Insulin And Oral Hypoglycaemics Important Notes
1. Insulin And Oral Hypoglycaemics Classification of Insulins
- Conventional
- Short-acting – regular insulin, prompt insulin zinc suspension
- Intermediate-acting – insulin zinc suspension, neutral protamine (Isophane)
- Long-acting – extended insulin zinc suspension, protamine zinc suspension
- A highly purified insulin preparation
- Single peak insulin
- Monocomponent insulin
Read And Learn More: Pharmacology Question and Answers
2. Insulin And Oral Hypoglycaemics Oral hypoglycaemic drugs
- Sulphonylureas
- First generation – tolbutamide, chlorpropamide
- Second generation – glibenclamide, glopizide
- Biguanides
- Meglitinides
- Alpha glycosidase inhibitor – acarbose
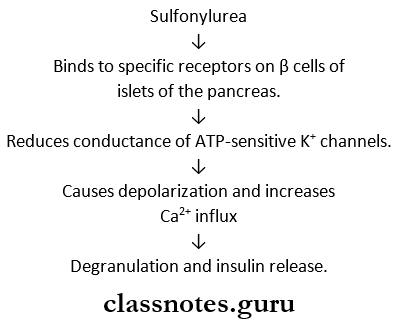
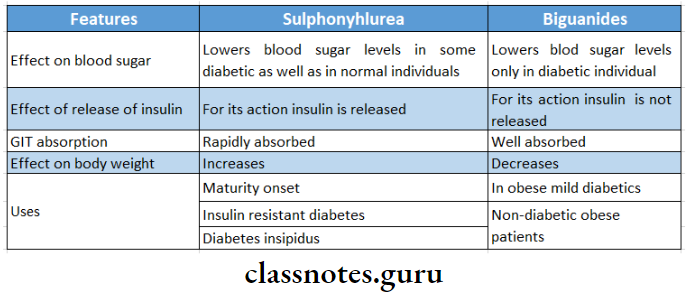
3. Insulin And Oral Hypoglycaemics Sulphonylureas
- Stimulators of beta cells
- Reduces blood glucose in normal subjects and type 2 diabetes
- Mode of action
- Brings the release of insulin by activating receptors on beta cells of the pancreas
- Reduces glucagon secretion
- Increases insulin receptors on target cells
- Inhibits gluconeogenesis in the liver
Oral hypoglycemic drugs classification questions and answers
4. Insulin And Oral Hypoglycaemics Metformin
- It is a biguanide, an oral hypoglycaemic drug
- Contraindications
- Hypotension
- CVS diseases
- Respiratory diseases
- Hepatic and renal diseases
- Alcoholics
- Action
- Suppresses hepatic gluconeogenesis and glucose output from the liver
- Interferes with mitochondrial respiratory chain
- Not metabolized at all
- Excreted unchanged in the urine
5. Insulin And Oral Hypoglycaemics Chlorpropamide
- Long-acting hypoglycaemic
- Reduces urine volume in diabetes insipidus
- Sensitizes kidney to ADH action
Insulin And Oral Hypoglycaemics Long Essays
Question 1. Classify antidiabetic drugs and write about oral antidiabetic drugs.
Answer:
Anti-diabetic drugs:
- These drugs used lower blood glucose levels.
Anti-diabetic drugs Classification:
1. Insulin.
- Ultra short-acting or rapid-acting.
- Insulin lispro, insulin aspart, insulin glulisine.
- Short-acting.
- Intermediate acting.
- Insulin zinc suspension, neutral protamine hagedorn.
- Long-acting.
- Protamine zinc insulin, insulin glargine.
2. Oral hypoglycaemics.
- Sulfonylureas.
- First generation – tolbutamide, chlorpropamide.
- Second generation – Glibenclamide, Glipizide.
- Biguanide – metformin.
- Meglitinide or phenylalanine analogues.
- Repaglinide, Nateglinide.
- Thiazolidin editions.
- Rosiglitazone, pioglitazone.
- Alpha-glucosidase inhibitors.
- Dipeptidyl peptidase – 4 inhibitor.
- Sitagliptin, vildagliptin.
1. Anti-diabetic drugs Sulfonylureas:
- They were the first oral hypoglycaemic drugs.
