Diseases Of The Pulp And Periapical Tissues Important Notes
- Classification Of Pulp Disease
- Inflammatory disease
- Focal reversible pulpitis
- Acute pulpitis
- Chronic pulpitis
- Chronic hyperplastic pulpitis
- Miscellaneous
- Aerodositalgsa
- Necrosis
- Reticular atrophy
- Cakifscatkm
- Palpal metaplasia
- Inflammatory disease
- Focal Reversible Pulpitis Or Pulp Hyperemia
- It is a mild, transient localized inflammatory reaction in the pulp that can be treated by conservative means without involving any form of direct pulp therapy
- The tooth is sensitive to cold
- The involved tooth has a large carious lesion, large restoration, or restoration with defective margins
- Histopathology
- Dilatation of pulpal vessel
- Collection of edema fluid
- Displacement of odontoblast cell nuclei into dentinal tubules
- Infiltration of leukocytes
- Acute Pulpitis
- Mode of development
- Extension of focal reversible pulpitis
- As de novo
- As acute exacerbation of chronic pulpitis
- Clinical features
- The tooth is extremely sensitive to hot or cold
- Has short and severe lancinating pain
- Associated with microabscess formation
- Draining pus has a noxious odor
- Mode of development
- Chronic Pulpitis
- The tooth may be asymptomatic
- There may be an intermittent dull and throbbing pain
- Less sensitive to hot or cold stimuli
- Treatment
- Root canal treatment
- Extraction
- Pulp Polyp Or Chronic Hyperplastic Pulpitis
- Characterized by the overgrowth of tissue outside the boundary of the pulp chamber as a protruding mass
- Teeth commonly involved are
- Deciduous molars
- First permanent molar
- Affected tooth always has a large open carious cavity
- Periapical Granuloma
- Sequence of pulpitis
- It is a localized mass of chronic granulation tissue formed from infection
- Involved tooth is usually nonvital
- May produce dull sounds on percussion
- The patient may complain of pain on biting or chewing on solid food
- Radiographically appears as a thickening of the ligament at the root apex
- Loss of lamina dura
- Epithelium of it may arise from
- Respiratory epithelium
- Oral epithelium growing in through fistula
- Oral epithelium proliferating apically from a periodontal pocket
- Consists of
- Granulation tissue mass
- Chronic inflammatory cells
- Epithelial islands, cholesterol clefts, foam cells
- Giant cells
- Plasma cells
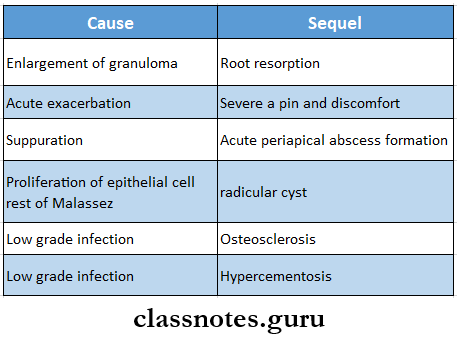
- Sequel
- Resorption of the root apex
- Acute exacerbation
- Suppuration
- Radicular cyst
- Osteosclerosis in apical region
- Hypercementosis
- Osteomyelitis
- Osteomyelitis Definition
- Osteomyelitis is defined as inflammation of bone and bone marrow along with surrounding periosteum
- Osteomyelitis Classification
- Acute osteomyelitis
- Acute suppurative osteomyelitis
- Acute subperiosteal osteomyelitis
- Acute periostitis
- Chronic osteomyelitis
- Nonspecific type
- Chronic intramedullary osteomyelitis
- Chronic focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periostitis
- Specific type
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis
- Nonspecific type
- Acute osteomyelitis
- Radiation-induced osteomyelitis
- Idiopathic osteomyelitis
- Osteomyelitis Definition
Diseases Of The Pulp And Periapical Tissues Long Essays
Question 1. Define and classif pulpitis. Write in detail about the pathogenesis, features, and histopathological features of acute pulpitis.
