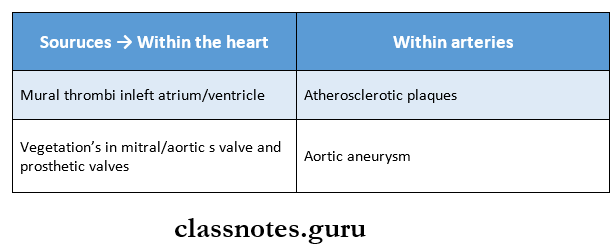
Hemodynamic Derangements Due To Obstructive Nature Important Notes
1. Virchow’s triad includes
- Endothelial injury
- Alteration in blood flow
- Hypercoagulability of blood
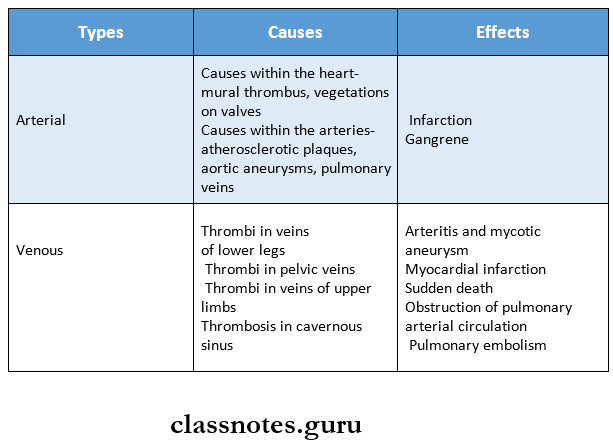
2. Arterial thrombi
- They are white, firm, mural
- It produces ischemia
3. Venous thrombi
- They are red, soft occlusive
- Causes embolism
- It may arise from thrombi in veins of the lower legs, pelvic veins, veins of upper limbs, cavernous sinus of the brain and right side of the heart
- It leads to obstruction of pulmonary arterial circulation leading to pulmonary embolism
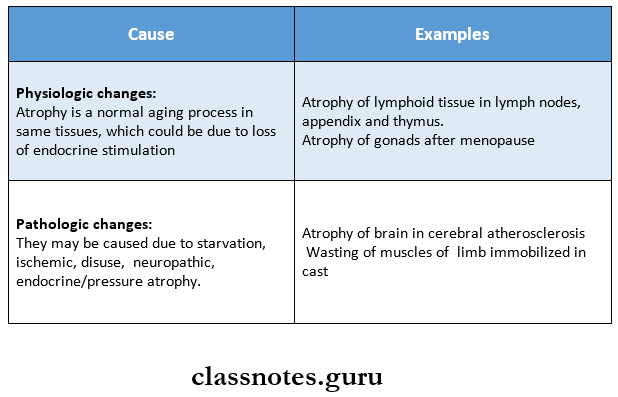
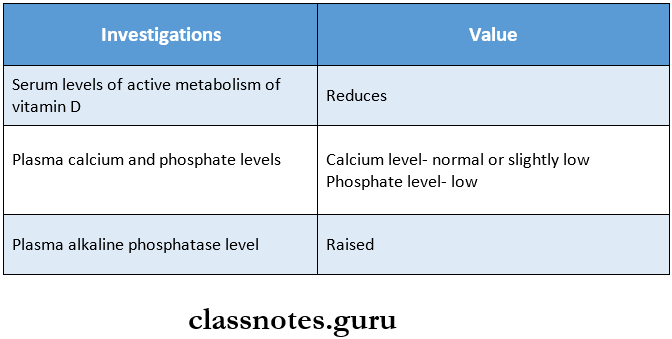
4. Infarcts
Hemodynamic Derangements Due To Obstructive Nature Long Essays
Question 1. Define thrombosis. Discuss etiopathogenesis of thrombus.
Answer:
Thrombosis:
- Thrombosis is a process of the formation of solid mass in circulation from the constituents of flowing blood.
- The mass itself is called a thrombus.
