Diseases Of The Periodontium Important Notes
- Periodontium
- Includes – gingiva, periodontal ligament, cementum, and bone
- Periodontium Functions
- Attaches tooth to the jaw bone
- Maintains integrity of masticatory system
- Gingiva
- Gingiva Parts
- Free gingiva
- Attached gingiva
- Interdental papilla
- Color – coral pink
- Surface – stippled- orange peel
- Fibers
- Circular
- Dentogingival
- Dentoperiosteal
- Alveologingival
- Transseptal
- Gingiva Parts
- Functions Of Gingival Fluid
- Cleanse material from the sulcus
- Improves adhesion of epithelium to the tooth
- Maintains structure of junctional epithelium
- Has antimicrobial property
- Periodontal Ligament
- It is dense connective tissue attached to the cementum on one end and alveolar bone on the other
- Principal fibers
- Alveolar crest group
- Horizontal Group
- Oblique group
- Apical group
- Interradicular group
- Cells
- Cementoblasts
- Osteoblasts
- Osteoclasts
- Epithelial remnants of Malassez
- Width – 0.2-0.4 mm
- Shape – hourglass shape
- AUG
- Also known as Vincent’s infection, Vincent’s stomatitis, trench mouth, fetid stomatitis, putrid stomatitis
- Smears from the lesions of ANUG show spirochaetes and fusiform bacilli
- Clinical Features
- Punched out crater-like depressions at the crest of interdental papilla covered by pseudomembrane and extending into marginal gingiva
- The pseudomembranous slough is demarcated from the remaining gingival mucosa by linear erythema
- c.Attached gingiva and alveolar mucosa are rarely involved
- Drugs Causing Gingival Enlargements
- Dilantin sodium
- Cyclosporine
- Calcium channel blockers
- Papillon Lefevre Syndrome
- Characterized by
- Cutaneous lesions
- Keratotic lesions of palmar and plantar surfaces
- Oral lesions
- Aggressive periodontitis
- Severe destruction of alveolar bone
- Rapid bone loss and pathological migration lead to loss of entire dentition at an early age
- Cutaneous lesions
- Characterized by
- Peri-Implants
- Peri-Implants is inflammation of the soft tissue surrounding the osseointegrated implant in function and progressive bone loss
- Peri-Implants begins at the coronal portion of the implant.
- Peri-Implants Clinical features:
- Erythema over the area
- Bleeding on probing
- Pocket formation
- Bone destruction
- Suppuration
- Presence of calculus
- Tooth mobility present
Diseases Of The Periodontium Long Essays
Question 1. Classify periodontal diseases. Describe in detail about acute necrotizing ulcerative gingivitis (ANUG).
Answer:
Periodontal Diseases Classification:
- Gingival diseases
- Plaque-induced gingival diseases
- Non-plaque-induced gingival diseases
- Periodontitis
- Chronic periodontitis
- Localized
- Generalized
- Aggressive periodontitis
- Localized
- Generalized
- Periodontitis associated with systemic diseases
- Necrotizing periodontal diseases
- Necrotizing ulcerative gingivitis
- Necrotizing ulcerative periodontitis
- Abscesses of the periodontium
- Gingival abscess
- Periodontal abscess
- Periocoronal abscess
- Periodontitis associated with endodontic lesion
- Developmental or acquired deformities
- Localized
- Mucogingival lesion around teeth
- Mucogingival lesion around edentulous ridges
- Occlusal trauma
- Chronic periodontitis
Read And Learn More: Oral Pathology Questions and Answers
Acute Necrotizing Ulcerative Gingivitis:
- Acute Necrotizing Ulcerative Gingivitis is an inflammatory destructive disease of the gingiva
Acute Necrotizing Ulcerative Gingivitis Etiology:
- Causative organisms are
- Prevotellaintermedia
- Fusobacterium
- Treponema
- Selenomonas species
Acute Necrotizing Ulcerative Gingivitis Precipitating Factors:
- Poor oral hygiene
- Trauma
- Smoking
- Stress
- Nutritional deficiency
- Chronic diseases
- Blood disorders
Acute Necrotizing Ulcerative Gingivitis Clinical Features:
- Prodromal symptoms
- Debilitating diseases
- Psychologic stress
- Intraoral signs
- Punch out crater-like depression
- Pseudomembranous slough
- Gingival hemorrhage
- Fetid odor
- Increased salivation
- Sensitive to pain
- Radiating gnawing pain
- Increased pain on having spicy food
- Metallic foul taste
- Extra-oral signs
- Lymphadenopathy
- Fever
- Loss of appetite
- Lassitude
- Leucocytosis
Acute Necrotizing Ulcerative Gingivitis Histopathology:
- Epithelial changes
- The surface epithelium is destroyed
- It is replaced by pseudomembrane
- This membrane consists of fibrin, necrotic epithelial cells, neutrophils, and various micro-organisms
- Connective tissue
- It is hyperaemic
- Contains numerous engorged capillaries
- Consists of dense infiltration of neutrophils and plasma cells
Acute Necrotizing Ulcerative Gingivitis Treatment:
- Antibiotics
- Penicillin-500 mg TDS or
- Metronidazole-200-400 mgBID
- Removal of pseudomembrane with the help of pellet soaked in hydrogen peroxide
- Scaling and root planning
- In severe cases, gingivoplasty
Question 2. Enumerate causes of gingival enlargement. Discuss the pathogenesis, clinical features, and histopathology of leukemic enlargement.