Answer:
Classify Pulpitis Definition: Pulpitis is the inflammation of dental pulp resulting from intreated caries, trauma, or multiple restorations
Classif Pulpitis Classification
- Inflammatory diseases
- Acute pulpitis
- Chronic pulpitis
- Depending on the extent of involvement of pulp
- Partial pulpitis
- Generalized pulpitis
- Based on the presence or absence of direct communication between dental pulp and oral environment
- Open pulpitis
- Closed pulpitis
Acute Pulpitis:
- Acute pulpitis is an irreversible condition characterized by acute, intense inflammatory reaction in the pulpal tissue
Acute Pulpitis Pathogenesis:
- Acute Pulpitis occurs through
- Extension of focal reversible pulpitis
- As a de novo condition, where inflammation is acute from the beginning
- Acute exacerbation of chronic pulpitis
Read And Learn More: Oral Pathology Questions and Answers
Acute Pulpitis Clinical Features:
- Occurs in the tooth with large carious lesion or restoration
- Severe pain occurs in the involved tooth
- It is sensitive to hot or cold stimuli
- Pain is not relieved even after the removal of the stimuli
- Pain increases during sleep
- Associated with micro-abscess formation along with liquefaction degeneration
- Formation of drainage
- The pus has a noxious odor
- Patients are apprehensive and ill
- When intrapulpal pressure increases, it may collapse of apical blood vessels
- This is known as the pulp-strangulation
Acute Pulpitis Histopathology
- Characterized by continued vascular dilatation
- Accumulation of edema fluid in connective tissue surronding
- Micro-abscess formation untreated
- Liquefaction and necrosis of pulp due to destruction of the odontoblastic cell layer of pulp
- Death of pulp along with tissue dehydration occurs
- This is known as dry gangrene of pulp
Question 2. Define and classify osteomyelitis. Write about the etiology, pathology, and clinical features of acute suppurative osteomyelitis
Answer:
Osteomyelitis Definition: Osteomyelitis is defined as inflammation of the bone narrowsrrow along with surrounding periosteum
Osteomyelitis Classification:
- Acute osteomyelitis
- Acute suppurative osteomyelitis
- Acute subperiosteal osteomyelitis
- Acute periostitis
- Chronic osteomyelitis
- Nonspecific type
- Chronic intramedullary osteomyelitis
- Chronic focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periostitis
- Chronic subperiosteal osteomyelitis
- Specific type
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis
- Nonspecific type
- Radiation-induced osteomyelitis
- Idiopathic osteomyelitis
Acute Suppurative Osteomyelitis
- Acute suppurative osteomyelitis is diffuse spreading inflammation characterized by extensive tissue necrosis
Acute Suppurative Osteomyelitis Etiology:
- Dental infection due to
- Fracture
- Gunshot wound
- Hematogenous spread
- Causative organisms
- Staphylococcus aureus
- Staphylococcus albus
- Variant streptococci
- Anaerobes- bacteroids, prevotella
Acute Suppurative Pathology:
Acute Suppurative Clinical Features
- Age-after 30years of age
- Sex-common in males
- Site- maxilla or mandible
- In the maxilla, the disease is well-localized
- In mandible disease is more diffuse and widespread
- Severe throbbing, deep-seated pain in the in
- Diffuse large swelling on the jaw
- Trismus
- Paraesthesia of lip
- Rise in body temperature
- Regional lymphadenopathy
- Regional teeth are loose and sore
- Difficulty in eating
- Exudation of pus from gingival margin
- Excessive salivation
- Bad breath
- In advanced cases, reddening of overlying skin or mucosa
- Anorexia, vomiting
- Metastatic spread of disease-causing cellulitis, bacteremia, septicemia
- Distension of periosteum due to pus accumulation
- Exfoliation of necrotic bone fragments or sequestrum spontaneously
- Pathological fracture may occur
