Diseases Of Cardiovascular System Important Notes
- Cyanosis
- It is a bluish discoloration of skin and mucous membrane
- Types: central and peripheral
- Causes:
- Pulmonary – high altitude, pneumonia, pneumothorax, COPD, severe acute asthma
- Cardiovascular causes – acute pulmonary edema, cyanotic heart disease
- Blood disorders-methemoglobin
- CPR (Cardiopulmonary Resuscitation)
- Rescues breathing in adult 12 times/min
- Compression to ventilation ratio in two people is 5:1
- Compression to ventilation ratio in one person is 15:2
- Compression should be 60-80 minute in adults and 100/minute in children
- Depth of compression should be 1 1/2 -2 inches at the lower half of the sternum at an average of each second
- Starling’s Law
- It states that an increase in the force of contraction is directly related to cardiac output
- It states that the force of ventricular contraction is directly related to the end-diastolic volume
- Co Pulmonale
- It is an enlargement of the right ventricle of the heart as a response to increased resistance or high blood pressure in the lungs
- It is a condition where there is right ventricular hypertrophy with or without failure resulting from diseases affecting the structure or function of the lungs.
- Rheumatic Fever
- It is an acute inflammatory disease that occurs as a sequel of infection caused by group A streptococci
- Jone’s criteria is used for its features
- Diagnostic features
- Leucocytosis
- Raised ESR
- Raised CRP
- Raised ASO titre
- Cardiomegaly
- Jone’s Criteria
- Used for diagnosis of rheumatic fever
- Major manifestations:
- Carditis
- Polyarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules over bones or tendons
- Minor manifestations:
- Fever
- Arthralgia
- Previous history of rheumatic fever
- Raised ESR
- Leucocytosis
- First or second-degree AV block
- Mitral Stenosis
- Symptoms:
- Breathlessness
- Oedema, ascites
- Palpitation
- Hemoptysis
- Cough
- Signs:
- Atrial fibrillation
- Mitral facies
- Auscultation
- Loud first heart sound
- Opening snap
- Mid diastolic murmur
- Pulmonary hypertension
- Pulmonary edema
- Symptoms:
- Endocarditis Prophylaxis
- AJ STANDARD PROPHYLAXIS:
- Amoxycillin
- Dose= Adult-2 gm
- Child- 50 mg 1 hour before surgery
- BJ Patient Unable To Take Orally:
- Ampicillin
- Dose: Adult – 2 gm IM/IV
- Child- 50 mg 1 hour before surgery
- CJ Patient Allergic To Penicillin
- Clindamycin
- dose: Adult – 600 mg
- Child- 300 mg 1 hour before surgery
- AJ STANDARD PROPHYLAXIS:
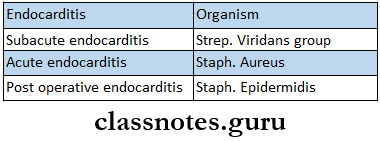
- Infective Endocarditis
- Etiology
- Clinical Features
- Roth spots
- Cerebral emboli
- Petechial hemorrhages of skin and mucous membrane
- Splinter hemorrhages and clubbing of nails
- Osier’s nodes
- Splenomegaly
- Haematuria
- Murmurs
- Arrhythmias
- Cardiac failure
- Etiology
- Myocardial Infarction
- Lab Investigations
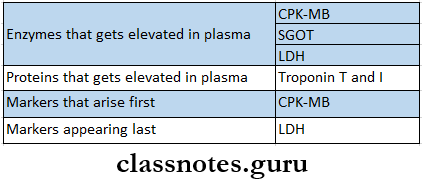
- Lab Investigations
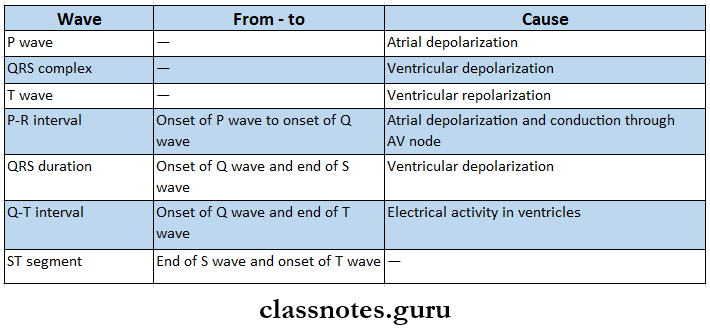
- Heart Sounds

- Risk Factors Of Atherosclerosis
- Cigarette smoking
- Hypertension
- Low HDL cholesterol
- Diabetes mellitus
- Family history of CHD
- Old age
- Life style
- Obesity
- Physical inactivity
- Atherogenic diet
- ECG Waves
Cardiovascular diseases short essay
Diseases Of Cardiovascular System Short Essays
