Diseases Of Thyroid And Parathyroid Glands Important Notes
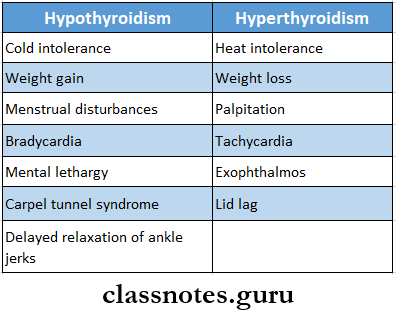
- Hyperthyroidism And Hypothyroidism
- Goitre
- It is the enlargement of the thyroid gland irrespective of its cause
- Goitre Classification
- Simple goitre
- Diffuse hyperplastic goitre
- Nodular goitre
- Colloid goitre
- Toxic goitre
- Diffuse toxic goitre
- Toxic nodular goitre
- Toxic nodule
- Neoplastic goitre
- Benign tumours
- Malignant tumours
- Thyroiditis
- Autoimmune
- Subacute
- Reidel’s thyroiditis
- Other rare causes
- Simple goitre
- Goitre Treatment
- Addition of iodide
- Discontinuation of offending drug
- Administration of thyroxin
- Surgical treatment for cosmetic purposes
- Retrosternal Goitre
- Mainly derived from the lower pole of the multinodular goitre
- Retrosternal Goitre Classification
- Substernal
- Plunging
- Intra-thoracic
- Retrosternal Goitre Treatment – resection
- Thyrotoxicosis Or Toxic Goitre
- Thyrotoxicosis Or Toxic Goitre Causes
- Grave’s disease
- Toxic multinodular goitre
- Toxic adenoma
- Other rare causes
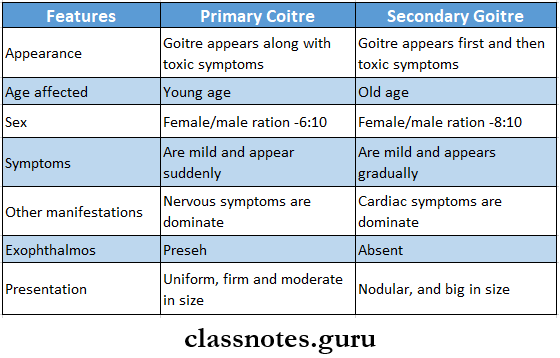
- Thyrotoxicosis Or Toxic Goitre Types
- Primary toxic goitre / Grave’s diseases
- Secondary toxic goiter
- Thyrotoxicosis Or Toxic Goitre Causes
- Thyroid Carcinoma
Diseases of thyroid and parathyroid question and answers
Diseases Of Thyroid And Parathyroid Glands Long Essays
Question 1. Describe clinical features, diagnosis and management of carcinoma of the thyroid.
Answer:
Thyroid Carcinoma is classified into four types:
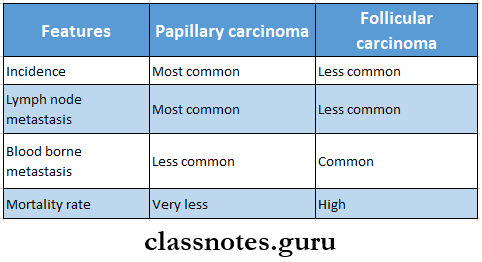
- Follicular Carcinoma:
- Follicular Carcinoma Clinical Features:
- Occurs in old age
- Common in females
- An asymptomatic slow-enlarging thyroid nodule is present
- Regional lymph nodes are involved
- Pain is present
- It invades adjacent structures
- Distant metastasis occurs
- Follicular Carcinoma Treatment:
- Low-grade carcinoma- treated by thyroid lobectomy
- If regional lymph nodes are involved- Dissection of lymph nodes
- Suppressive thyroid hormone therapy
- Aggressive follicular carcinoma- Treated by near-total thyroidectomy and postoperative radiotherapy
- Follicular Carcinoma Clinical Features:
- Papillary Carcinoma
- Papillary Carcinoma Clinical Features:
- Occurs at any age
- Common in females
- Slow growing tumour
- Tends to become malignant
- Asymptomatic nodules appear within the thyroid gland
- Regional lymph nodes are enlarged
- Papillary Carcinoma Treatment:
- Surgical excision
- Near Total thyroidectomy
- Suppressive dose of thyroid hormone post-operatively
- Papillary Carcinoma Clinical Features:
- Medullary Carcinoma:
- Arises from parafollicular C cells
- Medullary Carcinoma Types:
- Sporadic
- Familial variety
- Medullary Carcinoma Clinical Features:
- Associated with mucocutaneous neuroma
- It is present as a solid, hard, nodular tumour
- Medullary Carcinoma Treatment:
- Near total thyroidectomy
- Radical block dissection of lymph nodes
- Anaplastic Carcinoma:
- Age- Over 50 years of age o Enlarged thyroid occurs
- Gland is fixed
- Consistency is hard to firm
- Anaplastic Carcinoma Treatment:
- Total thyroidectomy with modified neck dissection
- Tracheostomy
- External irradiation
- Anaplastic Carcinoma Treatment:
Read And Learn More: General Surgery Question and Answers
Question 2. Describe clinical features, diagnosis and management of primary thyrotoxicosis.
