Disorders Of Red Blood Cells Important Notes
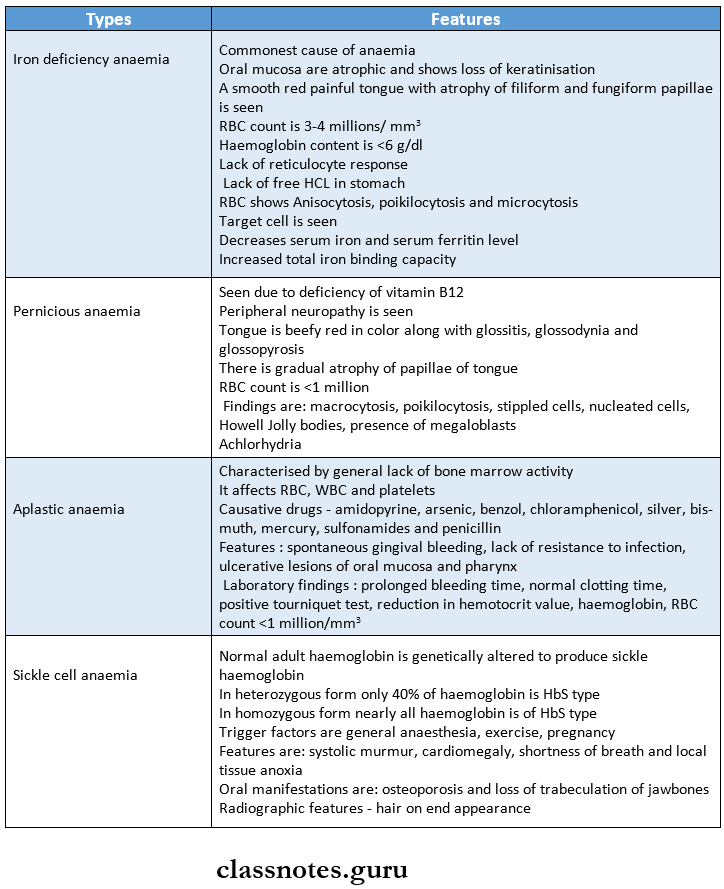
1. Types of Anaemia
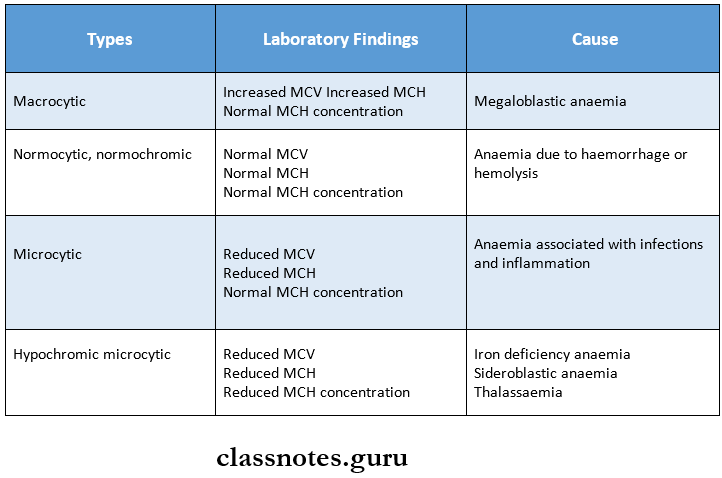
2. Morphological types of anaemia
3. Triad of Plummer-Vinson syndrome
- Iron deficiency anaemia
- Koilonychia or spoon-shaped nails
- Hysteric dysphagia
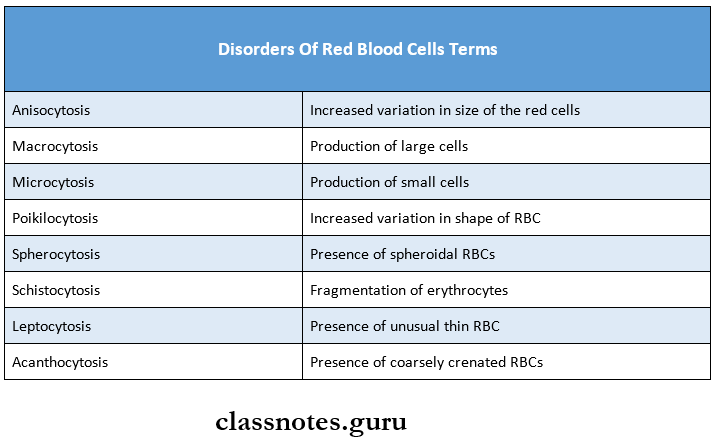
4. Disorders Of Red Blood Cells Terms
5. Thalassaemia
- α-thalassaemia is due to deficient synthesis of α chain
- β-thalassaemia is due to deficient synthesis of β chain
- heterozygous form of thalassaemia is called thalassaemia minor
- The homozygous form of thalassaemia is called thalassaemia major
Thalassaemia Features:
- Occurs within the first two years of life
- Siblings are commonly affected
- Present as
- Hypochromic and microcytic anaemia
- Prominent cheekbones
- Depression of nasal bridge
- Prominent premaxilla
- Protrusion of maxillary anterior teeth
Read And Learn More: Pathology Question And Answers
- Laboratory findings
- Target cells, safety-pin cells and normoblasts are seen
- Poikilocytosis, Anisocytosis present
- Elevated serum bilirubin level
- Bone marrow shows large immature RBC
- Radiographic findings
- Crew-cut or hair-on-end appearance on the surface of the skull
- Salt and pepper appearance of trabeculae pattern of maxilla and mandible
6. Hormones essential for RBC production
- Erythropoietin
- Androgens
- Thyroxine
7. Metals essential for RBC production
- Iron
- Cobalt
- Manganese
8. Vitamins essential for RBC production
- Vitamin B12
- Vitamin C
- Vitamin B6
- Vitamin E
- Vitamin B2
9. Types of haemoglobin
- Adult haemoglobin – HbA
- Consists of 2 alpha chains and 2 beta chains
- Fetal haemoglobin – HbF
- Consists of 2 alpha chains and 2 gamma chains
Disorders Of Red Blood Cells Long Essays
Question 1. Define and classify anaemia. Describe labora¬tory diagnosis and Clinical features of iron deficiency Anaemia.
Answer:
Anaemia: Anaemia is defined as haemoglobin concentration in blood below the lower limit of the normal range for the age and sex of the individual.
