Diseases Of Salivary Glands Important Notes
- Sialolith
- Mostly Occurs In Submandibular Glands Due To
- Highly viscous secretion
- Presence of gland gland-independent position
- Alkaline secretion with a high concentration of calcium and phosphate ions
- Gland duct is torturous
- Sialolith Complications
- Ductal stricture
- Acute sialadenitis
- Ductal dilation
- Sialolith Treatment
- Small stones are removed by manipulation
- Larger stones are removed by transoral sialolithotomy
- Mostly Occurs In Submandibular Glands Due To
- Nerves That Are At Risk During Submandibular Gland Excision Are
- Marginal mandibular branch of facial nerve
- Lingual nerve
- Hypoglossal nerve
- Classification Of Salivary Gland Tumours
- Based On Spread of Tumours
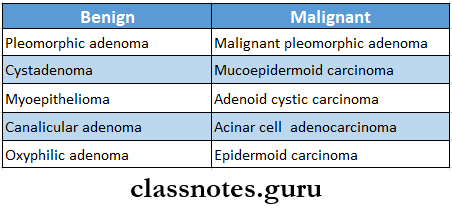
- Histological Classification
- Adenoma
- Pleomorphic
- Myoepithelioma
- Basal cell adenoma
- Warthin’s tumours
- Canalicular adenoma
- Cystadenoma
- Adenoma
- Carcinoma
- Acinic cell carcinoma
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Adenocarcinoma
- Squamous cell carcinoma
- Nonepithelial tumour
- Malignant lymphomas
- Secondary tumours
- Unclassified
- Tumor like lesions
- Sialoadenesis
- Oncocytosis
- Necrotizing sialometaplasia
- Salivary gland cyst
- Based On Spread of Tumours
- Malignant Transformation Of Pleomorphic Adenoma Occurs When Tumour
- Becomes painful
- Starts growing rapidly
- Feels stony hard
- Gets fixed
- Cervical lymph nodes get enlarged
- Causes restriction of movements of the jaws
- Mucous Retention Cyst And Ranula
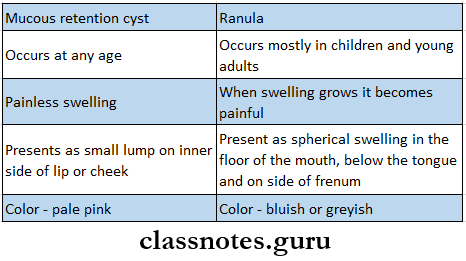
- Types Of Ranula
- Simple – ranula situated in the floor of the mouth without cervical prolongation
- Deep/plunging ranula – intra buccal ranula with cervical prolongation
- Complications Of Ranula
- Infection
- Bursting
- Repeated trauma
- Difficult in speech arid eating
- Causes Of Xerostomia
- Chronic anxiety and depression
- Dehydration
- Antimuscarinic and sympathomimetic drugs
- Salivary gland diseases like Sjogren’s syndrome
- Nutritional deficiencies
- Causes Of Sialorrhoea
- Painful oral ulcers
- Dentures
- Parkinson’s disease
- Atropine
Diseases of salivary glands question and answers
Diseases Of Salivary Glands Long Essays
Question 1. Describe clinical features, diagnosis, and management of carcinoma of the parotid gland and classify salivary gland tumors
Answer:
Carcinoma Of Parotid Gland: It consists of 70% of the salivary tumors
Carcinoma Of Parotid Gland Clinical Features:
- It starts growing rapidly
- Skin infiltration occurs
- Facial nerve paralysis
- Exhibits fixation to the masseter muscle
- Red, dilated veins over the surface
- Presence of regional lymphadenopathy
- Tumours become stony hard
Read And Learn More: General Surgery Question and Answers
Carcinoma Of Parotid Gland Investigations:
- Fine needle aspiration cytology
- It is done to confirm the diagnosis and rule out malignancy
- Diagnostic imaging techniques
- Radiograph of the bones- shows bone resorption
- Computrer tomography
- It allows direct, bilateral visualization of the salivary gland tumor and detects overall dimension and tissue invasion
- Demonstrate bony invasion
- Define extra glandular spread and cervical lymph node
- Magnetic resonance imaging
- Provides superior soft tissue delineation such as perineural invasion
Carcinoma of Parotid Gland Treatment:
- Radical Parotidectomy