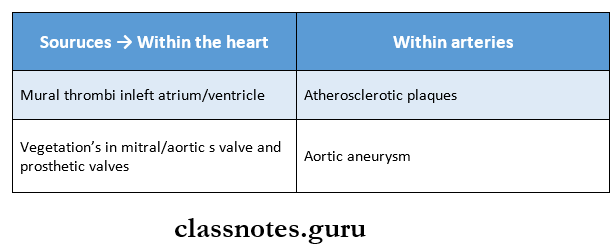
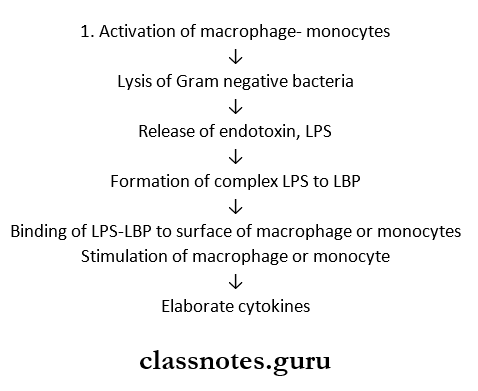
Thrombus Etiopathogenesis:
There are primary events that pre-dispose to thrombus formation. It is called as vir- chow’straid.
1. Endothelial injury:
The integrity of the blood vessel wall is important for maintaining normal blood flow.
- Vascular injury exposes the subendothelial connective tissue (For example. Collagen, elastin, fibronectin, calamine, and glycosaminoglycans) which are thrombogenic and thus play an important role in initiating hemostasis as well as thrombosis.
- Conditions and factors which cause endothelial injury and predispose to thrombogenesis are as follows:
- Endocardial injury in myocardial infarction, myocarditis, cardiac surgery, prosthetic valves.
- Ulcerated plaques in advanced atherosclerosis.
- Haemodynamic stress in hypertension.
- Arterial diseases
- Diabetes mellitus
- Endogenous chemical agents such as endotoxins, hypercholesterolemia
- Exogenous chemical agents such as cigarette smoke.
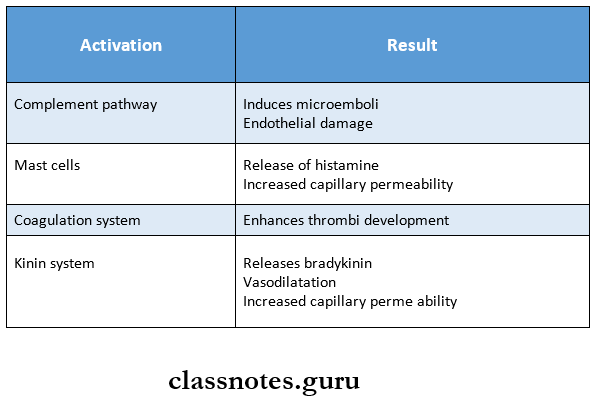
- Following endothelial cell injury, platelets come to play a central role sequence of events are:
- Platelet Adhesion: Platelets in circulation recognize the site of endothelial injury and adhere to exposed sub endothelial collagen (Primary aggre¬gation).
- Platelet release reaction: Activated platelets then undergo a release reaction by which platelet gran¬ules are released to the exterior.
- Platelet aggregation: Two main types of platelet granules are.
- Alpha granules containing fibrinogen, fibronectin, platelet factor 4, and cationic pro¬teins.
- Dense bodies – ADP (Adenosine diphosphate), 5 – HT (serotonin), histamine, epinephrine, ionic calcium.
Read And Learn More: Pathology Question And Answers
Following the release of ADP, potent platelet aggregating agent, aggregation of additional platelets takes place (secondary aggregation).
- This results in the formation of a temporary hemostatic plug.
- The stable hemostatic plug is formed by fibrin, thrombin, and thromboxane A2.
