Diseases Of The Oral Cavity Important Notes
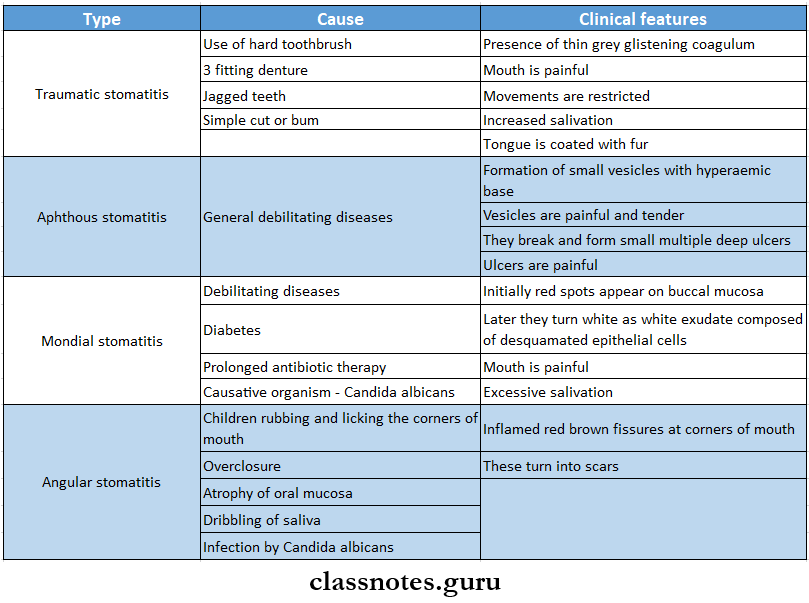
- Stomatitis
- Stomatitis describes inflammation of the lining of the mouth
- Stomatitis Types
Diseases of oral cavity questions and answers
- Cancrumoris
- Progression Of Lesion
- Area of edema and induration on the lip
- The area becomes ischaemic and necrotic
- Spreads over larger areas of lips, cheeks, and jaws and destroys them
- Progression Of Lesion
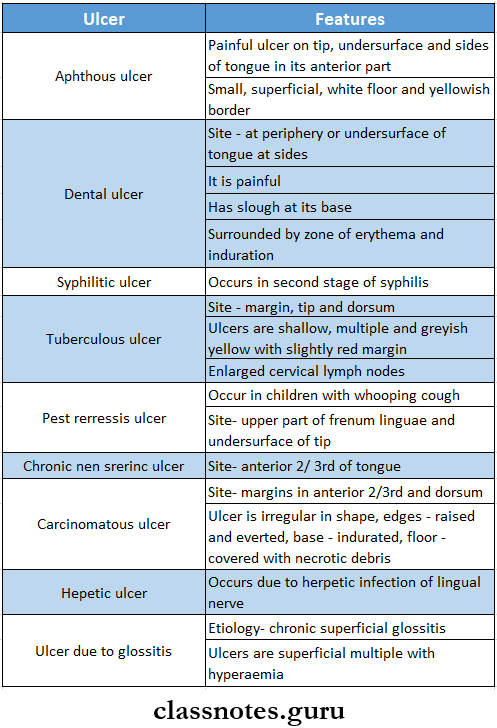
- Ulcers Of Tongue
- Carcinoma Of Tongue
- Sites
- Anierior or 2/ 3rd – 50 %
- Posterior 1 /3rd – 20 %
- Dorsum -10 %
- Tip – 10%
- Undersurface- 10%
- Predisposing Factor
- Pipe smoking
- Syphilis
- Chronic superficial glossitis
- Alcohol
- Chronic irritation
- Carcinoma Of Tongue Types
- An ulcer
- A warty growth
- An indurated plaque or mass
- A fissure
- Carcinoma Of Tongue Feature
- Presents as painless irregular ulcer
- Edges – raised and everted
- Floor – covered by yellowish-grey slough
- Base – indurated
- Repealed spitting
- Excessive salivation
- Fetor oris
- Ankyloglossia
- Hoarseness of voice and dysphagia
- Regional lymphadenopathy
- Later blood stained saliva occurs
- Pain occurs due to the involvement of the lingual nerve
- Presents as painless irregular ulcer
- Carcinoma Of Tongue Treatment
- Surgery
- Radiotherapy
- Block dissection in case of cervical Jymphadenopathy
- Sites
- Carcinoma Of Lip
- In 90% of cases, it involves the lower lip
- Related to exposure to sunlight
- Males are commonly affected
- Present as a flat nodule or indurated crack at skin-vermillion junction
- Etiology Of Carcinoma Of The Cheek
- Sepsis
- Smoking
- Spirit
- Sharp tooth
- Syphilis
- Spices
- Causes Of Macroglossia
- Lymphangioma
- Haemangioma
- Neurofibroma
- Muscular macroglossia
- Primary mesodermal amyloidosis
- Infiltrating carcinoma
Common oral diseases MCQs with answers
Read And Learn More: General Surgery Question and Answers
Diseases Of The Oral Cavity Long Essays
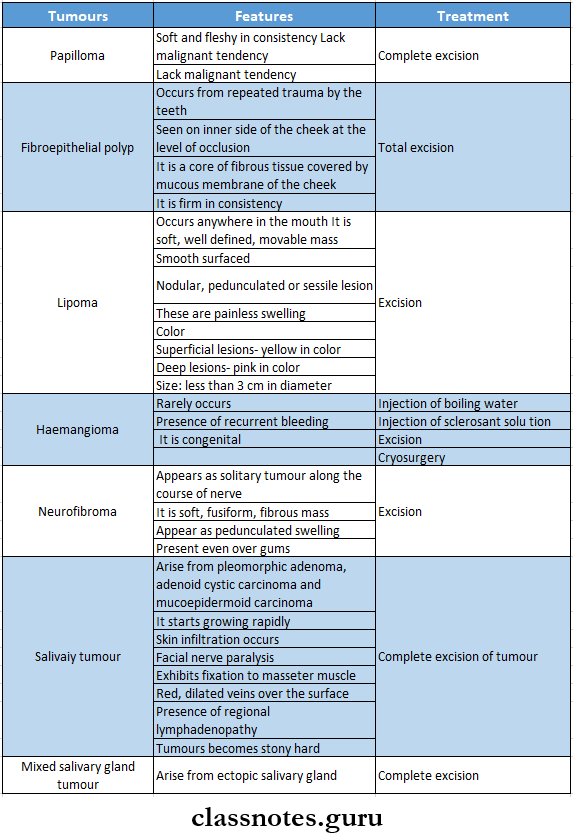
Question 1. Enumerate and write tumors of the cheek and floor of the mouth
Answer:
Tumors Of The Cheek And Floor Of The Mouth
Question 2. Discuss the etiology, clinical features, diagnosis, and management of carcinoma of the tongue.
Answer:
Carcinoma Of Tongue: Carcinoma of the tongue is a common lesion
Carcinoma Of Tongue Etiology:
- Premalignant conditions like
- Leukoplakia
- Erythroplakia
- Six
- Smoking
- Syphilis
