Malocclusions Definitions
1. Habits: It is a frequent or constant practice or acquired tendency, which has been fixed by frequent repetition
2. Preventive orthodontics: It is defined as the action taken to preserve the integrity of what appears to be normal occlusion at a specific time
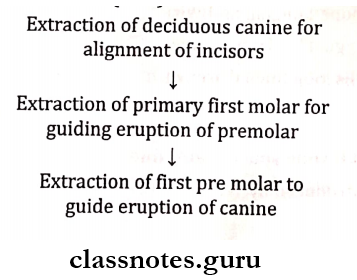
3. Serial extraction: It is defined as the correctly timed, planned removal of certain deciduous and permanent teeth in mixed dentition stages.
4. Space maintainers: Space maintainers can be defined as appliances used to maintain space or regain minor amounts of space lost, so as to guide the unerupted tooth into a proper position in the arch.
5. Myofunctional appliances: Defined as loose fitting/passive appliances which harness natural forces of orofacial musculature, that are trans¬mitted to teeth and alveolar bone.
6. Space regainers: Appliances used to regain the space lost due to early loss of primary teeth are called space regainers.
Read And Learn More: Pedodontics Short Essays Question And Answers
Malocclusions Long Essays
Question 1. Define and classify space maintainers. Write in detail about the lingual arch space maintainer.
Answer:
Space maintainers Definition: Space maintainers can be defined as appliances used to maintain space or regain minor amounts of space lost, so as to guide the unerupted tooth into a proper position in the arch.
Space maintainers Classification:
- Removal Space Maintainers
- Cast partial and wrought partial
- Active or passive
- Functional or non-functional
- Fixed Space Maintainers
- Bonded or Banded
- Active or Passive
- Functional or non-functional
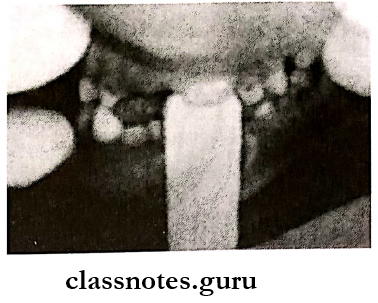
Lingual Arch Space Maintainer
It is a fixed, non-functional, passive mandibular arch appliance
Lingual Arch Space Maintainer Fabrication:
- Stainless steel wire is adapted over the lingual surfaces of teeth
- Bands are anchored over the first permanent molar
- The wire is soldered to the band
Lingual Arch Space Maintainer Indications:
- Bilateral loss of posterior teeth
- Minor movement of the anterior teeth
- Maintenance of leeway space
- Space regaining
Lingual Arch Space Maintainer Contraindications: Before the eruption of the mandibular incisors
Lingual Arch Space Maintainer Disadvantages:
- Loss of cementation and solder
- May cause untoward movement
Lingual Arch Space Maintainer Variations:
- Looped lingual archwire
- Lingual horizontal tube
- Ellis loop lingual archwire
- Lingual arch with canine spur
Question 2. Define space maintainers and space management. Write in detail about the eruption guidance appliances.
Answer:
- Space Maintainers and space management Definition: Space maintainers, can be defined as appliances used to maintain space or regain minor amounts of space lost, so as to guide the unerupted tooth into a proper position in the arch.
- Space management is defined as the process of maintaining a space in a given arch previously occupied by a tooth or a group of teeth
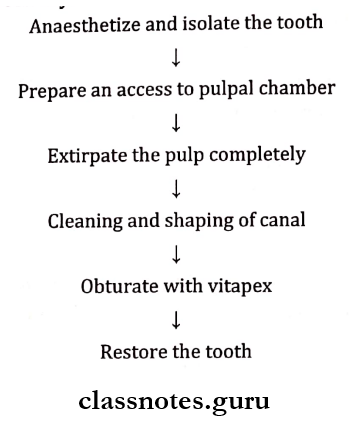
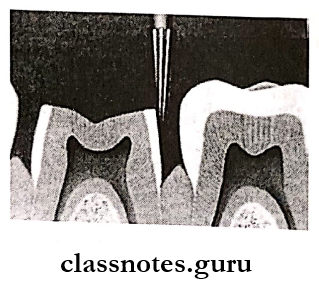
Eruption Guidance Appliance/ Distal Shoe appliance: Introduced by Willet
Eruption Guidance Appliance Indications:
- Premature loss of second primary molar
- Bilateral space loss
Eruption Guidance Appliance Contraindications:
- Inadequate abutments
- Poor patient control
- Congenital missing first molar
- Systemic diseases
Eruption Guidance Appliance Classification:
- Fixed:
- Removable:
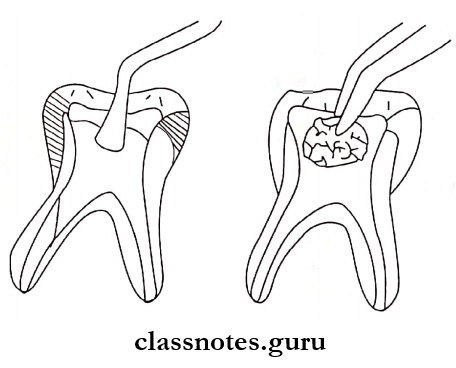
- Fabrication
- Depends on the distance between the distal surface of the primary molar to the mesial surface of the permanent molar
- The crown is fabricated over the permanent molar
- It has a mesial gingival extension
- This extension should be constructed to extend 1 mm below the marginal ridge
- Such an extension guide the eruption of underlying permanent teeth.