In an adult male 13 g/dl and for females 11.5 g/dl is taken as the lower lift of the normal haemoglobin range.
Classification of anaemias:
- Pathophysiologic:
- Anaemia due to increased blood loss
- Acute post-haemorrhagic anaemia
- Chronic blood loss
- Anaemias due to impaired red cell production
- Cytoplasmic maturation defects
- Deficient haem synthesis: Iron deficiency anaemia
- Deficient globin synthesis: Thalassaemic syndromes
- Nuclear maturation defects
- Vitamin B12 and/or folic acid deficiency: Megaloblastic anaemia
- Defects in stem cell proliferation and differentiation
- Aplastic anaemia
- Pure red cell aplasia
- Anaemia of chronic disorders
- Bone marrow infiltration
- Congenital anaemia
- Cytoplasmic maturation defects
- Anaemias due to increased red cell destruction [Haemolytic anaemias).
- Extrinsic (extracorpuscular) red cell abnormalities
- Intrinsic (intracorpuscular) red cell abnormalities
2. Morphologic:
- Microcytic, hypochromic
- Normocytic, normochromic
- Macrocytic, normochromic
Iron deficiency anaemia:
- Commonest nutritional deficiency disorder.
- Iron is mainly available from a diet rich in meat, liver, beans and green vegetables.
- Milk is a poor source of iron.
- The daily iron requirement is 1 mg in males and 2 mg in females.
- Absorption of iron is facilitated by the presence of acid in the stomach and vit. C, while antacids and calcium phosphates decrease it.
Anaemia Laboratory diagnosis:
- Serum iron and ferritin are low.
- Total iron binding capacity is increased
- Transferrin saturation is below 16%.
- Stool examination for parasites and occult blood is useful.
- Endoscopic and radiographic examination of the GI tract is needed to detect the source of bleeding.
Haematological findings: Examination of peripheral blood picture.
- Size: Microcytic anisocytosis
- Chromicity: Anisochromia is present.
- Shape: Poikilocytosis is often present, pear-shaped tailed variety of RBC, elliptical form common.
