Spirochaetes Long Essays
Question 1. Laboratory diagnosis of syphilis
(or)
Serological tests for syphilis
Answer:
1. Microscopy
- It is useful in primary and secondary syphilis
- Direct fluorescent antibody test is used for T. pallidum
- In this method, acetone fixed smear is subjected to fluorescently tagged anti-T. pallidum antiserum
2. Serological Tests
- Tests for antibodies reacting with cardiolipin anti¬gen
- Standard tests for syphilis
- Wassermann test
- Standard tests for syphilis
- It is a complement fixation test
Read And Learn More: Microbiology Question and Answers
Serological Tests For Syphilis Method:
- The patient’s serum is inactivated by heating at 56s C for 30 minutes
- Incubated with cardiolipin antigen and guinea pig antigen at 37° C for 1 hour
- The indicator is added to detect the presence or absence of a compliment
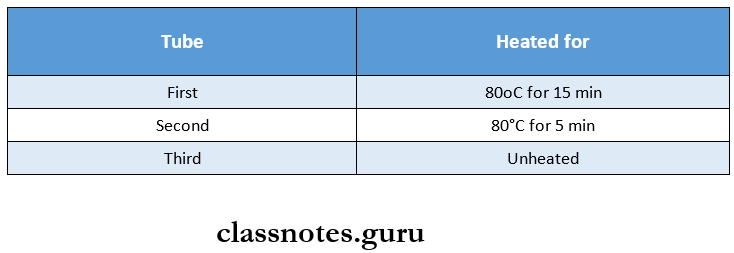
- 0.15 ml of inactivated serum is taken in three test tubes containing 0.05, 0.025, and 0.0125 ml of freshly prepared antigen dilution
- Tubes are shaken on Kahn’s and examined
Serological Tests For Syphilis Interpretation:
- If hemolysis does not occur, it indicates that the complement is utilized
- This is positive Wassmann’s reaction
- It hemolysis takes place, it indicates the comple¬ment is not been utilized in the tire’s primary reaction but utilized by the indicator system
- Kahn test
- It is a tube flocculation test
- The negative test shows uniform opalescence
- A positive test shows floccules
- VDRL test
- In this test, the inactivated serum is mixed with cardiolipin antigen on a special slide and rotated for 4 minutes
- The uniform distribution of crystals in the drop indicates tire serum is non-reacting
- The formation of clumps indicates it is reactive
- Tests for antibodies reacting with group-specific treponemal antigen
- Reiter protein complement fixation test
- In this method, lipopolysaccharide protein complex antigen derived from the cultivable Reiter’s stain is used
- It is less sensitive
- Reiter protein complement fixation test
- Tests for specific antibodies to pathogenic tre¬ponema
- Treponema pallidum immobilization test
- It employs live T. pallidum
- The test serum is mixed with actively motile Nichol’s strain of T. pallidum and incubated anaerobically
- If antibodies are present, the treponemas are immobilised
- Treponema pallidum immobilization test
- Fluorescent treponemal antibody absorption
- Test serum is preabsorbed with an extract of nonpathogenic treponemas to remove group-specific antigens
- It detects IgM and IgG
- It is the earliest test to become positive
- Microhaemagglutination test for treponema pallidum
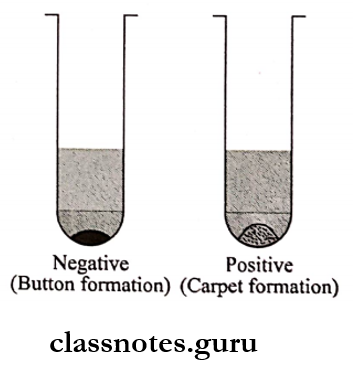
- T. pallidum antigen is coated onto the surface of red cells
- Tanned sheep RBCs are sensitized with an extract of T. pallidum