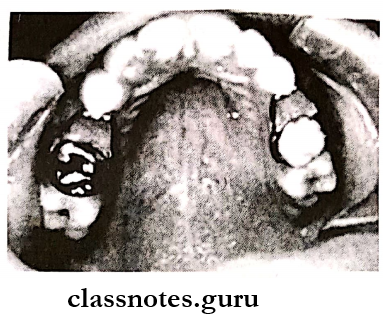
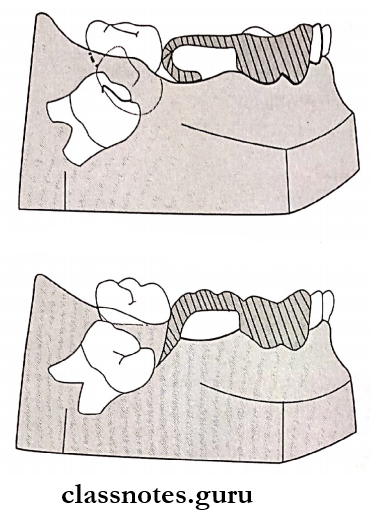
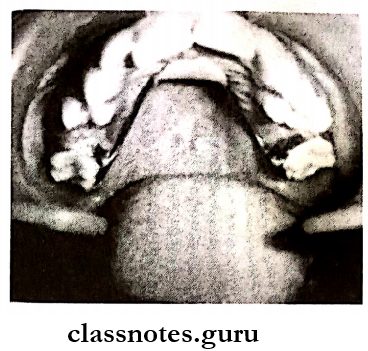
Question 3. Define serial extraction. Write about indication, contra-indications, and various methods of it.
Answer: It is defined as the correctly timed, planned removal of certain deciduous and permanent teeth in mixed dentition stages.
Serial extraction Indications:
- Class 1 with anterior crowding
- Lingually placed lateral incisors
- Severe anterior proclamation
- Unilateral loss of canine
- Abnormal resorption of deciduous
- Absence of primate spaces
- Ankylosis
- Ectopic eruption
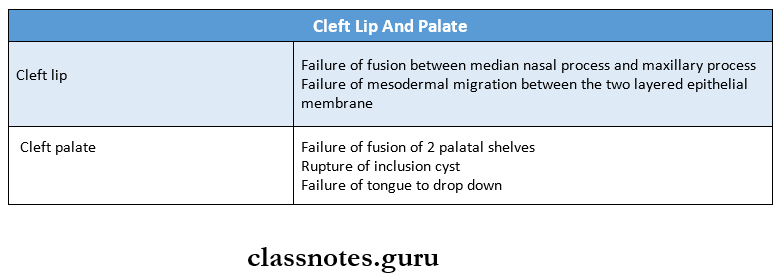
Serial extraction Contraindications:
- Mild to moderate crowding
- Congenital absence of teeth
- Extensive caries
- Deep bite or Open bite
- Severe class 2, 3
- Cleft lip and palate
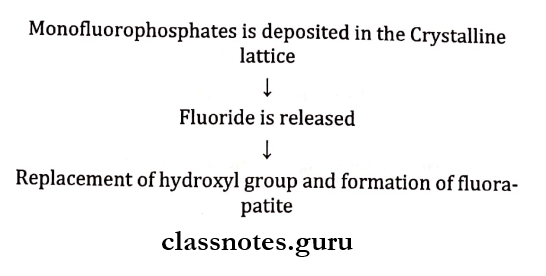
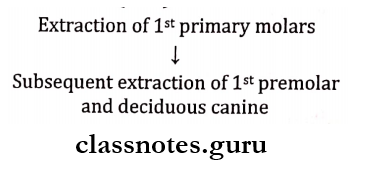
Serial extraction Method:
1. Dewel’s method (CD4):
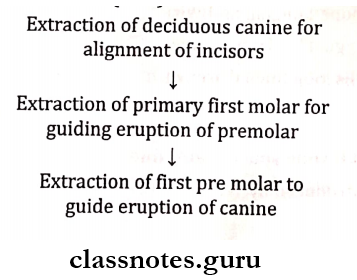
2. Tweed’s method (D4C):
Serial extraction Advantages:
- Minimizes the use of mechanotherapy
- Reduces complexity of treatment
Question 4. Define and classify oral habits. Discuss thumb-sucking habits, their effects on the oro-facial complex, and its management.