Answer:
Primary Thyrotoxicosis Clinical Features:
- Common in females a Loss of weight
- Increased smooth muscle activity
- Intolerance to heat
- Fine tremors
- Excitability
- Hyperkinetic movements
- Excessive sweating
- Raised pulse rate
- Diarrhoea
- Polyuria
- Hot moist palms
- Systolic hypertension
- Exophthalmos
- Moebius sign- loss of convergence of eyeball
- Stell Wag’s sign- infrequent blinking
- Von Giraffe’s sign-lid lag sign
Primary Thyrotoxicosis Diagnosis:
- Thyroid function tests- elevation of T3, T4 and decrease in TSH levels
- Thyroid scan
- Ultrasound- for the search of cysts
Primary Thyrotoxicosis Management:
- To restore the patient to the euthyroid state
- Antithyroid drugs
- Carbimazole-10 mg 6th hourly for 2-3 weeks
- Propranolol-10-20 mg, two-three times a day
- Lugol’s iodine-10-12 drops three times a day
- Potassium perchlorate- 20 mg three times a day
- Antithyroid drugs
- To reduce the functioning of thyroid mass
- Subtotal thyroidectomy
- Radio-iodine therapy
- To minimize complications
- Proper anaesthetic measures
- Good post-operative care
Important thyroid gland questions for exams
Question 3. Discuss Grave’s disease in detail.
Answer:
Grave’s Disease: It is a diffuse goitre affecting the whole functioning thyroid tissue, causing hypertrophy and hyperplasia due to abnormal thyroid stimulants
Grave’s Disease Etiology
- It is a systemic autoimmune disease
- It is hereditary
- Another causative factor is emotional disturbances
Grave’s Disease Clinical Features: It consists of a classical triad
- Grave’s Disease Goitre
- Characterised by an enlarged thyroid gland
- On palpation, the gland is smooth and irregular
- Bruit is heard
- Extreme vascularity is present.
- Grave’s Disease Thyrotoxicosis
- Common in females
- Loss of weight
- Increased smooth muscle activity
- Intolerance to heat
- Fine tremors
- Excitability
- Hyperkinetic movements
- Excessive sweating
- Raised pulse rate
- Diarrhoea
- Polyuria
- Hot moist calms
- Systolic hypertension
- Grave’s Disease Exophthalmos
- It means oro tarsi on of eyeball
- Spasm of the upper eyelid
- Proptosis with the widening of the palpebral fissure
- Supraorbital and infraorbital fissure
- Congestion and edema of the conjunctive
- Corneal ulceration
Grave’s Disease Investigations:
- Thyroid function tests
- T3 T4 levels are high
- TSH levels are low
- Presence of thyroid autoantibodies
Grave’s Disease Management
- To restore the patient to the euthyroid state
- Antithyroid drugs
- Carbimazole- 10 mg 6th hourly for 2-3 weeks
- Propranolol-10-20 mg two-three times a day
- Lugol s iodine- 10-12 drops three times a day
- Potassium perchlorate- 20 mg three times a day
- Antithyroid drugs
- To reduce the functioning of thyroid mass
- Subtotal thyroidectomy
- Radio-iodine therapy
- To minimize complications
- Proper anaesthetic measures
- Good post-operative care
Question 4. Classify thyroid tumours. Discuss etiopathology.
