Tetanus:
- Tetanus is a disorder of neuromuscular excitability
Etiology:
- Etiology is caused by exotoxin, tetanospasmin liberated by clostridium tetani
Etiology Clinical Features:
- Trismus
- Dysphagia
- Risussardonicus- in it eyebrows and corners of the mouth are drawn up due to spasms of the muscles of the face and jaw
- Opisthotonus- rigidity of the muscles of the neck and trunk
- Elevation of temperature
- Rapid pulse
- Cyanosis
Endocrine and metabolic diseases long essays
Etiology Types:
- Acute tetanus
- The incubation period is less than 10 days
- Chronic tetanus
- The incubation period is about a month
- Delayed tetanus or latent tetanus
- In it organism remains latent for many years
- Local tetanus
- There is the presence of local contraction of muscles
- Cephalic tetanus
- There is irritation or paralysis of the cranial nerves
- Bulbar tetanus
- There is an extensive spasm of the muscles of deglutition and respiration
- Late tetanus
- The inoculation period is prolonged
- Tetanus neonatorum
- Recurrent tetanus
Read And Learn More: General Medicine Question and Answers
Etiology Management:
- Passive immunization
- 1 Lac units of Anti-tetanus serum is given half intravenously and half intramuscularly
- Antibiotics
- Penicillin injection of 10 lac units every 4 hours
- Metronidazole
- Tetracycline
- Wound care
- Thorough cleansing and debridement
- Removal of all necrotic tissues and foreign bodies
- All stitches are removed
- Blood clots, foreign bodies, and pus are cleared
- The wound should be left open
- The patient is isolated to a quiet, dark, and well-ventilated room
- Further treatment depends on the severity of the cases
- In mild cases
- Prozac in -200 mg IM
- Barbiturate, amylobarbitone, or injection diazepam-5-40 mg 4 times in a day
- In moderate cases
- Passage of nasogastric tube for feeding
- Passage of self-retaining catheter to drain the bladder
- Administration of intravenous fluid
- Maintenance of intake and output chart
- Tracheostomy
- In very severe cases
- Use of muscle relaxant, 40 mg turbo- marine initially 4 and then IM injections
- Tracheostomy
- Sedation with pentothal sodium
- Nasogastric feeding
- Elimination of visceral stimuli
- Intravenous administration of fluid and electrolytes
- Constant nursing
- In mild cases
Long essay on endocrine system disorders
Question 2. Describe the etiology and clinical features of acromegaly with special experience in dental problems.
Answer:
Acromegaly:
- Acromegaly occurs due to excess secretion of GH later in life after epiphyseal closure
Etiology:
- Pituitary adenoma
- Pancreatic islet cell tumors
- Hypothalamic tumors
- Bronchial carcinoid
- Small cell carcinoma of Hung
Acromegaly Clinical Features:
- Thick bones-larger hands and feet
- Enlarged skull
- Increased intracranial pressure
- Headache
- Photophobia
- Visual disturbances
- Hepatomegaly
- Cardiomegaly
- Osteoporosis
- Arthralgia
- Excessive sweating
- Myalgia
- Bowing of legs
- Barrel shaped chest
Acromegaly Oral Manifestations:
- Enlarged mandible
- Class 3 malocclusion
- Macroglossia
- Thick lips
- Proclination of teeth
- Hypercementosis
- Large nose, ears, and prominent eyebrows
- Periodontitis
- Enlargement of maxillary air sinuses
Metabolic diseases long answer questions
Question 3. Enumerate the proliferating factors, pathogenesis, investigations, and management of diabetic ketoacidosis.