Question 1. Risk factors of IHD
Answer:
Risk factors Of IHD
- Age: Occurs in middle and old age
- Sex: More common in males than in females
- Family history – Hyperlipidaemia and hyperfibrinogenemia are genetically determined
- Smoking – Related to IHD
- Hypertension
- Systolic and diastolic blood pressure increases the risk of IHD
- Hypercholesterolaemia
- HDL cholesterol is a protective
- LDL cholesterol increases the risk of IHD
- Hyperfibrinogenaemia
- Increases risk of IHD
- Hyperhomocysteinaemia
- Elevated levels of homocysteine in blood may promote thrombosis
- Sedentary habits
- Regular exercise for 20 min 2-3 times a week increases HDL cholesterol, lowers BP, reduces blood clotting, and promotes collateral formation
- Diabetes mellitus
- Diabetes is associated with coronary atherosclerosis, obesity, and physical inactivity which further increases the risk of coronary heart disease
- Obesity
- It is associated with hypertension, diabetes, physical inactivity
- Alcohol
- A moderate quantity of alcohol has a protective effect, while heavy drinking is considered a risk factor
- Mental stress
- It aggravates symptoms of pre-existing heart disease
- Diet
- A deficiency of polyunsaturated fatty acids increases the risk of IHD
- Low levels of vitamins A, C, and E increase the production of oxidized LDL
Read And Learn More: General Medicine Question and Answers
Question 2. Clinical features of acute rheumatic fever Jone’s criteria
Answer: Used for diagnosis of rheumatic fever
Major Manifestations:
- Carditis
- Polyarthritis Chorea
- Erythema marginatum
- Subcutaneous nodules over bones or tendons
Minor Manifestations:
- Fever
- Arthralgia
- Previous history of rheumatic fever
- Raised ESR
- Leucocytosis
- First or second-degree AV block
Short notes on heart diseases
Question 3. Cyanosis.
Answer:
Cyanosis
Bluish discoloration of skin and mucous membranes is called cyanosis.
Sites Involved:
- Lips n Nail beds a Finger’s tip Ear lobule.
- The undersurface of the tongue,
- Malar eminences
- Creases of plans.
Cyanosis Types Of Causes:
- Central cyanosis.
- Pulmonary causes.
- High altitude
- Pneumonia.
- Pneumothorax
- COPD
- Severe acute asthma
- Respiratory failure.
- Cardiovascular causes.
- Acute pulmonary edema
- Cyanotic heart diseases
- Corpulmonale,
- Blood disorders,
- Methemoglobin.
- Pulmonary causes.
- Peripheral cyanosis,
- Decreased cardiac output
- Congestive cardiac failure
- Cold exposure
- Arterial obstruction
- Venous obstruction.
Cyanosis Features:
- Peripheral cyanosis.
- Occurs due to extraction of 02 from blood.
- Occurs in healthy persons due to cold exposure.
- Seen on lips, nails, tip of nose, ear lobule
- Central cyanosis.
- Occurs due to poor oxygenation of blood in the lungs.
- Seen on the undersurface of the tongue, mucous membrane of the oral cavity, and palate.
- Mixed cyanosis.
- It is a combination of peripheral and central cyanosis.
Question 4. Right Ventricular Failure.
Answer:
Right Ventricular Failure
Right Ventricular Failure is defined as heart failure due to right ventricular outflow or inflow tract obstruction leading to passive congestion of the viscera.
Right Ventricular Failure Causes:
- Acute corpulmonale.
- Chronic corpulmonale.
- Pulmonary valve disease.