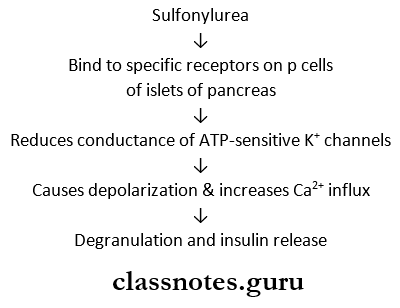
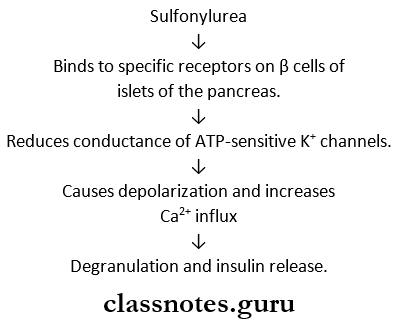
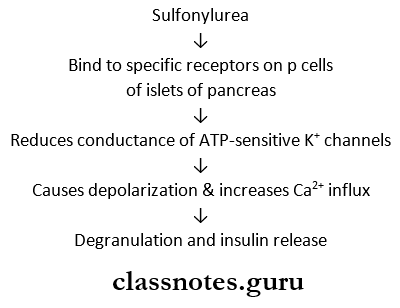
Sulfonylureas Mechanism of action:
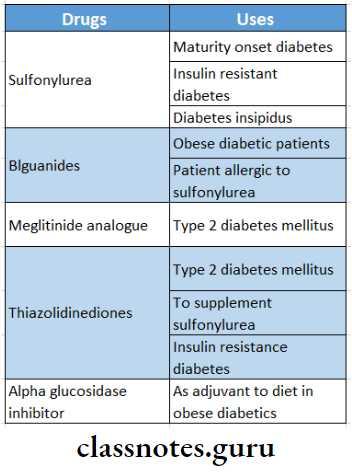
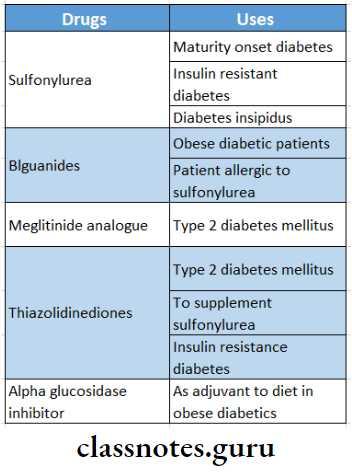
Sulfonylureas Uses:
- Used in patients with type II diabetes mellitus
Sulfonylureas Adverse effects:
- Hypoglycaemia.
- Nausea, vomiting, diarrhoea, headache, weight gain, paraesthesia, weight gain.
- Hypersensitivity reactions.
2. Anti-diabetic drugs Biguanides:
Biguanides Actions:
- Inhibit hepatic gluconeogenesis.
- Enhances insulin-mediated glucose disposal in muscle and fat
- Retards intestinal absorption of glucose.
- Promotes peripheral utilization of glucose
BiguanidesUse:
- Used in obese patients with type II diabetes mellitus.
3. Anti-diabetic drugs Meglitinide Analogues:
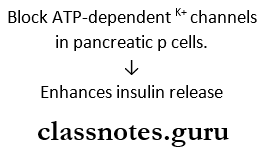
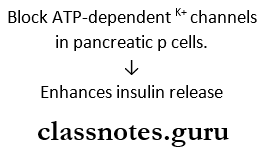
Meglitinide Analogues Mechanism:
Meglitinide Analogues Uses:
- Used in type 2 DM either alone or with metformin.
4. Anti-diabetic drugs Thiazolidinediones:
- They are selective agonists for the receptor nuclear peroxisome proliferator-activated receptor gamma.
Thiazolidinediones Uses:
- Type; 2 diabetes mellitus.
- Used to supplement sulfonylureas or metformin and in case of insulin resistance.
5. Anti-diabetic drugs Alpha-glucosidase inhibitors:
- Acarbose is one of the alpha-glucosidase inhibitors.
- It slows down digestion and absorption of polysaccharides and glucose.
- As an adjuvant to diet in obese diabetics.
Oral antidiabetic drugs MCQs with answers
Question 2. Describe the different preparations of insulin. Add a note on their merits and demerits.