- Includes removal of both the lobes of the parotid gland, facial nerve, parotid duct, fibres of the masseter, buccinator, pterygoids, and radical block dissection of the neck
- Postoperative Radiotherapy
- Indications
- If the deep lobe is involved
- If the lymph nodes are involved
- High-grade tumors
- If margins are positive
- Indications
Carcinoma Of Parotid Gland Classification:
- Epithelial Tumors:
- Adenomas
- Pleomorphic adenoma
- Cystadenoma
- Basal cell adenoma
- Warthin’s tumour
- Carcinoma
- Adenocarcinoma
- Epidermoid carcinoma
- Nonepithelial Tumours:
- Fibroma
- Lipoma
- Lymphoma
- Malignant Lymphoma
- Secondary Tumours
- Unclassified Tumors
- Tumour Like Lesions
- Sialadenitis
- Oncocytosis
- Necrotizing sialometaplasia
BDS salivary gland diseases questions
Question 2. What is mixed parotid tumor? Give clinical features and its management
Answer:
Mixed Parotid Tumour: Pleomorphic adenoma is called mixed parotid tumour
Mixed Parotid Tumour: Clinical Features:
- Age: 5th and 6th decade
- Sex: common in females
- Site: common in parotid gland
Mixed Parotid Tumour: Features:
- Slow growing
- Exophytic growth
- Solitary lesion
- Swelling of gland
- Smooth surface of the lesion
- No pain
- Superficial lesions
- Located near the angle of the mandible
- Deeper lesions:
- Over the lateral wall of oropharynx
- Minor gland neoplasms exhibit firm, nodular swelling
- Palatal lesion causes surface ulceration
- In buccal mucosa it is present as small, painless nodular lesion
Mixed Parotid Tumour: Investigation
- Duration of the lesion:
- Longer duration- malignancy
- Nature of onset
- Gradual and painless- malignant
- Sudden and painful- inflammatory
- Rapidity of growth
- Slow-benign
- Rapid- malignant
- Associated symptoms
- Discharge of pus
- Dryness of mouth
- Constitutional symptoms
- FNAC- to rule out malignancy
- CT Scan- for deeper lesions
- FNAC- for lymph nodes involvement
- X-ray of bone- for resorption
Mixed Parotid Tumour: Treatment:
- Surgical excision-parotidectomy
- It is a surgical treatment for salivary gland tumours
Mixed Parotid Tumour: Types:
- Superficial Parotidectomy
- Anesthetized
- Incision over the preauricular crease, curved downward upto tip of mastoid
- Elevation of skin and superficial fascia
- Preserve the facial nerve
- Dissect the gland away from each branch of gland
- Hemostasis
- Placement of drains
- Suturing
- Total Parotidectomy
- Involves removal of entire parotid gland
- Superficial parotidectomy done
- Then remove tumour deep to the facial nerve
Oral pathology salivary gland disorders questions
Question 3. What are the causes of acute parotitis? Describe its clinical features and management.
Answer:
Acute Parotitis: It is an acute inflammation of the salivary gland
Acute Parotitis Etiology:
- It is caused by Staphylococcus aureus
- Factors causing it are:
- When the salivary flow is reduced
- Partial obstruction of the duct with retention of secretions
Acute Parotitis Clinical Features:
- Pain and swelling of the side involved D There is brawny oedematous swelling over the parotid region
- The temperature is high n Cellulitis occurs on the overlying skin
- Pus may come out through the internal opening of the parotid gland
Acute Parotitis Management:
- Improve the general health of the patient and Maintain oral hygiene
- A soft diet should be prescribed and Antibiotics are started
- Gentle parotid massage is done at regular intervals
- Drainage of pus
Question 4. Describe the pathology, clinical features, and management of submandibular salivary calculus.