Answer:
Definition: It is a frequent or constant practice or acquired tendency, which has been fixed by frequent repetition
Oral Habits Classification:
- Obsessive:
- Non-Obsessive:
- Useful Habits and Harmful Habits:
- Pressure habits and Biting habits
- Empty habits and meaningful habits
- Compulsive habits and non-compulsive habits
Thumb Sucking Habit:
- Thumb Sucking Habit Etiology:
- Avoidance of parents
- Working mothers provide less time to the child’s nour¬ishment
- With siblings, child may feel neglected by the parents
- The insecurity felt by the children
- Weaning of bottle feeding
- Age: neonate feeling insecurity develop a habit of thumb sucking
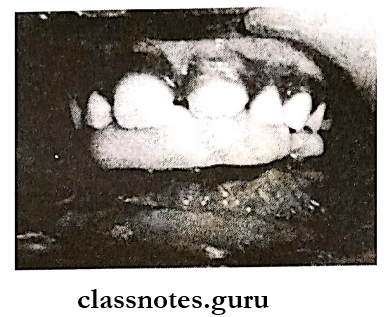
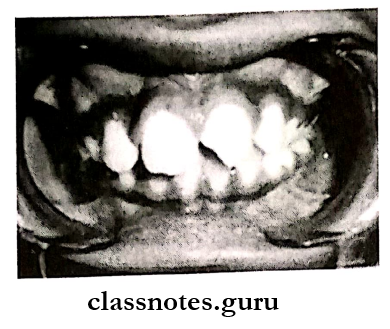
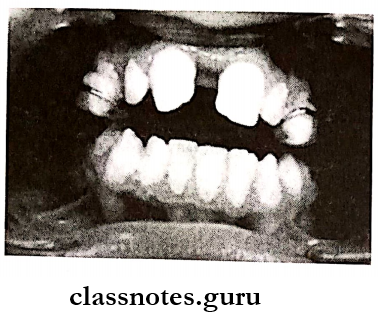
Effects On Oro Facial Complex:
- Labial tipping of maxillary anterior
- Proclination of maxillary anteriors
- Increased overjet
- Lingual tipping of mandibular anterior
- Anterior open bite
- Supra eruption of posteriors
- Narrowing of the maxillary arch
- Hypotonic upper lip
- Hyperactive mentalis activity
Thumb Sucking Habit Management:
1. Psychological approach:
- Dunlops beta hypothesis
- Dunlop suggests that the child should be asked to sit in front of the mirror and to suck his thumb
- This becomes effective when the child is asked to do it when he is engaged in an enjoyable activity
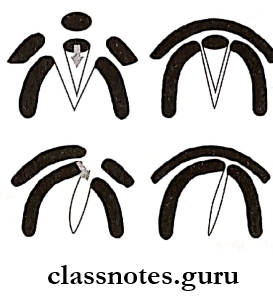
2. Mechanical aids:
- Habit-breaking appliances:
- Passive removable appliances are a palatal crib and clasps on posteriors create interference during habit
- Fixed appliances:
- Bands on molars fabricated by heavy gauge stainless steel wire
- Other aids:
- Bandaging the thumb
- Bandaging of elbow
3. Chemical aids:
Question 5. Define and classify space maintainers. Describe fixed space maintainers for bilateral loss of deciduous teeth.
Answer:
Space maintainers Definition: Space maintainers can be defined as appliances used to maintain space or regain minor amounts of space lost, so as to guide the unerupted tooth into a proper position in the arch.