Answer:
Insulin preparations:
- Insulin preparations differ in their source and duration of action.
1. Insulin preparations Conventional insulins:
- Rapid-acting.
- Insulin lispro, insulin aspart, insulin glulisine.
- Short during.
- Intermediate acting.
- Insulin zinc preparation, neutral protamins hatedom.
- Long-acting.
Conventional insulins Advantages/Mertis:
- Rapid onset
- Longer duration of action.
Conventional insulins Disadvantages/Demerits:
- Allergic.
- Not very stable
- Degraded in GIT, so not given orally.
- Antigenic.
2. Insulin preparations Highly purified insulins:
- Single peak insulin – regular, lente.
- Monocomponent insulin – regular, lente.
Highly purified insulins Advantages:
- Purified, thus contamination is negligible.
- Less antigenic.
- More stable.
- Lesser chances of resistance.
- Lesser chances of lipodystrophy.
Highly purified insulins Disadvantages:
3. Insulin preparations Human insulin:
- Produced by recombinant DNA technology
- They are regular, lente, and isophane.
Human insulin Advantages:
- Less antigenic.
- So less allergic reactions.
- Less injection site lipodystrophy.
Human insulin Disadvantages:
4. Insulin preparations Insulin analogues:
- Synthesized by genetic engineering.
- They include insulin lispro, insulin aspart, insulin glargine, insulin glulisine, and insulin detemir.
Insulin analogues Advantages:
- Rapid absorption.
- Can be given 10 minutes before food.
- Less hypoglycaemia.
- Favourable pharmacokinetics.
- Better blood glucose control.
- Greater stability
Insulin analogues Disadvantages:
Mechanism of action of oral hypoglycemic drugs
Question 3. Discuss Insulin pharmacological actions and adverse effects.
Answer:
Insulin Pharmacological Actions:
1. Carbohydrate metabolism.
- Insulin decreases blood glucose levels by
- Increasing glucose uptake and glycogen synthesis.
- Inhibits glycogenolysis and glucose output
- Inhibits gluconeogenesis.
- Facilitates glucose transport across the cell membrane
- Alters activity of enzymes involved in metabolism.
2. Protein metabolism.
- Facilitates protein synthesis.
- Inhibits protein breakdown.
- Thus, has an anabolic effect
3. Lipid metabolism.
- Promotes synthesis of triglycerides.
- Inhibits lipolysis.
4. Insulin increases potassium entry into cells and decreases urea output from the liver.
Insulin Adverse effects:
1. Hypoglycaemia.
- Most common side effect.
- Occurs due to large doses, improper time of administration, missing a meal, and vigorous exercise.
- Prolonged hypoglycaemia may cause permanent brain damage.
2. Local reactions.
- Swelling, erythema and stinging at the site of injection.
- Localized lipodystrophy.
3. Allergy.
- Occurs due to contaminating proteins.
- Utricaria, angioedema and anaphylaxis occur.
4. Insulin resistance.
- Develops when insulin requirement is increased.
Question 4. Write the mechanism of action and therapeutic uses of insulin.
Answer:
Insulin:
Insulin is a hormone that is synthesized in the beta cells of pancreatic islets.
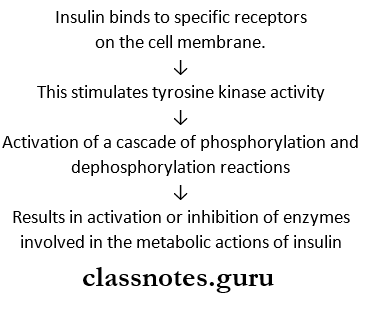
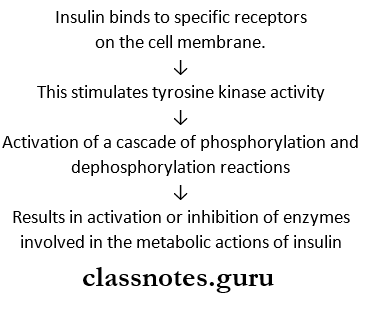
Insulin Mechanism of action:
Insulin Uses:
- In juvenile diabetes.
- When diabetes is not controlled by diet or exercise.
- Underweight patients.
- Failure of oral hypoglycaemic drugs.
- The stress of surgery, infections, trauma, pregnancy and labour.
