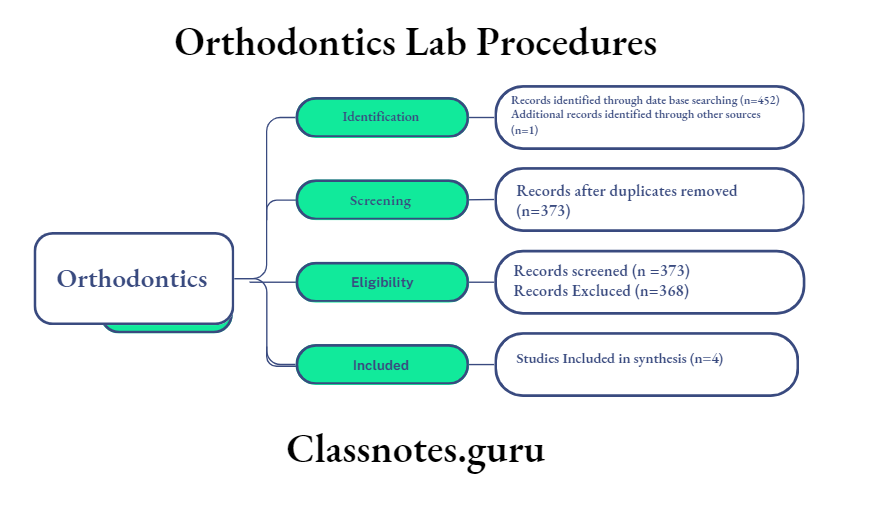
Cephalometrics Important Notes
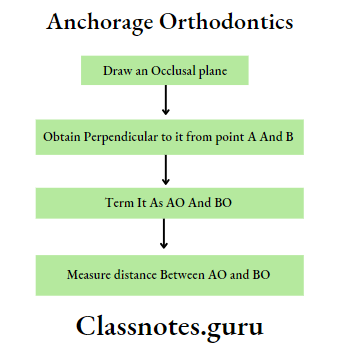
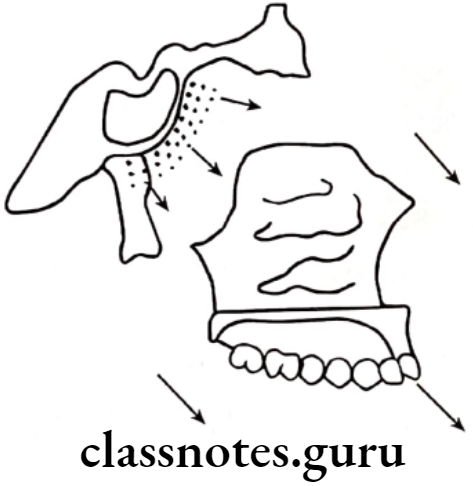
- Wit’s analysis
- It is a measure of the extent to which the maxilla and mandible are related to each other in antero-posterior direction
- It is used when the ANB angle is not reliable
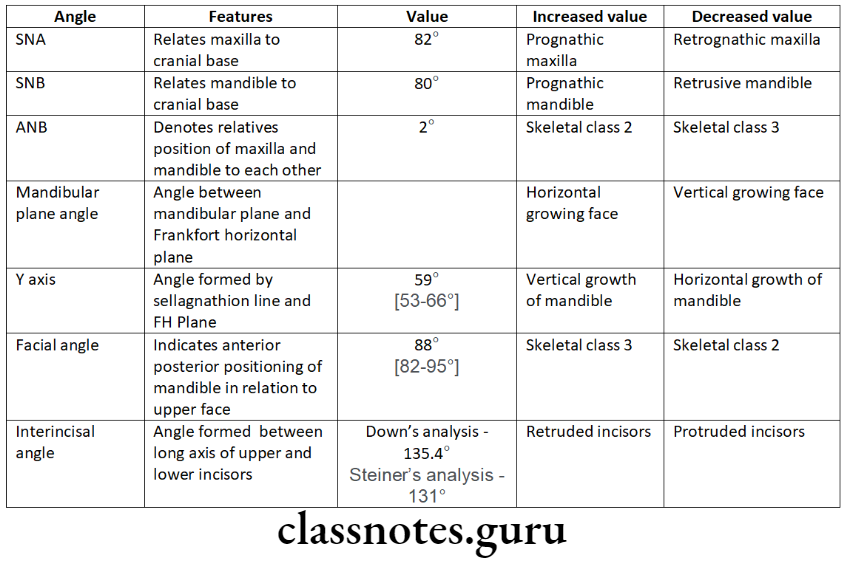
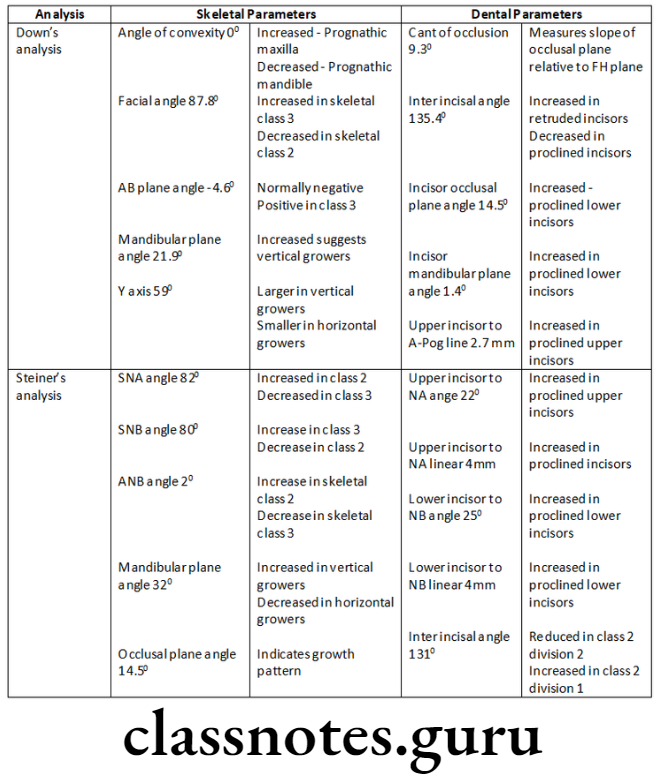
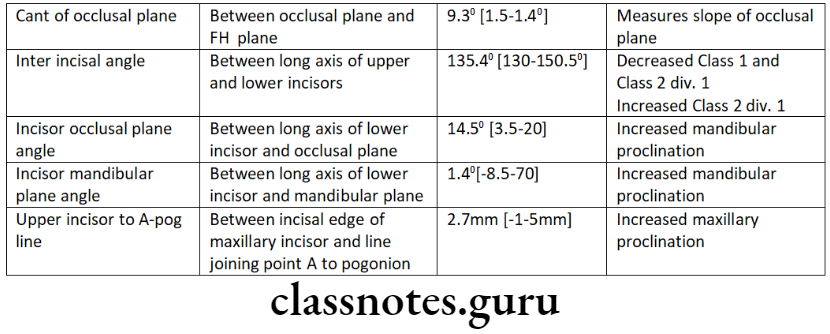
- Different analysis
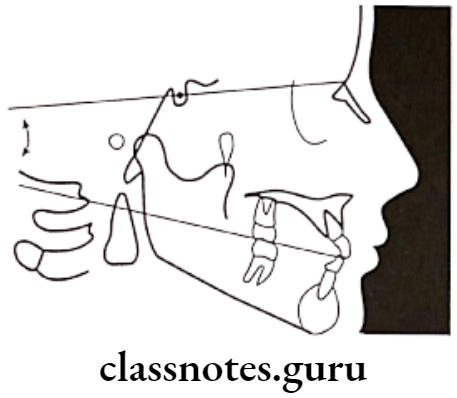
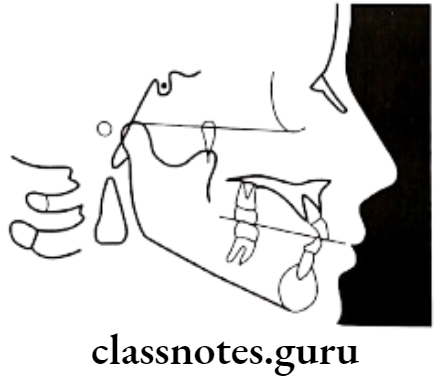
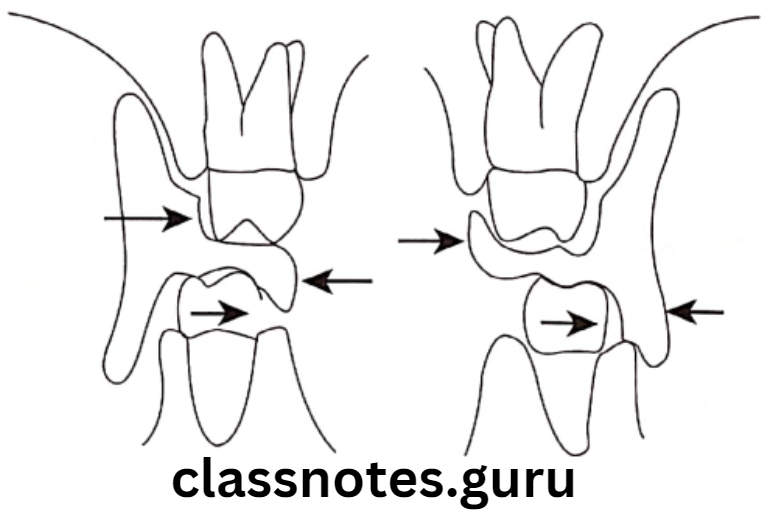
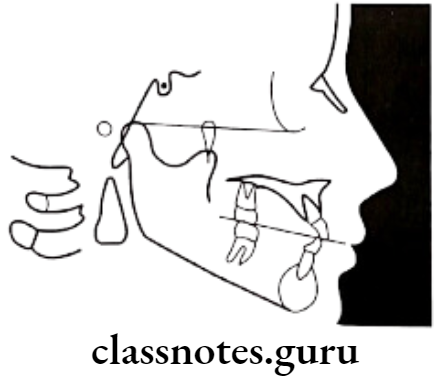
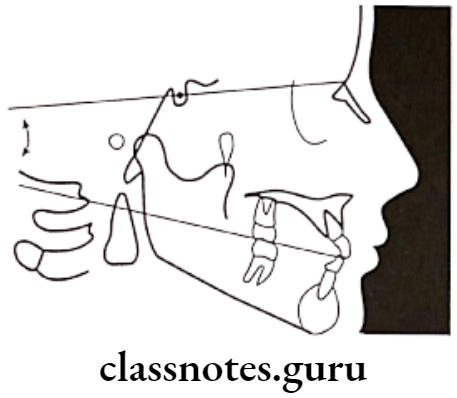
- Tweed’s analysis
- Forms a triangle by use of three planes
Read And Learn More: Orthodontics Short And Long Essay Question And Answers
Cephalometrics Long Essays
Question 1. What are diagnostic aids? Describe cephalometrics and its uses.
Answer.