Answer:
Thyroid Tumours Classification
- Benign tumours
- Adenoma
- Follicular adenoma
- Papillary adenoma
- Adenoma
- Malignant tumours
- Follicular cell origin
- Differentiated tumours
- Papillary carcinoma
- Follicular carcinoma
- Mixed papillary and follicular carcinoma
- Undifferentiated tumours
- Anaplastic carcinoma
- Differentiated tumours
- Parafollicular cell origin
- Medullary carcinoma
- Non-thyroid cell origin
- Malignant lymphoma
- Sarcoma
- Metastatic carcinoma
- Follicular cell origin
Differentiated Thyroid Tumours:
- Differentiated thyroid tumours are:
- Papillary carcinoma
- Follicular carcinoma
Thyroid Tumours Etiology:
- Iodide deficiency
- External irradiation
- Ionizing radiation
- Autoimmune thyroiditis
Thyroid and parathyroid disorders solved questions
Question 5. Describe the etiopathology, clinical features and treatment of solitary nodules in the thyroid gland.
Answer:
Solitary Nodule In Thyroid Gland: It can be classified into benign and malignant nodules
Solitary Nodule In Thyroid Gland Etiopathogenesis:
- Thyroiditis
- Follicular adenoma
- Carcinoma
- Thyroid cyst
- Colloid nodules
Solitary Nodule In Thyroid Gland Clinical Features:
- Age-20-40 Years of age
- Sex- common in females
- Stridor
- Tracheal deviation
- Neck vein engorgement
- Dyspnoea
- Dysphagia
- The solitary nodule is present
Solitary Nodule In Thyroid Gland Treatment:
- Excision of solitary nodule along with a margin of normal thyroid tissue
- If the nodule is present at the junction of the isthmus and lobe- hemithyroidectomy is done
- In the presence of malignancy- immediate total thyroidectomy is done
Question 6. Discuss clinical features and treatment of multinodular goitre. Mention four complications of it.
Answer:
Multinodular Goitre: Multinodular goitre is the end-stage result of diffuse hyperplastic goitre
Multinodular Goitre Clinical Features:
- Age- 40-60 years of age
- Sex- common in females
- Exophthalmos rarely occurs
- The presence of long-standing swelling in front of the neck
- Dyspnoea
- Dysphagia
- The gland is firm and irregular
Multinodular Goitre Treatment:
- Total or near-total thyroidectomy
- It is widely used to
- Avoid nerve injury
- Avoid recurrence
- Subtotal thyroidectomy
- In it, parts of the right and left lobes are removed along with the isthmus
- It avoids right laryngeal nerve paralysis and hypothyroidism
- It is widely used to
Multinodular Goitre Complications:
- Calcification
- Sudden haemorrhage
- Dyspnoea
- Secondary thyrotoxicosis with CVS involvement- called Plummer’s disease
- Development of follicular carcinoma
hyroid and parathyroid viva questions
Question 8. Discuss clinical features and management of toxic goitre.
Answer:
Toxic Goitre Or Thyrotoxicosis: It refers to an accumulation of clinical manifestations which are due to excess secretion of acute thyroid hormones.