- Spices
- Spirit
- Sepsis.
- Sharp tooth
Carcinoma of Tongue Clinical Features
- Age- 50 years of age
- Sex- males are commonly affected
- Site- common in anterior 2/3rd of tongue and edges
- Excessive salivation
- A painless lump or ulcer develops on the surface of the tongue
- Foetor oris
- Ankyloglossia
- Pain due to involvement of nerves
- Hoarseness of voice and dysphagia- if carcinoma involves posterior 1/3rd of tongue
- Enlarged cervical lymph nodes
Dental diseases questions and answers
Carcinoma of Tongue Diagnosis:
- Edge biopsy- done under general anesthesia
- FNAC- of lymph nodes
- Indirect and direct laryngoscopy- to examine posterior third growth
- CT scan to detect extension of carcinoma
- Chest radiograph- to detect bronchopneumonia
Carcinoma of Tongue Management
- Surgery
- Wide incision
- Indicated if the growth is less than 1 cm in diameter
- A wide incision with a 1 cm margin and depth of 1 cm is used
- Partial Glossectomy
- Indicated when the lesion is less than 2 cm and confined to the lateral border of the tongue
- About one-third of the tongue is removed
- Hemiglossectomy
- Indicated when radiotherapy fails
- Removal of half of the anterior 2/3rd of the tongue is done
- Total glossectomy
- Indicated in pervasive growth involving the entire tongue
- Combined with radiotherapy
- Commando Operation
- Indicated when carcinoma of the tongue is fixed to the mandible
- It comprises of
- Hemiglossectomy
- Hemimandibulectomy
- Removal of the floor of the mouth
- Radical neck dissection
- Wide incision
- Radiotherapy
- Interstitial radiotherapy
- Indicated as preliminary treatment when the growth is more than 1 cm in diameter in the anterior 2/3rd of the tongue
- Teletherapy
- Useful in carcinoma of posterior l/3rd of the tongue when the lesion is larger than 2 cm in diameter
- Cobalt 60 unit is used
- When there is a large tumor, both the primary site and neck are irradiated to 4500 rads
- Interstitial radiotherapy
- Chemotherapy
- Amethoprin- 50 mg/ day for 5 days can be used to reduce the size of the tumor
- Treatment of lymph node
- When lymph nodes are not enlarged- prophylactic block dissection of the neck is done
- When lymph nodes are enlarged- Commando’s operation is carried out
- When enlarged lymph nodes are fixed- deep radiotherapy is done
Oral cavity disorders short questions
Question 3. Describe the etiology, clinical features, diagnosis, and treatment of carcinoma of the cheek.
