Miscellaneous Short Essays
Question 1. Oral Candidiasis.
Answer:
- It is a fungal infection occurring in the oral cavity
Oral Candidiasis Causative Organisms:
- Candida albicans
- C. Krusei
- C. pseudotropicalis
Oral Candidiasis Features:
- Oral thrush
- Mucosa appears as a thick, white soft plaque
- However, it can be wiped off easily
- Method Of Preparation:
Read And Learn More: Periodontics Question and Answers
Oral Candidiasis Treatment:
- Topical and systemic administration of nystatin.
Question 2. Night guards
Answer:
- A night guard is a removable appliance that is worn by the patient during sleep, to protect his teeth and jaws from the damage that is caused by the habit.
- It is not necessarily a treatment procedure because the grinding habit is not exactly resolved, but the wearing of the appliance reduces the harmful effects of teeth grinding.
Night guards Types:
- A ready-made appliance that comes in standard sizes;
- A boil-and-bite appliance that offers some customization; and
- Custom-made appliances that dentists prefer and commonly prescribe. Custom dental night guards are different and rather effective,
Night guards Method of preparation:
- Step 1: Impression Taking.
- Step 2: Night Guard Fabrication.
- Step 3: Delivery. As soon as the night guards have been fabricated, they are delivered to the patients along with proper instructions for wear and care.
Question 3. Full mouth disinfection
Answer:
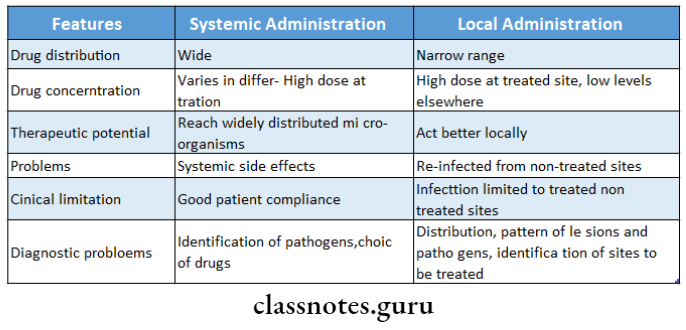
- Full mouth disinfection refers to an intense course of treatment for periodontitis typically involving scaling and root planing in combination with adjunctive use of local antimicrobial adjuncts to periodontal treatment such as chlorhexidine mouthwash
- It consists of organisms, keratotic debris, and inflammation. It is a technique to eliminate or reduce the pathogenic cells, desquamated cells bacteria from the buccal habitats which can provoke the reinfection of the places already treated
Full mouth disinfection Aims
- Complete and simultaneous elimination of all the bacteria in the periodontal sacs within less than 24 hours
Full mouth disinfection Steps
- Periodontal probing and diagnosis
- Hygiene instructions
- Removal of supra and subgingival plaque with ultrasound
- Radicular scraping and smoothing with Gracey curettes
- Radicular scaling with preset
- Brushing of the back of the tongue for 60 seconds with 0.12% chlorhexidine gel
- Mouthwashes with 0.12% chlorhexidine
- Subgingival irrigation of periodontal pockets above 5 mm with chlorhexidine gel
Question 4. Subepithelial connective tissue graft.
Answer:
- As described by Langer and Langer
Tissue graft Indications:
- Larger and multiple defects
- Defects with good vestibular depth
- Defects with an adequate gingival thickness
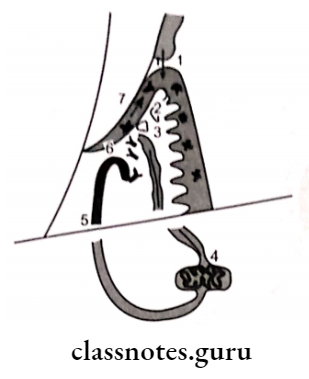
Tissue graft Surgical procedure:
- Raise a partial thickness flap with a horizontal incision 2 mm away from the tip of the papilla and 2 vertical incisions 1-2 mm away from the gingival margin
- Extend the flap to the mesiobuccal fold
- Thorough root planning is done
- Obtain connective tissue graft from the palate through a horizontal incision from the gingival margin of molars and premolars
- A palatal wound is sutured by primary closure
- Place the connective tissue graft over a denuded root and suture it
- The graft is covered by the partial thickness flap and sutured interdentally
- The graft is protected by surgical dressing
- After 7 days sutures and dressing is removed
Miscellaneous Short Question And Answers
Question 1. Active Immunity.