Question 3. Enumerate periapical lesions. Describe the etiology, histopathological, clinical, and radiographic features of periapical granuloma and mention its consequences
Answer:
Periapical Lesions:
- Acute apical periodontitis
- Periapical abscess
- Periapical granuloma
- Periapical cyst
- Dentigerous cyst
- Periapical scar
- Giant cell granuloma
- Osteomyelitis
- Periapical cemental dysplasia
- Langerhans cell disease
Periapical Granuloma:
- Periapical granuloma is a localized mass of granulation tissue around the root apex of a non-vital tooth
Periapical Lesions Etiology:
- Extension of pulpal inflammation or infection beyond the root apex
- Occlusal trauma
- Orthodontic tooth movement
- Acute trauma
- Perforation of root apex during endodontic therapy
- Spread of periodontal infection
- Chemical irritation
Periapical Lesions Clinical Features:
- The involved tooth is nonvital and slightly tender on percussion
- Mild pain occurs on biting or chewing on solid food
- The tooth may be slightly elongated in its socket
- Sensitivity occurs due to hyperemia, edema, and inflammation of the apical periodontal ligament
- The tooth is usually asymptomatic
- Pain occurs during acute exacerbations
Periapical Lesions Histopathology:
- Inflammation and locally increased vascularity of tissue are associated
- There is the proliferation of fibroblasts and endothelial cells formation of more tiny vascular channels occurs
- New capillaries are lined by swollen endothelial cells
- Cells present are
- Macrophages
- Indicates chronic inflammation
- Lymphocytes
- Indicates delayed hypersensitivity reaction
- Plasma cells
- Produces immunoglobulin
- Epithelial islands and foam cells
- Deposit of cholesterol and hemosiderin are present
- Cholesterol crystals appear clear needle-like spaces or clefts
- Presence of collagen bundles in connective tissue
- Macrophages
Periapical Lesions Radiographic Features:
- Thickening of the periodontal ligament at the root apex
- Periapical granuloma appears as a radiolucent area of variable size attached to the root apex
- It is well-circumscribed, well-demarcated from surrounding bone
- The thin radiopaque line representing the zone of sclerotic bone outlines the lesion
- In some cases, radiolucency may blend with the surrounding bone
- Advance lesions show root resorption and loss of apical dura
Periapical Lesions Complications:
Diseases Of The Pulp And Periapical Tissues Short Essay
Question 1. Chronic hyperplastic pulpitis
(or)
Pulp polyp
Answer:
Chronic Hyperplastic Pulpitis
- Pulp polyp is an unusual type of hyperplastic granulation-responsive pulp
- It is characterized by the overgrowth of tissue outside the boundary of the pulp chamber as a protruding mass
Pulp Polyp Clinical Features:
- Occurs in children and young adults
- Pulp Polyp involves teeth with large, open carious lesions
- Pulp Polyp appears as a small, pinkish-red, lobulated mass protruding out from the pulp chamber
- The teeth mostly involved are deciduous molars and the first permanent molar
- Lesion bleeds profusely on slight provocation
- If traumatized, the pulp polyp becomes ulcerated
- Then it appears as a dark red, fleshy mass with fibrinous exudate
Pulp Polyp Histopathology:
- Hyperplastic tissue is made up of delicate connective tissue fibers interspersed with a variable number of small capillaries
- Inflammatory cell infiltration includes lymphocytes, plasma cells, and polymorphonuclear leukocytes
- Presence of fibroblast and endothelial cell proliferation
- Granulation tissue gets epithelialized
- The epithelium is stratified squamous with well-formed rete pegs
- Pulp Polyp contains desquamated cells from the buccal mucosa, gingiva, and salivary gland carried by the saliva
- There is hyperemia and edema of pulpal tissue
- Focal areas of pulpal necrosis surrounded by fibrosis are seen