Answer:
Diabetic Ketoacidosis:
- Diabetic Ketoacidosis is a complication of diabetes mellitus
Diabetic Ketoacidosis Proliferating Factors:
- Undetected or undiagnosed type 1 diabetes
- Stress
- Infection
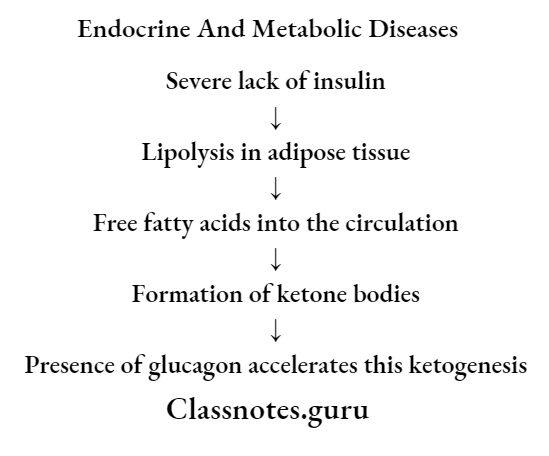
Diabetic Ketoacidosis Pathogenesis:
Diabetic Ketoacidosis Investigations:
- Diabetic ketoacidosis is confirmed by
- Hyperglycaemia
- Ketonaemia
- 1 leavy ketonuria
- Acidosis
Diabetic Ketoacidosis Management:
- Correction of hyperglycemia
- Administration of regular insulin 0.1 U/k bolus followed by 0.1 U/kg/ hour by ccontnousIV infusion till the patient recovers
- Correction of dehydration
- Normal saline infusion of 1 liter in the first hour
- Then 1 litre over the next 4 hours
- Then quantity is titrated
- Correction of acidosis
- Use of sodium bicarbonate
- Potassium
- 10-20 mEq/hour potassium chloride is added to the drip for rapid correction of hyperglycemia
Question 4. Classify diabetes mellitus. Discuss the complications and management of diabetes mellitus
Answer:
Diabetes Mellitus
- Diabetes mellitus is defined as a heterogeneous metabolic disorder characterized by the common feature of chronic hyperglycemia with disturbance of carbohydrate, fat, and protein metabolism
Diabetes Mellitus Classification:
- Primary diabetes
- Type 1- IInsulin-dependentdiabete mellitus
- IImmunemediated
- Nonimmune mediated
- Type 2- NNoninsulin-dependentdiabetes mellitus
- Obese
- Non-obese
- Type 1- IInsulin-dependentdiabete mellitus
- Secondary diabetes
- Pancreatic diabetes
- Hormonal or endocrinal abnormalities
- DDrug-inducedInsulin receptors antibodies
- Genetic syndromes
Diabetes Mellitus Complications:
- Acute metabolic complications
- Diabetic ketoacidosis
- Develop in patients with severe insulin deficiency
- Clinical Features:
- Nausea, vomiting, anorexia
- Deep and fast breathing
- Mental confusion
- Coma
- Hyperosmolar hyperglycaemia nonketotic coma
- It is a complication of type 2 diabetes mellitus
- Caused by severe dehydration which leads to sustained hyperglycemia diuresis
- Clinical Features:
- High blood sugar
- High plasma osmolality
- Thrombotic and bleeding complications
- Hypoglycaemia
- Develop in type 1 diabetes mellitus
- Clinical Features:
- Permanent brain damage
- Worsening of diabetic control
- Rebound hyperglycaemia
- Diabetic ketoacidosis
- Late systemic complications
- Atherosclerosis
- Common in both type 1 and type 2 diabetes mellitus
- Atherosclerosis may lead to
- Myocardial infarction
- Cerebral stroke
- Gangrene of toes and feet
- Diabetic microangiopathy
- It is the abasementmembrane thickening of small blood vessels and capillaries of different organs and tissues
- Occurs due to increased glycosylation of hemoglobin and other proteins
- Diabetic nephropathy
- It is a severe complication of diabetes mellitus
- Occurs in both types
- Features:
- Asymptomatic proteinuria
- Nephrotic syndrome
- Progressive
- Renal failure
- Hypertension
- Diabetic neuropathy
- Effects all parts of the nervous system
- Diabetic retinopathy
- It is the cause of blindness
- Other retinal complications include
- Glaucoma
- Cataract
- Corneal disease
- Infections
- Diabetic patients are more susceptible to infections like tuberculosis, pyelonephritis, otitis, carbuncles and diabetic ulcers
- Atherosclerosis
Diabetes Mellitus Management:
- Diet management
- The daily energy requirement for an individual is calculated according to age, weight, height, and activity
- Calorie requirement:
- For men- 36 kcal/kg
- For women-34 kcal/kg
- Lifestyle modification
- Physical exercise
- Reduction of weight
- Avoid alcohol and smoking
- Behavioural exercises
- Oral hypoglycaemic drugs
- Sulphonylureas
- Meglitinides
- Biguanides
- Thiazolidinedione derivatives