(or)
Describe the etiology, and pathology of carcinoma of the cheek and how you will manage it if it involves the mandible
Answer:
Carcinoma Of Cheek: Squamous cell carcinoma is a common carcinoma of the cheek
Carcinoma Of Cheek Etiology:
- Six Ss
- Smoking
- Spirit
- Spices
- Sharp tooth
- Sepsis
- Syphilis
- Premalignant Conditions
- Leukoplakia
- Erythroplakia
- Hyperplastic candidiasis
- Submucosal fibrosis
- Betel Nut Chewing
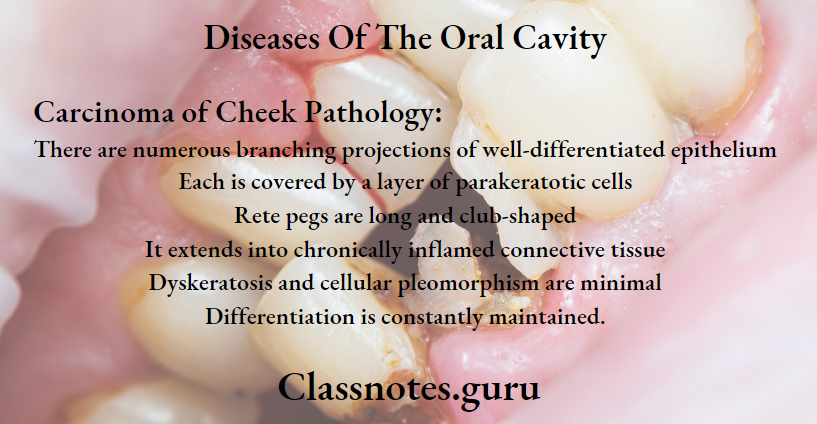
Carcinoma of Cheek Clinical Features:
- Development of exophytic growth- cauliflower-like growth
- Nonhealing ulcer develops
- Edges are everted
- Ulcer bleeds on touch
- Pain occurs when it is infected
- Fixity to underlying structures
- Trismus
- Dysphagia
- Halitosis
- Enlargement of submandibular and upper deep cervical lymph nodes
Carcinoma of Cheek Diagnosis:
- Wedge biopsy
- OPG- to rule out an extension
- FNAC- from lymph nodes
- CT scan- to detect extension
Carcinoma of Cheek Treatment
- Surgery
- Wide excision followed by split skin graft for small superficial ulcer
- Wide excision followed by flap reconstruction for infiltrative ulcer
- Radiotherapy
- External radiotherapy
- Large total doses of 6000-8000 cGy units are given
- Interstitial radiotherapy
- Indicated in infiltrative small lesions
- External radiotherapy
- Advanced Carcinoma Of The Cheek
- T3 and T4 lesions require surgery followed by postoperative radiotherapy
- Repaired by myocutaneous flap
- Reconstruction after surgery can be done by
- Split skin graft
- Deltopectoral cutaneous flap
- Forehead flap
- Pectoralis major myocutaneous flap
- Cortical bone graft
- Free flaps
- Chemotherapy
- Drugs used are
- Methotrexate
- Vincristine
- Bleomycin
- Adriamycin
- Drugs used are
Oral diseases viva questions
Question 4. Discuss the etiology, pathology, and clinical features of oral carcinoma and the management of gingival carcinoma
Answer:
Oral Carcinoma It is the common malignant neoplasm in the head and neck region
Oral Carcinoma Etiology:
- Tobacco smoking
- Use of smokeless tobacco
- Alcohol consumption
- Malnutrition
- 3 fitted dentures
- Radiations
- Viral Infections
- Immunosuppression
- Chronic infections
- Occupational hazards
- Genetic factors
- Pre-existing oral diseases
Oral Carcinoma Pathology: It is characterized by malignant cells
- These cells show variable degrees of differentiation
- Cells Invade through the basement membrane into the dermis
Oral Carcinoma Arrangement:
- Cellfi arc arranged in concentric layers called epithelial pearls
- They contain keratin material in the center of the coll masses
- Cells are separated by lymphocytes
Oral Carcinoma Clinical Features:
- Associated with oral leukoplakia and erythroplakia
- Initial Symptoms are
- Asymptomatic
- White or rod, variegated patch
- Nodule or fissure over oral mucosa
- Painless
- Later Symptoms
- Past enlarging
- Exophytic or invasive ulcer
- Persistent induration around the periphery
- Presence of superadded candidal infections
- Painful lesions due to secondary infections
- Fixation to the underlying tissues
- Trismus
- Invasion of the alveolar bone
- Enlarged regional lymph nodes
- Pathological fractures of the jaw bone
Gingival Carcinoma: Occurs due to tobacco and betel nut chewing
Gingival Carcinoma Management:
- Surgical excision
- Radiotherapy
- Chemotherapy
BDS oral pathology questions and answers
Question 5. Discuss differential diagnosis, clinical features, and management of gum swelling.