Diagnostic Aids
Comprehensive orthodontic diagnosis is established by the use of clinical implements called diagnostic aids
Cephalometrics:
- Introduced by Broadbent in USA and Hofrath in Germany in 1931
- It describes the analysis and measurements made on the cephalometric radiographs
Types Of Cephalometrics:
- Lateral cephalogram: Provides a lateral view of the skull
- Frontal cephalogram: Provides an antero-posterior view of the skull
Technical Aspects:
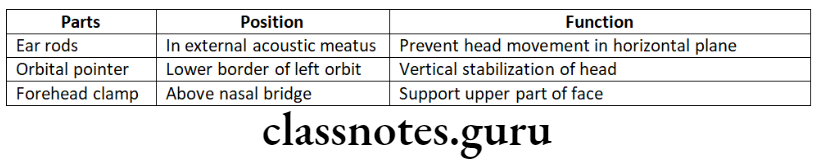
- Apparatus – X-ray source
- Cephalostat – two ear rods
- Orbital pointer
- Forehead clamp
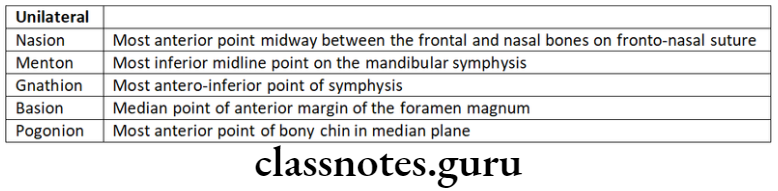
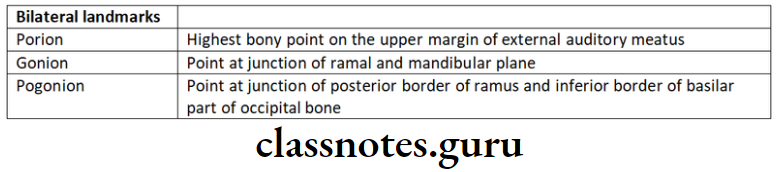
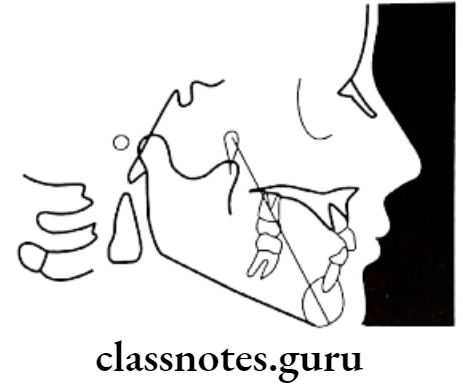
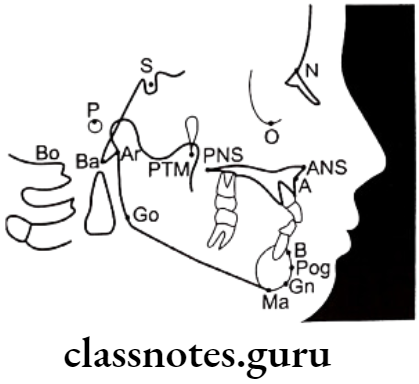
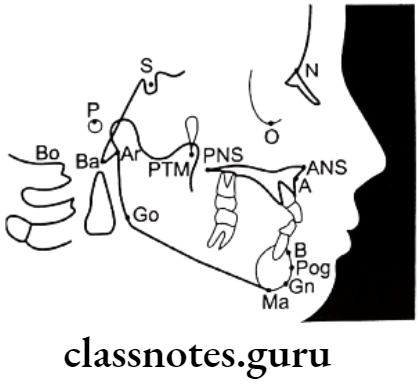
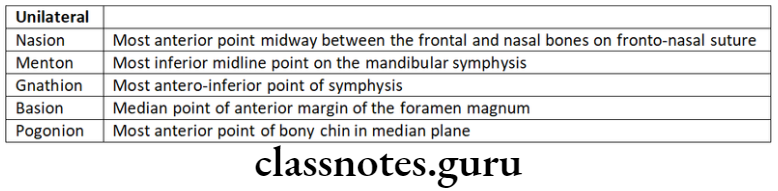
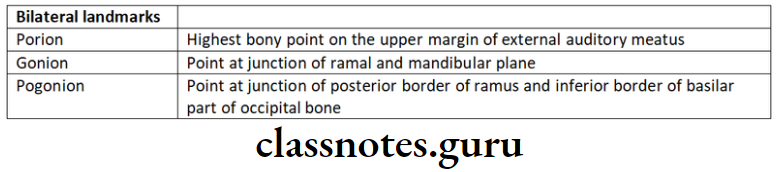
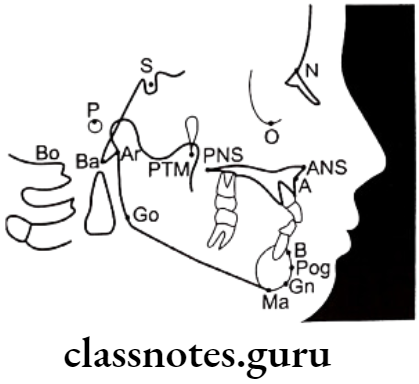
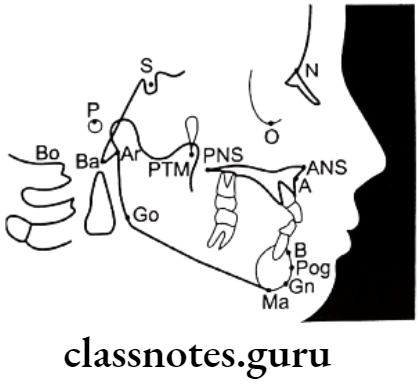
Landmarks:
- Used for quantitative analysis and measurements
Types Of Landmarks:
- Anatomic landmarks: Represent actual anatomic structures of the skull
- Derived landmarks: Obtained from anatomic structures
Requirements Of Land Marks:
- Easy to view
- Reproducible
- Provide valid measurements
Examples Of Landmarks:
- Nasion
- Orbitale
- Porion
- Sella
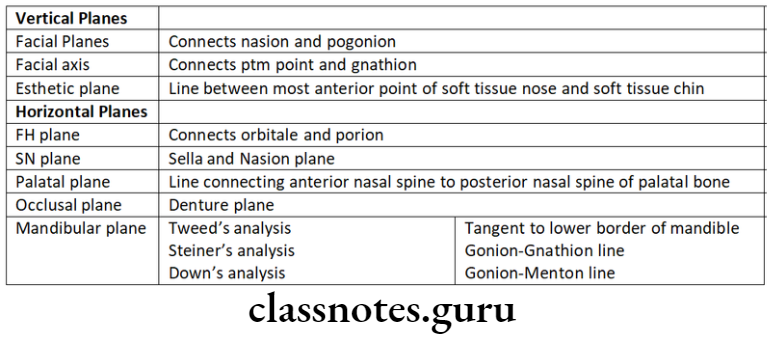
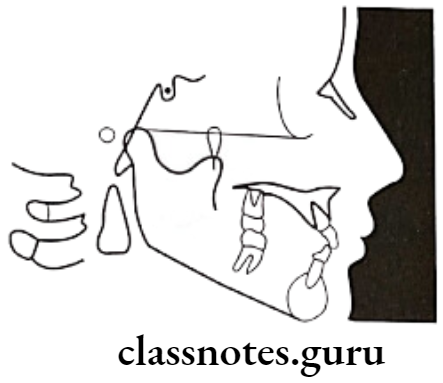
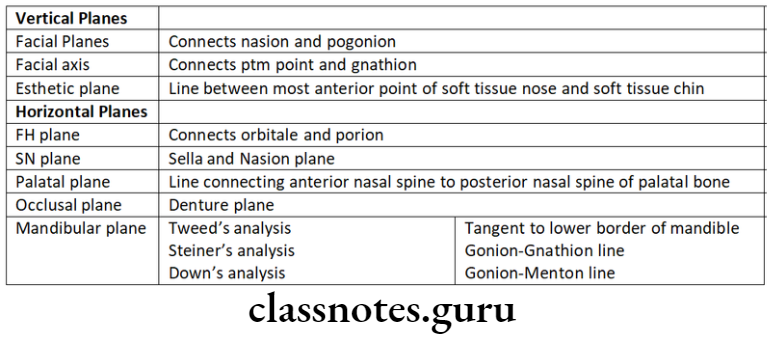
Lines And Planes:
- Obtained by connecting two landmarks
Types Of Lines And Planes:
- Horizontal Planes
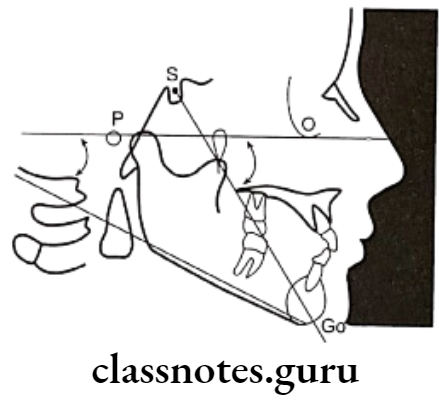
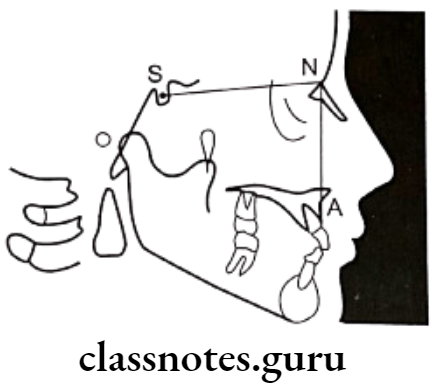
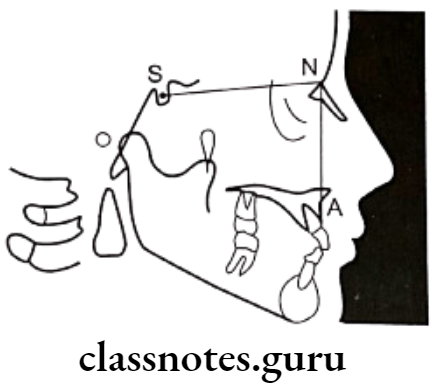
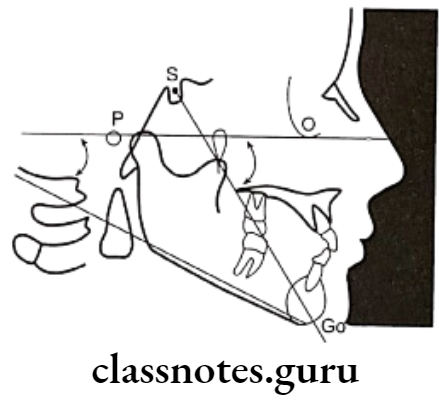
- Sella-Nasion Plane: Connecting sella and nasion
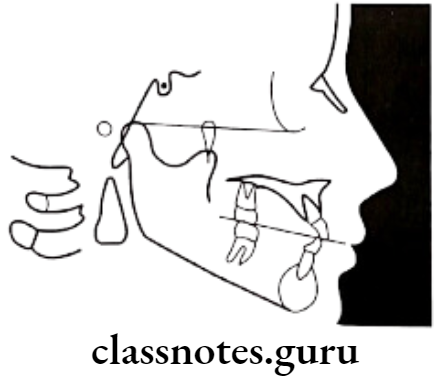
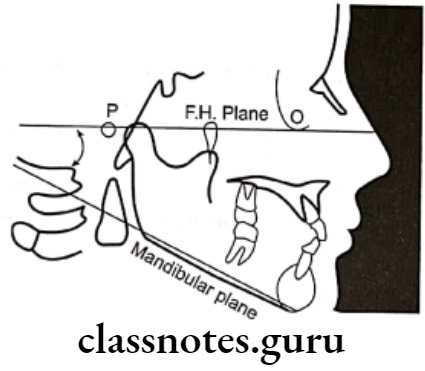
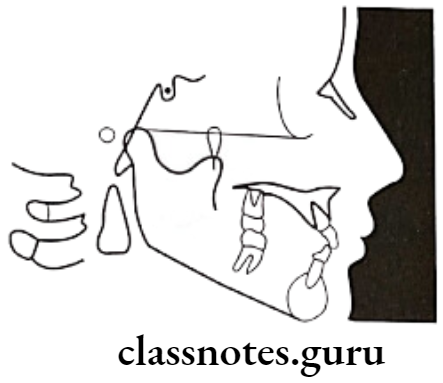
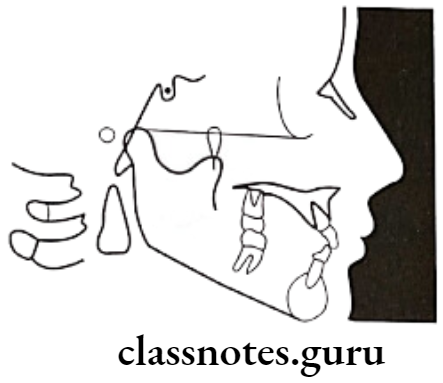
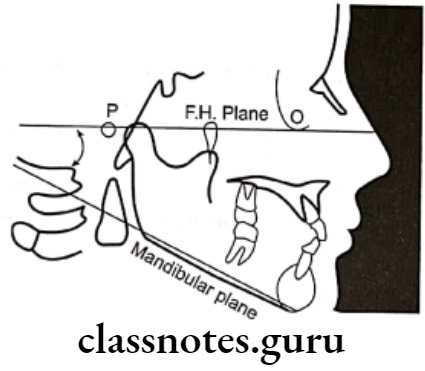
- Frankfort Horizontal Plane: Connecting orbitale and porion
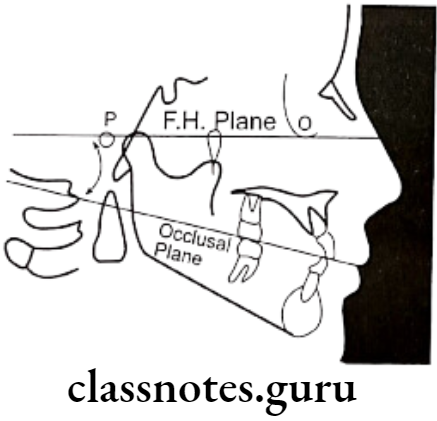
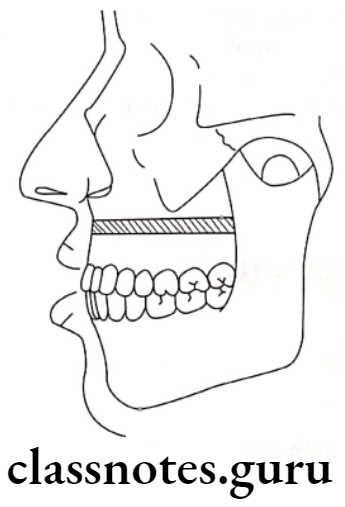
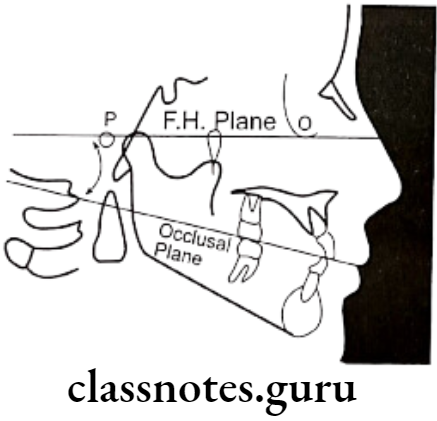
- Occlusal Plane: Connecting occlusal surfaces of posterior to anteriors
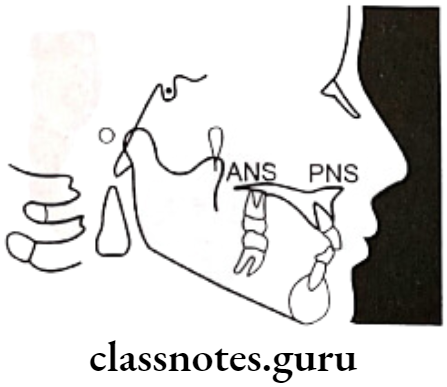
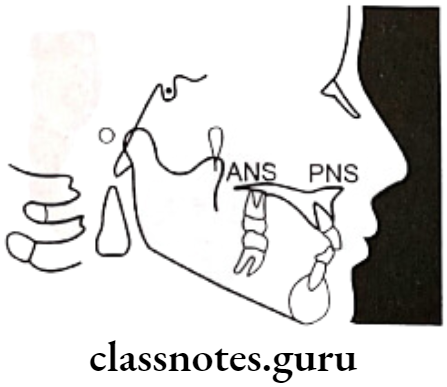
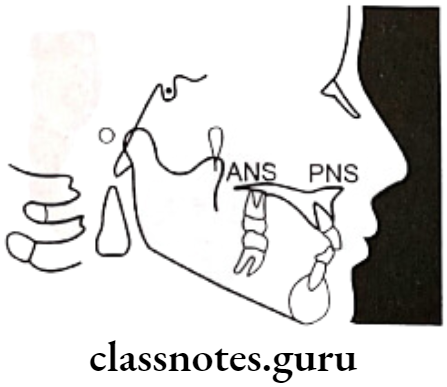
- Palatal Plane: Connecting ANS and PNS
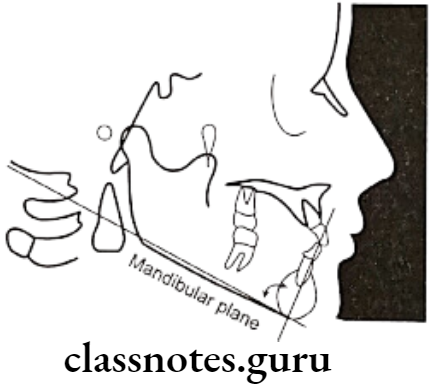
- Mandibular Plane:
- Tangent to lower border of mandible – Tweed
- The line connecting gonion & gnathion – Steiner
- The line connecting gonion & mention – Down’s
- Basion – Nasion Plane: Connecting Basion and Nasion
- Bolton’s Plane: Connecting Bolton’s Point and Nation