- Alpha-glucosidase inhibitors
- Insulin
Thyroid disorders long descriptive essay
Question 5. Discuss the complication of systemic ccorticosteroidtherapy with special reference to dental practice
Answer:
Complications Of Systemic Corticosteroids:
- Metabolic effects
- Mood changes from euphoria to depression
- Fluid retention and edema
- Hypertension
- Glucose intolerance
- Osteoporosis
- Increased susceptibility to infection
- Reactivation of latent tuberculosis
- Impaired wound healing
- Gastric erosions
- Masked perforation
- HHemorrhagefrom stomach and duodenum
- Suppression of hypothalamic-pituitary-adrenal axis
- It occurs with high-dose therapy
- This makes it difficult to withdraw steroids
Measures To Reduce Side Effects:
- Use of the lowest possible dose
- Administer on alternate days rather than daily
- Use of morning dose rather than any other time
- Use of steroids for established cases
- Monitor caloric intake to prevent weight gain and reduce sodium intake
- Use of H2 receptor blockers or proton pump inhibitors
- Provide high calcium intake and vitamin D
Question 6. Outline the conditions that produce pigmentation of oral mucosa. Discuss the clinical features of Addison’s disease.
Answer:
Causes Of Oral Pigmentation:
- Autoimmune adrenalitis
- Tubcrculousadrenalitis
- Bilateral adrenalectomy
- Drugs-ketoconazole
- Metastases in the adrenal
- Haemochromatosis
- Amyloidosis
- Histoplasmosis
Addison’s Disease:
- Addison’s Disease is due to progressive destruction of the three zones of the adrenal cortex and medulla with lymphatic infiltration
Oral Pigmentation Clinical Features:
- Glucocorticoid insufficiency
- Weight loss
- Nausea and vomiting
- Malaise
- Weakness
- Anorexia
- Diarrhea
- Constipation
- Postural hypotension
- Hypoglycaemia
- Mineralocorticoid deficiency
- Hypotension
- Loss of aandrogensReduction of pubic and axillary hair in females
- Increased ACTH secretion
- Pigmentation of exposed areas, pressure areas, mucous membranes, conjunctivae, and recently acquired scars
Adrenal gland disorders long essay
Question 7. Define hypo- and hyperthyroidism. Discuss clinical features, investigations, and treatment of hypothyroidism.
Answer:
Hyperthyroidism Definition:
- Hypothyroidism
- V is a clinical condition caused by low levels of circulating thyroid hormones
- Hyperthyroidism
- Hyperthyroidism is a clinical syndrome that results from exposure of the body tissues to excess circulating free thyroid hormones
Hypothyroidism Clinical Features:
- In new bom
- Cretinism
- Mental retardation
- Poor growth
- Difficult to nurse a baby
- Dwarfism
- During childhood or adolescence
- Juvenile hypothyroidism
- Child appears young
- Mental deficiency
- Abdominal distension
- Umbilical hernia
- Prolapse of rectum
- In adults
- Fatigue
- Weight gain
- Skin becomes thickened and puffy
- Muscle cramps
- Paraesthesia
- Impaired speech
- Reduced cardiac output
- Elevation of blood pressure
- Shortness of breath
- Abdominal distension
- Aches and pains
- Anaemia
- Alopecia
- Menorrhagia, infertility
- Constipation
Hypothyroidism Investigations:
- Serum T3 and T4 levels- low
- Serum TSH- high
- Thyroid peroxidase antibodies- present
- Serum cholesterol triglyceride- high
- ECG- shows bradycardia, low amplitude of QRS, and ST-T changes
- Blood- macrocytic anemia
- X-ray chest- shows cardiomegaly
- Photomtogram- delayed ankle jerk
Hypothyroidism Treatment:
- Replacement of thyroid hormones by L-thyroxine
- Initial starting dose-50-100 micrograms daily as a single dose empty stomach in the morning for the first 3-4 weeks
- The dose is increased to 150 micrograms daily
- The maximum dose is 300 micrograms in a day
- In older persons or persons with ischaemic heart disease, a low dose of L-thyroxine 25 microgram/day is started and gradually increased