Answer:
Causes Of Gingival Enlargement:
- Inflammation
- Acute
- Chronic
- Drug-induced
- Phenytoin
- Cyclosporins
- Systemic diseases
- Conditioned enlargements
- Puberty
- Pregnancy
- Non-specific
- Systemic diseases
- Leukemia
- Conditioned enlargements
- Neoplastic
- Benign tumors
- Malignant tumors
- False enlargements
- Idiopathic
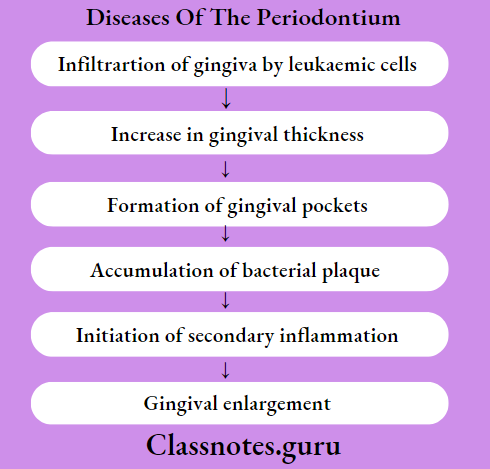
Leukaemic Gingival Enlargement Pathogenesis
Leukaemic Gingival Enlargement Clinical Features:
- Distribution
- Diffuse or marginal
- Localized or generalised
- It increases in size and gradually covers the tooth crown
- It appears as tumor enlargement
- Color-bluish red
- Surface-shiny surface
- Consistency-spongy-like and friable
- Gingiva bleeds spontaneously
- Increased susceptibility to infections
Leukaemic Gingival Enlargement Histopathology:
- Epithelium
- Hyperplastic
- Diminished keratinization
- Presence of inter and intracellular edema
- Consists of pseudomembrane containing fibrin, necrotic cells, neutrophils, and bacteria
- Reticular layer
- Contains immature and proliferating leukemic cells
- Papillary layer
- Contains few leukocytes
- Blood vessels
- Contains leukemic cells and RBCs
Leukaemic Gingival Enlargement Treatment:
- Scaling and curretage
- Antibiotic prophylaxis
- Incision and drainage
- Cleanse the area with a cotton pellet soaked in hydrogen peroxide
- Application of pressure with gauze.