Toxic Goitre Or Thyrotoxicosis Causes:
- Grave’s disease
- Toxic multinodular goitre
- Toxic adenoma
- The early stage of thyroiditis
- Neonatal thyrotoxicosis
- Iatrogenic hyperthyroidism
Toxic Goitre Or Thyrotoxicosis Types:
- Primary toxic goitre- Grave’s disease
- Secondary toxic goitre
Toxic Goitre Or Thyrotoxicosis Clinical Features:
- Primary Toxic Goitre
- It consists of a classical triad
- Goitre
- Characterised by an enlarged thyroid gland
- On palpation, the gland is smooth and irregular
- Bruit is heard
- Extreme vascularity is present
- Thyrotoxicosis
- Common in females
- Loss of weight
- Increased smooth muscle activity
- Intolerance to heat
- Fine tremors
- Excitability
- Hyperkinetic movements
- Excessive sweating
- Raised pulse rate
- Diarrhoea
- Polyuria
- Hot moist palms
- Systolic hypertension
- Goitre
- Exophthalmos
- It means protrusion of the eyeball
- Spasm of the upper eyelid
- Proptosis with the widening of the palpebral fissure
- Supraorbital and infraorbital swelling
- Congestion and edema of the conjunctiva
- Corneal ulceration
- It consists of a classical triad
- Secondary Toxic Goitre
- Toxic multinodular goitre
- Age- 40-60 years of age
- Sex- common in females
- Exophthalmos rarely occurs
- The presence of long-standing swelling in front of the neck
- Dyspnoea
- Dysphagia
- The gland is firm and irregular
- Toxic nodule
- Occurs at a young age
- Females are commonly affected
- Thyroid swelling occurs
- Presence of hyperthyroidism
- There is a sudden increase in the size of swelling due to necrosis and intraglandular haemorrhage
- Toxic multinodular goitre
Toxic Goitre Or Thyrotoxicosis Treatment:
- Toxic Multinodular Goitre
- To restore the patient to the euthyroid state
- Antithyroid drugs
- Carbimazole-10 mg 6th hourly for 2-3 weeks
- Propranolol-10-20 mg, two-three times a day
- Lugol’s iodine-10-12 drops three times a day
- Potassium perchlorate- 20 mg three times a day
- Antithyroid drugs
- To reduce the functioning of thyroid mass
- Subtotal thyroidectomy
- Radio-iodine therapy
- To minimize complications
- Proper anaesthetic measures
- Good post-operative care
- To restore the patient to the euthyroid state
- Toxic Nodule
- Anti-thyroid drugs
- Radiotherapy
- Subtotal thyroidectomy
Thyroid and parathyroid disorders solved questions
Question 9. What is toxic goitre? What are the differences between primary and secondary goitre? Outline the treatment of primary toxic goitre of the thyroid gland.
Answer:
Toxic Goitre Or Thyrotoxicosis: It refers to an accumulation of clinical manifestations which are due to an excess section of acute thyroid hormones.
Difference Between Primary and Secondary Goitre:
Question 10. Define goitre. Classify various types of goitre.
Answer:
Goitre Definition: Goitre refers to as enlargement of the thyroid gland irrespective of the cause
Goitre Classification
- Simple Goitre
- Diffuse hyperplastic goitre
- Nodular goitre
- Colloid goitre
- Toxic Goitre
- Diffuse toxic goitre
- Toxic nodular goitre
- Toxic nodule
- Neoplastic Goitre
- Benign tumours
- Malignant tumours
- Thyroiditis
- Autoimmune thyroiditis
- Subacute thyroiditis
- Reidel’s thyroiditis
- Other Rare Causes
Diseases Of Thyroid And Parathyroid Glands Short Essays
Question 1. Hypocalcaemia Or Tetany
Answer:
Hypocalcaemia Or Tetany
Hypocalcaemia is defined as the presence of low calcium levels in the blood
Hypocalcaemia Or Tetany Causes:
- Acute pancreatitis
- Acute and chronic renal failure
- Pancreatic and small intestinal fistulae
- Hypoparathyroidism
- Transient hypocalcaemia
Hypocalcaemia Or Tetany Clinical Features:
- Numbness and tingling sensation in the circumoral region and the tips of the fingers and toes
- Hyperactive tendon jerks
- Muscle cramps
- Carpopedal spasms
- Positive Chvostek’s sign