Space maintainers Classification:
- Removal Space Maintainers
- Fixed Space Maintainers
- Space maintainers for bilateral loss of Deciduous teeth
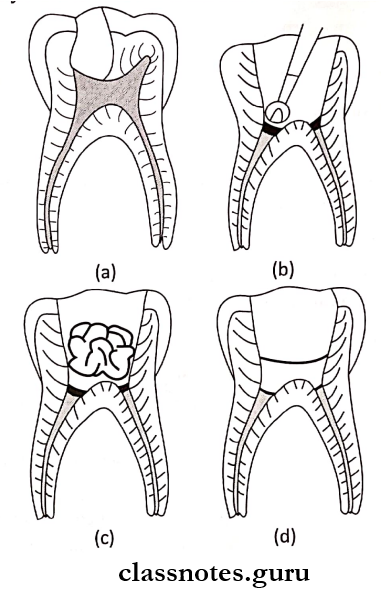
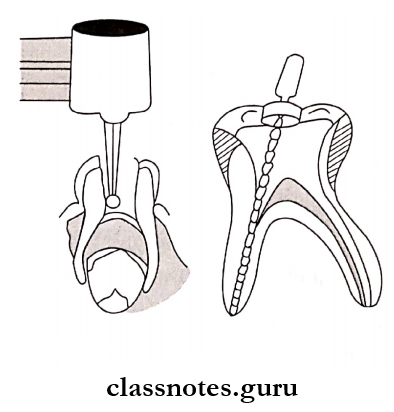
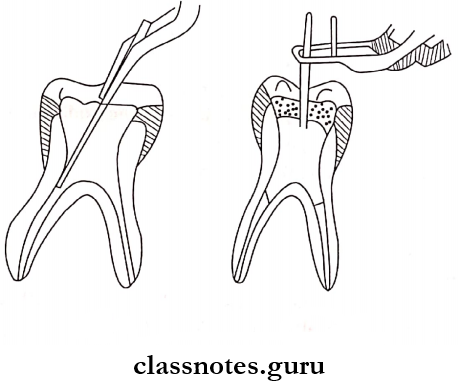
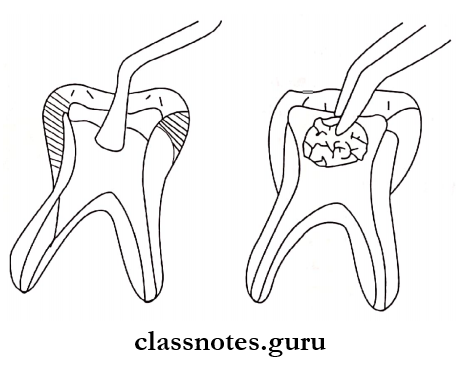
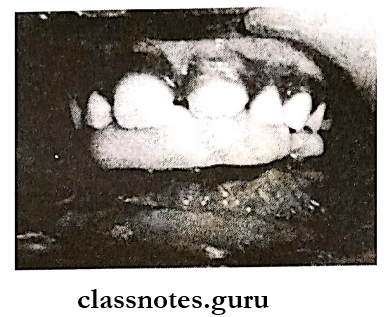
1. Band and Loop:
- The loop is solder to the band
- It should contact the mesial abutment at the contact point
- The band is used for anchorage over the distal abutment
- Space present within the loop permits the eruption of underlying permanent teeth
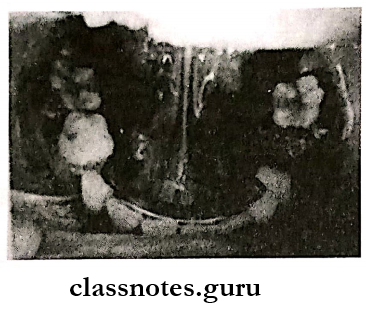
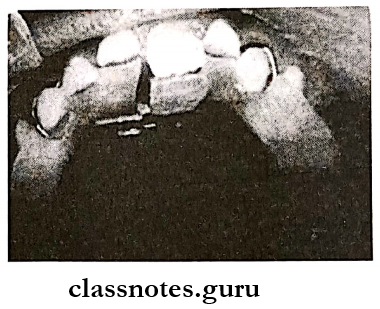
2. Lingual Arch:
- Stainless steel wire is adapted over the lingual surfaces of teeth
- Bands are anchored over the first permanent molar
- Wire is soldered to the band
Variations:
- Looped lingual archwire
- Lingual horizontal tube
- Ellis loop lingual archwire
- Lingual arch with canine spur
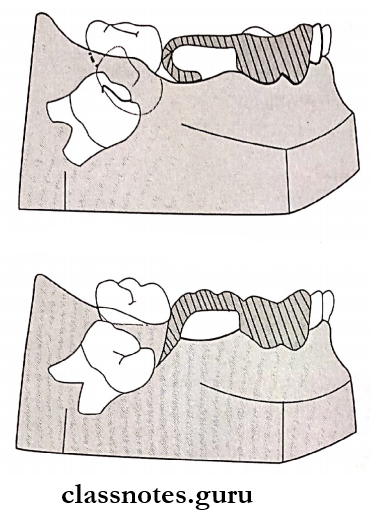
3. Distal shoe space maintainer: Introduced by Willet
Distal shoe space maintainer Design:
- Depends on the distance between the distal surface of the primary molar to the mesial surface of permanent molar
- The crown is fabricated over the permanent molar
- It has a mesial gingival extension
- This extension should be constructed to extend 1 mm below the marginal ridge
- Such an extension guide the eruption of underlying permanent teeth.
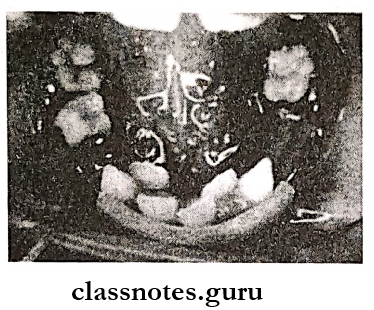
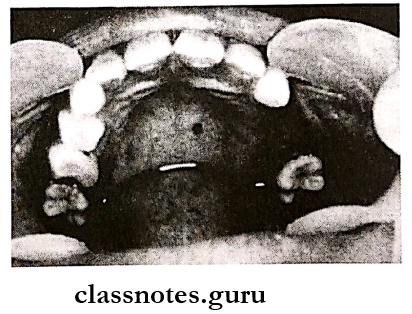
4. Nance palatal arch/nance Space holding appliance:
- Consists of bands on the upper molars
- Extend the wire from the lingual surfaces to the deepest and most anterior point in the middle of the hard palate
- An acrylic button is present on the slope of the palate
Question 6. Describe the classification, etiology, and effects of tongue thrusting habit. Write about its management.