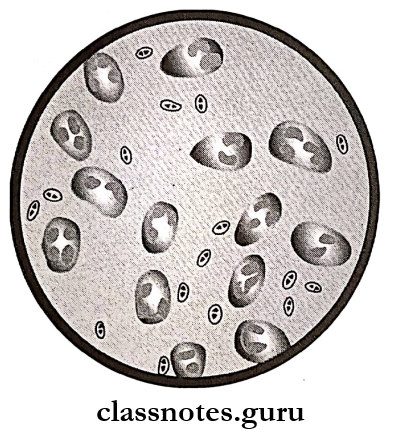
- When these sensitized erythrocytes are mixed with the patient’s serum containing anti¬bodies, the erythrocytes clump together
- Enzyme immunoassay
- They have been developed using T. pallidum antigens and are available commercially
- Fluorescent treponemal antibody absorption
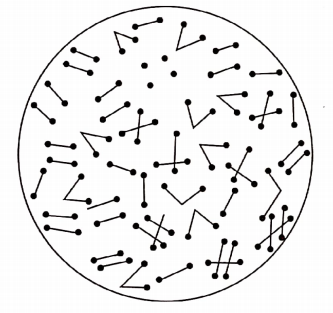
Spirochetes classification
Spirochaetes Short Question And Answers
Question 1. VDRL Test
Answer:
- Venereal Disease Research Laboratory test is the most widely used serological test for diagnosis of syphilis
- It is a simple and more rapid test that gives more quantitative results
- It requires only a small amount of serum and is sensitive
VDRL test Procedure:
- In this test, the inactivated serum is mixed with cardiolipin antigen on a special slide and rotated for 4 minutes
- The uniform distribution of crystals in the drop indicates the serum is non-reacting
- The formation of clumps indicates it is reactive
- By testing serial dilutions, the antibody titer can be determined
Question 2. Vincent’s angina
Answer:
- Vincent’s angina is a painful condition of the throat characterized by local ulceration of the tonsils, mouth, and pharynx
- Vincent’s bacilli is the causative organism
- It may occur as an acute illness with diffuse involve¬ment of tissue or as a chronic illness consisting of ulcera¬tion of tonsil
- It is insidious in onset with less fever and less discom¬fort
- The membrane that usually forms over the tonsil can be easily removed revealing an irregular ulcer on the tonsil
Question 3. Borrelia vincentii
Answer:
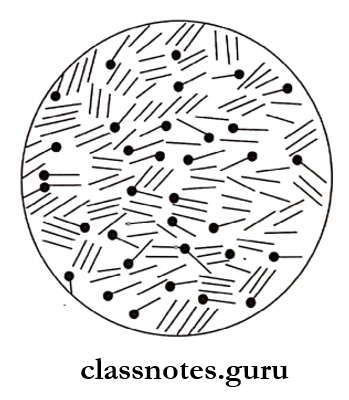
- It is a motile spirochaete which is a normal mouth commensal but a potential pathogen.
- Under predisposing conditions such as malnutrition (or) viral infections, it gives rise to ulcerative gin¬givostomatitis or oropharyngitis (Vincent’s angina).
- Borrelia vincenti in association with fusiform bacilli causes an infection known as fusospirochetosis.
- Diagnosis may be made by demonstrating spirochaetes and fusiform bacilli in stained smears of exudates from the lesions.
- Cultivation is difficult but can be done in enriched me¬dia anaerobically.
- Penicillin and metronidazole are effective in treatment.
Question 4. Congenital syphilis
Answer:
In congenital syphilis, the infection is transmitted from the mother to the fetus transplacentally.
Congenital Syphilis Clinical Features:
- Hutchinson’s triad
- Hyperplasia of the incisor and molar teeth
- Interstitial keratitis
- Eight nerve deafness.
- Frontal bossing
- Saddle nose
- High palatal arch
- Poorly developed maxillae
- Irregular thickening of clavicle
- Enlarged liver and spleen
- Diagnosis may be done by demonstrating spirochetes in lesions under dark dark-ground microscope.