Answer:
Submandibular Salivary Calculus Clinical Features:
- Age: middle-aged adults
- Sex: common in males
Submandibular Salivary Calculus Pathology:
- Site: common in the submandibular gland due to the following:
- Due to viscous secretion
- Higher concentration of calcium and phosphate
- Tortuous anatomy of the ducts
- Dependent position of the gland
Submandibular Salivary Calculus Features:
- Recurrent swelling of the gland region
- Recurrent episodes of sialadenitis
- Tense and tender gland
- Aggregates at the mealtime
- Type of pain: pulling or drawing sensation
- Severe, stabbing type
- Enlarged gland
- Location: unilateral
- In chronic cases: the formation of fistulas, sinus tracts, and ulcerations in the area
- Necrosis of the gland acini
- Lobular fibrosis
- Complete loss of secretion of the gland
- So there is an increased risk of infections
Submandibular Salivary Calculus Diagnosis:
- Manual palpation
- Occlusal radiograph in case of the submandibular gland
- Sialography
Submandibular Salivary Calculus Treatment:
- Locate the sialolith radiographically
- Suture behind and below the duct to prevent the spillage of stone
- If sialolith is present posteriorly, incision is given medially
- If sialolith is present anteriorly, an incision is placed medial to plicasublingualis
- Locate the duct
- Locate the stone
- Incise over the stone
- Remove it through the forceps
Salivary gland diseases MCQs with answers
Question 5. Discuss in detail about salivary gland tumors of clinical features, investigations, pathology, management, and complications of pleomorphic adenoma of parotid gland
Answer:
Pleomorphic Adenoma Clinical Features:
- Age: 5th hand 6th decade
- Sex: common in females
- Site: common in parotid gland
Pleomorphic Adenoma of Parotid Gland Features:
- Slow growing
- Exophytic growth
- Solitary lesion
- Swelling of gland
- Smooth surface of the lesion
- No pain
- Superficial lesions
- Located near the angle of the mandible
- Deeper lesions:
- Over the lateral wall of the oropharynx
- Minor gland neoplasms exhibit firm, nodular swelling
- The palatal lesion causes surface ulceration
- In buccal mucosa, it is present as a small, painless nodular lesion
Pleomorphic Adenoma of Parotid Gland Pathology:
- Pleomorphic adenoma is a benign parotid tumour
- It is derived from a mixture of epithelial and myoepithelial cells
- The tumor has three components
- Epithelial cell component
- Myoepithelial cell component
- Stromal component
- Pleomorphic Adenoma of Parotid Gland Investigation:
- Duration of the lesson:
- Longer duration- malignancy
- Nature of onset
- Gradual and painless- malignant
- Sudden and painful- inflammatory
- Rapidity of growth
- Slow- benign
- Rapid- malignant
- Associated symptoms
- Discharge of pus
- Dryness of mouth
- Constitutional symptoms
- FNAC- to rule out malignancy
- CT Scan- for deeper lesions
- FNAC- for lymph node involvement
- X-ray of bone- for resorption
- Duration of the lesson:
Pleomorphic Adenoma of Parotid Gland Treatment:
- Surgical excision-parotidectomy
- It is a surgical treatment for salivary glands tumors
Pleomorphic Adenoma of Parotid Gland Types:
- Superficial parotidectomy
- Anesthetized
- Incision over the pre auricular crease, curved downward upto tip of mastoid
- Elevation of skin and superficial fascia
- Preserve the facial nerve
- Dissect the gland away from each branch of gland
- Hemostasis
- Placement of drains
- Suturing
- Total parotidectomy
- Involves removal of entire parotid gland
- Superficial parotidectomy done
- Then remove tumour deep to the facial nerve
Pleomorphic Adenoma of Parotid Gland Complication:
- Facial palsy
- Frey’s syndrome
Question 6. Classify salivary glands tumors. Discuss the etiology, clinical features, and management of Warthin’s tumour.
