Bacterial Infections Of Oral Cavity Important Notes
- Tuberculosis
- Tuberculosis is caused by Mycobacterium tuberculosis
- The hard tubercle consists of epithelioid cells, Langhans giant cells, plasma cells, and fibroblasts Central part of the lesion contains caseous, soft, and cheesy necrotic material Causative organism is seen in ZN or acid-fast stain
- Diagnosis can be confirmed by
- Presence of acid-fast bacilli
- Tuberculin/ Mantoux test
- Tuberculosis Treatment
- Isoniazid + rifampicin for 9 months or
- Isoniazid + rifampicin + pyrazinamide for 2 months followed by isoniazid + rifampicin for 4 months
- Ghon’s Complex
- Ghon’s complex is primary complex tuberculosis – infection of an individual who has not been previously infected/ immunized
- Ghon’s complex Components
- Pulmonary component
- Lymphatic vessel component
- Lymph node component
- Leprosy
- Caused by mycobacterium leprae
- Forms: tuberculoid type and lepromatous type
- Sheets of lymphocytes with vacuolated macrophages called lepra cells are a distinct histological feature
- Leprosy Clinical features
- Leonine facies
- Collapse of nasal bridge
- Dry, wrinkled skin
- Loss of smell sensation
- Loss of hair
- Facial and trigeminal neuralgia paralysis
- The difficulty is dosing eyes
- Features Of Tetanus
- Lockjaw
- Risus sardonicus
- Trismus
- Opisthotonus
- Laryngospasm
- Dysphagia
- Caused by Clostridium tetani
- Toxins produced by it are
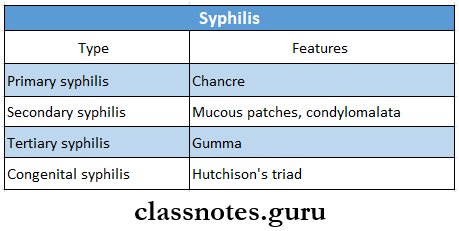
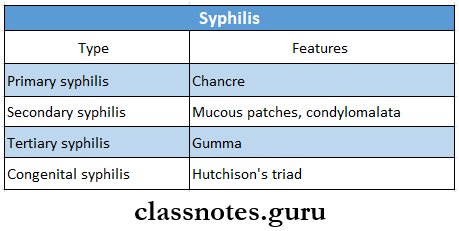
- Syphilis
- Caused by Treponema palladium
- Types and features:
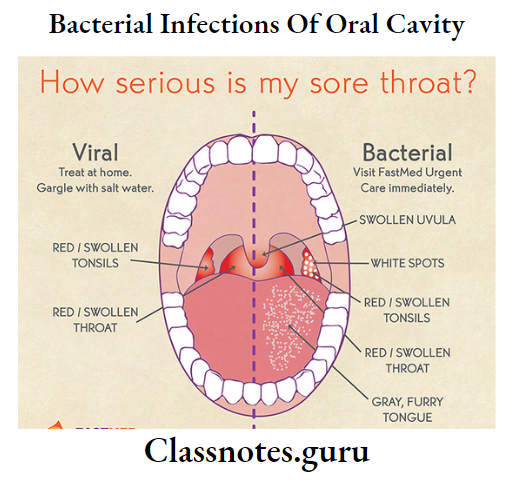
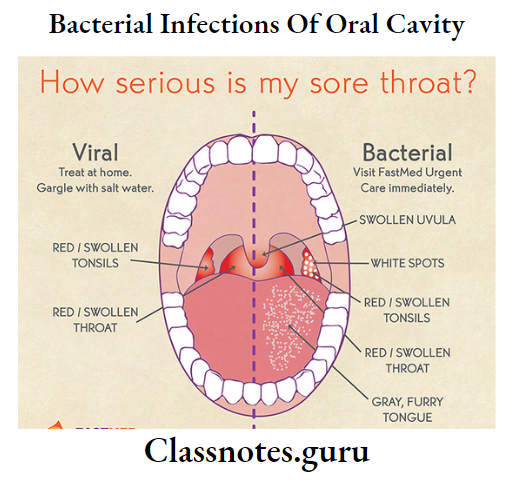
- Scarlet Fever
- Caused by streptococcus B-hemolytic
- Systemic manifestations occur first
- Skin rashes appear on 2nd and 3rd day and lasts for one week
- On the face, skin rashes appear as sunburn with goose pimples
- Oral manifestations
- Initially, the tongue is covered with a white coat through which enlarged and reddened fungiform papillae project
- This is strawberry tongue
- Later, the coating is lost and the tongue appears beefy red with hyperplastic numerous fungiform papillae
- This is called raspberry tongue
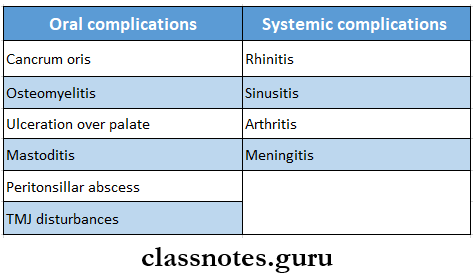
- Scarlet Fever Complications:
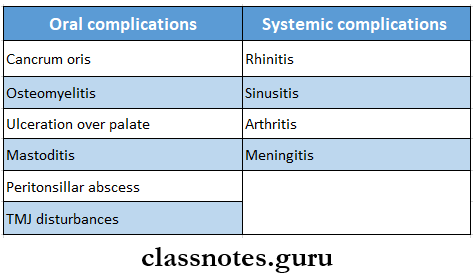
- Noma or Cancrum Oris
- Caused by specific Vincent’s organism
- Noma or Cancrum Oris is rapidly spreading mutilating, gangrenous stomatitis
- Tire odor arising from gangrenous tissues is extremely foul
- This leads to necrotizing ulcerative mucositis
- Over skin, it leads to
- Initially small, dark, reddish-purple area