- Tricuspid valve disease
- Mitral valve disease
- Isolated right ventricular cardiomyopathy.
Right Ventricular Failure Clinical Features:
- Fatigue.
- Dyspnoea.
- Hypochondria pain.
- Protuberant abdomen.
- Swelling of leg.
- Distended neck veins.
- fender, soft, smooth hepatomegaly,
- Pitting edema.
- Ascites
- Pleural edema.
- Ascites
- Pleural effusion.
Right Ventricular Failure Treatment:
- Salt restriction
- Diuretics
- ACE inhibitors.
Common cardiovascular disorders short answer
Question 5.Congenital Cardiac Disease.
Answer:
Congenital Cardiac Disease
Congenital heart disease may present in early childhood or remain asymptomatic till adult life.
Congenital Cardiac Disease Classification:
- Acyanotic.
- Acyanotic with left to right shunt.
- Atrial septal defect
- Ventricular septal defect.
- Patent ductus arteriosus.
- Acyanotic without shunt.
- Pulmonary stenosis.
- Aortic stenosis.
- Coarctation of aorta.
- Acyanotic with left to right shunt.
- Cyanotic.
- Complete transposition of great vessels.
- Persistent trances arteriosus.
- Tetralogy of Fallot.
- Common atrium.
Etiology:
- Infections – rubella infection.
- Chromosomal defects – Down’s syndrome, Turner’s syndrome.
- Connective tissue disorders
- Alcohol abuse.
- Teratogenic drugs.
Congenital Cardiac Disease Clinical Features:
- Breathlessness.
- Central cyanosis.
- Clubbing.
- Growth retardation.
- Syncope.
- Short stature.
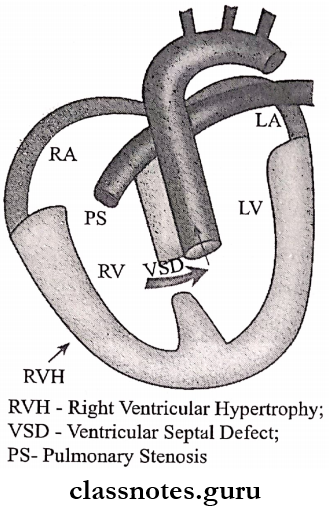
Question 6. Tetralogy of Fallot.
Answer:
Tetralogy Of Fallot Components:
- Pulmonary stenosis.
- Ventricular septal defect.
- Over-riding of the aorta at the level of ventricular septal defect.
- Right ventricular hypertrophy.
Pathogenesis:
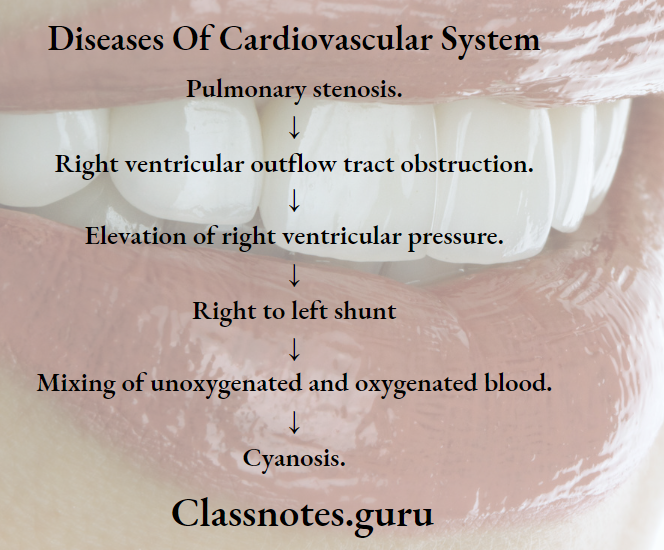
Tetralogy Of Fallot Clinical Features:
- Cyanosis – develops after 1 year of age.
- Grade 4 dubbing of fingers and toes
- Stunted growth.
Tetralogy Of Fallot Diagnosis:
- ECG – shows right ventricular hypertrophy.
- The second heart -sound – shows delayed splitting.
- Echocardiography – demonstrates aorta.
- X-ray chest – Boot-shaped heart.