- Complications of diabetes – diabetic coma, ketoacidosis, gangrene of extremities.
Question 5. Write the mechanism of action, uses and adverse effects of sulfonylureas.
Answer:
Sulfonylureas:
- They were the first oral hypoglycaemic drug to be introduced.
Sulfonylureas Mechanism of action:
Sulfonylureas Uses:
- Maturity onset diabetes
- Insulin resistant diabetes
- Diabetes insipidus.
Sulfonylureas Adverse effects:
- Hypoglycaemia.
- Nausea, vomiting, diarrhoea, constipation.
- Headache, paresthesia.
- Weight gain.
- Hypersensitivity – rashes, photosensitivity, purpura.
- Agranulocytosis, transient leukopenia.
Metformin pharmacology questions
Question 6. Mention the hormones secreted by the pancreas. What is diabetic coma? What are the principles of treatment?
Answer:
Hormones secreted by the pancreas are:
1. Hormones secreted by the pancreas Insulin.
- It is a hypoglycaemic hormone.
- Synthesized by p cells of pancreatic islets.
- It is two chain polypeptide having 51 amino acids.
- It facilitates glucose transport and inhibits glycol- analysis, and gluconeogenesis.
- Thus lowering blood glucose levels.
2. Hormones secreted by the pancreas Glucagon.
- It is a hyperglycaemic hormone.
- Secreted by cells of pancreatic islets.
- It enhances glycogenolysis and gluconeogenesis.
- Thus increasing blood glucose levels.
Glucagon Diabetic coma:
- Severe hyperglycaemia and glycosuria result in severe dehydration and increased plasma osmolarity leading to coma.
- Seen in insulin-dependent diabetes mellitus.
Glucagon Symptoms:
- Hyperglycaemia.
- Acidosis
- Hyperventilation
- Dehydration
- Hypotension
- Shock
- Impaired consciousness.
Glucagon Management:
1. Correction of hyperglycaemia.
- Intravenous regular insulin 0.1 U/kG bolus followed by 0.1 U/kg/hour by continuous IV infusion till patient recovers.
2. Correction of dehydration.
- IV fluids – normal saline IV1 litre/hour.
3. Correction of acidosis,
- Use of sodium bicarbonate.
4. Correction of hypokalemia.
5. Supportive treatment – done by use of antibiotics.
Insulin And Oral Hypoglycaemics Short Essays
Question 1. Sulfonylurea.
Answer:
Sulfonylurea was the first oral hypoglycaemic drug to be introduced.
Sulfonylurea Classification:
1. First generation – Tolbutamide, chlorpropamide
2. Second generation – Glibenclamide, glipizide, Gli- clazide, Glimepride.
Question 2. Oral antidiabetic drugs.
Answer:
Oral antidiabetic drugs are drugs that lower blood glucose levels and are effective orally.
Oral antidiabetic drugs Classification:
1. Sulfonylureas.
- First generation – Tolbutamide, chlorpropamide.
- Second generation – Glibenclamide, glipizide.
2. Biguanide – metformin.
3. Meglitinide, phenylalanine analgues.
- Repaglinide, nateglinide.
4. Thiazolidinediones.
- Rosiglitazone, pioglitazone.
5. Alpha-glucosidase inhibitors.
6. Dipeptidyl peptidase – 4 inhibitor.
- Sitaglipitin, vildagliptin.
Oral antidiabetic drugs uses:
Oral antidiabetic agents classification chart
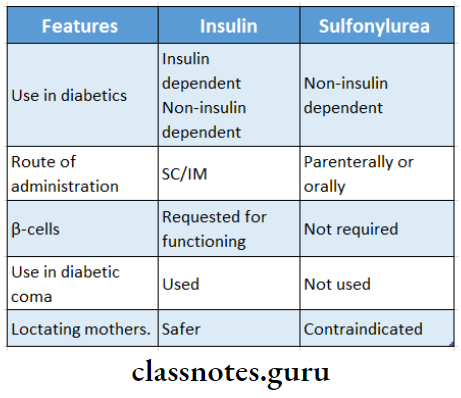
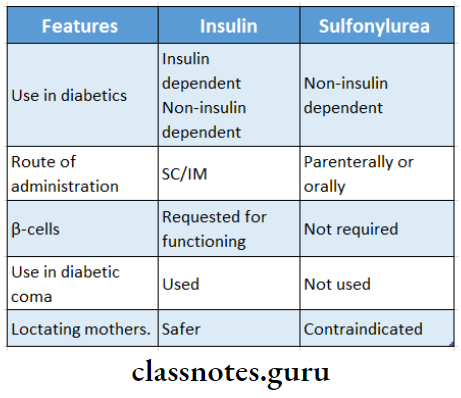
Question 3. Insulin and sulphonylureas.