- Reticulocytes: Present, either normal / reduced
- Osmotic fragility: Slightly decreased
- ESR: Seldom elevated
- Absolute value: MCV, MCH and MCHC are reduced.
Bone marrow findings:
- Marrow cellularity – increased due to erythroid hy¬poplasia micronormoblast
- Marrow iron-reduce reticuloendothelial iron stores and absence of siderotic iron granules from developing normoblasts.
Anaemia Clinical Features:
1. Anaemia:
- Usual symptoms are weakness, fatigue, dyspnoea on exertion, palpitations, pallor of skin, mucous membranes and sclera.
- Older patients may develop angina and congestive cardiac failure.
- Women-menorrhagia is a common symptom.
2. Epithelial tissue changes:
- Nails (koilonychia or spoon-shaped nails)
- Tongue (Atrophic glossitis)
- Mouth (angular stomatitis)
Question 2. Describe in detail clinical fea¬tures, peripheral blood smear and bone marrow findings in megaloblastic anaemia.
Answer:
Megaloblastic anaemia Clinical Features:
- Aneamia,
- Glossitis,
- Neurological manifestations –
- Numbness,
- paraesthesia,
- weakness,
- Ataxia, dimihinshed reflexes.
- Others- mild jaundice,
- Angular stomatitis, purpura, malabsorption, Anorexia.
1. Blood picture:
- Haemoglobin concentration- falls.
- MCV and MCH increases
- MCHC decreases/remains normal,
- Reticulocyte count – is low
- Red blood cells – blood smear demonstrates aniso- cytosis, poikilocytes and presence of macroscale-cytes
- Leucocytes – total WBC count is less than c Thrombocytes – giant platelets are present.
2. Bone marrow findings:
- Marrow cellularity – hypercellular bone marrow with decreased myeloid: erythroid ratio,
- Erythropoiesis – erythroid hyperplasia is due to characteristic megaloblastic erythropoiesis.
- Megaloblasts are abnormal, large, nucleated erythroid precursors, having nuclear cytoplas¬mic asynchrony. Nuclei are large, having fine re¬ticular and open chromatin,
- Abnormal mitosis may be seen in megaloblasts.
- Marrow iron – increase in the number and size of the iron granules in erythroid precursors. Iron in reticulum cells is increased.
Disorders Of Red Blood Cells Short Essays
Question 1. Sings and Symptoms of Anaemia
Answer:
Signs and symptoms of anaemia :
- CNS: Faintness, giddiness, headache, tinnitus, drowsiness, numbness, and tingling sensations of hands and feet.
- Cardiovascular system: Hyperdynamic circulation may be present with tachycardia, collapsing pulse, cardiomegaly, and dyspnoea, in elderly with congestive heart failure.
- Gastrointestinal system: Nausea, constipation, weight loss, anorexia, flatulence.
- Renal system: Mild proteinuria.
- Ocular: Retinal haemorrhages if there is associated vascular disease.
- Reproductive system: Menstrual disturbances such as menorrhoea and menorrhagia, loss of libido.
- General: Pallor (of mucous membranes, conjunctiva, skin), tiredness, weakness, easy fatiguability, leth¬argy, headache).
Disorders Of Red Blood Cells Short Question And Answers
Question 1. ESR
Answer: If a sample of blood with an anticoagulant is allowed to stand in a vertical tube, the RBC settles down due to gravity as compared to plasma with a clear supernatant layer of plasma. The rate at which the cells settle down is called ESR.
Method of Estimation of ESR:
- There are two standard methods as follows:
- Wintrobe’s and Landsberg’s method: ESR is meas-ured in undiluted blood in a haematocrit tube.
- Westergren’s method: ESR is measured in venous blood diluted accurately with 31.3 g/L trisodium cit¬rate in the proportion of 1:4 (1 volume of 3.8% so¬dium citrate and 4 volume of blood).
- The conditions were ESR is markedly raised are as follows:
- Infective: Tuberculosis, kala-azar, in most of chronic infections.
- Inflammation: Rheumatoid arthritis, rheumatic fever, other connective tissue disorders.
- Neoplastic: Multiple myeloma, lymphoma, parapro- anaemia.
- Miscellaneous: Aplastic anaemia, autoimmune disorders, mixed connective tissue disorders.