Diseases Of The Periodontium Short Essays
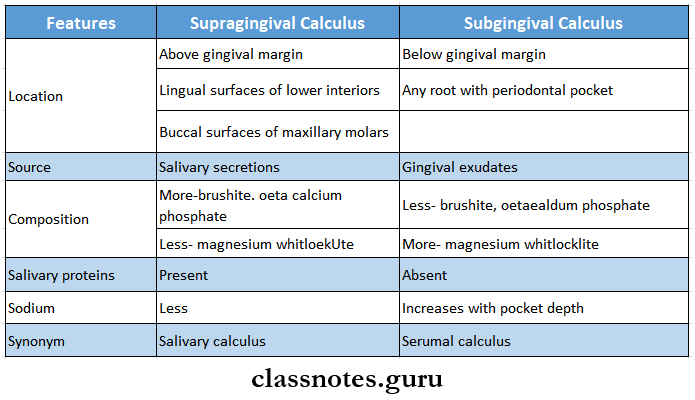
Question 1. Difference between supragingival and subgingival calculus
Answer:
Difference Between Supragingival And Subgingival Calculus
Question 2. Juvenile periodontitis or Aggressive periodontitis
Answer:
Juvenile Periodontitis
- Rapid loss of attachment and bone loss occurring in an otherwise clinically healthy patient with the amount of microbial deposits inconsistent with disease severity and familial aggregation of diseased individuals
Juvenile Periodontitis Or Aggressive Periodontitis Etiology:
- Hereditary
- A.actinomycetumcomitans
- Capnocytophaga
Juvenile Periodontitis Or Aggressive Periodontitis Types:
- Localized Aggressive Periodontitis:
- Localized Aggressive Periodontitis Clinical Features:
- Age-20 years
- Sex- common in females
- Lack of inflammation
- Deep pockets
- A small amount of plaque
- Mobility of first molars and incisors
- Midline diastema
- Root sensitivity
- Deep dull radiating pain
- Periodontal abscess
- Lymphadenitis
- Localized Aggressive Periodontitis Radiographic Features:
- Vertical/ angular bone loss
- Arc-shaped loss of alveolar bone extending from distal surface of 2nd premolar to mesial surface of 2nd molar
- Bilateral involvement results in a “mirror image” pattern
- Localized Aggressive Periodontitis Clinical Features:
- Generalized Aggressive Periodontitis:
- Characterized by generalized interproximal attachment loss affecting at least three permanent teeth other than the first molar and incisors
- Generalized Aggressive Periodontitis Clinical Features:
- Age- puberty to 30 years of age
- Site- All teeth are affected
- Severely inflamed tissue
- Spontaneous bleeding
- Suppuration
- Deep pockets
- Attachment and bone loss
- Weight loss
- Mental depression
- General malaise
- Generalized Aggressive Periodontitis Radiographic Features:
- Severe bone loss
- Osseous destruction
Question 3. Vincent infection or ANUG
Answer:
Vincent Infection Or ANUG
- Vincent infection is also known as acute necrotizing ulcerative gingivitis
Vincent Infection Or ANUG Clinical Features
- Gingival hemorrhage
- Fetid odor
- Increased salivation
- Sensitive to pain
- Radiating gnawing pain
- Increased pain on having spicy food
- Metallic foul taste
- Lymphadenopathy
- Fever
- Loss of appetite
Question 4. Micro-organisms causing ANUG
Answer:
Micro-Organisms Causing ANUG
- Causative organisms of ANUG are
- Prevotella intermedia
- Fusobacterium
- Treponema
- Selenomonas species
Question 5. Periodontal abscess
Answer:
Periodontal Abscess
- Papillon Lefevre syndrome is an autosomal recessive inherited disease
Periodontal Abscess Etiology:
- Mutation of chromosome
- Autosomal recessive disorder
Periodontal Abscess Clinical Features:
- Age- before 4 years
- Hyperkeratotic skin lesions
- Calcification of dura
- Early bone loss
- Severe periodontal destruction
- Premature loss of primary and permanent teeth
Question 6. Epulis
Answer:
Epulis
- Epulis refers to solid swelling situated on the gum
Epulis Types:
- Granulomatous epulis
- It manifests as a mass of granulation tissue around the teeth on the gums
- It is a soft to firm fleshy mass and bleeds on touch
- Fibrous epulis
- Arises from the periodontal membrane
- It may undergo a sarcomatous change
- It is firm, polypoidal mass, slow growing, and non-tender
- Giant cell epulis
- It is an osteoclastoma arising in the jaw
- It is present as hyperaemic vascular oedematous, soft to firm gums with indurated mass due to expansion of bone