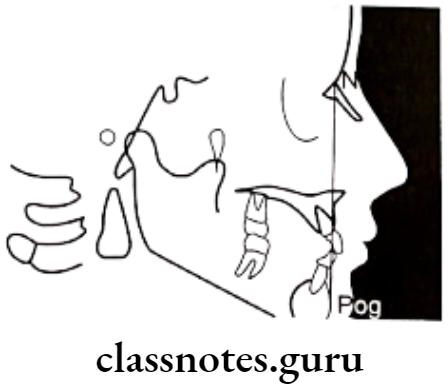
Vertical Plane
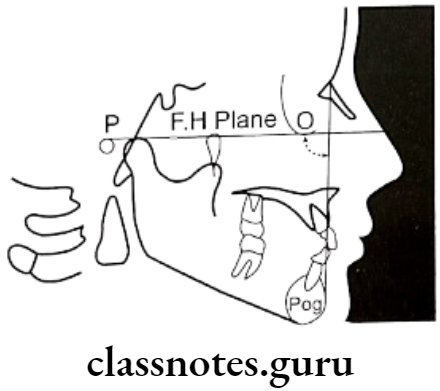
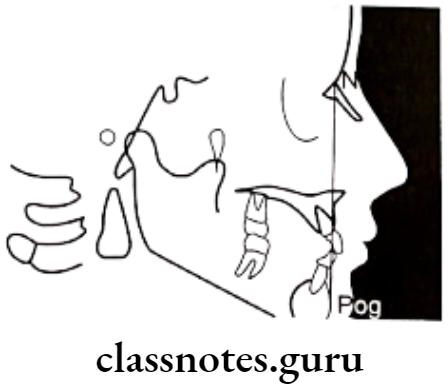
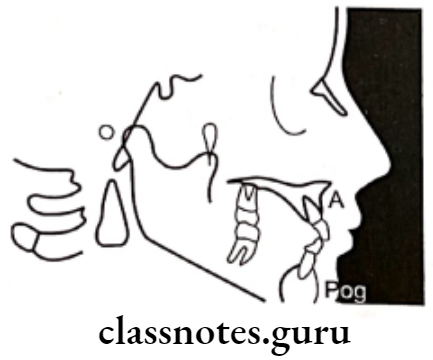
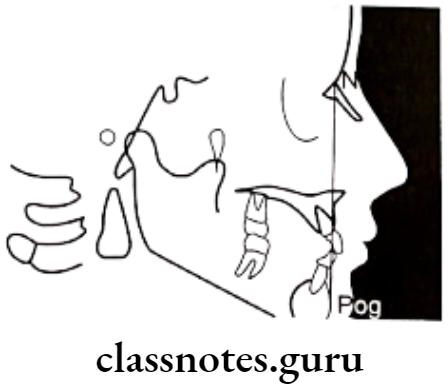
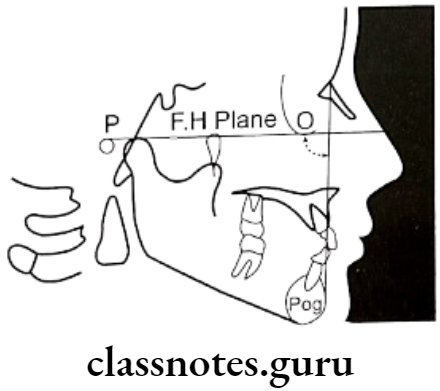
- A.Pog line: Point A to Pogonion
- Facial Plane: Nasion to pogonion
- Facial axis: Ptm point to gnathion
- E.Plane: Soft tissue nose to the soft tissue of the chin
Cephalometrics Uses:
- For diagnosis
- Study of dental and soft tissue structures
- Classify skeletal and dental abnormalities
- Assess facial type
- For treatment planning
- For presuming the changes
- For predicting growth-related changes
- For research work
Cephalometrics Short Essays
Question 1. Cephalogram.
Answer.
Cephalogram
- Cephalogram is a cephalometric radiography introduced by Holly Broadbent and Herbert Hofrath in 1931
Types Of Cephalogram:
- Lateral cephalogram
- This provides a lateral view of the skull
- Frontal cephalogram
- Provides an antero-posterior view of skull
Cephalogram Uses:
- For diagnosis
- Study of dental and soft tissue structures
- Classify skeletal and dental abnormalities
- Assess facial type
- For treatment planning
- For presuming the changes
- For predicting growth-related changes
- For research work
Cephalogram Limitations:
- Exposure to a patient is harmful
- Provides two three-dimensional views of three-dimensional structures
- Not well standardized
- Absence of anatomic references
- Has limited relevance
Question 2. Uses of Cephalometrics
Answer.
Uses of Cephalometrics
- For diagnosis
- Study of dental and soft tissue structures
- Classify skeletal and dental abnormalities
- Assess facial type
- For treatment planning
- For presuming the changes
- For predicting growth-related changes
- For research work
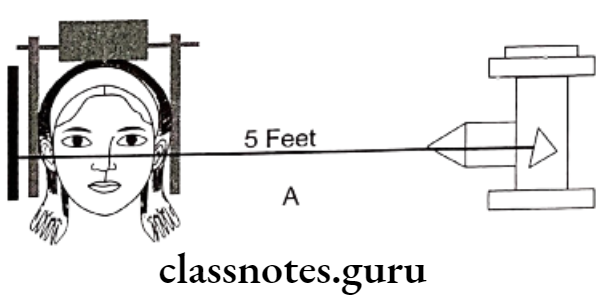
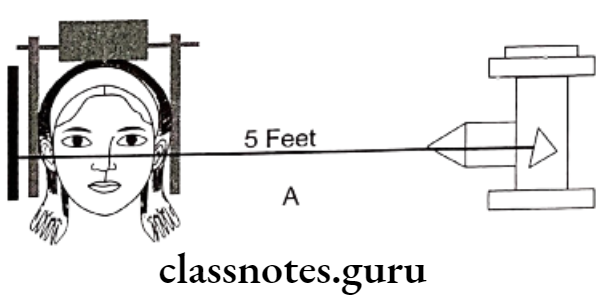
Question 3. Cephalostat.
Answer.
Cephalostat
- It is head holding device
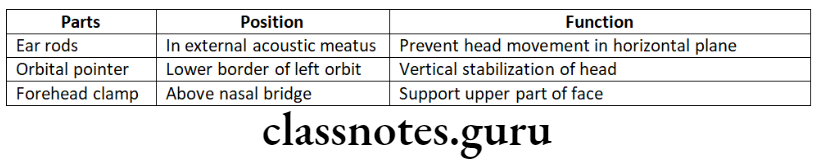
- Position: The distance between the X-ray source and the mid-sagittal plane of the patient is 5 feet
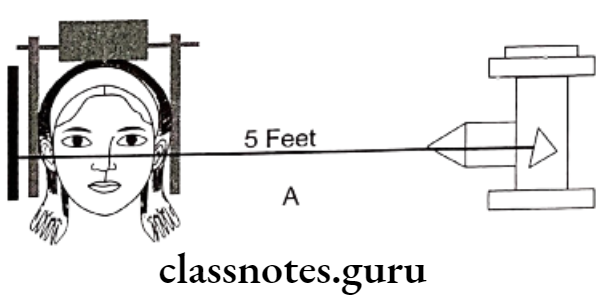
Uses Of Cephalostat:
- For standardizing radiography
- Comparing serial radiographs
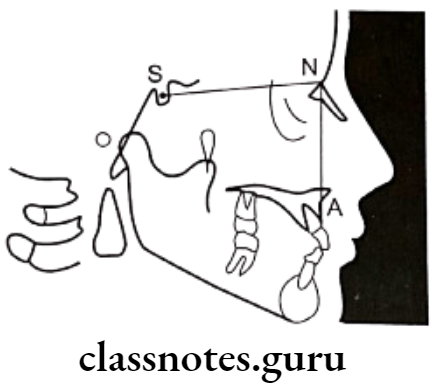
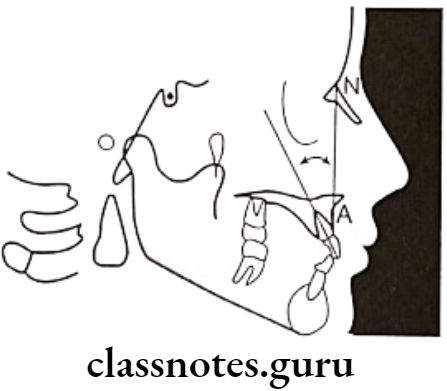
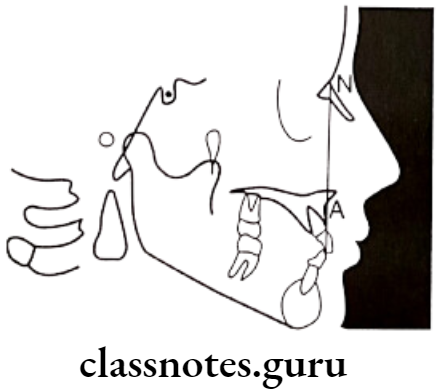
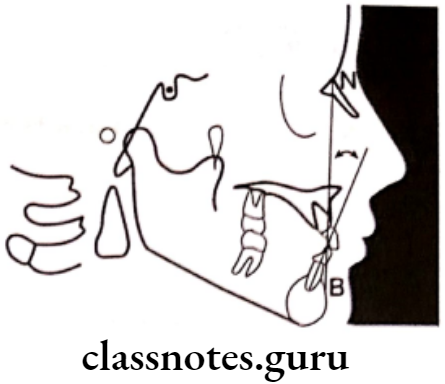
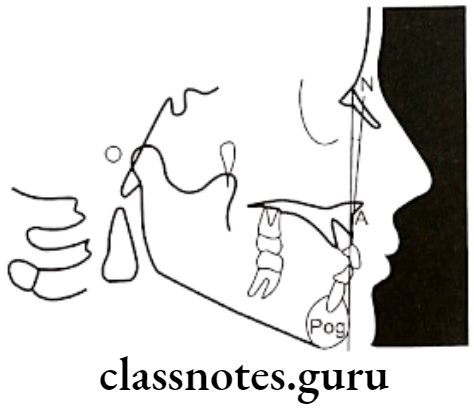
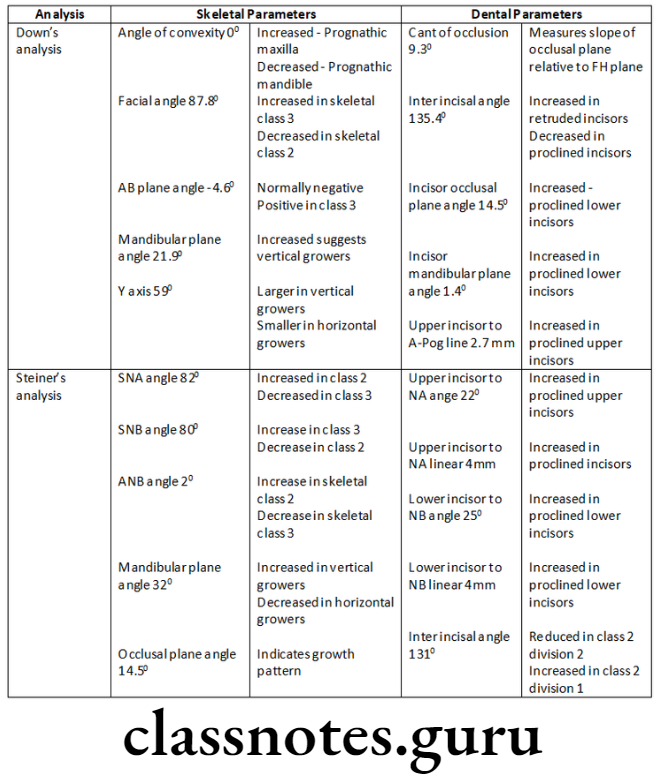
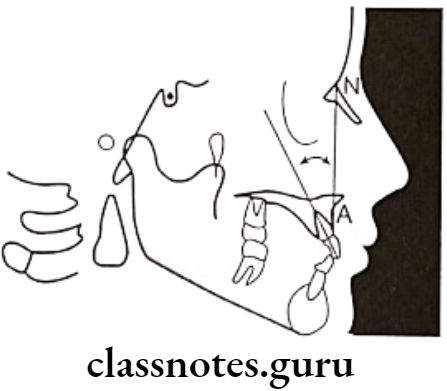
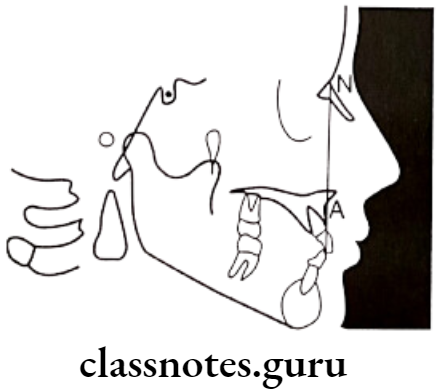
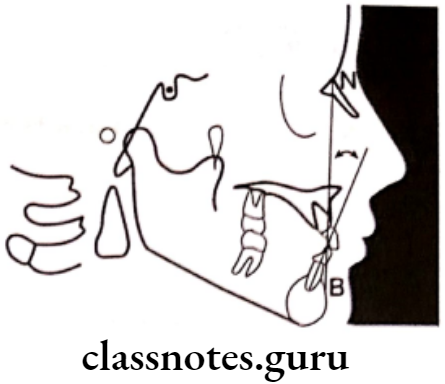
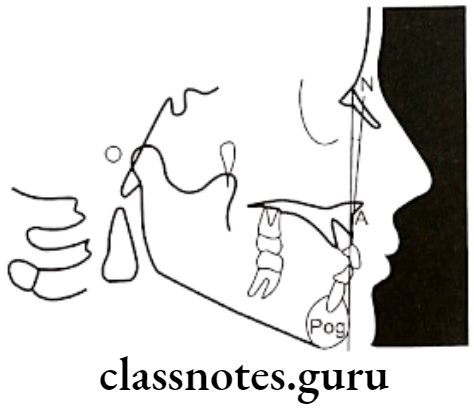
Question 4. Steiner Analysis.