Answer:
Gum Swelling Differential Diagnosis:
- Chronic gingivitis
- Gingival abscess
- Periodontitis
Gum Swelling Clinical Features:
- Mandibular gingiva is more affected than maxilla
- The attached gingiva Is more affected than the free gingiva
- The initial lesion appears as verrucous leukoplakia or as a small ulceration with an indurated margin
- bony invasion occurs
- Mobility and premature loss of teeth
- Nonhealing extraction socket
- Extends to the neighboring structures
Gum Swelling Management:
- Surgical excision
- Radiotherapy
- Chemotherapy
Question 6. Discuss the etiology of oral cancer and how to detect nearly oral cancer and describe the steps to prevent it.
Answer:
Oral Cancer It is the common malignant neoplasm in the head and neck region
Oral Cancer Etiology:
- Tobacco Smoking
- Cigarettes
- Bidis
- Pipes
- Cigars
- Use Of Smokeless Tobacco
- Snuff dipping
- Gutkha
- Tobacco chewing
- Alcohol Consumption
- Malnutrition
- Vitamin deficiency
- 3 fitted Dentures
- Broken prosthesis
- Chronic irritation
- Radiations
- Actinic radiation
- X-ray radiation
- Viral Infections
- Herpes simplex virus
- Human papilloma virus
- Human immunodeficiency virus
- Epstein burr virus
- Immunosuppression
- AIDS
- Organ transplants
- Chronic Infections
- Candidiasis
- Syphilis
- Occupational hazards
- Genetic factors
- Pre-existing oral diseases
Oral Cancer Investigation
- Histopathological Examination
- Exhibit excessive proliferation of malignant cells
- Cellular pleomorphism
- Xuclear hyperchromatic
- Breakdown of basement membrane
- Intense inflammatory cell infiltration
- Radiographic Examination
- Exhibits bone destruction
- Shows ill-defined radiolucent areas
- Expansion and destruction of cortical plates
- Pathological fractures of bone
- Exfoliative Cytology
- Used to detect the neoplastic cells as these cells tend to exfoliate or shed to the surface
- Toluidine Blue Test
- Detects dysplastic changes
- Acridine Binding Method
- Detects dysplastic cells
- DNA Probe
- Help to determine the DNA content of tumor cells
- Tumor Markers
- Carcinoembryonic antigen and alpha-fetoprotein are tumor markers that detect tumor
Oral Cancer Prevention:
- Primary Prevention
- Avoid exposure to tobacco and other deleterious habits
- Primary Prevention Methods
- Reducing tobacco habits by making tax hikes for tobacco-related products
- Making changes in the manufacturing process of tobacco items
- Secondary Prevention
- It Includes
- Early detection and treatment of already-developed cancer
- Prompt management of potentially risky precancerous lesions and conditions
- Treatment of early cancer
- It Includes
Oral lesions questions and answers
Question 7. Define oral ulcer. Classify ulcers. Discuss the differential diagnosis of ulcers of the oral cavity and management of ulcers of the palate.