Answer:
Tongue thrusting habit Classification:
- Physiologic – Comprises normal swallowing
- Habitual – Present even after correction
- Functional – Adaptive function
- Anatomic – Persons having a large tongue
Tongue thrusting habit Etiology:
- Persistence of infantile swallowing pattern
- Presence of upper respiratory tract infection
- Motor disability
- Missing incisors
- Bottle feeding
- Presence of other oral habits
- Macroglossia
- Hereditary
Tongue thrusting habit Effects:
1. Extraoral:
- Incompetent lips
- Backward mandibular movement
- Speech problems
- Increase in anterior facial height
2. Intraoral:
- Anterior open bite
- Increase in overjet
- Proclamation of interiors
- Posterior open bite
- Posterior crossbite
Tongue thrusting habit Management:
1. Myofunctional exercises:
- Ask to position the tongue in the rugae area for 5 minutes and swallow
- Place the tongue on the spot, salivate, squeeze against the spot, and swallow
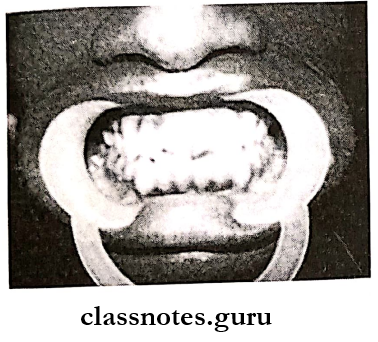
2. Pre-orthodontic trainer:
Tongue tags are used to position the tongue while tongue guards prevent the habit
3. Speech therapy:
- Ask the child to repeat simple multiplication tables of sixes
- Ask the child to pronounce words with ‘S’ sounds
4. Mechanotherapy:
- Nance Palatal Arch Appliance:
- The acrylic button of the appliance used to guide the tongue in position
- Removable Appliance:
- Hawley’s appliance is used with modifications
- They are
- Absence of acrylic portion from gingival mar¬gin of lingual surfaces of maxillary anterior
- The crib is incorporated, its loops are reduced gradually as the patient starts correct positioning of the tongue
- Fixed Appliance:
- Crowns and bands over first permanent lar along with lingual bar “
- Oral Screen:
- Modified with the addition of wire loop bar¬rier to prevent tongue thrusting
5. Surgical treatment: Orthognathic surgical procedures are carried out
Malocclusions Short Essays
Question 1. Myofunctional appliances.
Answer:
Definition: Defined as loose fitting/passive appliances which harness natural forces of orofacial musculature, that are transmitted to teeth and alveolar bone.
Myofunctional appliances Uses: Intercept and treat jaw discrepancies
Myofunctional appliances Changes:
- Increase/decrease jaw size
- Change spatial jaw relationship
- Changes direction of jaw growth
- Accelerates desired growth
Mode Of Action Of Functional Appliance.
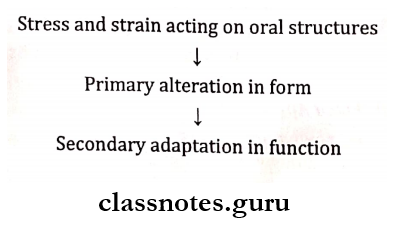
- Force Elimination by
- Bite planes – Effects:
- Disocclude the posterior teeth
- Differential eruption of posteriors
- Intrusion of incisors
- Downward and backward mandibular rotation
- Reduces mandibular prognatism
- Shields/Screens – Effects:
- Prevents muscular forces on dental alveolar structures
- Allows unrestricted growth of the jaw
- Construction bite – Effects:
- Displaces mandible from its rest position
- Stretches muscles
- Displaces mandible in the sagittal and transverse plane
Question 2. Mixed dentition analysis.
Answer:
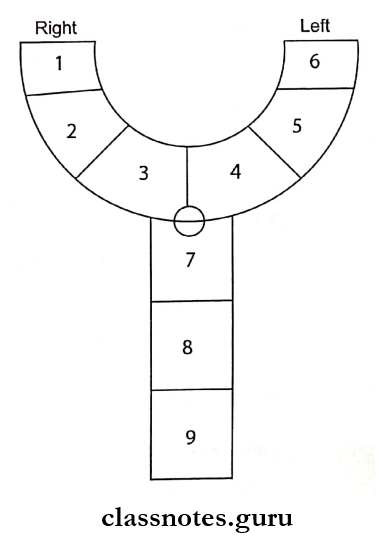
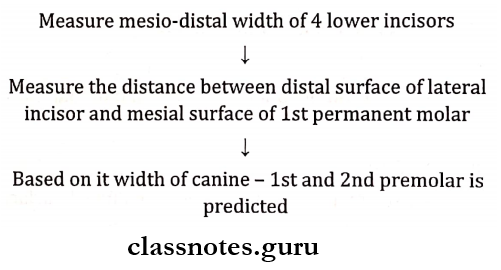
Moyer’s Mixed Dentition Analysis: To evaluate the amount of space available in the arch for erupting permanent canine and premolar
1. Mixed dentition analysis Procedure:
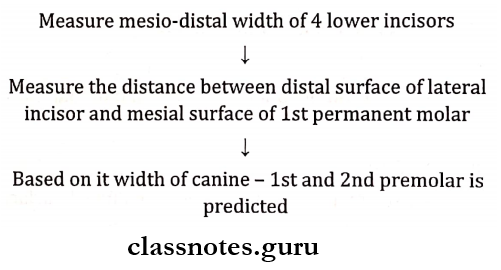
Mixed dentition analysis Inference:
- Compare tooth sizes of 3, 4, and 5 and the arch lengths available
- Predicted value > arch length available → Crowding
2. Radiographic method:
- Determine the width of unerupted teeth
- Erupted teeth in a radiograph and on a cast
- Formula Y1 = XI * Y2 / X2
- i.e. Width of the unerupted tooth to be determined
- Width of tooth erupted on cast * Width of tooth erupted on the radiograph
- Width of erupted tooth in the oral cavity on the radiograph
Question 3. Nance’s Arch Holding Appliance.