Hypocalcaemia Or Tetany Treatment:
- Intravenous administration of calcium gluconate or chloride
- Oral administration of calcium lactate along with vitamin D
Parathyroid hormone disorder questions
Question 2. Thyroid crisis Or Thyroid storm
Answer:
Thyroid Crisis Or Thyroid storm
- It is a severe thyrotoxic reaction
- It appears suddenly within 3-4 days after the operation
- It is an acute exacerbation of hyperthyroidism
Thyroid Crisis Or Thyroid Storm Clinical Features:
- Tachycardia
- Fever
- Restlessness
- Delirium
Thyroid Crisis Or Thyroid storm Treatment:
- Sedatives- morphine or pethidine
- Control of hyperpyrexia- by use of ice bag, tepid sponging, hypothermic blanket
- Oxygen administration
- Potassium administration
- Use of 100 mg cortisone
- Lugol’s iodine is given intravenously
- 20-40 mg propranolol
- Digitalis to treat atrial fibrillation
Question 3. Adenoma Thyroid
Answer:
Adenoma Thyroid
All benign tumours of the thyroid gland arise from glandular tissues and are called adenomas
Adenoma Thyroid Types:
- Follicular adenoma
- Papillary adenoma
Adenoma Thyroid Clinical Features:
- Gradual swelling of the thyroid gland
- Swelling is palpable
- Bleeding in the tumour causes pain and a rapid increase in the size of the swelling
Adenoma Thyroid Investigations:
X-ray of the neck- for swelling
Adenoma Thyroid Treatment:
- Excisional biopsy
- Lobectomy and removal of adenoma with surrounding healthy tissue
- Replacement doses of L-thyroxine
Question 4. Hashimoto’s thyroiditis
(or)
Autoimmune thyroiditis
Answer:
Autoimmune Thyroiditis
Autoimmune Thyroiditis is also called Hashimoto’s disease or lymphedema- noid goitre
Hashimoto’s Thyroiditis Etiology:
- It is an autoimmune disease
- Four antigens are detected
- Thyroid cell microsomes
- Thyroid cell nuclear component
- Thyroglobulin
- Nonthyroglobulin colloid
Hashimoto’s Thyroiditis Clinical Features:
- Females are commonly affected the Onset is insidious
- Thyroid enlargement with slight pain
- Tenderness in the region of the thyroid
- Mild hyperthyroidism
- Shortness of breath
- Fatigue
- Increase in weight
- Thyroid gland examination
- Diffuse swelling
- Nodular
- Firm or rubbery in consistency
- Diffuse swelling
- Increased incidence of rheumatoid arthritis, hemo- Iyitc anaemia, myasthenia gravis and pernicious anaemia
Hashimoto’s Thyroiditis Treatment: Surgical excision
Thyroid disorders short answer questions
Question 5. Solitary nodule of thyroid
(or)
Thyroid nodule
Answer:
Solitary Nodule Of Thyroid
Solitary Nodule Of Thyroid can be classified into benign and malignant nodules
Thyroid Nodule Etiopathogenesis:
- Thyroiditis
- Follicular adenoma
- Carcinoma
- Thyroid cyst
- Colloid nodules
Thyroid Nodule Clinical Features:
- Age- 20-40 Years of age
- Sex- common in females
- Stridor
- Tracheal deviation
- Neck vein engorgement
- Dyspnoea
- Dysphagia
- The solitary nodule is present
Thyroid Nodule Treatment:
- Excision of solitary nodule along with a margin of normal thyroid tissue
- If the nodule is present at the junction of the isthmus and lobe- hemithyroidectomy is done
- In the presence of malignancy- immediate total thyroidectomy is done
Question 6. Retrosternal Goitre
Answer:
Retrosternal Goitre
Retrosternal goitre is derived from the lower pole of the multinodular goitre
Retrosternal Goitre Clinical Features:
- Usually asymptomatic
- Symptoms occur as obstruction
- Obstruction of trachea- Dyspnoea
- Obstruction of the oesophagus- Dysphagia
- Obstruction to the major veins in the thorax- Engorgement of neck veins
Retrosternal Goitre Investigations:
- Thyroid scan
- Thyroid function tests
- Barium swallow
- Chest X-ray
Retrosternal Goitre Treatment: Resection of retrosternal goitre
Hypothyroidism and hyperthyroidism questions
Question 7. Gasification of goitre.