Answer:
Oral Ulcer Ulcer is a break in the continuity of the covering epithelium
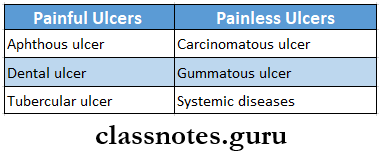
Oral Ulcer Classification:
- Clinically
- Spreading ulcer
- Healing ulcer
- Callous ulcer
- Pathological
- Nonspecific Ulcer
- Traumatic ulcer
- Arterial ulcer
- Venous ulcer
- Neurogenic user
- Infective ulcer
- Specific Ulcer
- Syphilitic ulcer
- Tubercle ulcer
- Malignant Ulcer
- Epithelioma
- Rodent ulcer
- Nonspecific Ulcer
Oral Ulcer Differential Diagnosis:
- Aphthous Ulcer
- It is a small painful ulcer seen on the tip, undersurface, and sides of the tongue in its anterior part
- It is small and superficial
- Surrounded by a hyperaemic zone
- It is quite painful
- Has yellowish border
- It is a painful ulcer
- Dental Ulcer
- Caused by mechanical irritation
- Occurs at the periphery or undersurface of the tongue
- It is elongated
- Presents a slough at the base and is surrounded by a zone of erythema and induration
- It is painful
- Syphilitic Ulcer
- Called snail track ulcer
- Occurs rarely on the tongue
- Tuberculous Ulcer
- Young adults are affected
- Ulcers are shallow, multiple, and greyish-yellow in color
- Seen at the tip, margin, and dorsum of the tongue
- Post Pertussis Ulcer
- Occurs in children with whopping cough
- Seen at the upper part of frenum linguae and undersurface of the tip
- Chronic Nonspecific Ulcer
- Occurs in the anterior 2/3rd of the tongue
- It is moderately indurated
- Painless
- Carcinomatous Ulcer
- Occurs in elder persons
- The site involves- the anterior 2/3rd of the tongue
- It may be a single or multiple
- Herpetic Ulcer
- Common in children and young adults
- Associated with acute neuralgic pain
- Vesicles appears
- Ulcers Due To Glossitis
- Ulcers are superficial and multiple with hyperemia
- Pain occurs during meals
Management of Ulcer of Palate:
- Removal of the causative agent
- The membrane is swabbed away with pledgets of cotton soaked with hydrogen peroxide
- Mouth should be kept clean by repeated use of mouthwash
- Antibiotics used if required
Question 8. Surgical anatomy of the maxillary sinus, clinical features and management of maxillary sinusitis
Answer:
Maxillary Sinus: It is pyramidal with a base forming the lateral nasal wall and an apex at the root of the zygoma.
- Capacity: 10-15 ml
- Size: Height 3.5 cm; Width 2.5 cm; Anteroposterior depth 3.2 cm
- Roof: Formed by the floor of the orbit
- Floor: Alveolar process of maxilla
- Anterior Wall: Facial surface of maxilla
- Posterior Wall: Sphenomaxillary wall
Medial Wall: Lateral wall of nasal cavity
Vascular And Nerve Supply:
- Blood Supply: Facial artery
- Infraorbital artery
- Greater palatine artery
- Nerve Supply:
- Infraorbital nerve
- Anterior, middle, and posterior superior alveolar nerves
- Lymphatic Drainage: Submandibular lymph nodes
Maxillary Sinusitis Clinical Features:
- Pain on lowering your head
- Tenderness in canine fossa
- Redness of the area
- Nasal discharge
- Nose block
- Change in voice
- Dry cough
- Fever
- Malaise
- Headache
Maxillary Sinusitis Management:
- Antibiotics:
- Decongestants:
- Analgesics
- Antihistamines
- Steam inhalation
- Local heat application
- Antral lavage
- Irrigation of sinus through lukewarm water
Oral cavity diseases long and short questions
Question 9. What are the causes of oral malignancy? How do you manage carcinoma of the cheek?