- It may ulcerate and result in hemorrhage
- Carcinomatous epulis
- This is epithelioma arising from the mucous membrane of the alveolar margin
- It presents as a non-healing painful ulcer
- It slowly infiltrates the bone
Question 7. Staining Of Teeth
Answer:
Staining Of Teeth Causes:
- Intrinsic stains
- Pre-eruptive causes
- Disease- hematological disorders
- Medication-Tetracycline
- Post-eruptive causes
- Pulpal changes
- Trauma
- Aging
- Dental caries
- Pre-eruptive causes
- Extrinsic stains
- Acquiredstains
- Plaque
- Tobacco use
- Poor oral hygiene
- Gingival hemorrhage
- Chemicals
- Chlorhexidine
- Metallic stains
- Acquiredstains
Question 8. Periodontal abscess
Answer:
Periodontal Abscess
- Periodontal abscess is a localized accumulation of pus within the gingival wall of a periodontal pocket
Periodontal Abscess Etiology:
- Presence of plaque and calculus
Periodontal Abscess Clinical Features:
- Involves deep periodontal structures
- Localized pain
- Deep pockets
- Vital tooth
- Tenderon lateral percussion
- Tooth mobility
- Associated fistula
Periodontal Abscess Treatment:
- Drainage
- Flap surgery
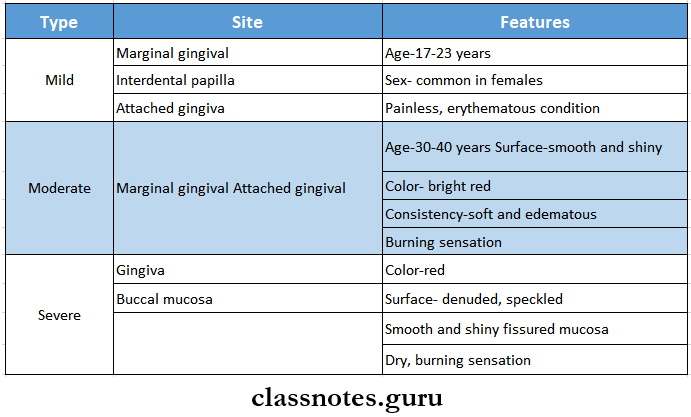
Question 9. Desquamative gingivitis
Answer:
Desquamative Gingivitis
- Desquamative gingivitis is characterized by intense erythema, desquamation, and ulceration of free and attached gingiva
Desquamative gGingivitis Clinical Features:
Question 10. Scorbutic gum
Answer:
Scorbutic Gum
- Scorbutic gum is seen in scurvy, vitamin C deficiency
Scorbutic Gum Clinical Features:
- The site involved- free and attached gingiva
- Color- brilliant red
- Swollen gums
- Spongy in consistency
- The disappearance of lamina dura
- Reduced bone density
- Loss of bony trabeculae
- Mobile teeth
- Impaired healing
- Increased bacterial pathogenicity
Question 11. Granulomatous diseases of periodontium
Answer:
Granulomatous Diseases Of Periodontium
- Granulomatous diseases of periodontium are:
- Eosinophilic granuloma
- Giant cell granuloma
- Wegener’s granulomatosis
- Pyogenic granuloma
Question 12. Dilantin gingival hyperplasia
Answer:
Dilantin Gingival Hyperplasia
- It occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in the maxilla
- The site involved- marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion n Has lobulated surface
- Firm to resilient in consistency
- No tendency to bleed
Question 13. Gum boil or parulis
Answer:
Gum Boil Or Parulis
- A gum boil is defined as a drainage point for an abscessed tooth
Desquamative Gingivitis Etiology:
- Dental caries
- Gum infection
- Failure of root canal treatment
- Weak immune response
Desquamative Gingivitis Features:
- Occurs around the root of the tooth
- Appears as small, red, bulging over gingiva
- When pressed it drains out pus
- Painful swelling
- Earache
- Fever
- A foul taste in my mouth
- Bad breath
Diseases Of The Periodontium Viva Voce
- Epulis fissuratum is caused by ill-fitting dentures
- Stippling is a form of adaptive specialization or reinforcement for the function
- Halitosis is an unpleasant odor exhaled while breathing or talking
- The mandibular third molar is commonly involved tooth in Pericoronitis
- A.a. contains predominate organisms causing chronic periodontitis
- A localized form of aggressive periodontitis is localized to the first molar and incisors
- The generalized form of aggressive periodontitis involves at least 3 teeth other than 1st molar and incisor.