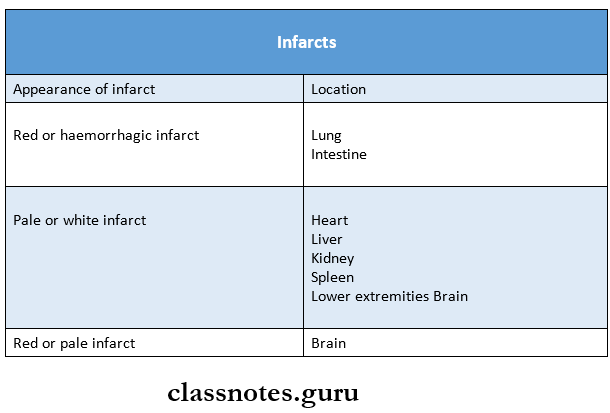
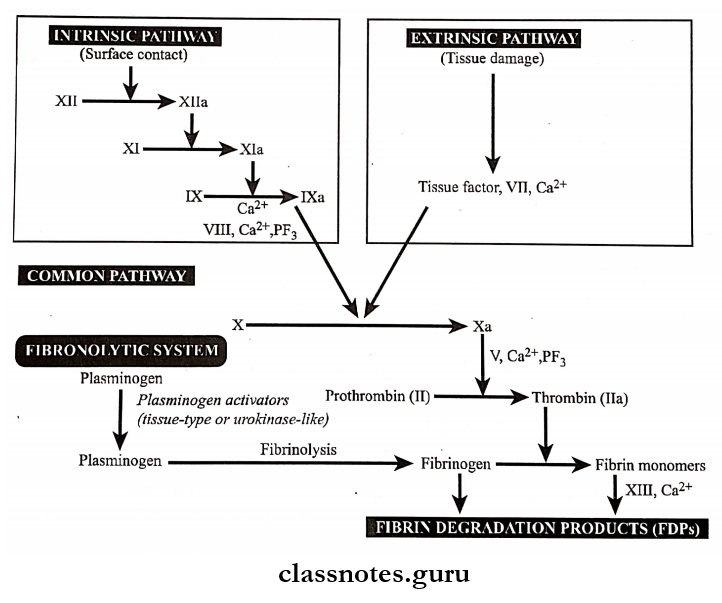
- The coagulation system is involved in both the hemostatic process and thrombus formation.
- The coagulation mechanism is the conversion of the plasma fibrinogen into a solid mass of fibrin.
- Pathways of the coagulation system and fibrinolytic system.
2. Alteration of blood flow:
- Normally, there is the axial flow of blood in which a rapidly moving central stream – consists of leu¬cocytes and red cells. Slow-moving laminar stream – adjacent to central stream – consists of platelets peripheral stream – consists of most slow-moving cell-free plasma.
- In thrombosis, turbulence and stasis occur. Where normal flow is disturbed when blood slow down, blood cells including platelets mar- migrate to the periphery and kind of pavement closed to the endothelium. (Margination and pave- meeting).
- Stasis allows a higher release of oxygen from the blood and initiates venous thrombi even without evidence of endothelial injury.
- Turbulence injures the endothelium resulting in the deposition of platelets and fibrin – facilitating the formation of arterial and cardiac thrombi.
3. Hypercoagulability of blood:
- Hypercoagulability of blood is loosely defined as any alteration of coagulation pathways that pre¬disposes to thrombosis.
- It is brought about by following changes in the blood composition.
- Increase in coagulation factors like fibrinogen, prothrombin, factor 7 a, 7 a, and Xa.
- Increase in platelet count and their adhesiveness
- Decreased levels of coagulation inhibitors like anti-thrombin 3, and fibrin split products.
Question 2. Mention types and discuss the fate of the thrombus.