- This undergoes gangrenous necrosis
- Due to the sloughing of tissues, a large hole develops on the cheek
Bacterial Infections Of Oral Cavity Long Essays
Question 1. Describe congenital and acquired syphilis
Answer:
1. Congenital Syphilis: It is an infection of the fetus established by the passage of spirochaetes from the mother through the placenta
Congenital Syphilis Clinical Features:
- Within the first 2 weeks of life, it leads to
- Rhinitis
- Chronic nasal discharge
- Loss of weight
- Bullae, vesicle formation
- Superficial desquamation with cracking and scaling of reddened soles and palms
- Petechiae, mucous patches
- After 2 years it leads to
- Interstitial keratitis
- Vascularization of cornea
- Eight nerve deafness
- Arthropathy
- Neurosyphilis
- Anterior tibial bowing
Read And Learn More: Oral Pathology Questions and Answers
Congenital Syphilis Oral Manifestations:
- Postrhagadic scarring
- These are linear lesions found around oral and anal orifices
- These are seen from 3rd-7th week after birth
- They appear as red or copper-colored linear areas covered with soft crush
- Syphilitic rhagades
- They are radially arranged and perpendicular to the mucocutaneous junction
- Teeth
- Retarded root resorption of deciduous teeth
- Sparing of permanent incisors
- Spacing between cuspid and incisors
- Malocclusion
- Open bite
- The crown of the molar is irregular- mulberry-shaped
- Incisors are screwdriver-shaped
- Rounding of mesial and distal incisal line angle
- Hypoplastic maxilla
- Frontal bossing
- Saddle nose
2. Acquired Syphilis
- Primary syphilis
- Incubation period- about 21 days
- Chancre develops
- It is a solitary, painless, indurated, non-tendered, ulcerated, or eroded lesion
- Initially, it was a dull red macule
- Later it becomes ulcerated
- Regional lymphadenopathy
- Secondary syphilis
- Appears about 6-8 weeks
- Skin lesions appear as macules, papules, follicles, or papulosquamous patches
- Circinate lesions develop on the face
- Headache
- Fever, anorexia
- Joint and muscle pain
- Laryngitis, pharyngitis
- Generalised lymphadenopathy
- Lesions develop over the mucocutaneous junction
- Tertiary syphilis
- Develops about 5-10 years after primary infection
- Affects the skin, central nervous system, CVS, mucous membrane
- Lesions are called gumma
- It is a localized, chronic granulomatous lesion with a nodular or ulcerated surface
- Causes generalized paresis, dementia, and strokes
- Bone lesions cause osteomyelitis and destruction of joints
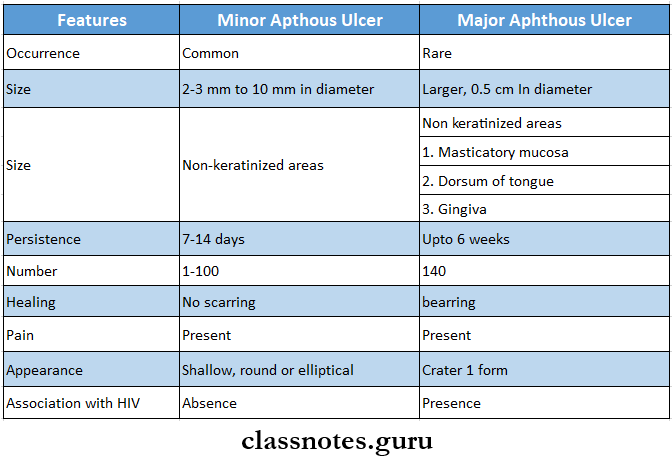
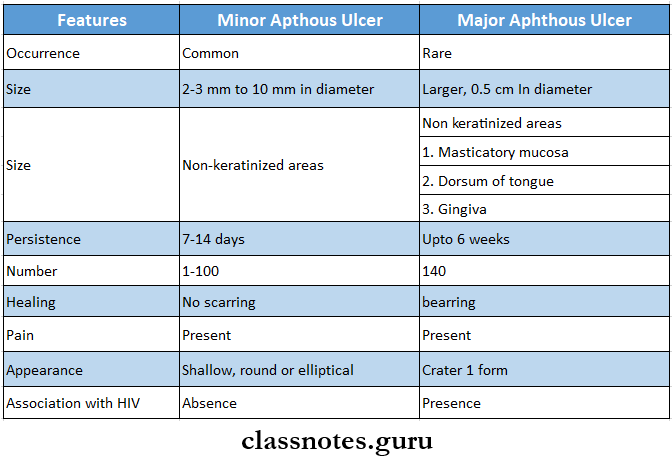