Answer:
Nance’s Arch Holding Appliance Indications:
- Bilateral loss of deciduous molars
- Combined with habit-breaking appliances
Nance’s Arch Holding Appliance Contraindications:
- If either of the molars has not erupted
- Palatal lesions
Nance’s Arch Holding Appliance Disadvantages: Tissue hyperplasia and infection due to poor oral hygiene
Nance’s Arch Holding Appliance Design:
- Consists of bands on the upper molars
- Extend the wire from the lingual surfaces to the deepest and most anterior point in the middle of the hard palate
- An acrylic button is present on the slope of the palate
Question 4. Clinical Features of Mouth Breathing.
Answer:
Extraoral
- Increased facial height Increased mandibular plane
- Retrognathic mandible
- Long and narrow face
- Narrow nose
- Short and flaccid upper lip
- Speech deformities
- Decreased sense of smell and taste
Intraoral
- High palatial vault
- Retroclined interiors
- V-shaped palate
- Posterior crossbite
- Constricted maxillary arch
- Decrease overbite
- Hyperplastic gingiva
- Marginal gingivitis
- Deep pockets
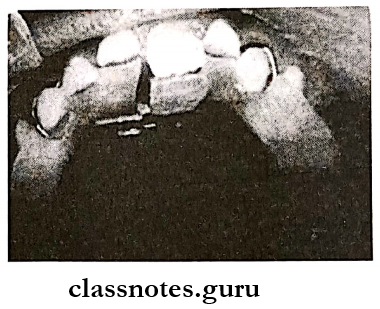
Question 5. Band and Loop.
Answer:
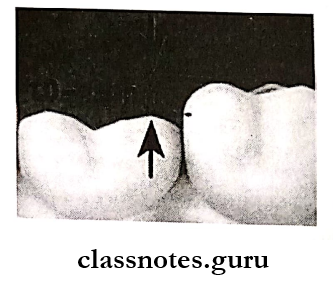
Band and Loop Indications:
- Premature loss of primary first molar
- Unerupted premolar
Band and Loop Contraindications:
- Extreme crowding
- High caries activity
Band and Loop Modifications:
- Loop on only one side of the arch
- Addition of occlusal rest to prevent slippage of appliance gingivally
- Fabrication of a crown instead of a band
- Reverse – by the anchoring band on the mesial abutment
Question 6. Space Regainers./Fixed space regainers.
Answer: Appliances used to regain the space lost due to early loss of primary teeth are called space regainers.
1. Fixed Space Regainers:
- Open Coil Space Regainer:
- The molar band is fitted to the 1st permanent molar
- Molar tubes are soldered over it
- Stainless steel wire is bent into U shape
- Select the open coil spring and it is slide on the wire
2. Gerber Space Maintainer:
- U assembly welded to the tube is fitted in the tube
- U bend contact the tooth mesial to the edentulous area
3. Horizontal lingual arch:
- The wire is adapted along the lingual surfaces of teeth
- Canine spurs are added to it
4. Lip Bumper:
- The wire is adapted along the labial surfaces of teeth
- U bent is incorporated just before it enters the mo¬lar tube
- The acrylic portion is present in the anterior region
5. Removable Space Regainer:
- Free End Loop:
- Labial wire with a back action loop spring is used
- Split Block:
- Acrylic block is splittedbuccolingually and joined by wire in the form of a loop
- Slingshot:
- Wire elastic holder with hooks is used
- Jack screw:
- Incorporate and expand screw
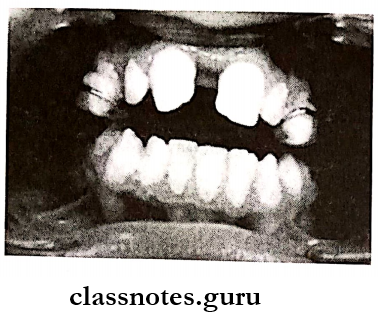
Question 7. Crossbite.