Answer:
Causes of Oral Malignancy
- Tobacco Smoking
- Cigarettes
- Bidis
- Pipes
- Cigars
- Use Of Smokeless Tobacco
- Snuff dipping
- Guikha
- Tobacco chewing
- Alcohol Consumption
- Malnutrition
- Vitamin deficiency
- 3 fitted Dentures
- Broken prosthesis
- Chronic irritation
- Radiations
- Actinic radiation
- X-ray radiation
- Viral Infections
- Herpes simplex virus
- Human papilloma virus
- HIV
- Epstein Burr virus
- Immunosuppression
- AIDS
- Organ transplants
- Chronic Infection
- Candidiasis
- Syphilis
- Occupational Hazards
- Genetic Factors
- Pre-Existing Oral Diseases
Diseases Of The Oral Cavity Short Essays
Question 1. Stomatitis
Answer:
Stomatitis
- Stomatitis used to describe any kind of inflammation of the lining of the mouth
- It may affect the surface of the tongue
Stomatitis Causes:
- Trauma
- Mechanical
- Chemical agents
- Thermal injury
- Radiotherapy
- Idiopathic
- Malnutrition
Stomatitis Types:
- Traumatic Stomatitis
- It is covered by a thin grey glistening coagulum
- It heals on its own
- Aphthous Stomatitis
- May be solitary or multiple
- Small vesicles with hyperaemic base appear
- These are painful and tender
- These vesicles break and form painful ulcers
- Monilial Stomatitis
- Occurs due to Candida albicans
- Starts as a spot on the buccal mucosa
- Excessive salivation occurs
- Swallowing is painful
- Occurs due to Candida albicans
- Recurrent Aphthous Ulceration
- Seen in adults
- Seen on the inner sides of the lips and cheek and the undersurface of the tongue
- These recur in different parts of the mouth
- Ulcers are very painful
- There is excessive salivation
- They heal on their own
Question 2. Erythroplakia
Answer:
Erythroplakia
- Erythroplakia is a red patch or plaque which cannot be characterized clinically or pathologically as any other condition and which has no apparent cause
- Erythroplakia has clearly defined margins
Erythroplakia Types:
- Homogenous Erythroplakia
- The lesion appears bright red, velvety soft areas on the oral mucosa
- Has irregular but well-defined margins
- Erythroplakia Interspersed With Patches Of Leukoplakia
- There is the presence of multiple, irregular erythematous areas
- Few white leukoplakic patches occur
- Speckled Erythroplakia
- There is the presence of soft, irregular, raised, erythematous areas in the epithelium with a granular surface
- There are some tiny, focal white plaques distributed all over red surfaces
Erythroplakia Differential Diagnosis
- Erosive lichen planus
- Early squamous cell carcinoma
- Atrophic candidiasis
- Kaposi’s sarcoma
- Contact allergy
Erythroplakia Treatment:
- Deep and wide surgical excision of the lesion
- Regular follow up
Oral mucosal diseases questions
Question 3. Carcinoma of lip
Answer:
Carcinoma Of Lip Clinical Features:
- Age/sex: elderly males
- Non-healing ulcer
- Edge is everted
- Induration present
- The floor is covered with slough
- Bleeding spots present
- Fix to underlying subcutaneous tissue
- Cervical Lymphadenopathy
Carcinoma Of Lip Differential Diagnosis:
- Keratoacanthoma
- Ectopic salivary gland tumour
- Pyogenic granuloma
- Leukoplakia
Carcinoma Of Lip Treatment:
- Surgery:
- Abbe flap
- Estlander flap
- Radiotherapy
- Dose: 4000-6000 cGv units
Question 4. Etiology, clinical features, and management of malignant sinusitis
Answer:
Malignant Sinusitis Etiology
- Genetic mutation
- Smoking
- Long-term exposure to chemicals and irritants
- Infections like human papillomavirus
Malignant Sinusitis Clinical features
- Difficulty breathing through the nose
- Loss of sense of smell
- Nose bleed
- Discharge from nose
- Facial pain and swelling
- Watery eyes
- A sore or lesion on the roof of the mouth
- Vision problems
- Lump in neck
- Difficulty in the opening of the mouth
Questions on dental caries and oral infections
Question 5. Write about Leukoplakia
Answer:
Leukoplakia
Leukoplakia is a whitish patch or plaque that cannot be characterized, clinically or pathologically, as any other disease and which is not associated with any other physical or chemical causative agent except the use of tobacco.
Leukoplakia Etiology:
- Smoking
- Spices
- Spirits
- Sharp tooth
- Sunlight
- Syphilis
Leukoplakia Stages
- Keratosis
- Acanthosis
- Dyskeratosis
- Speckled leukoplakia
- Carcinoma in situ
Leukoplakia Treatment
- Stoppage of all habits
- Surgical excision
- Cryosurgery
- Administration of vitamin A
Diseases Of The Oral Cavity Short Answers
Question 1. Angular stomatitis
Answer:
Angular Stomatitis
Angular Stomatitis is a superficial ulceration at the corner of the mouth
Angular Stomatitis Causes:
- Licking the corners of the mouth
- Over closure
- Dribbling of saliva