Answer:
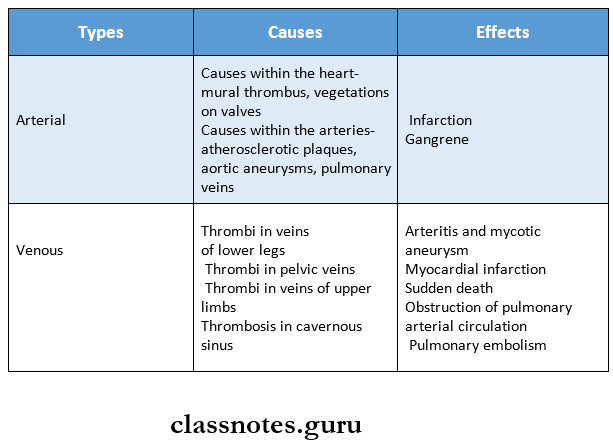
Types of Thrombi:
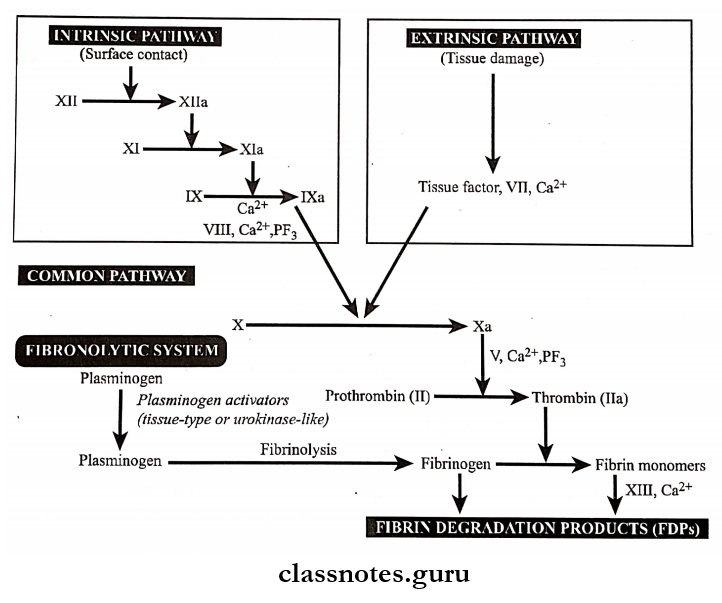
- Thrombi can develop anywhere in the cardiovascular system i.e., in cardiac chambers, on valves, or in arteries, veins/capillaries.
- The size and shape of the thrombus depend on the site of origin and the cause.
Various types of thrombi are as follows:
1. Mural thrombi:
- Thrombi occurring in the heart chambers or in the aortic lumen are known as mural thrombi.
- Abnormal myocardial contraction or endomyocar¬dial injury promotes cardiac mural thrombi.
2. Arterial thrombi:
- They are white or pale in color.
- Microscopically, distinct lines of Zahn composed of platelets, and fibrin with enlarged red and white blood cells are seen.
- Arterial thrombi produce ischemia and infarction.
3. Venous thrombi:
- Venous thrombi are red and occlusive
- Microscopically, distinct lines of Zahn with more abundant red blood cells are seen.
- Red (venous) thrombi have more abundant red cells, leucocytes, and platelets entrapped in fibrin meshwork. Thus, red thrombi closely resemble blood clots in vitro.
- Venous thrombi cause embolism.
4. Post mortum thrombi:
They are gelatinous with a dark red dependent portion where red cells have settled by gravity and a yellow chicken fat supernatant and they are usually not attached to the underlying wall.
5. Vegetation:
- Thrombi occurring on the heart valves are called vegetation.
- Bacterial or fungal blood-borne infections can cause valve damage, leading to large thrombotic masses.
- Sterile vegetation can also develop on non-infected valves in a hypercoagulable state, so-called non-bacterial thrombotic endocarditis.
The fate of Thrombus:
1. Resolution:
- Thrombus activates the fibrinolytic system with the consequent release of plasmin which may dissolve the thrombus completely resulting in resolution.
- Usually, lysis is complete in small venous thrombi while large thrombi may not be dis¬solved.
2. Organisation:
- If the thrombus is not removed, it starts getting organized phagocytic cells (neutro¬phils and macrophages) appear and begin to phagocytose fibrin and cell debris. Capillaries grow into the thrombus from the site of the attachment and fibroblasts start invading the thrombus.
- Thus, fibrovascular granulation tissue is formed which subsequently becomes dense and less vascular and is covered over by endothelial cells.
- This way thrombus is excluded from the vascular lumen and becomes part of the vessel wall.
- The new vascular channels in it may be able to re-establish the blood flow, called recanaliza¬tion.