Pituitary diseases long answer question
Question 8. Discuss the etiology, clinical features, and management of thyrotoxicosis. Mention a note on thyroid function tests
Answer:
Thyrotoxicosis is a syndrome resulting from an increased level of free thyroxin
Thyrotoxicosis Clinical Features
- Hyperactivity
- Irritability
- Heat intolerance
- Palpitations
- Fatigue
- Weakness
- Weight loss
- Increased appetite
- Tachycardia
- Systolic hypertension
- Presence of tremors
- Cardiac arrhythmias
- Excessive sweating
- Exophthalmos
Thyrotoxicosis Management:
- General management
- Rest
- Nutritious diet
- Drug therapy
- Carbimazole
- Initial dose of 30 nag/ day, maintenance dose of 10-20 mg/day is given
- Potassium perchlorate – 800 nag/day in divided doses
- Sodium or potassium iodide 6-10 nag/day
- Surgical treatment
- Subtotal thyroidectomy
- Radioiodine treatment
- Iodine is given in ddosesof 8-10 millicuries
Thyroid Function Tests:
- Measurement of radioactive iodine uptake
- The normal value is 30%
- Higher values indicate thyrotoxicosis
- It is no longer used because of
- Lack of sensitivity
- Lack of specificity
- Time-consuming
- Complicated procedures
- Measurement of total T3 and T4 in blood by radioimmunoassay
- Widely used
- Normal Values:
- Serum T3 total- 70-200 ng/1
- Serum T4 total- 5.5-13.5 microgram/1
- Drawbacks:
- Measure the total amount of hormone
- Gets changed with the fluctuations in their binding protein
- Measurement of free T3 and T4 in blood
- NORMAL VALUES
- Serum free T3-1-2.6 nmol/1
- Serum free T4-10-27 nmol/1
- Estimation of TSH
- Normal value- 0.15-3.5 mIU/1
- High levels of ooccurin primary hypothyroidism
- Low levels ooccurin hyperthyroidism and hypopituitarism
- Ultrasound of thyroid
- Measure the size and mass of the thyroid
- Detects shape and nodularity of thyroid
- Thyroid scan
- It is used to detect functioning and nonfunctioning nodules in the thyroid
- I131 or 99mTc is used for
- Antithyroid antibodies
- Detects autoimmune thyroid disorders
- Stimulating antibodies and TSH receptor-blocking antibodies are raised in Grave’s disease
- Needle biopsy of thyroid
- Detects malignancy
Parathyroid gland disorders long essay
Question 9. Discuss ethetiology, clinical features, and management of myxoedema
Answer:
Myxoedema:
- Myxoedema indicates severe hypothyroidism
Etiology:
- Primary causes
- Spontaneous atrophic hypothyroidism
- Iodine deficiency
- Following 1131 therapy
- Post thyroidectomy
- Hashimoto’s thyroiditis
- Radiation
- Secondary causes
- Destruction of the pituitary gland
- Post-surgery
- Post radiation
- Tumour
- Disorders of hypothalamus
Myxoedema Clinical Features:
- General symptoms
- Age and sex- Middle-aged males are frequently affected
- Weakness
- Fatigue
- Lethargy
- Low blood pressure
- Mental retardation
- Dry coarse skin
- Swelling of the face and extremities
- Cold intolerance
- Husky voice
- Decreased sweating
- Anorexia
- Loss of memory
- Hearing impairment
- Arthralgia
- Muscle cramps
- Paraesthesia
- Oral manifestations
- Peri-orbital puffiness
- Loss of facial hair
- Swollen tongue, lips, and eyelids
- Difficulty in speech
- Underdevelopment of maxilla and mandible
Myxoedema Management:
- Replacement of thyroid hormones by L-thyroxine
- Initial starting dose-50-100 micrograms daily as a single dose empty stomach in the morning for the first 3-4 weeks
- The dose is increased to 150 micrograms daily the maximum dose is 300 micrograms every day
- In older persons or persons with ischaemic heart disease, a low dose of L-thyroxine 25 microgram/day is started and gradually increased
Disorders of growth and metabolism long essay
Question 10. Describe etiology, clinical features, diagnosis, and treatment of hyperthyroidism.