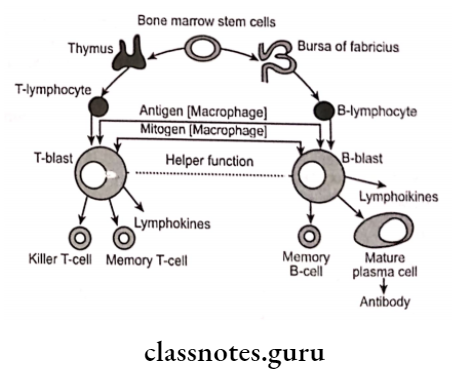
Answer:
- It is the immunity that an individual develops as a result of infection or by specific immunization
- It may be acquired in 3 ways
- Following clinical infection – Ex. Chickenpox
- Following subclinical infection – Ex. Polio
- The following immunization
- It is superior to passive immunity
Question 2. Define.
Answer:
- Neoplasia: A mass of tissue formed as a result of the abnormal, excessive, uncoordinated, autonomous, and purposeless proliferation of cells.
- Hypertrophy: It is an increase in the size of cells re- resulting in the enlargement of the organ or tissue, without any change in the number of cells.
- Hyperplasia: It is an increase in the number of parenchyma cells resulting in the enlargement of the organ or tissue.
Question 3. Stillman’s Clefts.
Answer:
- Apostrophe shaped indentation
Extend of Stillman’s Clefts: Marginal gingiva to varying depth
Clefts Site of Stillman’s Clefts: Facial surface
Clefts Margins of Stillman’s Clefts: Rolled underneath linear gap in the gingiva
Clefts Size of Stillman’s Clefts: Blunt over remaining gingiva
Cause of Stillman’s Clefts: Occlusal trauma
Stillman’s Clefts Treatment: Repair spontaneously
Stillman’s Clefts Types:
- Simple: Occurs in a single direction
- Complex: Occurs in more than one direction
Question 4. McCall’s Festoons.
Answer:
- Life-preserver-shaped enlargements of the marginal gingiva.
- Site: Canine and premolar areas on the facial surface
McCall’s Festoons Features:
- Initially – Normal gingiva
- Accumulation of food debris leads to secondary in-inflammatory changes
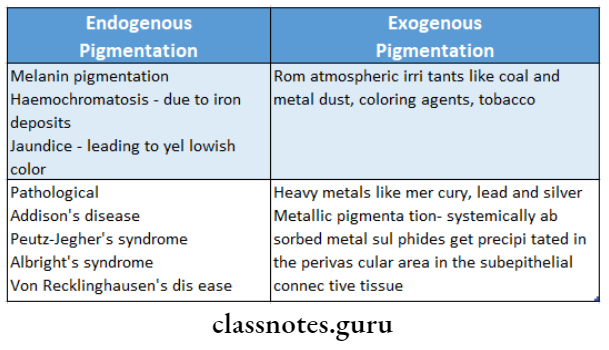
Question 5. Gingival Pigmentations.
Answer:
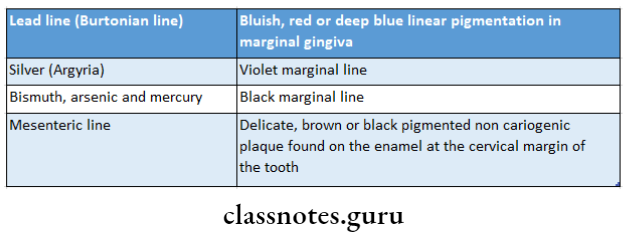
- By therapeutic use or occupational environment
- Various metal causes different pigmentation.