- The fibrosis thrombus may undergo hyalinization and calcification example phlebitis in the pelvic reins.
3. Propagation:
Thrombus may enlarge in size due to more and more deposition from the constitu¬ents of flowing blood. In this way, it may ultimately cause obstruction of some important ves¬sel.
4. Thrombo embolism:
Thrombi in the early stage and infected thrombi are quite friable and may get detached from the vessel wall. These are released in the bloodstream as emboli which produce ill effects at the site of their lodgement.
Question 3. Define embolism. Give an account of various types of embolism.
Answer:
Embolism: Embolism is the partial/complete obstruc¬tion of some part of the cardiovascular system by any mass carried in the circulation, the transported intravas¬cular mass detached from the site of origin is called an embolus.
Types of Emboli:
1. Depending upon the matter in the emboli.
- Solid
- Example: Detached thrombi (thrombotic emboli), tissue fragments, parasites, and foreign bodies.
- Liquid
- Examples: Fat globules, amniotic fluid, bone marrow.
- Gaseous
- Example: Air, other gases
2. Depending upon whether infected or not.
- Bland – when sterile
- Septic – when infected
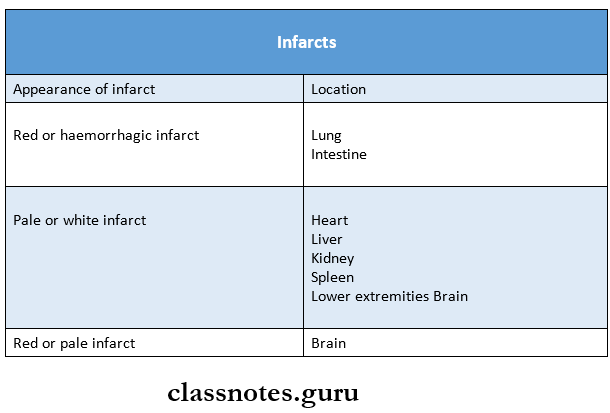
3. Depending upon the source of emboli.
- Cardiac emboli
- Example: Bmboli originating from atrium and atrial appendages, infarct in the left ventricle.
- Arterial emboli
- Example: In systemic arteries in the brain, spleen, kidney, and intestine.
- Venous emboli
- Example: In systemic arteries in the brain, spleen, kidney, and intestine.
- Lymphatic emboli can also occur.
4. Depending upon the flow of blood.
- Paradoxical embolus: An embolus which is carried from the venous side of circulation to the arterial side/vice versa is called paradoxical/crossed em¬bolus.
- Retrograde embolus: An embolus which travels against the flow of blood is called retrograde em-bolus.
Question 4. Define infarction. Describe the pathology of the infarct.
Answer:
Infraction:
Definition: Infarction is the process of tissue necrosis resulting from some form of circulatory insufficiency, the localized area of necrosis of developed is called an “infarct.
Infarct Etiology:
- Interrupted arterial blood supply is called ischemic necrosis.
- Less commonly venous obstruct (stagnant hypoxia).
- Sudden complete and continuous occlusion by thrombosis/embolism produces infarcts.
- Also by mono occlusive circulatory insufficiency.
- Example: Incomplete atherosclerotic narrowing of coro¬nary arteries may produce myocardial due to acute coronary insufficiency.
Types of infarcts:
1. Acc to colour:
- Pale/Anaemic: due to arterial occlusion And are seen in compact organs example., In the kidneys, heart, and spleen.
- Read/Haemorrhagic: Seen in soft loose tissue And are caused either by pulmonary arterial obstruction (example, in the lungs) or by arterial/venous occlusion (example In the intestines)
2. Acc. to age:
3. Acc. to presence/absence of infection: Bland, when free of bacteria contamination septic, when infected.
Infarct Pathogenesis:
- Localized hyperemia occurs immediately after ischemia. Within a few hours, the affected part becomes swol¬len because of edema And hemorrhage.
- Early changes are cloudy swelling And degeneration. Pro-gressive autolysis of necrotic tissue And hemolysis of red cells follows.