- Reparative secondary dentin may be formed
Question 2. Garre’s osteomyelitis
Answer:
Garre’s Osteomyelitis
- Garre’s Osteomyelitis represents a reactive periosteal osteogenesis in response to low-grade infection or trauma
Garre’s Osteomyelitis Clinical Features:
- Occurs at a young age
- Site involved
- The posterior part of the mandible
- Maxilla
- Toothache
- Pain in jaw
- Bony hard swelling on the outer surface of the jaws size of swelling varies from a few centimeters to the entire length of the mandible
- Slight pyrexia
- Moderate leucocytosis
Garre’s Osteomyelitis Radiographic Features:
- Presents as a mottled radiolucent lesion with few radiopaque foci
- The cortex of bone exhibits many concentric or parallel opaque layers giving onion skin appearance
- Garre’s Osteomyelitis shows focal overgrowth of bone on the outer surface of the cortex
- Described as a duplication of the cortical layer of bone
- Few newly formed bony trabeculae are oriented perpendicular to onion skin layers
Garre’s Osteomyelitis Histopathology:
- The lesion consists of new bone and osteoid
- Osteoblasts border the trabeculae
- Trabeculae are oriented perpendicular to the cortex
- They are arranged parallel to each other
- Connective tissue contains lymphocytes and plasma cells
- Garre’s Osteomyelitis is fibrous
- There may be the presence of sequestrum
Question 3. Chronic focal sclerosing osteomyelitis
Answer:
Chronic Focal Sclerosing Osteomyelitis
- Chronic focal sclerosing osteomyelitis is a rare nonsuppurative inflammatory condition of bone
Chronic Focal Sclerosing Osteomyelitis Etiology:
- Chronic pulpitis
- Traumatic malocclusion
Chronic Focal Sclerosing Osteomyelitis Clinical Features:
- Occurs in children and young adults
- Common in mandibular first molars
- Presents as a large carious lesion
- The associated tooth is non-vital
- Asymptomatic condition
Chronic Focal Sclerosing Osteomyelitis Radiographic Features:
- Presents as a well-circumscribed radiopaque mass of sclerotic bone surrounding the apex of the root of the involved tooth
- Lamina dura is intact
- Widening of periodontal ligament
- The border of the lesion is smooth and distinct
Chronic Focal Sclerosing Osteomyelitis Histopathology:
- Consist of a dense mass of bony trabeculae with little interstitial marrow tissue
- Osteocytic lacunae are empty
- Bony trabeculae exhibit many resting and reversal lines
- Bone marrow if present, is fibrotic and infiltrated by chronic inflammatory cells
Question 4. Focal Reversible Pulpitis
Answer:
Focal Reversible Pulpitis
Focal Reversible Pulpitis is an acute inflammatory response to noxious stimuli
Focal Reversible Pulpitis Etiology
- Trauma
- Thermal injury
- Chemical stimulus
- Deep restoration
Focal Reversible Pulpitis Symptoms:
- Sharp sudden pain on stimulus
- Pain relieves on removal of stimuli
Focal reversible Pulpitis Diagnosis:
- Clinically – caries
- Traumatic occlusion
- Percussion test – Negative
- Radiograph – Normal PDL and lamina dura
- Vitality – Early response
Focal Reversible Pulpitis Treatment:
- No endodontic treatment is required Sedative dressing placed
- Desensitize the tooth
- Use of cavity varnish
Question 5. Apical Periodontal cyst
Answer:
Apical Periodontal Cyst
Apical Periodontal Cyst is also called a radicular cyst
Apical Periodontal Cyst Clinical Features:
- Age- young age
- Sex- common in males
- Site- common in maxillary anterior
- Involved teeth are nonvital
- Smaller cysts are asymptomatic
- Larger lesions produce slow enlarging, bony hard swelling
- Expansion and distortion of cortical plates
- Severe bone destruction
- The springiness of jaw bones
- Pain occurs if a secondary infection is present
- Intraoral and extraoral pus discharge
- Pathological fractures
- Formation of abscess called “cyst abscess”