Answer.
Parameter:
Skeletal
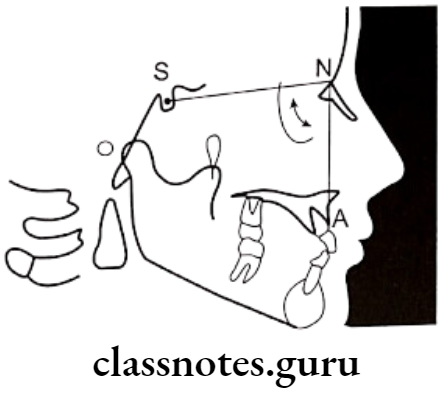
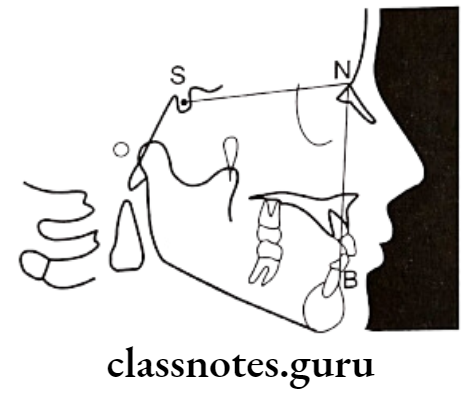
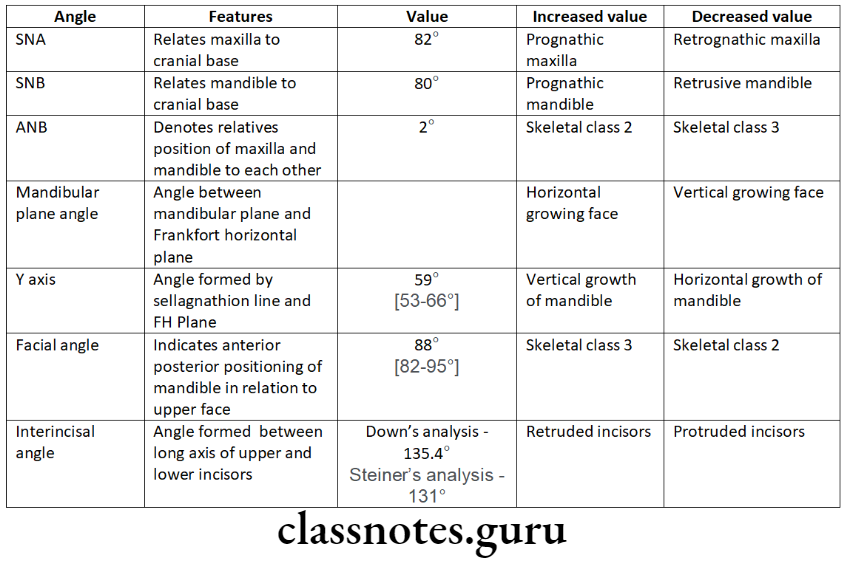
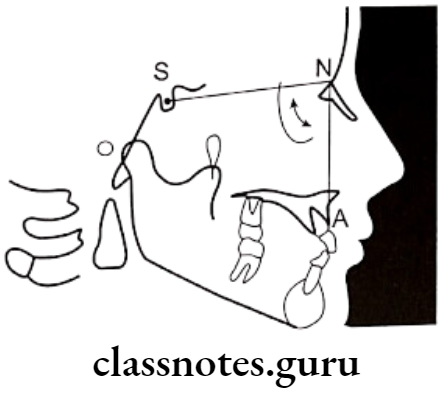
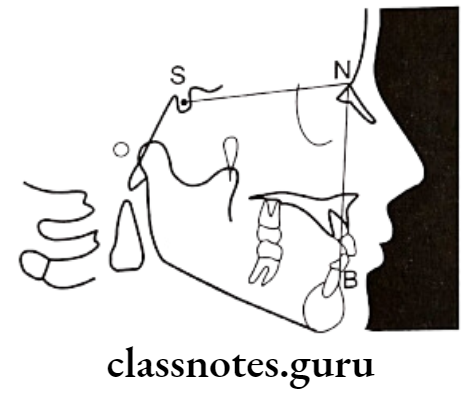
- SNA angle:
- SN plane and line joining nasion and point A – 82°
- Increased – Class 2; Decreased – Class 3
- SNB angle:
- Between SN plane and the line joining nasion and point B – 80°
- Increased – Class 3; Decreased – Class 2
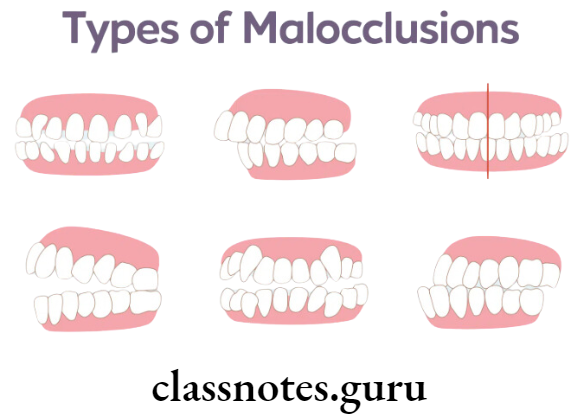
- ANB angle:
- Between the line joining Maison and point A and Nation and point B – 2°
- Increased – Skeletal Class 2; Decreased – Skeletal Class 3
- Mandibular Plane angle:
- Between SN plane and mandibular plane – 32°
- Low angle – Horizontal grower; High angle – vertical grower
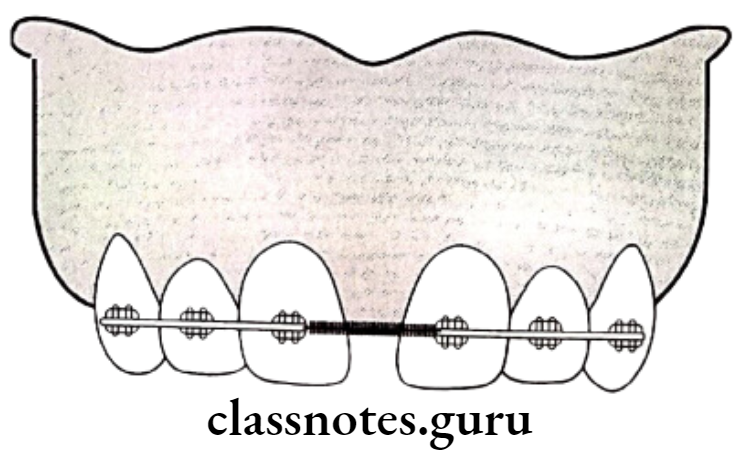
- Occlusal plane angle:
- Between occlusal plane and SN plane – 14.5°
- Indicates growth pattern of individual
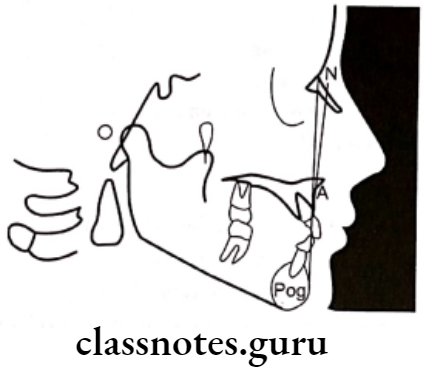
Dental:
- Upper Incisor to N-A:
- Between the long axis of the upper incisor and nasion to point A – 22°
- Increased – proclination of upper incisors
- Upper Incisor to N-A:
- Linear measurement between labial surface of upper incisor and line joining nasion to point A – 4mm
- Lower Incisor to N-B:
- Between long axis of lower incisor and nasion to point B – 25°
- Increased – Proclined lower incisor
- Lower Incisor to N-B:
- The linear distance between the labial surface of the lower central incisor and the line joining nasion to point B – 4mm
- 131°
- Inter-incisor angle:
- Between the long axis of the upper and lower central incisor
- Increased – Class 2 div 2, Decreased – Class 2 div 1, Class 1
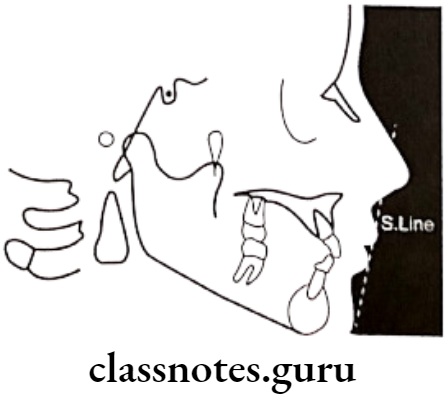
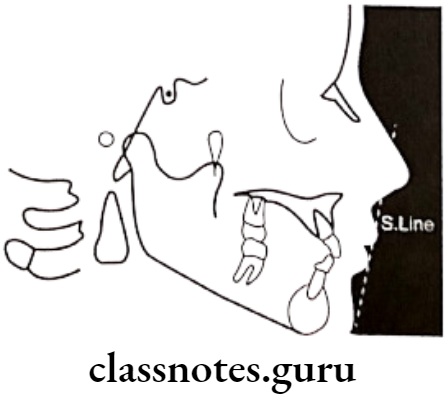
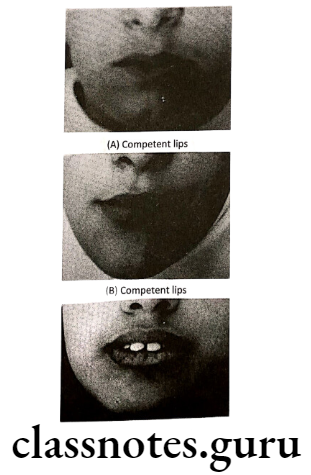
Soft Tissue analysis
According to Steiner the lips in a well-balanced face should touch a line extending from the soft tissue of the chin to the middle of the ‘S’ formed by the lower border of the nose
- Protrusive – Lips beyond this line – Convex profile
- Retrusive – Lips behind this line – Concave profile
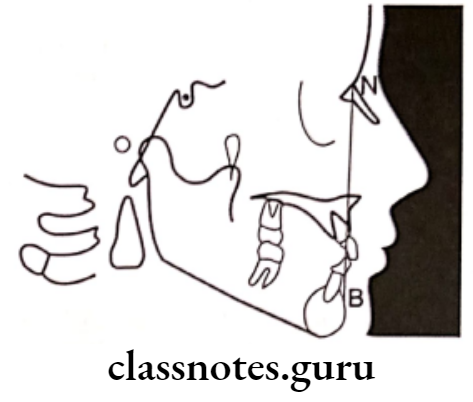
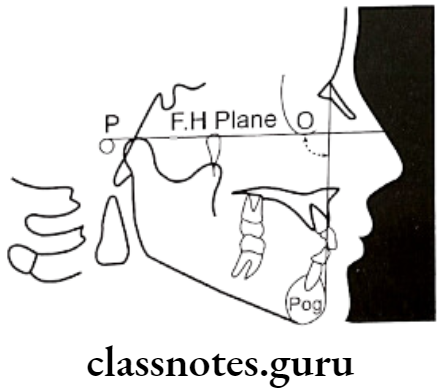
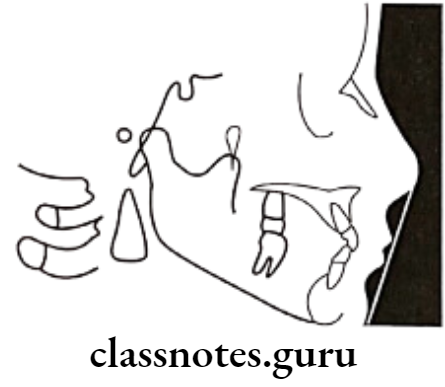
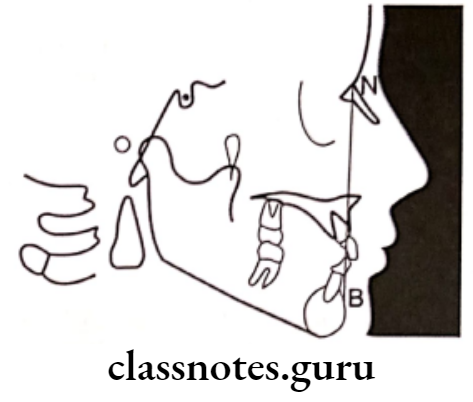
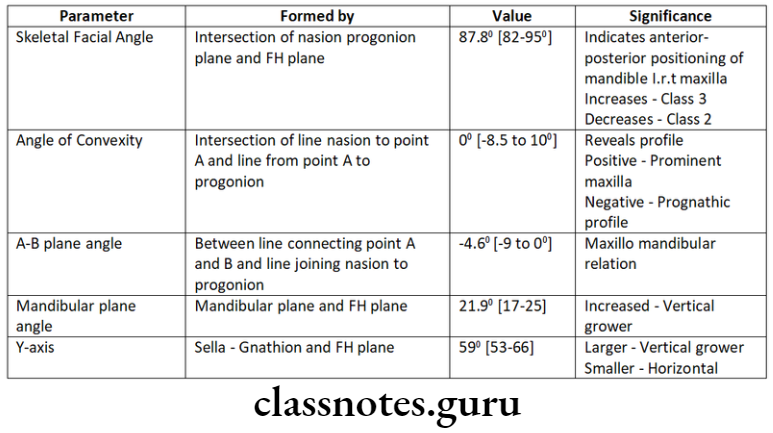
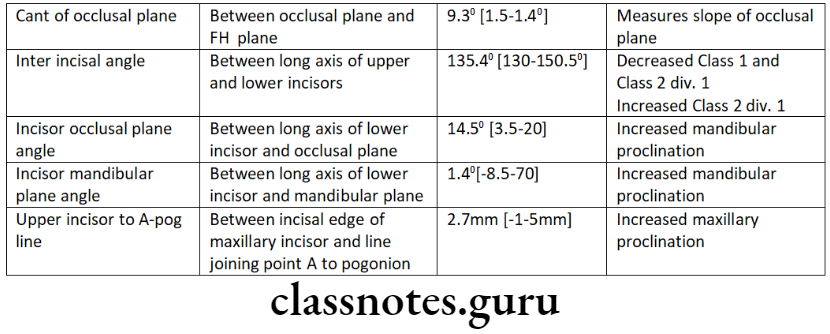
Question 5. Down’s Analysis.