Question 2. Thalassemia
Answer:
- Thalasemia are hereditary disorder characterized by quantitative abnormalities of globin chain synthesis, i.e., reduce production of globin chains.
- Reduction in alpha chain synthesis leads to alpha thalassemia and that of the beta chain leads to beta thalassemia.
- Beta thalassemia major (Cooley’s anaemia) is a severe disease and manifests in childhood. This condition is transfusion dependent and generally fatal by 30 years of age.
- Beta thalassemia minor is a mild disease, nontransfusion dependent and patients can live full normal lives.
Thalassemia Clinical features:
- The important clinical manifestations are anaemia, re-current mild jaundice and hepatosplenomegaly.
- The family history may be positive.
- Expansion of bones.
- Iron overload due to repeated blood transfusion.
Thalassemia Laboratory findings:
Tests such as
- Haemoglobin electrophoresis,
- Decreased osmotic fragility,
- Amniocentesis and chorionic villi biopsy are performed for prenatal diagnosis in inherited conditions like thalassemia.
Thalassemia Treatment:
- Supportive treatment in the form of packed cell transfusion may be needed. However, repeated transfusion may lead to iron overload which in turn may require treatment with chelating agents, deferoxamine. Folic acid, 5 mg daily is given to meet the increased demand.
- Bone marrow transplantation is curative in thalassemia.
Question 4. Aplastic anaemia
Answer:
Aplastic anaemia is characterized by
- Anaemia
- Leukopenia
- Thrombocytopenia
- Hypocellular bone marrow
Aplastic anaemia Etiology:
- Idiopathic
- Secondary to drugs, viruses, pregnancy
- Hereditary
Aplastic anaemia Clinical Features:
- Anaemia
- Excessive tendency to bleed
- Easy bruising
- Epistaxis
- Gum bleeding
- Heavy menstrual flow
- Petechiae
- Predisposition to infections
Aplastic anaemia Investigations:
- Blood smear- shows normocytic, microcytic anaemia, decreased granulocytes and platelet count
- Chromosomal studies for inherited disorders
Aplastic anaemia Treatment:
- Bone marrow transplantation
- Immunosuppressive therapy
- Packed red cell transfusions
- Granulocytes transfusions
Question 5. Pernicious anaemia
Answer:
- Also known as Addisonian megaloblastic anaemia.
- Pathogenesis – an autoimmune reaction against gastric parietal cells that causes atrophy of gastric mucosa.
- About 2 – 3% of cases of pernicious anaemia develop carcinoma of the stomach.
Pernicious anaemia Lab Diagnosis:
- Hyper gastrinemia,
- Biochemical tests reveal serum bilirubin,
- LDH, Hb, ferritin and iron.
- Hematologic findings in blood and bone marrow are the same as those of megaloblastic anaemia.
Pernicious anaemia Treatment:
- Parenteral Vit. B12 replacement therapy
- Symptomatic and supportive therapy such as physiotherapy for neurologic deficits and occasionally blood transfusion.
Question 6. PCV
Answer: Packed cell volume is defined as the ratio of the volume of RBCs to that of whole blood and is expressed as a percentage Also called as haematocrit.
Methods of estimation of PCV:
- Macro (Wintrobe’s) method: Blood is centrifuged for half an hour at 3000 rpm.
- Micro haematocrit method: Using a capillary tube, blood is centrifuged at 12,5000 rpm.
- Electronic method: Employ automated counters, where the derivation of RBC count, PCV, and MCV are closely interrelated.
Three layers are observed after centrifugation.
- Plasma layer: Top most, clay yellow/straw coloured.
- Buffy coat: Middle layer of WBC and platelets about 1 mm thick.
- Column of RBC: Bottom layer.
- Increased buffy coat: Severe degree of leucocyte- sis/leukaemia.
- Colour of plasma layer:
- Red colour – Haemolysis,
- Yellow colour – jaundice.
- Diseases causing raised PCV:
- Polycythaemia,
- Burns,
- Shock
- Dehydration due to severe vomiting, diarrhoea,
- Profuse sweating.
- Diseases causing low PCV:
- Anaemia,
- Pregnancy.