Question 2. Classify aphthous ulcers and describe its etiology, clinical features, and differential diagnosis
Answer:
Aphthous Ulcers: Aphthos ulcer is a non-traumatic ulcerative condition of the oral mucosa
Aphthous Ulcers Classification:
- Minor aphthous ulcers
- Major aphthous ulcers
- Herpetiform ulcers
Aphthous Ulcers Etiology:
- Genetic predisposition
- Exaggerated response to trauma
- Immunological factors- immunosuppression
- Microbiologic factors- herpes simplex virus
- Nutritional deficiency
- Systemic condition- Behcet’s syndrome, Crohn’s disease
- Hormonal imbalance
- Nonsmoking
- Allergy and chronic asthma
- Stress and anxiety
Aphthous Ulcers Clinical Features:
- Develops over movable, non-keratinized oral mucosa
- Produces burning or tingling sensation
- Recurs in about 3-4 weeks
- Minor Aphthous Ulcer
- Occurs either single or in clusters
- It is painful, shallow, round, or elliptical
- Size-2-3 mm in diameter
- It is surrounded by an erythematous halo
- Covered by yellowish fibrinous membrane
- Lasts for 7-10 days
- Heals without scarring
- Major Aphthous Ulcer
- Size- larger, 0.5 cm in diameter
- More painful lesion
- Makes the patient ill
- Appears crateriform
- Heals with scar formation
- Transforms into malignancy
- Herpetiform ulcers
- Extremely painful, small ulcers
- Number-few dozen to hundred
- An ulcer is surrounded by a zone of erythema
- Size-1-2 mm in diameter
- Lasts for several weeks or months
- Heals within 1-2 weeks
Aphthous Ulcers Differential Diagnosis:
- Herpetic ulcers
- Traumatic ulcers
- Pemphigus Vulgaris
- Cicatricial pemphigoid
- Ulcers due to neutropenia
Bacterial Infections Of Oral Cavity Shot Essays
Question 1. Difference Between major and minor aphthous ulcers
Answer:
Difference Between Major And Minor Aphthous Ulcers
Question 2. Tuberculous ulcer of the oral cavity
Answer:
Tuberculous Ulcer Of The Oral Cavity
Tuberculous lesions of the oral cavity occur secondary to pulmonary Infections
- Chronic ulcers
- Present over tongue, palate, gingiva, lips, buccal mucosa, alveolar ridge and vestibules
- Superficially located
- Have Irregular edges and Induration
- The base Is granular and covered by pseudomembrane
- Presence of single or multiple nodules
- Size- pinhead size
- Color- green color
- Tongue lesion
- Seen over lateral borders
- They are well-defined, painful, firm, and yellowish-grey In color
- Surrounding mucosa appears Inflamed and edematous
- Palatal lessons
- Seen over the hard palate
- They are small ulcers
- Lip lesions
- Produces small, nongendered, granulating ulcers at mucocutaneous junctions
- Gingival lesions