Answer:
Hyperthyroidism:
- Hyperthyroidism is a clinical syndrome that results from exposure of the body tissues to excess of circulating free thyroid hormones
Etiology:
- Common
- Grave’s disease
- Toxic nodular goitre
- Multinodular
- Solitary nodule
- Less common
- Thyroiditis
- Drug-induced
- Self-induced
- Iodine excess
- Rare causes
- Pituitary or ectopic TSH
- Thyroid carcinoma
Hyperthyroidism Clinical Features:
- Goitre
- Gastrointestinal symptoms
- Weight loss
- Diarrhea
- Vomiting
- Cardiovascular symptoms
- Sinus tachycardia
- Exertional dyspnoea
- Arrhythmias
- Precipitation of angina
- Neuromuscular symptoms
- Nervousness, irritability
- Restlessness
- Tremors of hands
- Muscular weakness
- Exaggerated tendon reflexes
- Dermatological symptoms
- Increased sweating
- Clubbing of fingers
- Loss of hairs
- Redness of palms
- Reproductive symptoms
- Menstrual irregularity
- Abortions
- Infertility
- Loss of libido
- Ophthalmological
- Lid retraction
- Wide palpebral fissures
- Exophthalmos
- Diplopia
- Excessive watering of eyes
- Miscellaneous
- Heat intolerance
- Excessive thirst
- Fatigue
- Oral manifestations
- Early exfoliation of deciduous teeth
- Premature eruption of permanent teeth
- Alveolar bone atrophy
- Increased susceptibility to oral infections
Hyperthyroidism Diagnosis:
- T3 and T4 levels- elevated
- TSH levels- low
- 131I uptake is increased
- Serum cholesterol level- low
- ECG changes- shows tachycardia, arrhythmias, ST- T changes
- USG- shows diffuse goitre
- Increased BMR
- Decreased urinary excretion of iodine
Hyperthyroidism Treatment:
- Drug therapy
- Anti-thyroid drugs
- Carbimazole
- Propylthiouracil -100-150 mg
- Beta-blockers
- Propanolol-80-160 mg daily
- Metoprolol-50 mg/ day
- Anti-thyroid drugs
- Radioactive ablation of thyroid
- Subtotal thyroidectomy
- Treatment of relapse
- Long-term drug therapy is used
- Radioactive iodine therapy
- Management of ophthalmopathy
- Use of 60 mg of prednisolone daily
- Management of dermopathy
- Local betamethasone ointment or triamcinolone injection may be used
Obesity and metabolic syndrome long essay
Question 11. What are the causes of hypocalcemia? Describe clinical features and outline the treatment of tetany
Answer:
Hypocalcaemia:
- Hypocalcaemia is a condition of low levels of calcium
Causes Of Hypocalcaemia:
- Sepsis
- Burns
- Acute pancreatitis
- Acute renal failure
- Alkalosis
- Drugs like diuretics, protamine, heparin, and glucagon
- Toxic shock syndrome
- Hypomagnesaemia
- Plasmapheresis
- Extensive transfusion
- Malignancy
Tetany:
- Tetany is a clinical condition characterized by low levels of ionized calcium leading to increased neuromuscular excitability
Tetany Clinical Features:
- In children
- Characteristic triad- carpopedal spasm, stridor and convulsion
- Carpopedal spasm- flexion at metacarpophalangeal joints and extension at interphase- large joints with other position of the thumb
- Stridor- closure of the glottis
- In adults
- Tingling sensation in peripheral parts of limbs or around the mouth
- Painful carpopedal spasm
- Rarely stridor and convulsions
- Signs
- Trousseau’s sign
- Raising the blood pressure above systolic level by inflation of the sphygmomanometer cuff produces carpal spasm within 3-5 minutes
- Chvostek’s sign
- A tap at the facial nerve at an angle of the aw produces twitching of facial muscles
- Trousseau’s sign
Tetany Treatment:
- Treatment of hypocalcemia
- Injection of 20 ml of 10% calcium gluconate
- Treatment of alkalosis
- Intravenous administration of isotonic saline
- Withdrawal of alkalies
- Inhalation of 5% CO2in oxygen- to treat hyperventilation
- Psychotherapy