- IgM FTA – ABS test, the modification of indirect immune fluorescence test is useful for the diagnosis of congenital syphilis and distinguishing from seropositivity due to passively transferred maternal antibodies
Spirochetes structure
Spirochaetes Viva Voce
- Technic acid of the cell wall of staphylococci facilitates the adhesion of cocci to the host cell
- ASO test is used for the diagnosis of rheumatic fever
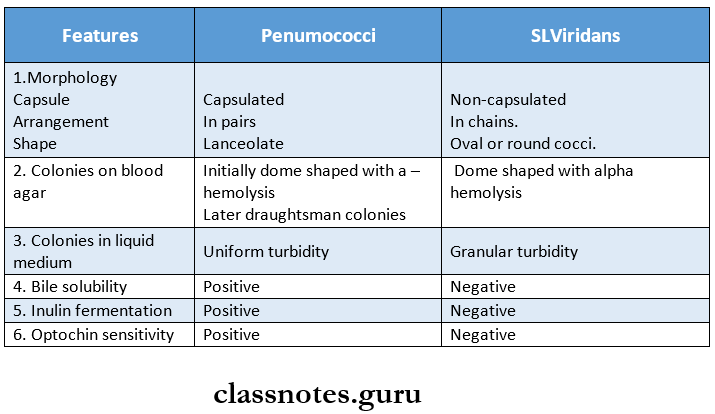
- Pneumococci gives draughtsman or carom coin appearance on blood agar
- Modified Thayer Martin, selective media is used for meningococci
- Corynebacterium diphtheria shows Chinese letter or cuneiform arrangement
- DTP vaccine consists of diphtheria toxoid, tetanus toxoid, and pertussis vaccine
- Bacillus coreus causes food poisoning
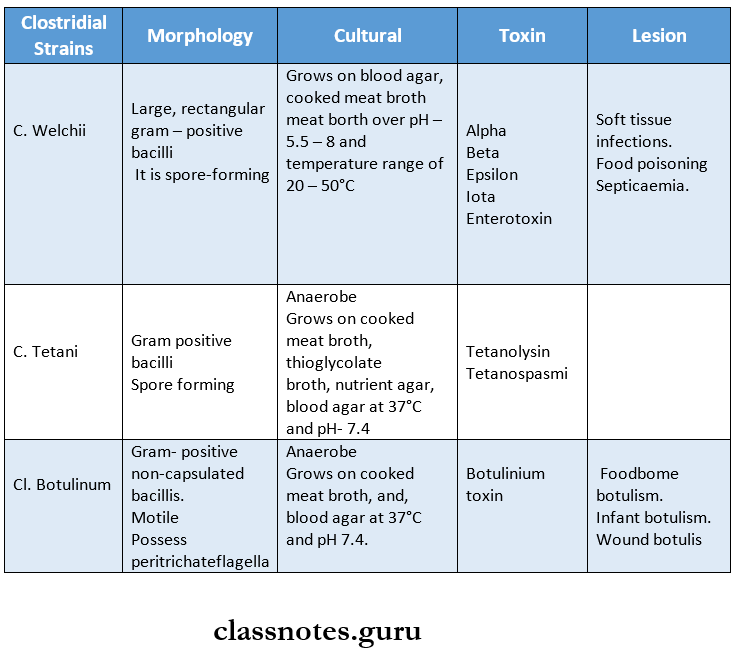
- Clostridium contains peritrich flagella for motility
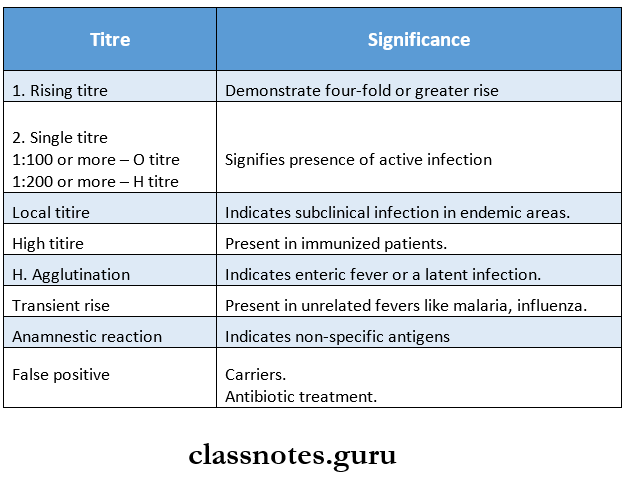
- Widal test is used for diagnosis of typhoid fever
- Dreyer’s tube and Felix’s tube are used in Widal test
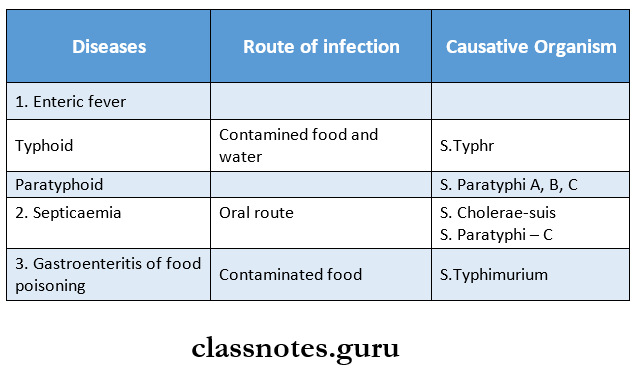
- Food poisoning is caused by any salmonella except salmonella typhi
- Yersinia pestis is a causative agent of plaque or black death
- Treponema pallidum is the causative agent for syphilis
- VDRL test is used for syphilis
- Actinomycetes gives sun ray appearance on culture
- H payroll causes peptic ulcer