Answer: It is an abnormal labiolingual relationship between one or more teeth
Crossbite Classification:
- Anterior and Posterior
- Unilateral and Bilateral
- True and Functional
- Combination
Crossbite Causes:
- Tooth size-jaw size discrepancy
- Skeletal discrepancy
- Palatally placed teeth
- Supernumerary teeth
- Presence of any pathology
- Decreased muscle tone
- Ectopic eruption
- Cleft palate
- Premature contacts
- Mouth breathing habit
Crossbite Treatment:
- Anterior Crossbite:
- Removal of premature tooth contact:
- Tongue blade therapy:
- Lower incisors are used as fulcrums
- The tongue blade is placed at 45° behind the tooth
- Push the locked teeth
- Used for 1-2 hours daily for 10-14 days
- Lower inclined plane:
- Catlan’s Appliance:
- An acrylic inclined plane is fabricated
- It is cemented over the lower anterior teeth
- It is fabricated at 45° to the long axis of the lower incisors
- Stainless steel crown: For lower incisor
- Composite inclines: Build up over lower teeth
- Removable Hawley’s appliance:
- Adam’s clasp over molars
- Z springs incorporated into acrylic resin
- Fixed appliances:
- Auxiliary springs used along lingual or palatal arches
- Posterior Crossbite
- Occlusal equilibrium: Removal of occlusal interfer-ences
- Removable W arch appliance:
- Cross elastic appliance:
- Bands are adapted over teeth
- A hook is welded to bands to engage elastic
- Removable Hawley’s appliance:
- Skeletal Correction: Use of expansion appliances
Question 8. Midline Diastema.
Answer: It is the spacing present between the maxillary anterior
Midline Diastema Etiology:
- Ugly duckling stage
- Thumb sucking habit
- High frenum attachment
- Supernumerary teeth i.e. mesiodens
- Tooth size – a material discrepancy
- Presence of pathology
Midline Diastema Treatment:
1. Removable appliances:
- Acrylic plate along with finger springs
- Hawley’s appliance
- Split labial bow
2. Fixed appliances:
- Closed coiled springs
- M shaped elastic
Question 9. Anterior crossbite.
Answer:
Anterior crossbite Definition: It is defined as malocclusion resulting from the lingual position of the maxillary anterior teeth in relationship with the mandibular anterior teeth.
Anterior crossbite Etiology
- Persistence of deciduous teeth
- Arch length- tooth material discrepancy
- Presence of habits such as thumb-sucking and mouth breathing
- Retarded development of the maxilla
- Narrow upper arch
- The collapse of the maxillary arch
- Unilateral hypo or hyperplastic growth of any of the jaws
Anterior crossbite Management
1. Use of removable appliances
- Use of tongue blade
- It is used to treat single-tooth anterior crossbite
- It resembles ice cream stick
- It is placed inside the mouth contacting the palatal aspect of the tooth in crossbite
- Rest the blade on the mandibular tooth
- The patient is asked to rotate the oral part of the blade upwards and forward
- Repeat the exercise for 1-2 hours for about 2 weeks
- Catlan’s appliance
- It is a lower inclined plane constructed on a maxillary arch
- Have 45° angulation
- Forces the maxillary teeth to a more labial position
- Use of Z spring
- Used to treat anterior cross bites involving one or two maxillary teeth
- Used when there is adequate space for labialization
2. Use of fixed appliances
- Multilooped archwires or nickel-titanium archwires are used for corrections
- Indications
- Dental anterior crossbites involving one or more teeth
- Requirement of more tooth movement along with correction of crowding and rotations
- Patients who exhibit minimal overbite
Malocclusions Short Answers
Question 1. Gebner’s space regainer.
Answer:
- Gerber appliance may be fabricated directly in the mouth or in a relatively short appointment period and requires no lab work
- A seamless orthodontic band or crown is selected for the tooth to be destabilized
- This space regainer consists of U-shaped hollow tubing soldered or welded to the mesial aspect of the first molar to be moved distally
- U-shaped rods with open coil springs of adequate length are fitted into the above tubing so that they contact the mesial aspect of the first molar to be moved distally
- The forces generated by compressed coil springs bring about a distal movement of the first molar
Question 2. Inclined Plane/Catlan’s appliance.
Answer:
Inclined Plane Use:
- Treatment of anterior crossbite
- Palatally displaced maxillary incisor
Inclined Plane Design: Acrylic/metal covering the maxillary incisor at 45° angulation
Inclined Plane Disadvantage:
- Problem in speech
- Dietary restriction
- Supra eruption of posteriors
Question 3. Treatment of Anterior Crossbite.
Answer:
Crossbite: Condition where one/more teeth may be malposed abnormally, buccally or lingually or labially with reference to the opposing tooth/teeth.
Crossbite Classification:
- Single tooth crossbite
- Segmental cross bite
Crossbite Treatment:
- Use of tongue blade
- Catlan’s appliance
- Z spring
- Screw appliances
- Face mask
- Frankel 3
- Chin cup appliances
Question 4. Space Regainers.
Answer: Appliances used to regain the space lost due to early loss of primary teeth are called space regainers.
1. Fixed Space Regainers:
- Open Coil Space Regainer
- Gerber space maintainer
- Horizontal lingual arch
- Lip bumper
2. Removable space regainers:
- Free end loop
- Split block
- Slingshot
- Jack screw
Question 5. Lingual arch space maintainer.