Answer:
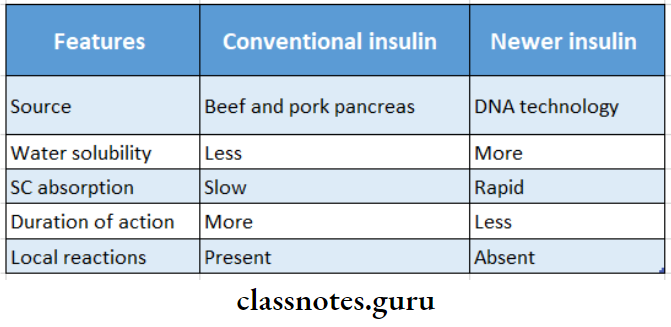
Question 4. Advantages of newer insulin.
Answer:
Newer insulins are derived from the human pancreas.
- Hence, the risk of antigen-antibody reactions is avoided.
- They are highly purified preparations.
- Can be used in insulin resistance diabetes
- Can be used during pregnancy without teratogenicity.
- Can be used in case of injection site lipodystrophy caused by conventional preparation.
Question 5. Give reasons – glibenclamide is not useful in treating childhood diabetes mellitus.
Answer:
Glibenclamide is a second-generation sulphonylurea.
- Sulphonylurea causes the release of insulin from the pancreas.
- They act on receptors present on the pancreatic beta cell membrane.
- Causes depolarization by reducing the conductance of ATP-sensitive K+ channels.
- This enhances Ca2+ influx degeneration and insulin resistance.
- They cannot cause hypoglycaemia in pancreatic-atomized animals or in type I diabetes mellitus.
- Since type I diabetes occurs in children glibenclamide cannot be used to treat it.
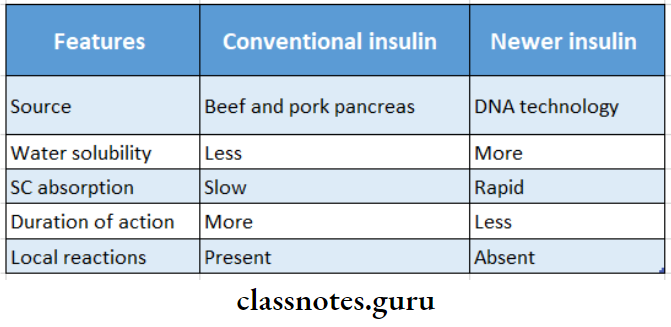
Question 6. Compare and contrast conventional insulin with newer insulin.
Answer:
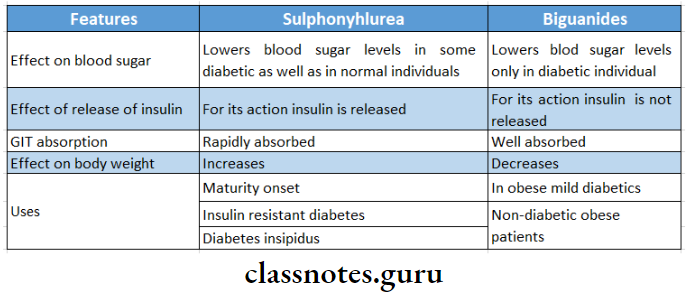
Question 7. Compare and contrast sulphonylurea and biguanides
Answer:
Question 8. Biguanides.
Answer:
- It is an oral hypoglycaemic drug
- It is not metabolized at all
- Excreted unchanged in the urine
Biguanides Actions:
- Inhibits hepatic gluconeogenesis
- Enhances insulin-mediated glucose disposal in muscle and fat
- Retards intestinal absorption of glucose
- Promotes peripheral utilization of glucose
Biguanides Use:
- Used in obese patients with type II diabetes
Biguanides Contra-Indications:
- Hypotension
- CVS diseases
- Respiratory diseases
- Hepatic and renal diseases
- Alcoholics
Oral hypoglycemic agents short notes
Insulin And Oral Hypoglycaemics Short Question And Answers
Question 1. Advantages of newer insulins.