Answer:
Warthin’s Tumour Classification:
1. Based on the spread of tumors
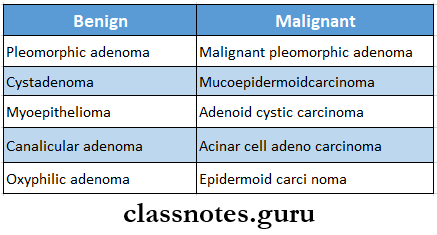
2. Histological classification
- Adenoma
- Pleomorphic
- Myoepithelioma
- Basal cell adenoma
- Warthin’stumours
- Canalicular adenoma
- Cystadenoma
- Carcinoma
- Acinic cell carcinoma
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Adenocarcinoma
- Squamous cell carcinoma
- Nonepithelial tumour
- Malignant lymphomas
- Secondary tumours
- Unclassified
- Tumor like lesions
- Sialoadenesis
- Oncocytosis
- Necrotizing sialometaplasia
- Salivary gland cyst
Warthin’s Tumor Clinical features
- Age: 50-70 years
- Sex: common in males
- Site: common in parotid gland especially in lower part overlying angle of the mandible
- Characterised by slow enlarging, well-circumscribed soft, painless swelling of gland
- Well-capsulated and movable
- Present over angle of mandible
- Size – 2-4 cm in diameter
- Shape- spherical in shape
- Occurs bilaterally
- Produces compressible and doughy feeling on palpation
- Little movable in all directions
Warthin’s Tumour Etiology:
- Warthin’s Tumor is derived from salivary tissue inclusions present in lymph node
Warthin’s Tumor Management:
Anesthetize the area
↓
The incision is given over the pre-auricular area
↓
Elevate skin and superficial fascia
↓
Isolation of facial nerve
↓
Dissection of the superficial portion of the parotid gland from underlying tissues
↓
Removal of gland along with tumor inside
↓
Hemostasis
↓
Placement of drains
↓
Suturing
Diseases Of Salivary Glands Short Essays
Question 1. Salivary fistula/ parotid fistula
Answer:
Salivary Fistula
- A parotid fistula may arise from the parotid gland or parotid duct
- Openings
- Internally inside the mouth
- Externally to the exterior
Salivary Fistula Causes:
- Penetrating injuries
- Rupture of parotid abscess
- Inadvertent incision and drainage
- Complications of superficial parotidectomy
Salivary Fistula Clinical Features:
- Opening in the cheek with discharge
- Discharge comes out during meals
Salivary fistula Investigations:
- A sialogram with a watery solution of lipiodol is performed
Salivary Fistula Treatment:
- When the fistula is connected with the main duct- reconstruction of the duct by Newman or Seabrock’s operation is performed
- If reconstruction fails, resection of the auriculotemporal nerve is done
- If the above measures fail, a complete parotidectomy is done
Sialadenitis and sialolithiasis questions and answers
Question 2. Salivary gland or submandibular gland calculi
Answer:
Salivary Gland
Salivary Gland is a pathological condition characterized by the presence of one or more calcified stones within the salivary gland itself or within its duct
Salivary Gland Etiology:
- Stagnation of saliva
- Ductal epithelial inflammation and injury
- Biological factors
Salivary Gland Pathogenesis:
- Formation of the soft nidus of mucin, protein, bacteria and desquamated cells.
- Allows concentric, lamellar crystallization
- Gradually sialolith increases in size
Submandibular Gland Calculi Composition Of Sialolith:
- Calcium phosphate
- Calcium carbonate
- Salts of Mg, Zn, etc
- Glycoproteins
- Mucopolysaccharides
- Cellular debris
Submandibular Gland Calculi Clinical Features:
- Age: middle-aged adults
- Sex: common in males
- Site: common in the submandibular gland due to the following:
- Due to viscous secretion
- Higher concentration of calcium and phosphate
- Tortuous anatomy of the ducts
- Dependent position of the gland
Submandibular Gland Calculi Features:
- Recurrent swelling of the gland region
- Recurrent episodes of sialadenitis
- Tense and tender gland
- Aggregates at mealtime
- Type of pain: pulling or drawing sensation
- Severe, stabbing type
- Enlarged gland
- Location: unilateral
- In chronic cases: formation of fistulas, sinus tracts & ulcerations in the area
- Necrosis of the gland acini
- Lobular fibrosis
- Complete loss of secretion of the gland
- So there is an increased risk of infections
submandibular Gland Calculi Diagnosis:
- Manual palpation
- Occlusal radiograph in case of submandibular gland
- Sialography
Submandibular Gland Calculi Treatment:
- For submandibular gland:
- Locate the sialolith radiographically
- Suture behind and below the duct to prevent the spillage of stone