Coronary artery disease short essay
Question 7. Angina pectoris — clinical features.
Answer:
Angina Pectoris Clinical Features:
- Common in 40 – 60-year-old males, n Retrosternal pain.
- Pain radiates to the left arm or the right arm, throat, back, chin, and epigastrium.
- It gets precipitated by exertion and relieved by rest.
- The patient feels heaviness, pressure, squeezing, or choking sensation.
- Nocturnal angina.
Question 8. Hypertensive encephalopathy.
Answer:
Hypertensive Encephalopathy
Hypertensive Encephalopathy is a neurological symptom occurring due to high blood pressure.
Hypertensive Encephalopathy Clinical Features:
- Transient abnormalities in speech or vision.
- Paraesthesia.
- Disorientation
- Fits.
- Loss of consciousness.
- Papilloedema.
Hypertensive Encephalopathy Treatment:
- Bed rest
- Sedation
- Intravenous sodium nitroprusside – 0.3 – 1 mcg/kg/min.
- Diuretics.
- Parenteral use of labetalol, hydralazine, or nitroglycerine.
Question 9. Complications and management of hypotension.
Answer:
Hypotension Complications:
- Headache
- Dizziness
- Fainting,
- Risk of accidents.
- Deprive of oxygen to vital organs, n Damage to the brain and heart.
Hypotension Treatment:
- Fluid administration – to treat dehydration,
- Use of compression stockings.
- Change body positions slowly,
- Increase salt intake.
- Fludrocortisone is used.
Question 10. Beta-blockers.
Answer:
Beta-Blockers
Bela blockers are drugs that block the actions of catecholamines mediated through beta receptors.
Beta-Blockers Classification:
- Non-selective.
- Propranolol, timolol, satalol.
- Cardio-selective.
- Metoprolol, atenolol, esmolol, betaxolol.
- Partial agonists.
- Pindolol, oxprenolol, carteolol.
- With additional alpha-blocking properties.
- Labetalol, carvedilol.
- β1 blockers β2 agonist.
- Celiprolol.
Beta-Blockers Uses:
- Hypertension.
- Angina pectoris,
- Cardiac arrest
- Myocardial infarction.
- Congestive cardiac failure,
- Obstructive cardiomyopathy,
- Pheochromocytoma.
- Thyrotoxicosis.
- Glaucoma.
- Prophylaxis of migraine.
- Anxiety.
Beta-Blockers Adverse Reactions:
- Bradycardia.
- Precipitates CCF and acute pulmonary edema,
- Cold extremities.
- Precipitates asthma.
- Insomnia, depression, hallucination, fatigue.
- Weakness, dizziness. a Rebound hypertension.
Question 11. Digoxin.
Answer:
Digoxin
Digoxin is a cardiac glycoside.
Digoxin Uses:
- Congestive cardiac failure.
- Cardiac arrhythmia.
- B Atrial fibrillation
- Atrial flutter
- Paroxysmal supraventricular tachycardia.
Digoxin Adverse Effects:
- Inhibits Na+/K+ – ATPase.
- Anorexia, nausea, vomiting, diarrhea.
- Directly stimulates chemoreceptor trigger zone (CTZ)
- Weakness.
- Confusion, hallucination.
- Blurred vision.
- Gynaecomastia.
- Cardiac toxicity.
Digoxin Contraindications:
- Hypokalemia.
- Myocardial infarction.
- Thyrotoxicosis.
- Acid-base imbalance.
Hypertension short note
Question 12. Anti-platelet drugs.
Answer:
Anti-Platelet Drugs
Antiplatelet drugs are drugs that interfere with platelet function.
Anti-Platelet Drugs Classification:
- PG synthesis inhibitor – Aspirin.
- Phosphodiesterase inhibitor – dipyridamol.
- ADP antagonists – ticlopidine, clopidogrel.
- Glycoprotein 2b/3a receptors antagonist – Abciximab.
- Others – PGI2.
Anti-Platelet Drugs Uses:
- Myocardial infarction.
- Unstable angina.
- In patients with prosthetic heart valves, valvular disease and, and se, coronary artery bypass surgery.
- Cerebral thrombosis.
- Atrial fibrillation.