Answer:
Derived from the human pancreas.
- So, lesser risks of antigen-antibody reactions.
- They are highly purified.
- Can be used in insulin resistance diabetes
- Can be used during pregnancy.
- Can be used in case of injection site lipodystrophy.
Question 2. Sulphonylurea.
Answer:
Sulphonylurea was the first oral hypoglycaemic drug introduced.
Sulphonylurea Classification:
1. First generation – tolbutamide and chlorpropamide.
2. Second generation – Glibenclamide, glipizide.
Sulphonylurea Uses:
- Maturity onset diabetes.
- Insulin resistant diabetes
- Diabetes insipidus.
Question 3. Tolbutamide.
Answer:
Tolbutamide is an oral hypoglycaemic drug.
- It is first generation sulphonylurea.
Tolbutamide Features:
- Weaker
- Short-acting.
- Flexible dosage.
- Safer for those prone to hypoglycaemia.
- Daily dose – 0.4 – 3 g.
- Half-life – 6 – 8 hours.
- Duration of action – 6 – 8 hours.
Tolbutamide Use:
- Type II diabetes mellitus.
Question 4. Glibenclamide.
Answer:
Glibenclamide is an oral hypoglycaemic drug.
- It is second generation sulphonylurea.
Glibenclamide Features:
- Potent
- Slow acting.
- Marked insulinemic action.
- Effective in a single dose.
- Higher incidence of hypoglycaemia.
- Plasma t ½ – 4 – 6 hours.
- Duration of action – 18 – 24 hours.
- Daily dose 5-15 mg.
Glibenclamide Use:
Type II diabetes mellitus.
Question 5. Insulin preparations.
Answer:
Based on onset and duration of action, insulin preparations are:
1. Rapid acting.
- Insulin lispro, insulin aspart, insulin glulisine.
2. Short-acting – regular insulin.
3. Intermediate-acting – insulin zinc suspension iso-phane insulin.
4. Long-acting – protamine zinc insulin, insulin glargine.
Question 6. Uses of insulin.
Answer:
Uses are diabetes is not controlled by diet and exercise.
- Primary or secondary failure of oral hypoglycaemic drugs.
- In underweight patients.
- Temporary to overcome infections, trauma, and surgery.
- In complications of diabetes like ketoacidosis, gangrene of extremities.
Question 7. Drug treatment of juvenile diabetes.
Answer:
Juvenile diabetes is insulin-dependent diabetes mellitus.
juvenile diabetes Treatment:
- Insulin therapy along with diet
- Started with regular insulin parenterally before each major meal.
- Condition is assessed by regular testing of urine or
- blood glucose level.
Question 8. Adverse effects of insulin.
Answer:
- Hypoglycaemia.
- Local reactions – swelling, erythema and stinging.
- Localized lipodystrophy.
- Allergy – urticaria, angioedema and anaphylaxis.
Question 9. Oral hypoglycaemic drugs.
Answer:
1. Sulphonylurea.
- First generation – Tolbutamide, chlorpropamide.
- Second generation – Glibenclamide, glipizide.
2. Biguanide – metformin.
3. Meglitinide analogues – repaglinide, nateglinide.
4. Thiazolidinediones – rosiglitazone, pioglitazone.
5. Alpha glucosidase inhibitors.
6. Dipeptidyl peptidase – 4 inhibitor.
- Sitagliptin, vildagliptin.
Oral antidiabetic agents classification chart
Question 10. Protamine zinc insulin.
Answer:
It is a long-acting oral hypoglycaemic drug.
- The onset of action – 4 – 6 hours.
- Duration of action – 24 – 36 hours.
- It can be mixed with regular insulin.
- Produces relatively low, smooth and peakless blood Insulin levels.
- Once daily administration produces constant Insulin action.
Question 11. Glimepiride.
Answer:
- It is second generation sulphonylurea
- Has stronger extrapancreatic action
- Has less hyperinsulinaemia
- Daily dose – 1-6 mg
- Plasma half-life – 5-7 hours
- The duration of action is 24 hours