Answer.
Down’s Analysis
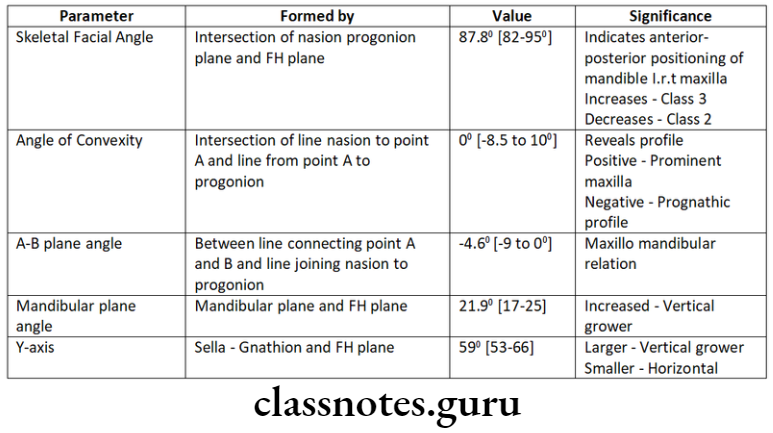
Dental
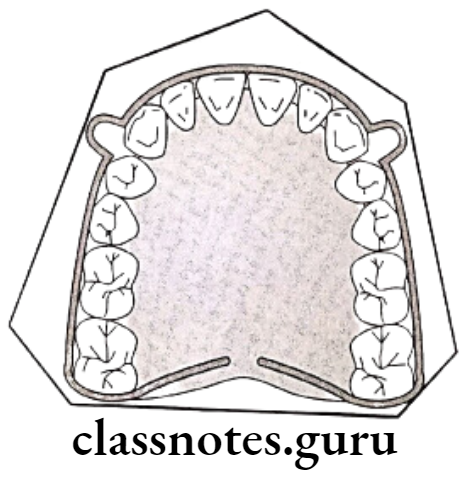
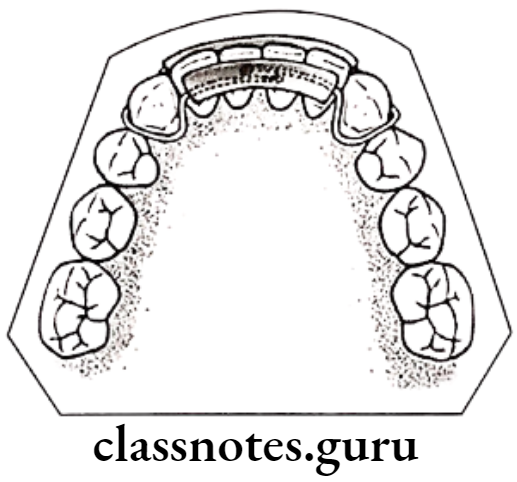
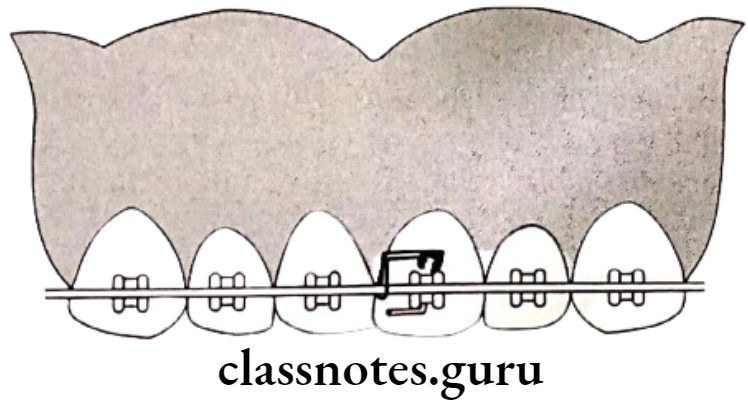
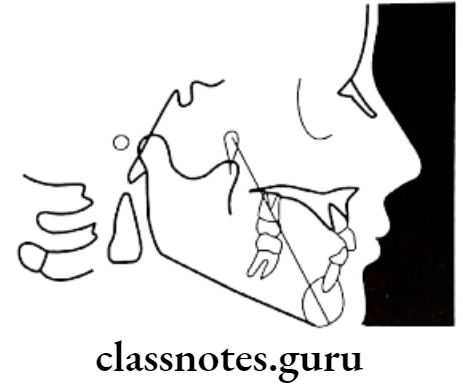
Question 6. Visual treatment objective (VTO).
Answer.
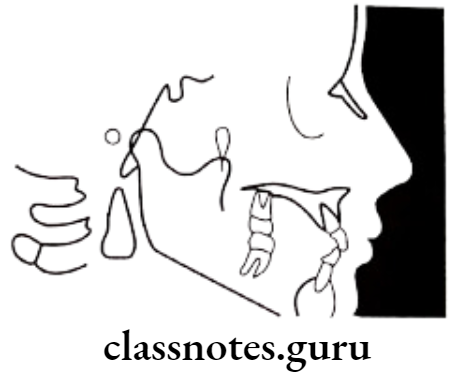
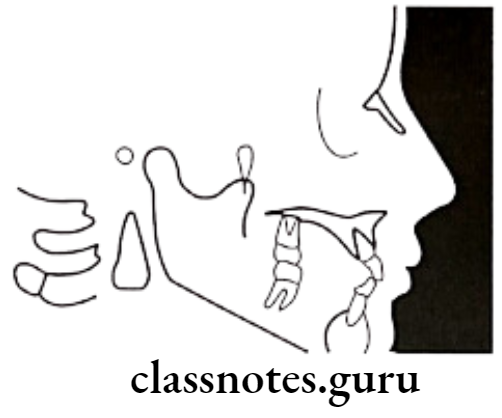
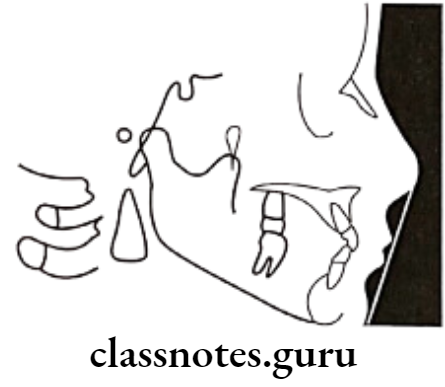
Types Of Visual Treatment Objectives
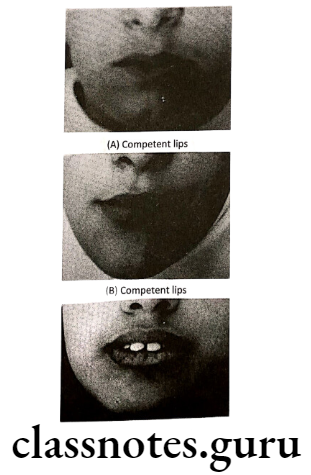
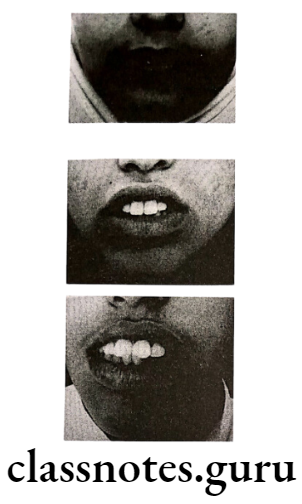
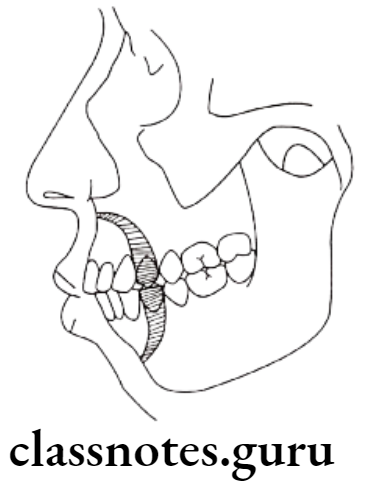
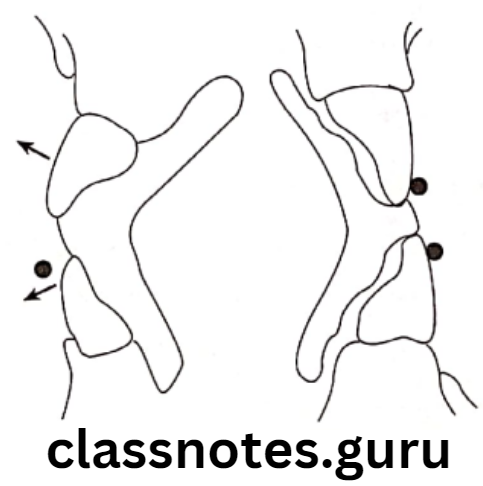
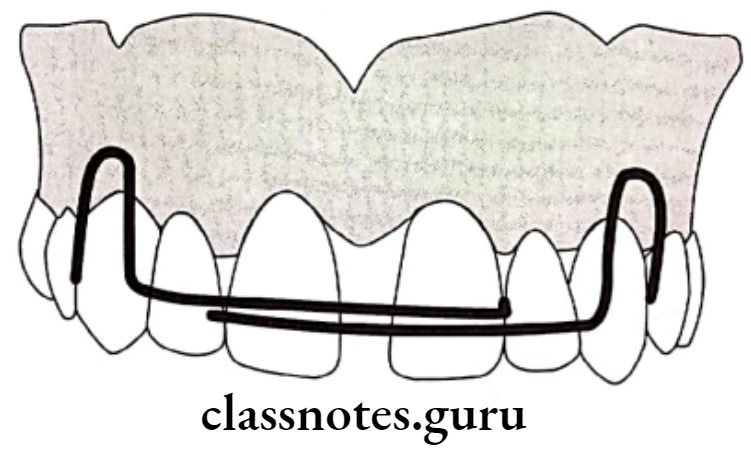
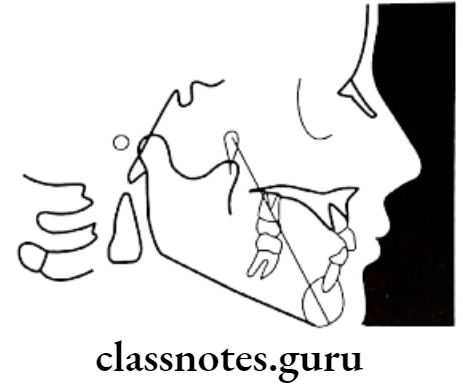
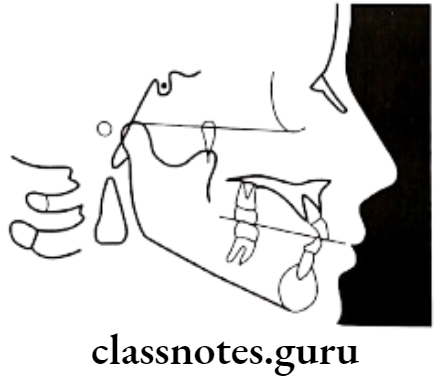
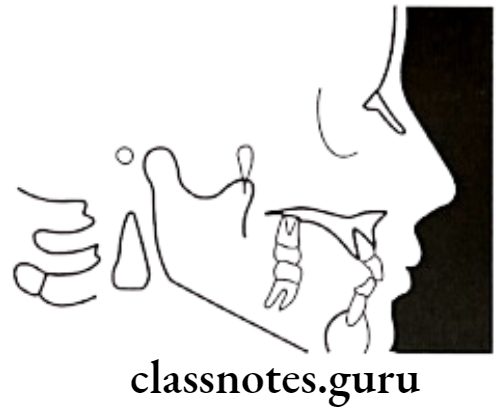
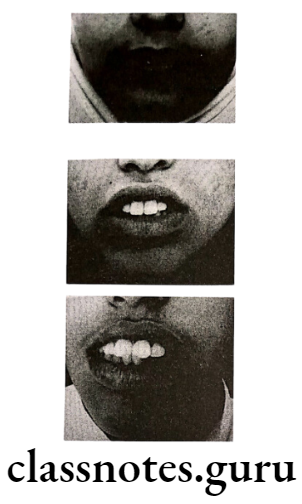
Clinical VTO:
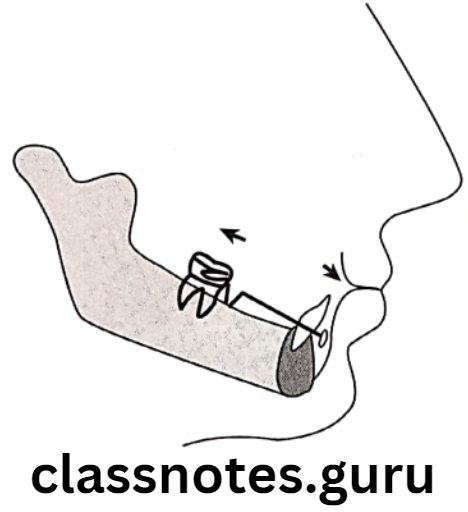
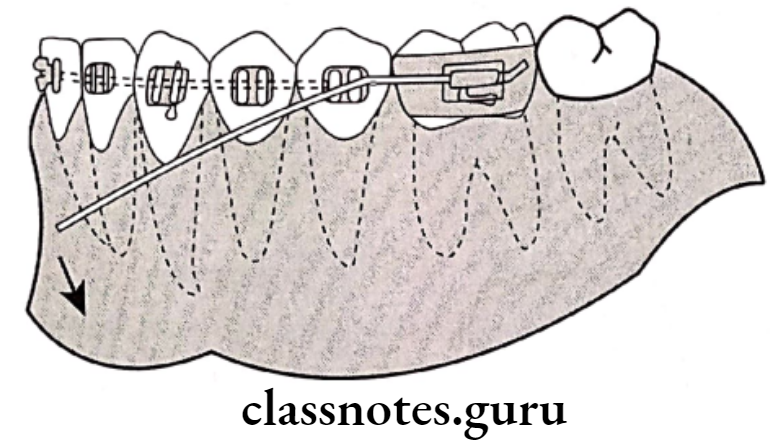
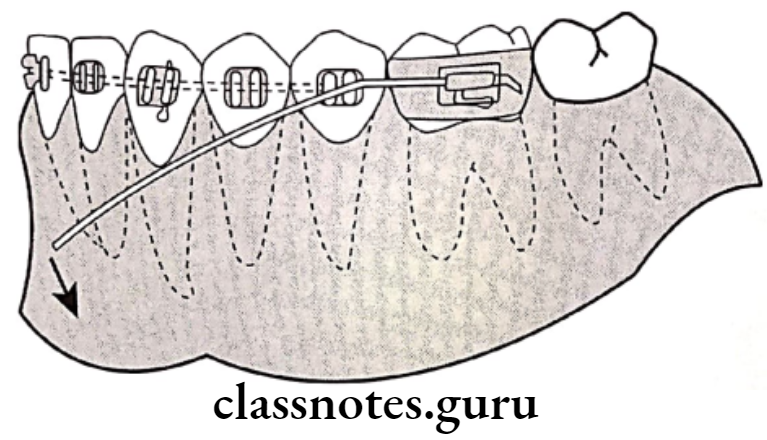
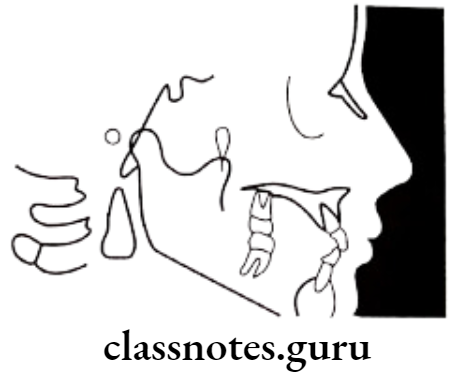
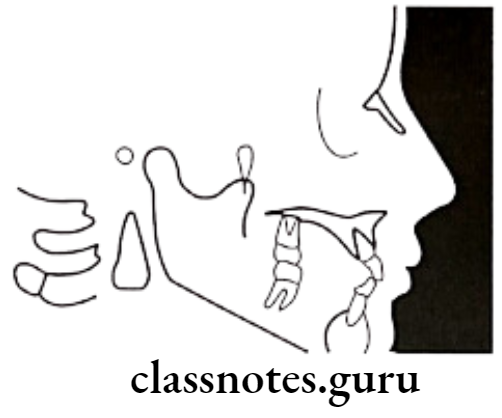
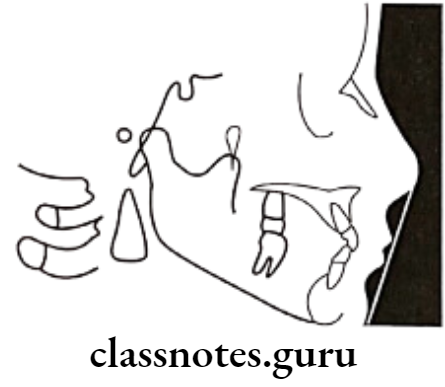
- It is an aid to decide the type of appliance in skeletal class 2 malocclusion
- The procedure consists of asking the patient to bring the mandible to an edge-to-edge bite relation and note the changes in appearance of the patient at two levels