- An acute inflammatory reaction And hyperemia appear in the. surrounding tissue. Blood pigments are deposited in the infarct.
- There is progressive ingrowth of granulation tissue. Finally, the infarct is replaced by a fibrous scar.
Gross Appearance:
- All infarcts tend to be usually wedge-shaped, the apex pointing towards the occluded vessel And the wide base on the surface of the organ.
- Infarct due to arterial occlusion is pale while those due to venous obstructions are hemorrhagic.
- The recent infarcts are generally slightly elevated over the surface while the old infarcts are shrunken And de-pressed under the surface of the organ.
Histologic Characteristics of Infraction:
- The dominant histologic characteristic of infarction is ischemic coagulative necrosis of the affected area.
- It generally contains the same amount of hemorrhage.
- At the periphery, there is inflammatory reactions pre-dominated by neutrophils initially later even macro¬phages and fibroblasts appear.
- Most infarcts are ultimately replaced by fibrous tissue, which at times may show calcification. The brain is an exception. In CNS, liquefactive necrosis takes place.
Question 5. Describe the morphology and microscopic structure of cardiac infarction.
Answer:
Cardiac infarction Morphology:
- Infarcts of solid organs are usually wedged shaped
- Apex points towards the occluded artery and base on the surface of the organ
- Infarcts due to arterial occlusion appear pale and due to venous obstruction are hemorrhagic
- Red cells are lysed
- Cerebral infarcts
- Poorly defined
- Central softening
- New infarcts appear slightly elevated over the surface
- Old infarcts are shrunken and depressed under the surface
Cardiac infarction Microscopic Structure:
- It shows coagulative necrosis of the affected area of tissue or organ
- Shows some amount of hemorrhage
- At the periphery inflammatory reaction is seen
- Cerebral infarcts show liquefaction necrosis
- Gliosis occurs later
- Initially
- Neutrophils are predominately present
- Other cells present are macrophages and fibro¬blasts
- Later
- The necrotic area is replaced by a fibrous scar
- May show dystrophic calcification
Hemodynamic Derangements Due To Obstructive Nature Short Essays
Question 1. Fat emboli
Answer:
- Obstruction of arterioles and capillaries by fat globules constitutes fat embolism.
- If the obstruction in the circulation is by fragments of adipose tissue, it is called a fat-tissue embolism.
Fat emboli Etiology:
1. Traumatic causes:
- Trauma to bones- a most common cause.
- Example: In fractures of long bones leading to the passage of fatty marrow in circulation, after orthopedic surgi¬cal procedures, etc.
- Trauma to soft tissue
- Example: Laceration of adipose tissue and in puerperium due to injury to pelvic fatty tissue.
2. Non-traumatic causes:
- Extensive burns
- Diabetes mellitus
- Fatty liver
- Pancreatitis
- Sickle cell anemia
- Decompression sickness
- Inflammation of bones and soft tissues
- Extrinsic fat/oils are introduced into the body.
Fat emboli Pathogenesis:
There are few mechanisms to explain the pathogenesis.
- Mechanical theory: Mobilisation of fluid fat following trauma to bones or soft tissues Releases fat glob¬ules which may enter venous circulation.
- Emulsion instability theory: In non-traumatic cases, fat emboli are formed by aggregation of plasma lipids due to disturbance in the natural emulsification of fat
- Intravascular coagulation theory: In stress, the release of some factors activates intravascular coagulation (DIC) and aggregation of fat emboli.
- Toxic injury theory: Blood vessels of the lungs are chemically injured resulting in increased vascular permeability and consequent pulmonary edema.
Fat emboli Consequences:
- Pulmonary fat embolism: Widespread obstruction can result in sudden death.
- Systemic fat embolism: Petechial skin rash, petechial hemorrhages, decreased glomerular filtration, renal insufficiency, etc.