- If sialolith is present posteriorly, incision is given medially
- If sialolith is present anteriorly, an incision is placed medial to plicasublingualis
- Locate the duct
- Locate the stone
- Incise over the stone
- Remove it through the forceps
For Parotid gland:
- Locate the sialolith
- Semilunar incision given anterior to the opening of the duct
- Reflection of the gland and Locate the stone
- Incise over the stone ” Remove it
Question 3. Surgical anatomy of the parotid gland
Answer:
Surgical Anatomy Of Parotid Gland
- The parotid gland is present on the lateral aspect of the face
- The surgical Anatomy Of the Parotid Gland is divided by the facial nerve into
- Superficial lobe- overlies masseter and mandible
- Deep lobe- present between the mastoid process and the styloid process, ramus of the mandible, and the medial pterygoid muscle
- Parotid duct
- It arises from the superficial lobe
- It is called Stenson’s duct
- It is 2-3 mm in diameter
- It receives tributaries from the superficial, deep, and accessory lobes
- It passes through the buccinator muscle and opens in the mucosa of the cheek opposite the upper 2nd molar tooth
- The parotid gland is covered by a
- True capsule which is a condensation of the fibrous stroma of the gland,
- False capsule
- Parotid fascia
- Parotid swellings are very painful
- They can be infected by the mumps virus
- The spread of infection from the oral cavity can result in a parotid abscess
Question 4. Mucous cyst or mucocele
Answer:
Mucous Cyst Or Mucocele
- Mucous Cyst Or Mucocele is a swelling caused by the accumulation of saliva at the site of a traumatized or obstructed minor salivary gland duct
Mucous Cyst Types:
- Extravasation:
- It is formed as a result of trauma to a minor salivary gland excretory duct
- It is more common
- It does not have an epithelial cyst wall
- Retention:
- Caused by obstruction by calculus of duct
Mucous Cyst Clinical Presentation:
- Site:
- Extravasation: lower lip is more common
- Other sites involve buccal mucosa, tongue, floor of the mouth, and retromolar area
- Retention: palate or floor of the mouth
- Appearance:
- Discrete, painless, smooth-surface swelling
- Size:
- Ranges from a few millimeters to a few centimeters
- Colour:
- Superficial lesions have a blue hue
- Deeper lesions can be more diffuse, covered by normal appearing mucosa without blue color
Mucous Cyst Treatment:
- Surgical excision to prevent recurrence
- Aspiration of fluid does not provide long-term benefit
- Surgical management may cause trauma to adjacent structures and can lead to the development of new lesions
- Intralesional injections of corticosteroids
Tumors of salivary glands questions
Question 5. Ranula
Answer:
Ranula
- Special type of mucocele
- Resembles the belly of a frog
Site:
- Floor of the mouth
- Superficial or deep to the mylohyoid muscle
Ranula Cause:
- Trauma to duct
Ranula Features:
- Slow-growing unilateral lesion
- Soft and freely movable
- Superficial lesions:
- Thin-walled bluish lesion
- Deeper lesions:
- Well circumscribed
- Covered by normal mucosa
Ranula Types:
- Simple type
- Plunging ranula
Ranula Treatment:
- Marsupialization
Question 6. Adenolymphoma of parotid gland
(or)
Warthin’s tumour
Answer:
Adenolymphoma Of Parotid Gland
- Adenolymphoma Of the Parotid Gland is located in the inferior pole of the gland, posterior to the angle of the mandible
Adenolymphoma Of Parotid Gland Presentation:
- SEX: common in males
- AGE: 5th and 8th decade of life
- Presents as a well-defined, slow-growing mass in the tail of the parotid
- Painless but can become superinfected n It is smooth with well defined capsule
Adenolymphoma Of Parotid Gland Treatment:
- Easily removed with margin of normal tissue
- Large tumour treated by superficial parotidectomy
Question 7. Xerostomia
Answer:
Xerostomia
- Xerostomia refers to a subjective sensation of a dry mouth, but not always, associated with salivary hypofunction
Xerostomia Etiology:
- Development
- salivary gland aplasia
- Water or metabolic loss
- Impaired fluid intake
- Hemorrhage
- Vomiting or diarrhea
- Latrogenic
- Medications
- Antihistamines
- Decongestants
- Antidepressants
- Antipsychotic
- Radiation therapy
- Systemic diseases
- Diabetes mellitus