Question 7. Sickle cell anaemia
Answer:
- Sickle cell haemoglobin is produced due to substitution of valine for glutamine at the 6th position of a beta-globin chain of normal adult haemoglobin. (HbA).
- In heterozygous form – 40% of Hb is HbS,
- In homozygous – 100% of Hb is HbS (Individual suffers from sickle cell anaemia).
Sickle cell anaemia Clinical features:
- Severe haemolytic anaemia.
- Impaired growth and development, increased susceptibility to infectious.
- The distorted shape of sickle cells blocks blood circulation and causes repeated vaso-occlusive episodes.
- Oral findings – generalised osteoporosis, loss of tribe- collation of jawbones.
- Radiographic findings – hair on end appearance OR skull, tower-shaped skull, generalised osteoporosis, enlarged medullary cavities.
Sickle cell anaemia Lab findings:
- Anaemia, a positive sickling test,
- Sickle cells and target cells are seen on blood film.
Question 8. Megaloblastic anaemia
Answer:
- Megaloblastic anaemias are disorders caused by impaired DNA synthesis and are characterised by a distinc¬tive abnormally in the haematopoietic precursors in the bone marrow in which the maturation of the nucleus is delayed relative to that of the cytoplasm.
- Defective DNA synthesis due to deficiency of Vit Biz/folic acid (folate)
Megaloblastic anaemia Treatment: Hydroxycobalamin IM injection 1000 micro¬gram for 3 weeks, oral folic acid tablets daily for 4 months.
Question 9. Hereditary spherocytosis
Answer:
- Hereditary spherocytosis is a common type of hereditary haemolytic anaemia in which red cell membrane is abnormal.
- It is inherited as an autosomal dominant disorder.
- Pathogenesis: Deficiency in the structural protein of the red cell membrane spectrin.
- Clinical features: Anaemia, jaundice, splenomegaly and pigmented gall stones.
- Laboratory findings.
- Anaemia and reticulocytosis
- Rlnnd film shows mirrosnherorvtps.
- Osmotic fragility
- Negative direct Coomb’s test
- Spontaneous auto haemolysis.
Question 10. Lab diagnosis of anaemia
Answer: Laboratory diagnosis of anaemia includes
- Peripheral blood smear
- It shows
- Variations in size of RBCs- microcytic or macrocytic
- Variations in the shape of RBCs- poikilocytosis
- Spherocytosis- spindle-shaped RBCs
- Nucleated RBCs
- Inadequate haemoglobin formation
- Presence of Howell-Jolly bodies
- Irregularly contracted red cells
- It shows
Haemoglobin content: Haemoglobin content decreases in anaemia
- Red cell indices are used like MCV, MCH, MCHC
- ESR estimation
- Bone marrow aspiration
- Leucocyte and platelet count
- Reticulocyte count
Question 11. Hemosiderin
Answer: Hemosiderin is formed by aggregates of ferritin
Hemosiderin Microscopic Appearance:
- Appears as golden yellow to brown granular pigment
- Seen within the mononuclear phagocytes of the bone marrow, spleen and liver
Hemosiderin Pathological Conditions:
- Excessive hemosiderin occurs in
- In the presence of excessive breakdown of red cells
- During systemic overload of iron
- Thalassaemia
- Sideroblastic anaemia
- Alcoholic cirrhosis
- Multiple blood transfusions
Hemosiderin Effects:
- Black eye
- Brown induration in lungs
- Parenchymatous deposition of hemosiderin
- Reticuloendothelial deposition
Question 12. Pancytopenia.
Answer: It is the simultaneous presence of anaemia, leucopenia and thrombocytopenia.
Pancytopenia Causes:
- Aplastic anaemia,
- Paroxysmal nocturnal haemoglobinuria
- Megaloblastic anaemia.
- Bone marrow infiltrations.
Question 13. Beta thalassemia major.
Answer: It is stated with either a complete absence of beta chain synthesis or only a small amount of beta chains are formed
Beta thalassemia major Clinical Features:
- Cooley’s anaemia
- Bony expansion
- Hepatosplenomegaly
- Retarded growth
- Delayed puberty
- Diabetes Mellitus
- Damage to the liver and heart
Pancytopenia Treatment:
- Repeated blood transfusion
- Use of folic acid supplements
- Chelation therapy
- Bone marrow transplantation