- Lead Bluish red linear pigmentation of the marginal gingiva
- Silver – Violet marginal line
- Results from perivascular precipitation of metallic sul- fides in the subepithelial connective tissue.
Gingival Pigmentations Sites:
- Areas of inflammation
- Irritated mucosal areas
Gingival Pigmentations Treatment:
- Elimination of local irritating factors
- Restoration of tissue health
- Topical application of concentrated peroxide
- Insufflation of the gingiva with oxygen to oxidize the dark metallic sulfides
Question 6. Dentoalveolar Ablation.
Answer:
- Forceful frictional action between the oral soft tissue tissues.
Normal – Salivary pH, buffering capacity, and calcium and phosphorous content
Elevated – mucin level
Feature Sharply defined wedge-shaped depression in the cervical area of the facial tooth surface
Cause – Decalcification by acid beverages.
- The combined effect of salivary secretion and friction
Question 7. Fremitus test and tension test.
Answer:
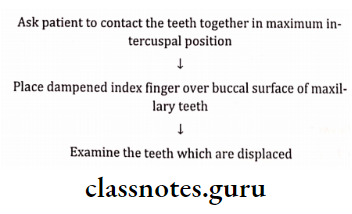
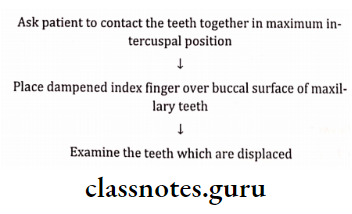
Tension test Fremitus Test:
Tension test Procedure:
Tension test result:
- Class 1 – Mild vibration
- Class 2 – Easily palpable but no visible movements
- Class 3 Movements visible with the naked eye
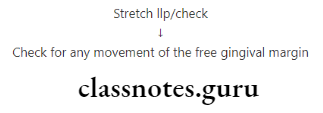
Tension Test:
- Diagnostic to measure the width of attached gingiva
tension test Procedure:
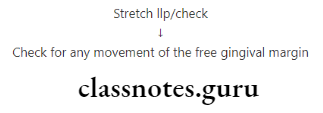
tension test Result:
- If the free gingival margin moves then the attached gingiva is considered inadequate.
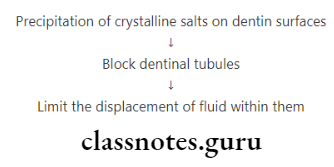
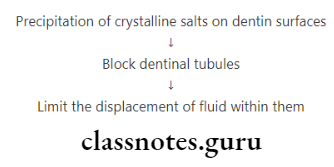
Question 8. Name 2 desensitizing agents. Write about the mode of action of anyone.
Answer:
Agents:
- Dentrifices
- Varnishes
- Fluoride compounds
Mode Of Active
Question 9. Osteoplasty and Osteotomy.
Answer:
Osteotomy Osteoplasty:
- Reshaping of the alveolar process to achieve a more physiologic form without the removal of supporting bone
- Reshaping the bone without removing tooth-supporting bone
Osteotomy:
- Includes removal of tooth-supporting bone
- Place dampened index finger over the buccal surface of the maxilla
- It is defined as the excision of bone/portion of bone
- It is done to correct/reduce deformities caused by pe- periodontitis and includes the removal of the supporting bone
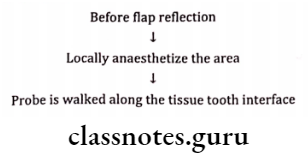
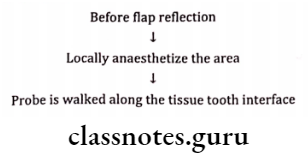
Question 10. Transgingival Probing.