- Atrophic oral mucosa
Angular Stomatitis Clinical Features:
- Inflamed red-brown fissures at the comer of the mouth
- Results in scar formation
Angular Stomatitis Treatment:
- Improve general health
- Application of mercurochrome or Gentian violet B Vitamin supplement
- Iron supplements
Question 2. Tongue tie
(or)
Ankyloglossia
Answer:
Tongue Tie
Tongue Tie is a congenital developmental condition characterized by fixation of the tongue to the floor of the mouth
Tongue Tie Clinical Features:
- Males are commonly affected
- Defective speech
- Dental deformities
- Difficulty in sucking
- Difficulty in swallowing
- Tension in anterior lingual gingiva
Tongue Tie Treatment:
- Frenulectomy- in severe cases of ankyloglossia
Fungal infections of oral cavity questions
Question 3. Cancrum Oris
Answer:
Cancrum Oris
Cancrum Oris is an extensive ulcerative disease of cheek mucosa occurring in malnourished children
Cancrum Oris Precipitating Factors:
- Malnutrition
- Major diseases like diphtheria
- Vincent’s organism
Cancrum Oris Treatment:
- Ryle’s tube-feeding
- Improve the nutrition
- Antibiotics: metronidazole-400 mg TID for 7-10 days
- Reconstructive surgery
Cancrum Oris Complications:
- Fibrosis
- Septicaemia
- Restricted jaw movement
- Death
Question 4. Lingual thyroid
Answer:
Lingual Thyroid
- Lingual thyroid is a round red swelling seen at the back of the tongue at the foramen caecum
- The lingual thyroid contains thyroid tissue at the foramen caecum
Lingual Thyroid Complications:
- Hemorrhage
- Respiratory obstruction
- Dysphagia
- Speech impairment
Lingual Thyroid Treatment: L-thyroxin replacement therapy- to reduce the size of the swelling
Salivary gland disorders questions
Question 5. Ulcers Of Tongue
Answer:
Ulcers Of Tongue
- Aphthous Ulcer
- It is a small painful ulcer seen on the tip, undersurface, and sides of the tongue in its anterior part
- It is small and superficial
- Surrounded by a hyperaemic zone
- Dental Ulcer
- Caused by mechanical irritation
- Occurs at the periphery or undersurface of the tongue
- Syphilitic Ulcer
- Called snail track ulcer
- Occurs rarely on the tongue
- Tuberculous Ulcer
- Ulcers are shallow, multiple, and greyish-yellow in color
- Seen at the tip, margin, and dorsum of the tongue
- Post pertussis Ulcer
- Occurs in children with whopping cough
- Seen at the upper part of frenum linguae and undersurface of the tip
- Chronic Nonspecific Ulcer
- Occurs in the anterior 2/3rd of the tongue
- It is moderately indurated
- Carcinomatous Ulcer
- Occurs in elder persons
- The site involves- the anterior 2/3rd of the tongue
- It may be a single or multiple
- Herpetic Ulcer
- Common in children and young adults
- Associated with acute neuralgic pain
- Vesicles appear
- Ulcers Due To Glossitis
- Ulcers Are Superficial And Multiple With Hyperemia
- Pain Occurs During Meals
Question 6. Haemangioma of tongue
Answer:
Haemangioma Of Tongue
- Cavernous haemangioma occurs on tongue
- Arises from veins
- It consists of multiple dilated venous channels
- It is a spongy swelling
Haemangioma Of Tongue Management:
- Conservative Treatment
- Injection of sclerosing agent
- Cautery
- Surgery
- Ligation of feeding vessels
- Excision of the lesion
- Diathermy to control hemorrhage
Oral manifestations of systemic diseases Q&A
Question 7. Predisposing factors- carcinoma of the tongue
Answer:
Predisposing Factors- Carcinoma Of TheTongue
- Predisposing factors of carcinoma of the tongue are
- Pipe smoking
- Syphilis
- Chronic superficial glossitis
- Alcohol
- Chronic irritation
- Betel nut
Question 8. Glossitis
Answer:
Glossitis
Involvement of the tongue due to any cause with or without inflammation is called glossitis
Glossitis Causes:
- Local Causes
- Mechanical trauma
- Mechanical irritation
- Allergic reaction
- Dry mouth
- Systemic Causes
- Herpes simplex virus
- Iron deficiency anemia
- Aphthous ulcer
- Oral lichen planus
- Pemphigus Vulgaris
Glossitis Clinical Features:
- Pain and tenderness in the tongue
- Swelling in the tongue
- Color changes to beefy dark red or pale
- Halitosis
- Difficulty in speech, eating, and swallowing
- Loss of papillae on the tongue
Question 9. Sinusitis
Answer:
Sinusitis Etiology:
- Nasal infections
- Dental infections
- Trauma
Sinusitis Causative Organisms:
- Streptococcus
- Pneumococci
- Staphylococci
- Clinical Features:
- Pain on lowering your head
- Tenderness in canine fossa
- Redness of the area
- Nasal discharge
- Nose block
- Change in voice
- Dry cough
- Fever
- Malaise
- Headache
Question 10. Anaplasia
Answer:
Anaplasia Definition:
- Anaplasia is a lack of differentiation and is a characteristic feature of most malignant tumors.