Question 2. Caissons disease
Answer:
- Decompression sickness is a specialized form of gas embolism and is known as Caisson’s disease
- It occurs when individuals are exposed to sudden changes in atmospheric pressure
- As seen in the deep sea, in underwater construction workers, and in individuals in unpressurized aircraft
Fat emboli Pathogenesis:
Produced when the individual decompresses suddenly either from high atmospheric pressure to normal level or from normal to low level
Fat emboli Features:
- Formation of minute gas bubbles in
- Skeletal muscles
- Supporting tissues in and about the joints
- This creates bends
- In the lungs, edema, hemorrhage, and focal atelectasis or emphysema may appear
- It may lead to sudden respiratory distress called chokes
Fat emboli Treatment:
Place the individual in a compression chamber which permits slow decompression of the individual
Question 3. Air emboli
Answer:
- Air embolism occurs when air is introduced into venous or arterial circulation.
- Gas bubbles within the circulation can obstruct vascular flow.
Venous air embolism: Air may be sucked into systemic veins during.
- Operations on head and neck and trauma
- Obstetrical operations and trauma
- Intravenous infusion of blood and fluids
- Angiography.
Arterial air embolism: Entry of air into pulmonary veins or its tributaries may occur in the following conditions:
- Cardiothoracic surgery and trauma
- Paradoxicalair embolism
- Arteriography.
Hemodynamic Derangements Due To Obstructive Nature Short Question And Answers
Question 1. Atrial embolism
Answer:
Arterial emboli may lead to infarction, myocardial infarc¬tion, gangrene, and sudden death.
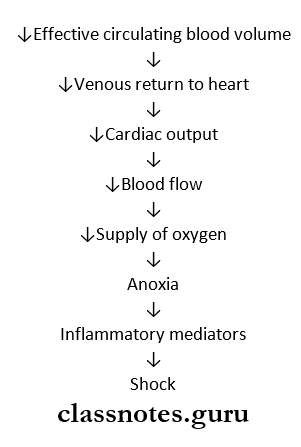
Question 2. Pulmonary embolism
Answer:
Definition: Pulmonary embolism is the most common and fatal form of venous thromboembolism in which there is occlusion of a pulmonary arterial tree by thrombotic emboli.
Pulmonary embolism Etiology:
Thrombi originating from large veins of lower legs are 95%, less commonly thrombi originate from varicosities superficial veins of legs, and pelvic veins.
Pulmonary embolism Pathogenesis:
Detachment of thrombi produces thrombo-embolus that flows through venous drainage into large veins draining into right side of the heart
Pulmonary embolism Consequences:
- Acute corpulmonale
- Pulmonary hypertension
- Pulmonary infarction
- Chroniccorpulmonale
- Pulmonary hemorrhage
- Sudden death.
Question 3. Thromboembolism
Answer:
A detached thrombus or part of a thrombus forms thromboembolism
Question 4. Causes of ischemia
Answer:
Ischemia is defined as a deficiency of blood supply to a part of a tissue.
Etiology: Various causes of ischemia are as follows.
1. Causes in the heart: Inadequate cardiac output may result from.
- Heart block
- Ventricular arrest
- Fibrillation.
This may lead to ischaemic injury to the brain.
2. Causes in the arteries: These are
- Luminal occlusion such as due to
- Causes in the arterial wall such as
- Vaso spasm
- Hypothermia
- Arteriole sclerosis
- Poly arteritis nodosa.
- Outside pressure on the artery such as ligature tour¬niquet torsion tight bandages.
3. Causes in the veins: Blockage of venous drainage may lead to engorgement and obstruction to arterial supply resulting in ischemia.
Examples:
- Luminal occlusion as in.
- Thrombosis of mesenteric veins
- Cavernous sinus thrombosis.
- Causes in vessel wall- varicose veins of legs.
- Outside pressure on the vein.
- Strangulated hernia
- Intussusceptions’.
- Causes in the microcirculation.
- Luminal occlusion.
- By red cells example In sickle cell anemia
- By white cells example In chronic myeloid leu¬kaemia
- By fibrin, for example, defibration syndrome o by fat embolism.
- Causes in microvasculature walls such as.
- Vasculitis example Arthus reaction and
- Frostbite injures wall of small blood ves¬sels.
- Outside pressure on microvasculature as in bed sores.