Answer:
Transgingival Probing Use:
- To detect alveolar bone los
- Done under local anesthesia
- Confirms the extent and configuration of infrabony component of the pocket and of furcation defects
Transgingival Probing How To Use:
Question 11. Attrition
Answer:
Attrition Definition:
- Loss by wear of the surface of tooth or restoration caused by tooth to tooth contact during mastication or para-function
Attrition Clinical Features:
- Wear on occluding surfaces
- Shiny facets on amalgam contacts
- Fractures of cusps or restorations
Attrition Types:
- Physiological-Causes
- Old age- increasing age causes attrition
- Pathological-causes
- Abnormal occlusion
- Premature extraction of teeth
- Abnormal chewing habits
- Structural defects in teeth
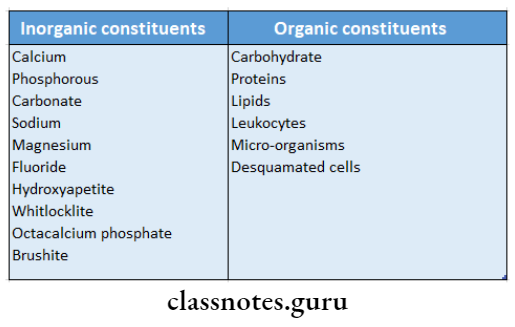
Question 12. Hydroxyapatite
Answer:
- It is calcium phosphate biomaterials used for grafting
Hydroxyapatite Advantages:
- Excellent tissue compatibility
- Doesn’t cause any inflammation or foreign body re- response
- Act as a scaffold for blood clots
- Allows bone formation
Hydroxyapatite Disadvantage:
- It is encapsulated by collagen
Question 13. Supracontacts
Answer:
- The gradual movement of teeth as a result of changes, such as a loss of a tooth or wear, can cause “supra contacts”.
- This is where the upper and lower teeth meet at this point first and causes the opposing teeth not to meet evenly.
- The jaw tries to grind away this contact that is in the way and may lead to excessive muscle activity and jaw joint dysfunction.
- Very thin marking paper, called articulating paper, can highlight the contacts of the teeth and an adjustment may be made to allow a more even bite or allow the jaw to move more freely.
- Three separate assessments are made:
- Occlusal assessment:
- Muscle assessment:
- Within the mouth
- Outside the mouth
- Neck muscles
- Measuring the amount of opening of the jaw and the various movements of the jaw and neck.
- Joint assessment
Question 14. Measurements of tooth mobility
Answer:
1. Miller mobility index:
- Grade 0- Normal tooth mobility
- Grade 1- slightly more than normal
- Grade 2- Moderately more than normal
- Grade 3- Severe mobility faciolingually
2. Grace and Smales mobility index:
- Grade 1- Mobility <1 mm buccolingually
- Grade 2- Mobility 1-2 mm Buccolingually
- Grade 3- Mobility >2 mm buccolingually and/or vertical tooth mobility
Question 15. Causes of tooth mobility
Answer:
- Alveolar bone loss
- Extension of inflammation to periodontal region
- Trauma from occlusion
- Hormonal changes
- Cysts and tumors involving the maxilla and mandible
- Periodontal surgery
Question 16. Priceline
Answer:
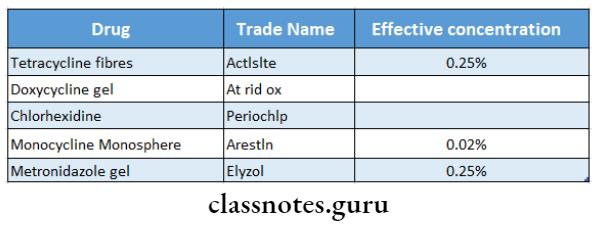
- Periocline contains a therapeutic agent which acts as a first-line defense in the treatment of moderate to severe chronic adult periodontal disease
- The active ingredient in it is minocycline
- It binds to the surface of the tooth and is gradually re- leased over time to provide simple adjunctive treatment for periodontitis
Question 17. Bicuspidization
Answer:
- Section of the root along with the respective crown portion
Bicuspidization Indications:
- Periodontal disease
- Severe bone loss
- Untreatable roots
- Root fracture
Bicuspidization Contra-Indications:
- Fused roots
- Lack of Osseous support
- Uncooperative patients