- Sjogren’s syndrome
- HIV infections
- Local Factors
- Decreased mastication
- Smoking
- Mouth breathing
Xerostomia Clinical Features:
- Reduction in salivary secretions
- Residual saliva is either foamy or thick
- Mucosa appears dry
- Tongue is fissure
- Difficulty in mastication and swallowing
- Food adheres to the oral membranes
- Increased prevalence of candidiasis
- More prone to dental caries
Xerostomia Treatment:
- Elimination of causative agents
- Avoid medications causing xerostomia
- Use of noncarbonate sugarless fluids, xylitol-containing gums
- Use of pilocarpine to treat xerostomia
Parotid gland diseases question and answers
Question 8. Submandibular sialadenitis
Answer:
Submandibular Sialadenitis Causes
- Occurs due to
- Sequel to acute inflammation
- Intermittent obstruction by calculus
- Autoimmune disease
- Bilateral Sjogren’s syndrome
Submandibular Sialadenitis Features
- Recurrent attacks of pain and swelling
- Discharge of a small amount of pus
- Dilatation of ductules, atrophic acini
- Replacement of gland by chronically inflamed scar tissue
- Unilateral pain and swelling
- Reduced salivary flow
Submandibular Sialadenitis Treatment
- Antibiotics to control infection
- Removal of calculus
- Dilatation of constricted ducts
- Duct irrigation
- Radiotherapy
- Total conservative parotidectomy
Question 9. Adenoid cystic carcinoma
Answer:
Adenoid Cystic Carcinoma
- Adenoid Cystic Carcinoma is a highly malignant tumour of the salivary gland
Adenoid Cystic Carcinoma Clinical Features
- Slow growing
- Spreads along perineural tissue
- May invade periosteum or medullary bone
- Bony tenderness occurs
- It is hard and fixed
- Produce anaesthesia of skin overlying the tumour
- Spreads through local infiltration, lymphatics, and blood
Adenoid Cystic Carcinoma Pathology
- Contains cords of dark staining cells with cystic spaces containing mucin
- Contains myoepithelial cells and duct epithelium
Adenoid Cystic Carcinoma Treatment
- Radical parotidectomy with block dissection of neck
- Palliative radiotherapy to reduce pain and to arrest the progress of the disease
Mucocele and ranula questions and answers
Diseases Of Salivary Glands Short Answers
Question 1. Ranula
Answer:
Ranula
- Special type of mucocele
- Resembles the belly of a frog
Ranula Site:
- Floor of the mouth
- Superficial or deep to mylohyoid muscle
Ranula Cause:
- Trauma to duct
Ranula Features:
- Slow-growing unilateral lesion
- Soft and freely movable
- Superficial lesions:
- Thin walled bluish lesion
Ranula Deeper lesions:
- Well circumscribed
- Covered by normal mucosa
Question 2. Sialogram
(or)
Sialography
Answer:
Sialogram
Used for investigation of sialolith
Sialogram Procedure:
- Identification of duct
- Exploring of the duct
- Introduction of cannula
- Introduce contrasting media
- Lipid soluble or
- Water soluble agents
- Amount of the agent
- Submandibular gland: 0.5-0.75 ml
- Parotid gland- 0.76-1 ml
- Radiograph is taken
- Occlusal view
- AP view
Sialogram Interpretation:
- Parotid Gland- tree in winter appearance
- Submandibular gland- Bush in winter appearance
- Sjogren’s syndrome- Cherry blossom appearance
- Malignant tumour- Ball holding in hand appearance
Question 3. Acute parotitis
(or)
Parotid abscess
Answer:
Acute Parotitis
- Acute Parotitis is an acute inflammation of the salivary gland
Acute Parotitis Etiology:
- It is caused by Staphylococcus aureus
- Factors causing it are:
- When the salivary flow is reduced
- Partial obstruction of the duct with retention of secretions
Acute Parotitis Clinical Features:
- Pain and swelling of the side involved
- There is brawny oedematous swelling over the parotid region
- The temperature is high
- Cellulitis occurs in the overlying skin
- Pus may come out through the internal opening of the parotid gland
Question 4. Salivary calculus
Answer:
Salivary Calculus
- Salivary Calculus is a pathological condition characterized by the presence of one or more calcified stones within the salivary gland itself or within its duct
Salivary Calculus Etiology:
- Stagnation of saliva
- Ductal epithelial inflammation and injury
- Biological factors
Salivary Calculus Pathogenesis:
- Formation of the soft nidus of mucin, protein, bacteria, and desquamated cells.