Answer:
Gasification Of Goitre
Goitre refers to the enlargement of the thyroid gland irrespective of the cause
Gasification Of Goitre Classification:
- Simple Goitre
- Diffuse hyperplastic goitre
- Nodular goitre
- Colloid goitre
- Toxic Goitre
- Diffuse toxic goitre
- Toxic nodular goitre
- Toxic nodule
- Neoplastic Goitre
- Benign tumours
- Malignant tumours
- Thyroiditis
- Autoimmune thyroiditis
- Subacute thyroiditis
- Reidel’s thyroiditis
- Other Rare Causes
Question 8. Thyroglossal Fistula
Answer:
Thyroglossal Fistula
- A Thyroglossal cyst may rupture unexpectedly resulting in a draining sinus known as a Thyroglossal fistula
- It can develop when the removal of the cyst has not been fully completed
- It is usually noticed when bleeding in the neck occurs causing swelling and fluid ejection around the original wound of removal
- It is lined by columnar epithelium
Thyroglossal Fistula Types
- Congenital
- Thyroglossal fistula is a disorder of the Thyroglossal duct which develops from the thyroid primordium in the floor of the primitive pharynx at the site of foramen caecum
- If involution of the Thyroglossal duct is incomplete, the Thyroglossal fistula may develop
- Acquired
- Incomplete removal of Thyroglossal cyst
- Rupture of Thyroglossal cyst
Thyroglossal Fistula Treatment: Sistrunk operation
Diseases Of Thyroid And Parathyroid Glands Short Answers
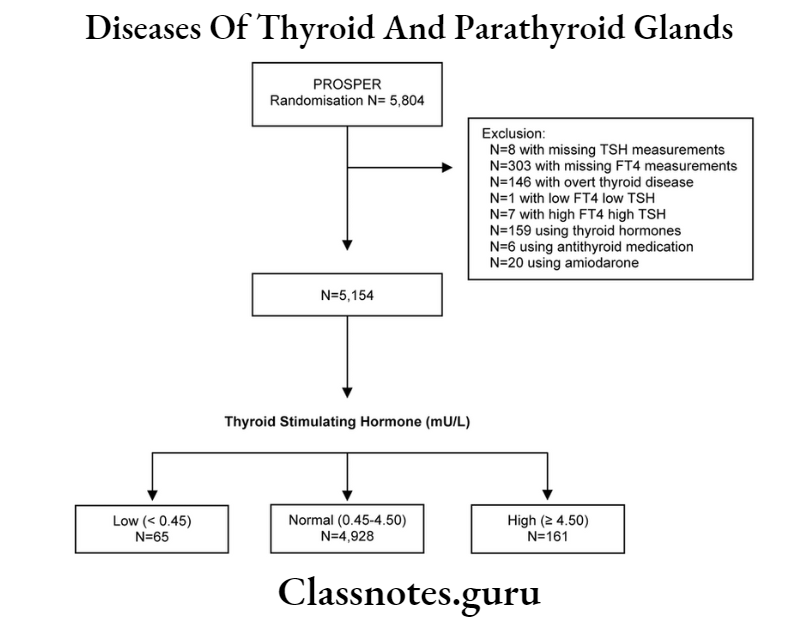
Question 1. TSH
Answer:
TSH
- Thyroid stimulating hormone is a peptide hormone synthesized and secreted by thyrotrope cells in the anterior pituitary gland
- It regulates the endocrine function of the thyroid gland
- It controls the rate of secretion of thyroxine and triiodothyronine by the thyroid gland
- It controls the rates of most intracellular chemical reactions in the body
- TSH secretion is regulated via a negative feedback loop by T4 and T3, when their levels are low, the production of TSH is increased
- When their levels are high, TSH production is decreased
Question 2. Goitre
Answer:
Goitre
Goitre refers to the enlargement of the thyroid gland
Goitre Clinical Features:
- Hoarseness of voice
- Coughing
- Dysphagia
- Dyspnoea
GoitreTreatment:
- Use of antithyroid drugs
- Use of Levothyroxine in euthyroid patients
- Thyroidectomy
Question 3. Thyroid scan I131
Answer:
Thyroid Scan I131
I131 is obtained at 24 hours
Thyroid Scan I131 Indications:
- When a solitary nodule is palpated
- In retrosternal goitre
- In ectopic thyroid tissue
- In toxic nodular goitre
Thyroid Scan I131 Uses:
- To distinguish functioning and non-functioning thyroid nodules
- To diagnose pathology of the thyroid gland
- To assess the nature of the nodule
- Detect areas of abnormality
- Determine the spread of thyroid cancer
- Evaluate changes in the gland
Question 4. Exophthalmos
Answer:
Exophthalmos
- It means protrusion of the eyeball
- Spasm of the upper eyelid
- Proptosis with the widening of the palpebral fissure
- Supraorbital and infraorbital swelling
- Congestion and edema of the conjunctiva
- Corneal ulceration
Question 5. Hoarseness of voice
Answer:
Hoarseness Of Voice
Hoarseness Of Voice is an abnormal change in voice
Hoarseness Of Voice Causes:
- Acid reflux
- Smoking
- Alcohol
- Screaming
- Allergies
- Inhaling toxic substances
- Coughing
- Polyps on the vocal cords
- Throat, thyroid or lung cancer