Answer: It is a fixed, non-functional, passive mandibular arch appliance
Lingual arch space maintainer Indications:
- Bilateral loss of posterior teeth
- Minor movement of the anterior teeth
- Maintenance of leeway space
- Space regaining
Lingual arch space maintainer Contraindications: Before the eruption of the mandibular incisors
Lingual arch space maintainer Disadvantages:
- Loss of cementation and solder
- May cause untoward movement
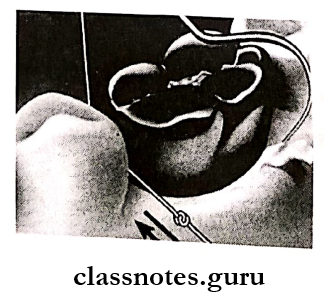
Question 6. Oral Screen.
Answer: Introduced by Newell in 1912
Oral Screen Principle:
- Application of muscular forces to teeth or
- Elimination of forces to teeth
Oral Screen Indications
- Interception of habits
- Treatment of mild malocclusion
- For muscular exercises
- Correction of mild anterior proclamation
Question 7. Transpalatal arch.
Answer:
Transpalatal arch Indications Unilateral space loss
Transpalatal arch Contraindications Bilateral space loss
Transpalatal arch Appliance:
- Used in the maxillary arch
- Wire crosses the palate
- Bands are fabricated over molars
- Wire are soldered to the bands
Question 8. Lip Bumper.
Answer: Combined removable fixed appliance
Lip Bumper Mode Of Action: Force application/elimination
Lip Bumper Uses:
- Interception of lip-biting habits
- Increases arch length
- Reduces crowding
- In the case of hyperactive mentalis activity
- For augmentation of anchorage
- For visualization of 1st molar
- Used as space regainer
Lip Bumper Designs:
- Stainless steel wire from one molar to the opposite molar passing away from anterior
- An acrylic portion from canine to canine
Question 9. Angle’s Classification.
Answer:
- Class 1 – The mesiobuccal cusp of the upper first permanent molar coincides with the mesial groove of a lower first permanent molar.
- Class 2 – The distobuccal cusp of the upper first permanent molar coincides with the mesial groove of the lower first permanent molar
- Class 3 – The mesiobuccal cusp of the upper first permanent molar coincides interdentally between the lower first and second permanent molar
Question 10. Factors considered before placement of space maintainers.
Answer:
- Patient’s cooperation
- Appliance integrity
- Space required
- Space available
- Position of incisors
- Crowding severity
- Depth of curve of Spee
- Position of midline
- Leeway space
Question 11. Tanaka and Johnston Analysis.
Answer:
- Half the mesiodistal width of 4 lower incisors + 10.5 = Mandibular 3 + 4 + 5 in one quadrant
- Half the mesiodistal width of 4 lower incisors + 11.0 = Maxillary 3 + 4 + 5 in one quadrant
Question 12. Masochistic Habits/Self-Mutilating Habits.
Answer: Repetitive acts that result in physical damage to the individual
Masochistic Habits Etiology:
- Syndrome associated
- Superimposed on a pre-existing lesion
- Secondary to habit
- Unknown etiology
Masochistic Habits Types:
- Frenum thrusting
- Bobby Pin Opening
Question 13. Bruxism
Answer: It is a habitual grinding of teeth either during sleep in the night or unconsciously during day time.
Bruxism Causes:
- Occlusal disturbances
- Emotional disturbances
- Occupational
Bruxism Features:
- Attrition of teeth
- Loosening and drifting of teeth
- Gingival recession
- Hypertrophy of muscles
- Sensitivity of teeth
- Facial pain
- Trismus
Bruxism Treatment: Use of occlusal splints
Question 14. Inclined plane
Answer:
Inclined plane Use:
- Treatment of anterior crossbite
- Palatally displaced maxillary incisor
Inclined plane Design:
Acrylic/metal covering the maxillary incisor at 45o angulation
Inclined plane Disadvantage:
- Problem in speech
- Dietary restriction
- Supra eruption of posteriors
Question 15. Dunlop’s beta hypothesis
Answer:
- It is used for thumb-sucking habit
- Dunlop suggests that the child should be asked to sit in front of the mirror and to suck his thumb
- This becomes effective when the child is asked to do it when he is engaged in an enjoyable activity
Malocclusions Viva Voce
- Space maintainers are contraindicated in crowded occlusions
- Nance is called the father of serial extraction
- A lip bumper is also called a modified vestibular screen
- Maximum space is lost during six months of extraction
- Space regained by space regainers should be maintained until adjacent permanent teeth have erupted completely
- Reverse band and loop is indicated where there is premature loss of the primary second molar and the permanent molar have not erupted fully
- A lingual arch space maintainer is the most effective appliance of space maintenance and minor tooth movement in the lower arch
- Self-injurious habits are also called masochistic habits
- Masochistic habits have a higher incidence in mentally retarded children
- Nail biting is a sign of internal tension
- Mouth breathing habit is diagnosed by mirror test, water holding test, butterfly test, and rhinometry.
- Tongue thrusting habit often self-corrects by 8-9 years of age
- Bluegrass appliance is used to manage thumb suck-ing habits in children between 7-13 years of age