- Edge-to-edge relation
- Midway between existing occlusion and edge-to-edge position
- Interpretation:
- If the profile worsens at the edge-to-edge position, the fault lies in the maxilla
- If the profile improves at the edge-to-edge position, the fault lies in the mandible
- If the profile improves at the midway position, there is a fault in both the maxilla and mandible
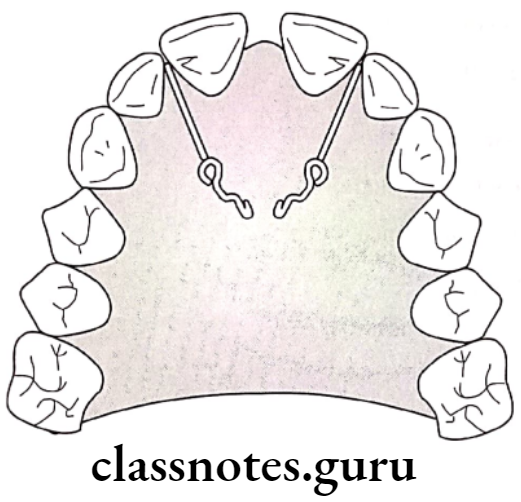
Cephalometric VTO:
- It is like a visual plan to predict the normal growth of a patient and anticipate the effects of the treatment for an individual patient
- It permits the development of alternative treatment plans and to set goals in advance for the treatment
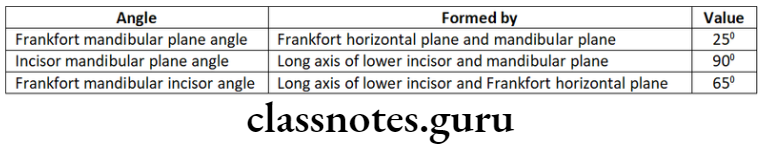
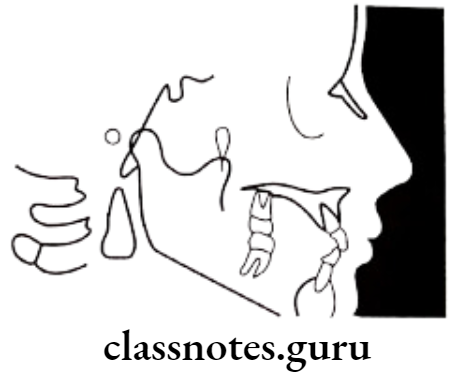
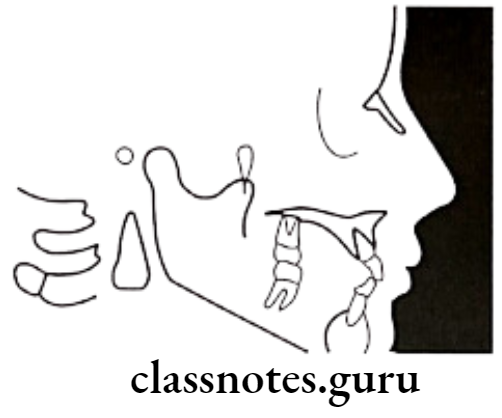
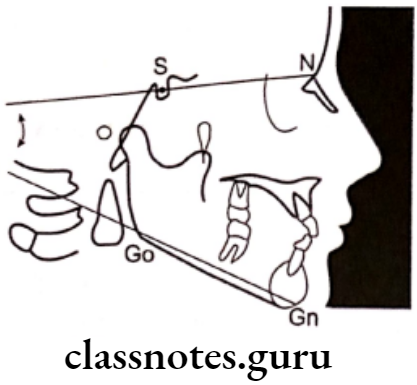
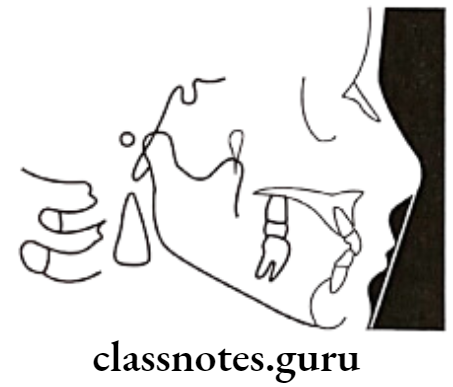
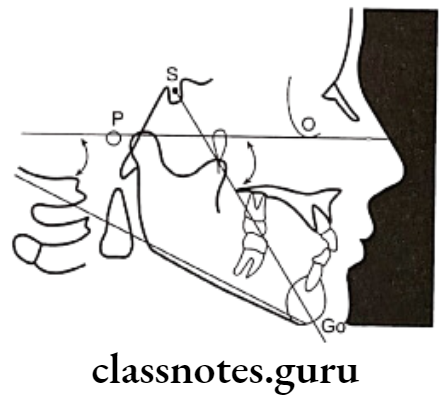
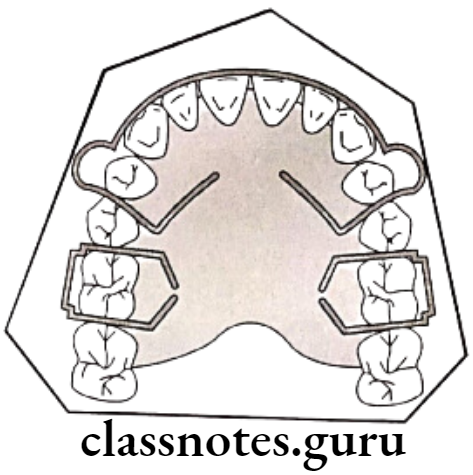
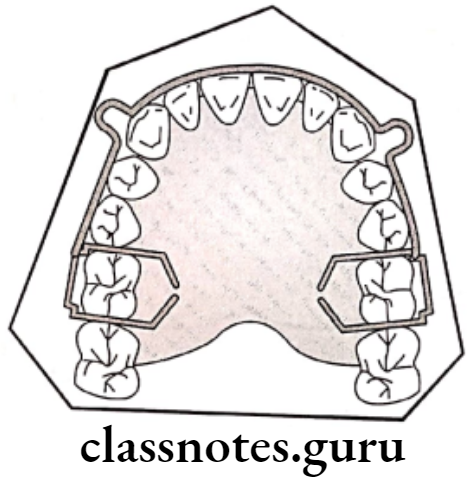
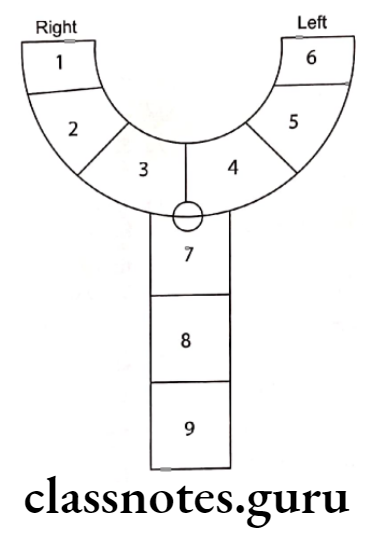
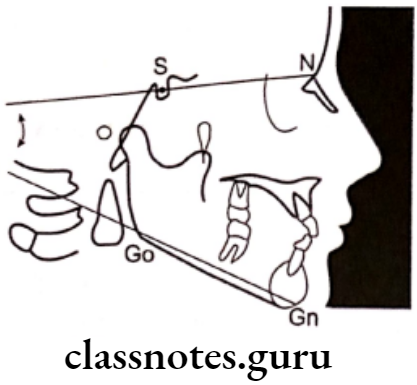
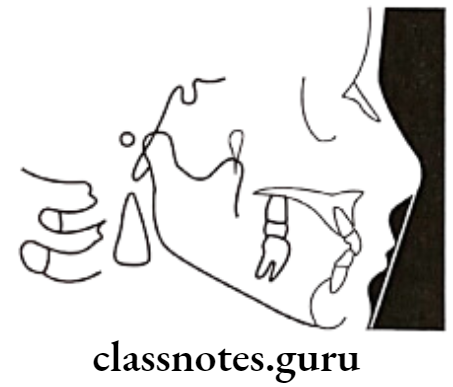
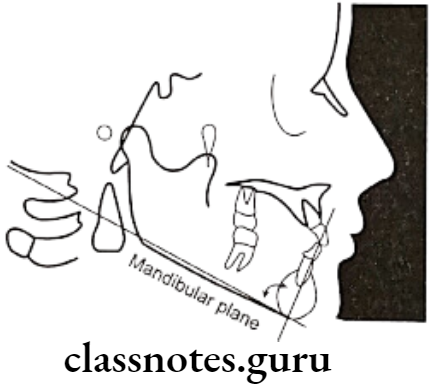
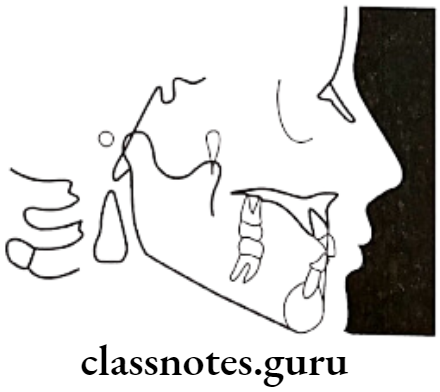
Question 7. Tweed’s triangle.
Answer.