- Damage to the throat
- Aortic aneurysm
Hoarseness Of Voice Treatment:
- Rest your voice for a few days
- Avoid talking and shouting B Drink plenty of fluids
- Take hot showers and Use lozenges Avoid smoking
- Eliminate allergens
Question 6. Causes of dyspnoea in goitre
Answer:
Causes Of Dyspnoea In Goitre
- Pressure due to enlarged thyroid gland
- Formation of haematoma
- Tracheomalacia
- Bilateral recurrent laryngeal nerve injury
- Hypocalcaemia
Hypothyroidism and hyperthyroidism questions
Question 7. Metastasis in papillary carcinoma of the thyroid.
Answer:
Metastasis In Papillary Carcinoma Of The Thyroid
- Papillary carcinoma of the thyroid invades the lymphatic’s and spreads to other sites
- Vascular invasion is rare
- If occurs, it occurs through the lungs and bones
- Direct extension into soft tissues of the neck occurs in approx. 25% of cases
Question 8. Post-operative complications of thyroid surgery.
Answer:
Thyroid Surgery Complications:
- Minor Complications
- Seromas
- Poor scar formation
- Rare Complications
- Damage to the sympathetic trunk
- Major Complications
- Bleeding
- Injury to recurrent laryngeal nerve
- Hypoparathyroidism
- Thyrotoxic storm
- Injury to the superior laryngeal nerve
- Infection
Question 9. Thyroglossal cyst
Answer:
Thyroglossal Cyst: It is a cystic swelling developed in the remnant of the thyroglossal tract
Thyroglossal Cyst Etiology: Develops from the ventral portion of the endoderm between the first and second branchial arch
Thyroglossal Cyst Clinical Features:
- Age- common between 15-30 years of age n Sex- common in women h Pain in cyst
- Size: 0.5 cm to 5 cm in diameter
- Shape: spherical or oval
- Cysfbecomes tender
- It may develop anywhere along the thyroglossal tract
- Firm or hard in consistency
- Cyst moves with deglutition
Thyroglossal Cyst Management: Excision of the cyst
Question 10. Plunging goitre
Answer:
Plunging Goitre
- Plunging goitre is also called wandering goitre or diving goitre
- Plunging goitre is freely movable above or below the sternal notch
- Plunging goitre is usually not palpable
- Plunging goitre is palpable during coughing, and sneezing due to increased intrathoracic pressure
Question 11. Hypercalcaemia
Answer:
Hypercalcaemia
Hypercalcaemia is a condition in which the calcium level in the blood is above normal
Hypercalcaemia Causes:
- Overactive parathyroid glands
- Cancer
- Calcium and vitamin D supplements
Hypercalcaemia Clinical features
- Excessive thirst and frequent urination
- Nausea, vomiting, constipation
- Bone pain. Muscular weakness
- Confusion, lethargy, depression
- Palpitation, cardiac arrhythmia
Hypothyroidism and hyperthyroidism questions
Question 12. Gynaecomastia
Answer:
Gynaecomastia
Gynaecomastia is an endocrine disorder in which a noncancerous increase in size of male breast tissue occurs
Gynaecomastia Causes:
- Altered ratio of Estrogen to androgen
- Diseases like liver disease, kidney failure, low testosterone
- Certain medications
Gynaecomastia Clinical features
- Male breast enlargement with soft, compressible and mobile subcutaneous chest tissue
- Enlargement may occur on one side or both
- Asymmetry of chest tissue occurs
Diseases Of Thyroid And Parathyroid Glands Viva Voce
Among simple goitre, nodular goitre is more prone to malignant transformation