- Depending upon the degree of differentiation, the extent of anaplasia is also variable i.e., poorly differentiated malignant tumors have a high degree of anaplasia.
Result of Anaplasia:
- Loss of polarity
- Pleomorphism
- N: C ratio changes from 1:5 to 1:1
- Anisonucleosis.
- Hyperchromatism.
- Prominent nucleolus
- Tumorgaint cells
- Chromosomal abnormalities.
Oral cancer signs symptoms questions
Question 11. Metaplasia
Answer:
Metaplasia Definition: Metaplasia is defined as a reversible change of one type of epithelial or mesenchymal adult cells to another type of adult epithelial or mesenchymal cells, usually in response to abnormal stimuli.
Metaplasia Types: Metaplasia is divided into the following two types.
- Epithelial Metaplasia
- Squamous metaplasia
- Columnar metaplasia
- Mesenchyme Metaplasia
- Osseous metaplasia
- Cartilaginous metaplasia
Question 12. Oral thrush
Answer:
Oral Thrush Features:
- The lesions appear soft, white, and slightly elevated plaques
- The Sites Involved Are:
- Buccal mucosa
- Tongue
- Gingiva
- Palate
- The floor of the mouth
- Entire oral cavity’ is involved in severe cases
Oral Thrush Person Affected Arc
- HIV patients
- Cancer patients undergoing chemotherapy or radiotherapy
- Neonates and infants
- Debilitated and chronically ill patients
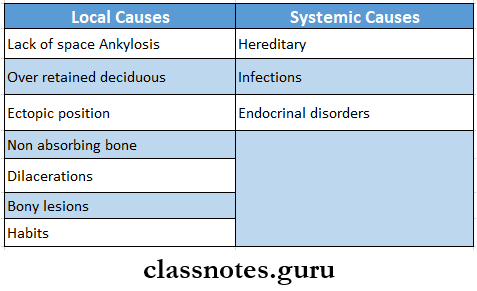
Question 13. Impacted teeth
Answer:
Impacted Teeth Definition: It is the cessation of the eruption of a tooth caused by a physical barrier or ectopic positioning of a tooth
Impacted Teeth Causes:
Question 14. Micrognathia
Answer:
Micrognathia
Micrognathia is an orofacial anomaly characterized by the development of jaws smaller than normal
Micrognathia Causes:
- Pierre- Robin syndrome
- Hallerman- Steriff syndrome
- Trisomy 13
- Trisomy 18
- Turner syndrome
- Marfan syndrome
- Progeria
Micrognathia Types:
- Pseudo micrognathia
- True micrognathia
Micrognathia Clinical Features:
- Defective alignment of teeth
- Crowding
- Malocclusion
- Retruded chin
- Difficulty in feeding
- Difficulty in speech
Question 15. Macroglossia
Answer:
Macroglossia
Macroglossia is characterized by an abnormally large tongue in the oral cavity
Macroglossia Types:
- Congenital
- Acquired
Macroglossia Clinical Features:
- Causes displacement of teeth
- Develops tongue-thrusting habits
- Results in obstructive sleep apnea
- Spacing in teeth
- Distortion of the mandibular arch
- The lateral margin of the tongue exhibits scalloping indentation
- Defective speech
- Unesthetic appearance
Macroglossia Treatment:
- Removal of the causative agent
- Surgical reduction or trimming
Multiple choice questions on precancerous oral lesions
Question 16. Giant cell epulis
Answer:
Giant Cell Epulis
- Peripheral giant cell granuloma is also called giant cell epulis
- It appears in the mouth as an overgrowth of tissue due to irritation or trauma
- They frequently appear on gingiva Color ranges from red to bluish-purple
- It can be pedunculated or sessile
- Common in females
- More often found over the mandible rather than the maxilla
- The underlying alveolar bone can be destroyed resulting in cauterization
- Treatment involves surgical removal of bone
Clinical case-based questions on oral infections
Question 17. Causes of Macroglossia
Answer:
Causes of Macroglossia
Macroglossia is an abnormally large tongue
Question 18. Subacute osteomyelitis
Answer:
Subacute Osteomyelitis
- It is a chronic low-grade infection of bone characterized by lack of systemic manifestation
- The causative organism is Staphylococcus
- The onset is insidious
- Pain is a common symptom
- Swelling and tenderness over the involved area are seen
- Subacute Osteomyelitis Treatment
- Surgical debridement
- Antibiotics
Diseases Of The Oral Cavity Viva voce
1. Cancrum Oris is associated with leukemia
2. Carcinoma of the lip commonly occurs over the lower lip