- Allows concentric, lamellar crystallization
- Gradually sialolith increases in size
Composition Of Sialolith:
- Calcium phosphate
- Calcium carbonate
- Salts of Mg, Zn, etc
- Glycoproteins
- Mucopolysaccharides
- Cellular debris
Salivary gland infection question bank
Question 5. Mikulicz’s disease
Answer:
Mikulicz’s Disease
- Mikulicz’s Disease is a benign lesion
- Characterize by symmetric lacrimal, parotid, and submandibular gland swelling with associated lymphocytic infiltration
- Mikulicz’s Disease is associated with prominent infiltration of IgG4- positive plasmocytes into the involved gland, so-called IgG4-related plasmacytic endocrinopathy
Etiology:
- It is unknown
- Been speculated that autoimmune, viral, or genetic factors are involved
Mikulicz’s Disease Presentation:
- Affects middle-aged persons
- Unilateral or bilateral salivary gland swelling
- Reduced salivary flow
Mikulicz’s Disease Treatment:
- Methylprednisolone pulse therapy and prednisolone
Question 6. Mixed parotid tumour
(or)
Pleomorphic adenoma
Answer:
Mixed Parotid Tumor Clinical Features:
- Age: 5th and 6th decade
- Sex: common in females
- Site: common in parotid gland
Mixed Parotid Tumour Features:
- Slow growing
- Exophytic growth
- Solitary lesion
- Swelling of gland
- Smooth surface of the lesion
- No pain
- Superficial lesions
- Located near the angle of the mandible
- Deeper lesions:
- Over the lateral wall of the oropharynx
- Minor gland neoplasms exhibit firm, nodular swelling
- Palatal lesion causes surface ulceration
- In buccal mucosa it is present as small, painless nodular lesion
Question 7. Xerostomia
Answer:
Xerostomia
- Xerostomia refers to a subjective sensation of a dry mouth, but not always, associated with salivary hypofunction
Xerostomia Clinical Features:
- Reduction in salivary secretions
- Residual saliva is either foamy or thick
- Mucosa appears dry
- Tongue is fissure
- Difficulty in mastication and swallowing
- Food adheres to the oral membranes
- Increased prevalence of candidiasis
- More prone to dental caries
Xerostomia Treatment:
- Elimination of causative agents
- Avoid medications causing xerostomia
- Use of noncarbonated sugarless fluids, xylitol-containing gums
- Use of pilocarpine to treat xerostomia
Question 8. Sjogren’s syndrome
Answer:
Sjogren’s Syndrome
- Sjogren’s Syndrome is a chronic autoimmune disease
- Characterize by oral and ocular dryness, exocrine dysfunction, and lymphocytic infiltration
Sjogren’s Syndrome Etiology:
- It is unknown
Sjogren’s Syndrome Presentation:
- Decreased salivary function
- Dry mouth
- Difficulty in chewing, swallowing, and speech
- Dry, cracked lips
- Angular cheilitis
- Mucosa is painful and sensitive to species
- Mucosa is pale and dry
- Friable or furrowed
- Minimal salivary pooling
- Tongue is smooth and painful
- Increased dental caries and erosion of enamel
- Susceptible to infection
- Increased risk of developing malignant lymphoma
- Hypergammaglobulinemia
- Autoantibodies
- Elevated sedimentation rate
- Decreased WBC
- Monoclonal gammopathies
- Hypocomplementemia
Histopathology of salivary gland tumors questions
Question 9. Plunging ranula
Answer:
Plunging Ranula
- When the intrabuccal ranula has a cervical prolongation it is called plunging or deep ranula.
- Plunging Ranula is derived from the cervical sinus
- Plunging Ranula passes beyond the floor of the mouth along the posterior border of the mylohyoid muscle and appears in the submandibular region
Plunging Ranula Complications:
- It bursts due to repeated trauma
- Rarely infected
- Causes difficulty in rating and speech
Plunging Ranula Differential Diagnosis:
- Sublingual dermoid
- Lipoma
- Submandibular lymph node swelling
- Submandibular salivary gland swelling
Plunging Ranula Treatment:
- Complete excision of the ranula
Clinical features of Sjogren’s syndrome questions
Question 10. Sialadenitis
Answer:
Sialadenitis Causes
- Occurs due to
- Sequel to acute inflammation
- Intermittent obstruction by calculus
- Autoimmune disease
- Bilateral Sjogren’s syndrome
Sialadenitis Features
- Recurrent attacks of pain anti-swelling
- Discharge of a small amount of pus
- Dilatation of ductules, atrophic acini
- Replacement of gland by chronically inflamed scar tissue
- Unilateral pain and swelling
- Reduced salivary flow
Diseases Of Salivary Glands Viva Voce
- The commonest location of the pleomorphic adenoma in the parotid gland is the tail of the gland
- Superficial parotidectomy is the treatment of choice for pleomorphic adenoma
- Adenoid cystic carcinoma is the only tumor that shows a tendency for perineural invasion
- Tumors of the minor salivary glands are encountered most frequently in the palate
- Ranula usually arises from the glands of Blandin and Nuhn situated on the floor of the mouth