Tweed’s triangle
Question 8. Cephalometrics uses, advantages, and disadvantages.
Answer.
Uses Of Cephalometrics:
- For diagnosis
- Study of dental and soft tissue structures
- Classify skeletal and dental abnormalities
- Assess facial type
- For treatment planning
- For presuming the changes
- For predicting growth-related changes
- For research work
Advantages Of Cephalometrics:
- Tangible records that are relatively permanent
- Nondestructive and noninvasive
- Easy to store, transport, and reproduce
- Yield accurate information on the spatial relationship between surface and deep structures
- Low physiological cost
Disadvantages Of Cephalometrics:
- It gives a two-dimensional view of a three-dimensional object
- There can be errors while developing which can limit measuring accuracy to 0.5mm
- Needs a special X-ray apparatus with precise calibration
- Needs complex patient positioning arrays to avoid errors
Cephalometrics Short Questions And Answers
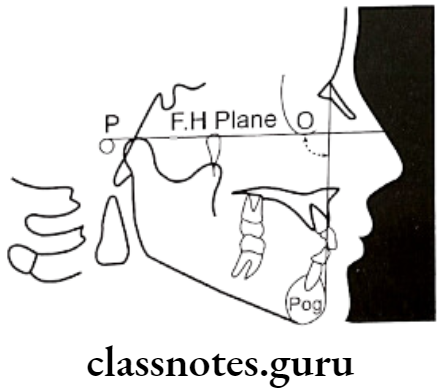
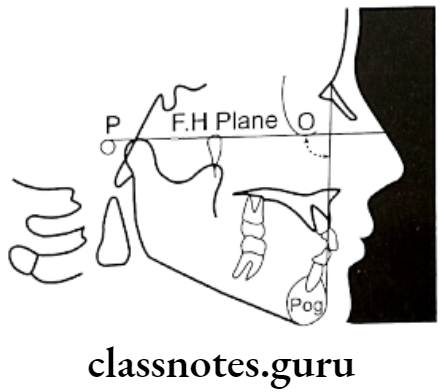
Question 1. Frankfort plane.
Answer.
Frankfort plane
Connects lowest point of orbit and superior border of external auditory meatus i.e. orbitale to portion
Significance Of Frankfort plane: Important in Down’s analysis
- Used in both dental and skeletal parameters
Question 2. Cephalostat.
Answer.
Cephalostat
It is head holding device
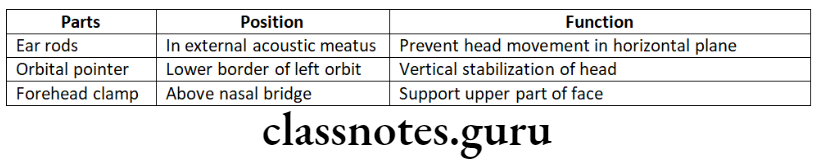
Position: The distance between the X-ray source the and mid-sagittal plane of the patient is 5 feet
Question 3. SNB angle.
Answer.
SNB angle
Used in Steiner’s Analysis
Angle: Between SN plane and the line joining nasion and point B
Importance: Indicates relative antero-posterior positioning of the mandible about the cranial base
Value: 80°
Changes:
- Increased – Prognathic mandible [Class 3]
- Decreased – Retrognathic mandible [Class 2]
Question 4. Registration Point.
Answer.
Registration Point
- It is derived from landmarks obtained on cephalogram
- It is the midpoint of the perpendicular drawn from the center of Sella Tursica to the Bolton plane
Question 5. Mandibular Plane.
Answer.
Mandibular Plane
Based on different analysis. There are several mandibular planes
Common are:
- Tangent to lower border of mandible – Tweed
- Line connecting gonion and gnathion – Steiner
- The line connecting Gonion and mention – Down’s
Question 6. SNA angle.
Answer.
SNA angle
Used in Steiner’s Analysis
Angle: Between SN plane and the line joining nasion and point A
Importance: Indicates relative antero-posterior positioning of the maxilla about the cranial base
Value: 82°
Changes:
- Increased – Prognathic maxilla [Class 2]
- Decreased – Retrognathic maxilla [Class 3]
Question 7. Occlusal Plane.
Answer.
Occlusal Plane
It is a denture plane
Extend: Occlusion of posterior to interiors
Significance Of Occlusal Plane:
- The angle formed between the occlusal plane and the SN plane is known as the occlusal plane angle
- It indicates the relation of the occlusal plane to the cranium and face
- It has a mean value of 14.5 degrees
Question 8. Cant of Occlusion.
Answer.
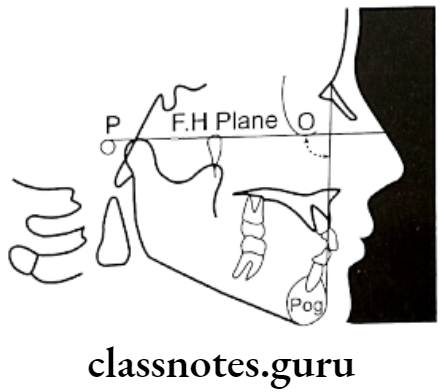
Cant of Occlusion
- Used in Down’s analysis
- The angle between the occlusal plane and the FH plane
- Value: 9.3°
- Range: 1.5 – 14°
- It measures the slope of the occlusal plane relative to the FH plane
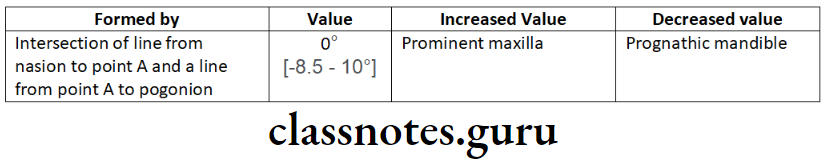
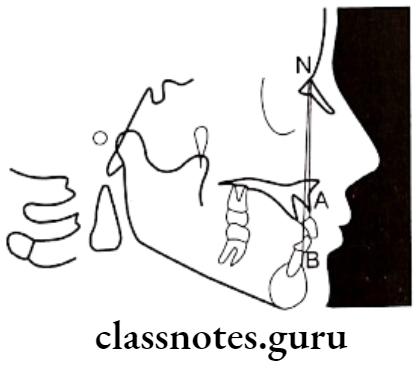
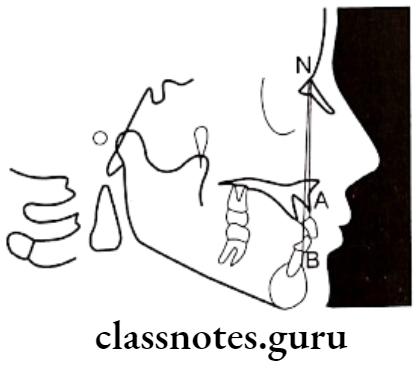
Question 9. ANB angle.
Answer.
ANB angle
Used in Steiner’s analysis
Angle: Between line joining nasion to point A and nasion to point B
Significance Of ANB angle: Relative position of maxilla to the mandible
Value: 2°
Changes:
- Increase – Skeletal Class 2
- Decrease – Skeletal Class 3
Question 10. Point A.
Answer.
Point A
It is an anatomic landmark of cephalometric
- The deepest point in the midline between the anterior nasal spine and alveolar crest between two central incisors
- Synonym: Subspinale
- Line/Plane derived from it:
- A.Pog line
- A.B plane angle – Used in Down’s Analysis
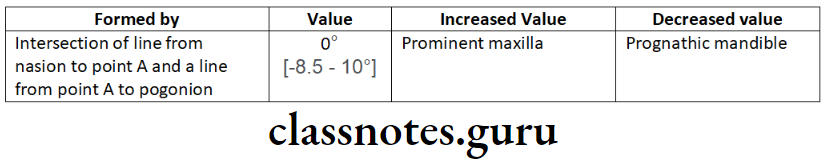
- The angle of convexity – Used in Down’s Analysis
- SNA angle – Used in Steiner’s Analysis
- ANB angle – Used in Steiner’s Analysis
Question 11. Key Ridge.
Answer.
Key Ridge
- It is an anatomic landmark of cephalometric
- It is the lowermost important point on the contour of the anterior wall of the infratemporal fossa
- In edentulous cases, it is useful in determining occlusion
Question 12. Y axis.
Answer.
Y-axis
Used in Down’s analysis
Synonym: Growth axis
Angle – Between sella – gnathion line and FH plane
Value: 59° [53-66°]
Variations Of the Y axis:
- Increased – Class 2
- Decreased – Class 3
Importance Of Y axis:
- Determines growth pattern
- Greater – Vertical growth
- Lesser – Horizontal growth
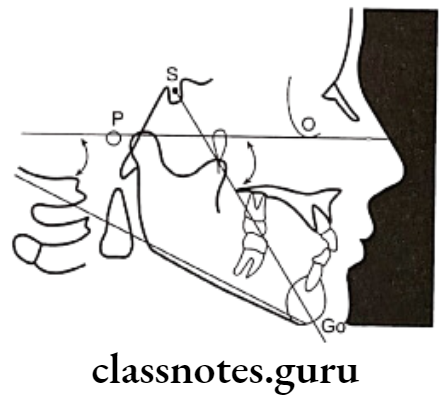
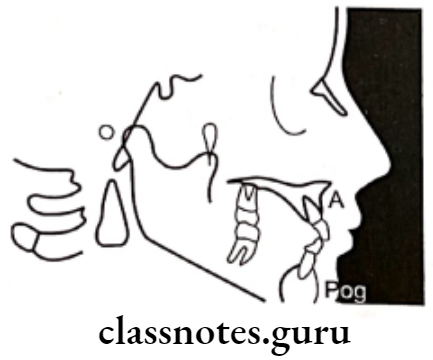
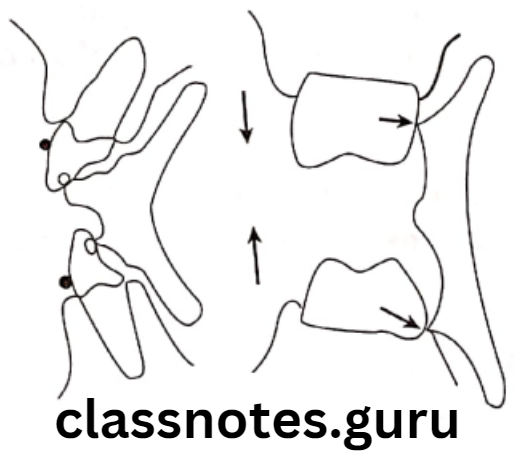
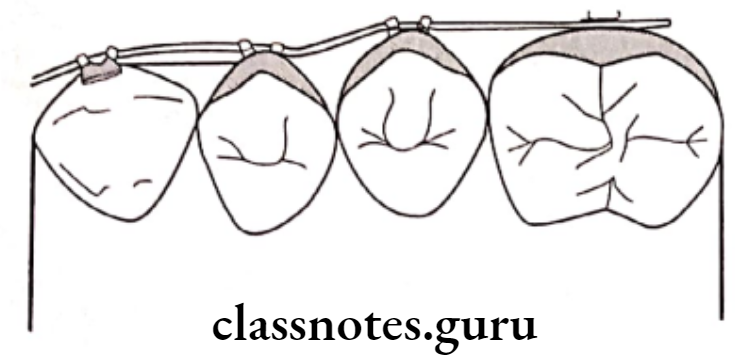
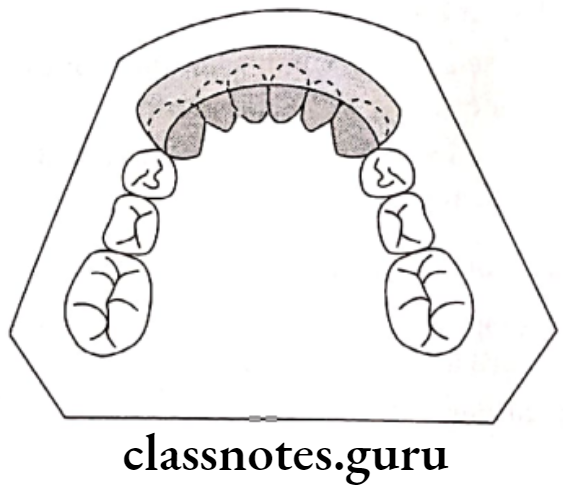
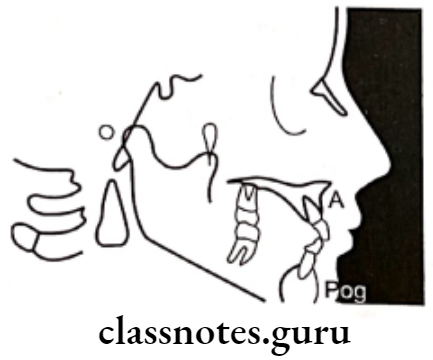
Question 13. Wit’s Appraisal.
Answer.
Significance Of Wits’s Apprasial: Measures relation of maxilla to mandible
Use: In nonreliable ANB cases
Obtained by:
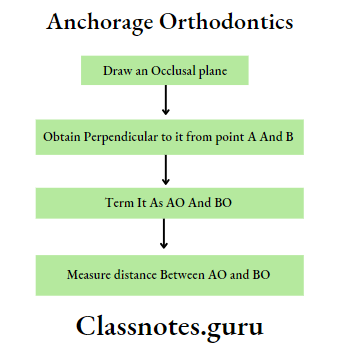
Variation Of Wit’s Appraisal:
- Males – BO ahead of AO
- Females – BO coincides with AO
- Skeletal Class 2 – BO behind AO
- Skeletal Class 3 – BO ahead of AO

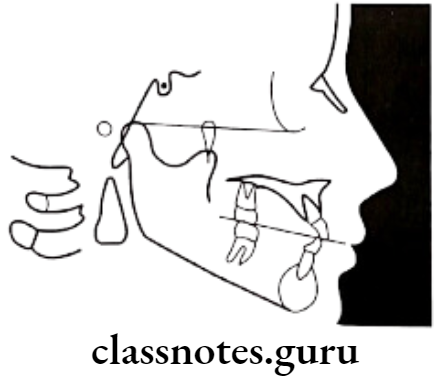
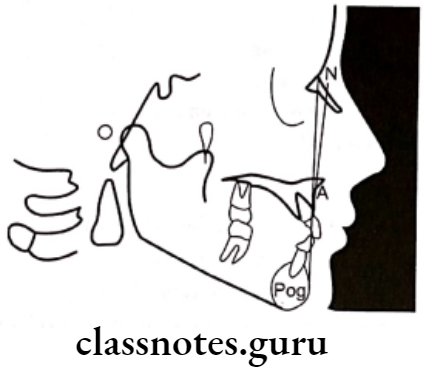
Question 14. FMA.