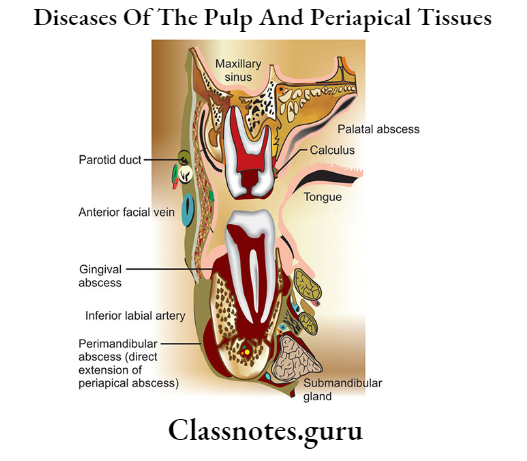
Question 6. Alveolar abscess
Answer:
Alveolar Abscess
- Also called a periapical abscess
- Alveolar Abscess is the acute or chronic suppurative process of the periapical region
Alveolar Abscess Clinical Features:
- Involved teeth are extremely painful
- It is slightly extruded from its socket
- Regional lymphadenitis
- There may be swelling of the tissues
- Fever
- There may be swelling of the tissues
- May develop into osteomyelitis
- Chronic condition leads to mild symptoms
Question 7. Classification of osteomyelitis
Answer:
Classification Of Osteomyelitis
- Acute osteomyelitis
- Acute suppurative osteomyelitis
- Acute subperiosteal osteomyelitis
- Acute perseids
- Chronic osteomyelitis
- Nonspecific type
- Chronic intramedullary osteomyelitis
- Chrome focal sclerosing osteomyelitis
- Chronic diffuse sclerosing osteomyelitis
- Chronic osteomyelitis with proliferative periostitis
- Chronic subperiosteal osteomyelitis
- Specific type
- Tuberculous osteomyelitis
- Syphilitic osteomyelitis
- Actinomycotic osteomyelitis
- Nonspecific type
- Radiation-induced osteomyelitis
- Idiopathic osteomyelitis
Question 8. Sequestrum
Answer:
Sequestrum
- Sequestrum is a fragment of dead tissue, usually bone, that has separated from healthy tissue as a result of injury disease
- Sequestrum is a vascular
Sequestrum Types:
- Primary sequestrum
- A piece of dead bone that completely separates from sound bone during the process of necrosis
- Secondary sequestrum
Sequestrum Treatment:
- Removed by sequestrum
Question 9. Garre’s osteomyelitis
Answer:
Garre’s Osteomyelitis
Garre’s Osteomyelitis represents a reactive periosteal osteogenesis in response to low-grade infection or trauma
Garre’s Osteomyelitis Clinical Features:
- Occurs at a young age
- Site involved
- The posterior part of the mandible
- Maxilla
- Toothache
- Pain in jaw
- Bony hard swelling on the outer surface of the jaw
- The size of swelling varies from a few centimeters to the entire length of the mandible
- Slight pyrexia
- Moderate leucocytosis
Question 10. Acute suppurative osteomyelitis
Answer:
Acute Suppurative Osteomyelitis
Acute suppurative osteomyelitis is diffuse spreading acute inflammation of the bone characterized by extensive tissue necrosis
Acute Suppurative Osteomyelitis Clinical Features:
- Age- after 30 years of age
- Sex- common in males
- Site- maxilla or mandible
- In the maxilla, the disease is well-localized
- In the mandible, the disease is more diffuse and widespread
- Severe throbbing, deep-seated pain in the involved jaw
- Diffuse large swelling of the jaw
- Trismus
- Paraesthesia of lip
- Rise in body temperature
- Regional lymphadenopathy
- Regional teeth are loose and sore
- Difficulty in eating
- Exudation of pus from gingival margin
- Excessive salivation
- Bad breath
- In advanced cases, reddening of overlying skin or mucosa
- Anorexia, vomiting
- Metastatic spread of disease pausing cellulitis, bacteremia, septicemia
- Distension of periosteum duo to pus accumulation
- Kxfollatlou of necrotic bono fragment or sequestrum spontaneously
- Pathological fracture may occur
Diseases Of The Pulp And Periapical Tissues Viva Voce
- Osteocalcin is a glycoprotein present In presenting
- Young people more often develop focal reversible pulpit Ih
- During acute inflammation, Intropulmonary pressure becomes very high causing the collapse of the apical blood vessels. This is called pulp strangulation
- Death of pulp along with I Issue dehydration is called dry gangrene of pulp
- Untreated pulpitis leads to necrosis of the pulp
- Aerodontalgia is dental pain during high altitude or deep sen diving
- Acute exacerbation of n chronic periapical lesion is known as a Phoenix abscess
- The presence of sequestrum is a feature of osteomyelitis