Answer.
Cephalometric FMA:
- FM – plane – extending from orbitale to prior
- Mandibular plane
- The angle formed between these two
- Value – 25°
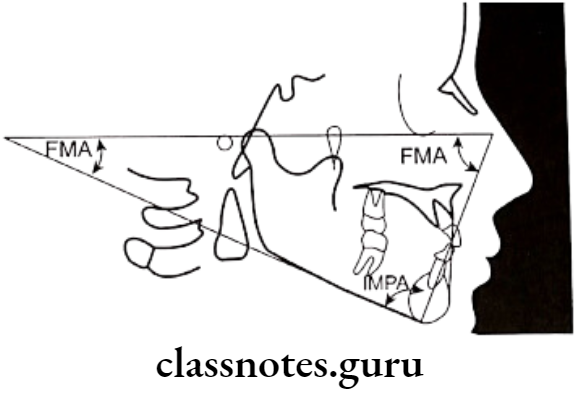
Clinical FMA:
- The angle formed between the lower border of the mandate ble and Frankfort horizontal plane
- Normally intersect at the occipital region
Significance Of FMA:
- Indicates growth pattern
- If coincides
- At occipital – Normal
- Beyond occipital – Horizontal
- Anterior to occipital – Vertical
Question 15. Cephalogram
Answer.
Cephalogram
- Cephalogram is a cephalometric radiography introduced by Holly Broadbent and Herbert Hofrath in 1931
Types Of Cephalogram:
- Lateral cephalogram – provides a lateral view of the skull
- Frontal cephalogram – provides an anteroposterior view of the skull
Cephalogram Uses:
For diagnosis:
- Study of dental and soft tissue structures
- Classify skeletal and dental abnormalities
- Assess facial type
- For treatment planning
- For presuming the changes
- For predicting growth-related changes
- For research work
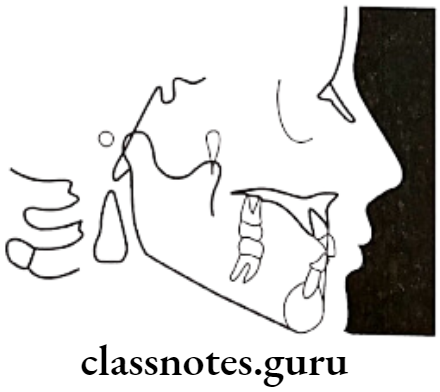
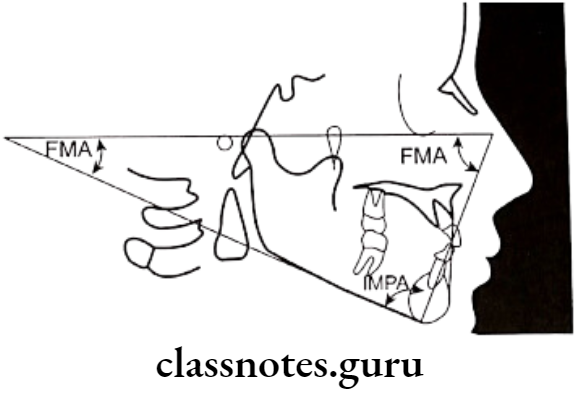
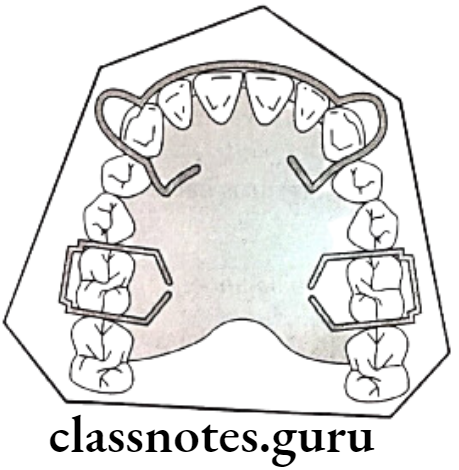
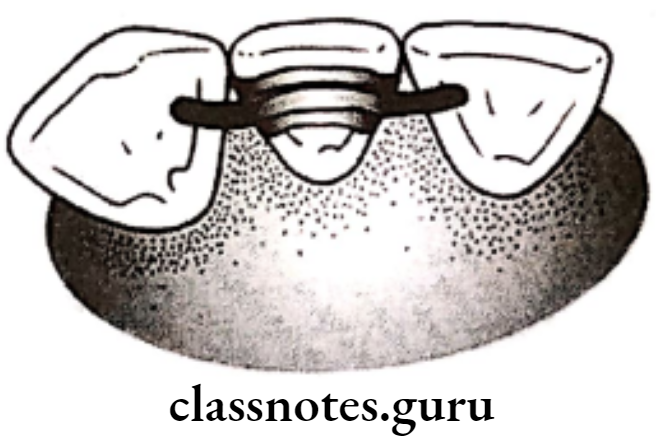
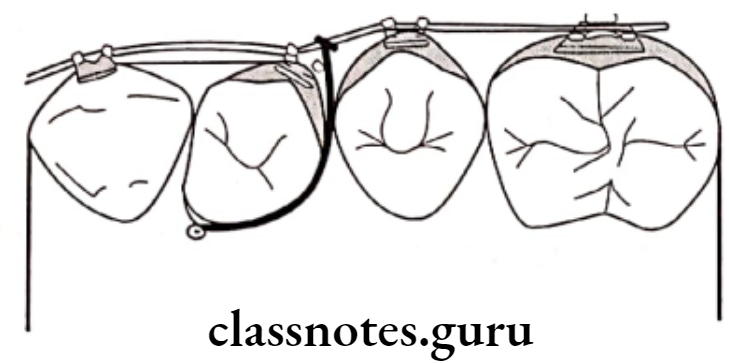
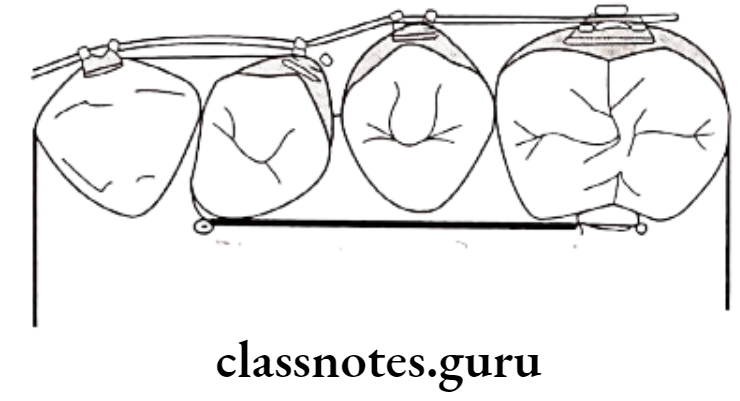
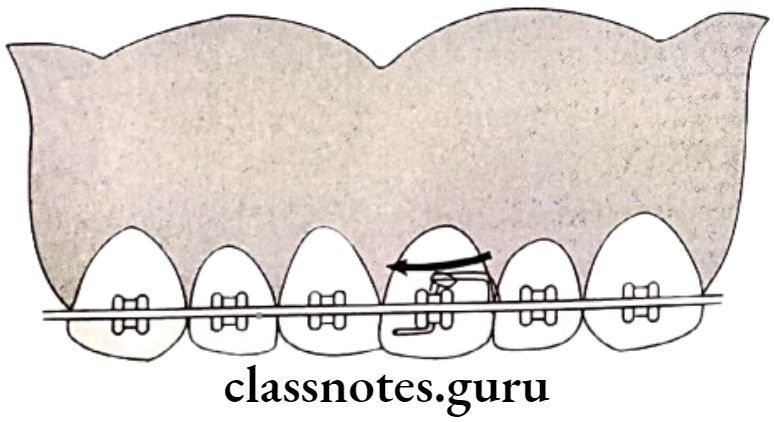
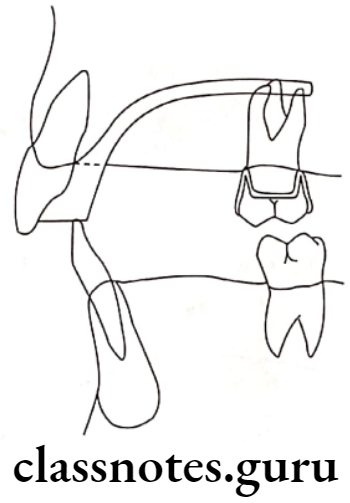
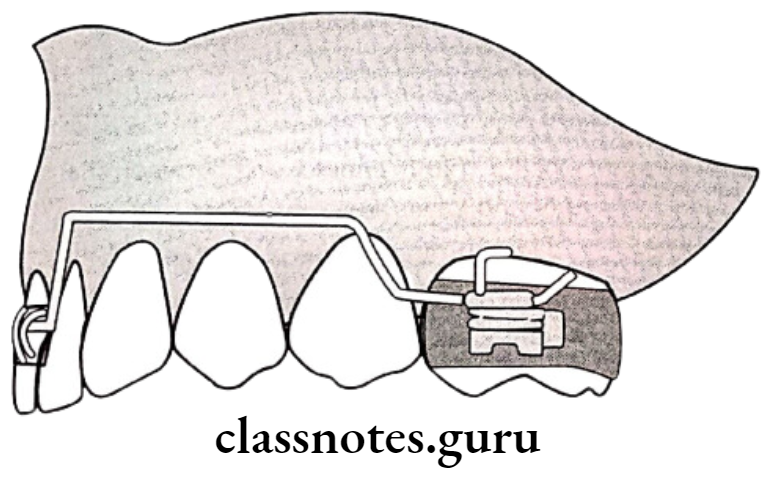
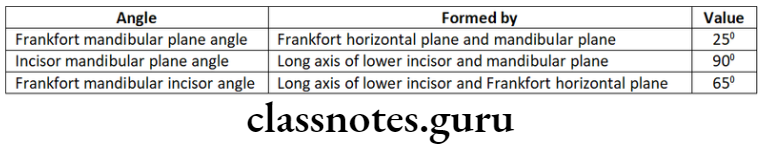
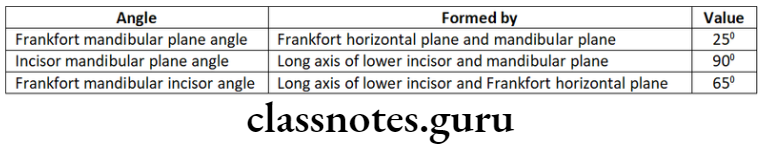
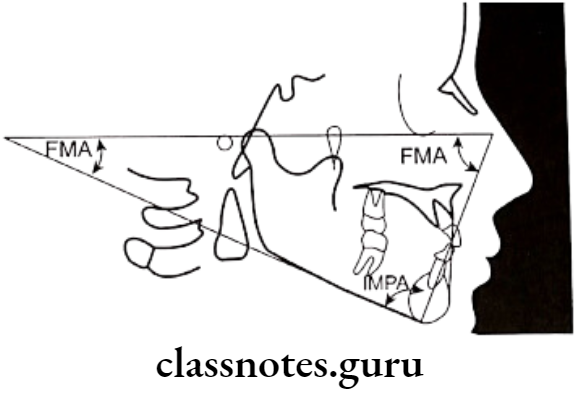
Question 16. Tweed’s triangle.
Answer.
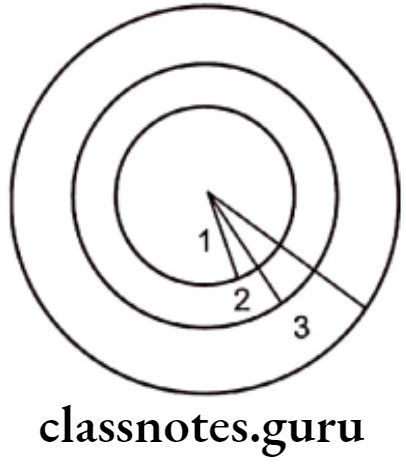
Formed by:
- Frankfort mandibular plane angle [FMPA] – 25°
- Angle by the intersection of the FH plane and mandibular plane
- Incisor mandibular plane angle [IMPA] – 90°
- The angle formed by the intersection of the long axis of lower incisor and mandibular plane
- Frankfort mandibular incisor angle [FMIA] – 65°
- The angle formed by the long axis of lower incisor and FH plane
Cephalometrics Viva Voce
- Y axis indicates the direction of the growth pattern of the mandible
- Richard A. Riedel introduced the ANB angle
- Cephalometric tracing is made on the frosted surface of an acetate tracing sheet
- E plane is also called the aesthetic plane
- Normal facial angle – 82-95°
- The normal value of the Y axis in Down’s analysis – 53-66°
- The normal value of cant of occlusion – 1.5 – 14°
- Normal value of interincisal angle – 130-150°
- The normal mandibular plane angle in Steiner’s analysis is 29°
- Decreased SNB angle indicates mandibular retrognathism
- Decreased ANB angle indicates skeletal Class 3
- The decreased facial angle indicates skeletal class 2
- A decreased angle of convexity indicates the prognathic profile
- Increased AB plane angle indicates class 3
- Increased upper incisor to NA angle indicates proclined upper incisors
- Increased lower incisor to NB angle indicates proclined lower incisors
- The facial angle indicates antero-posterior positioning of the mandible to the upper face
- AB plane angle signifies the maxilla-mandibular relationship to the facial plane’