- Produces small granulating ulcers or erosive lesions
- Gingival hyperplasia
- Presence of diffuse, hyperactive, nodular, or papillary projections from the gingival margin
- Salivary glands
- Generalized glandular swelling or abscess formation along with pain
- Facial nerve palsy
- Fistula tract formation
- Lesions of jawbones
- Sinus or fistula formation
- Osteomyelitis
- Trismus
- Paraeslhesla
- Lymphadenopathy
- Sinus or fistula formation
- Pain and swelling of |aw bones
Question 3. Scarlet Fever
Answer:
Scarlet Fever
- Scarlet fever is caused by streptococcus B- hemolytic
Scarlet Fever Clinical Features:
- Age 3-12 years of age
- Fever
- Headache
- Vomiting
- Tonsilitis, pharyngitis, generalized lymphadenopathy
- Tonsils, soft palate, and pharynx become erythematous
- Diffuse, bright red skin rash appears over the chest and spreads to other parts of the body
- Skin rashes undergo desquamation
Scarlet Fever Oral Manifestations:
- Skin rash over the face refers to sunburn with goose pimples
- Face is flushed
- The oral cavity exhibits generalized edema, elongation of uvula, and diffuse petechiae over the soft palate
- Congested and inflamed palate
- Congestion of oral mucosa
- Hal Koala
- Strawberry tongue reddened fungiform papillae project like small, red knobs
- Later tongue appears beefy red with hyperplastic fungiform papillae called raspberry tongue
Scarlet Fever Complications:
- Cancrurnoris
- Ulceration with perforation of the palate
- Osteomyelitis
- Peritonsillar abscess
- Mastoiditis, rhinitis, sinusitis, arthritis, meningitis
- Pneumonia
- Rheumatic fever
- Acute glomerulonephritis
- Septicaemia
Question 4. Diphtheria
Answer:
Diphtheria Etiology:
- Diphtheria is caused by Corynebacterium diphtheria
Diphtheria Clinical Features:
- Diphtheria is insidious at the onset
- Moderate grade fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on the tonsils
- Swollen neck- Bull neck
- Tender lymphadenopathy
- Nasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Acute circulatory failure
- Myocarditis
- Nerve palsies
- Dysphagia
- Dysphonia
- Paraesthesia in the limbs
Diphtheria Management:
- Antitoxin diphtheric serum (ADS)
- The dose varies from 20,000 to 1,00,000 units depending on the duration and severity of the disease
- In mild cases, a lesser dose may be used
- Antibiotics
- Penicillin G-6,00,000 units every 12 hourly intravenously or
- Amoxycillin 500 mg 8 hourly for 7-10 days
- Patient allergic to penicillin
- Erythromycin- 500 mg 6 hourly or
- Azithromycin 500 mg daily or
- Rifampicin 600 mg daily
- Tracheostomy
Question 5. Actinomycosis
Answer:
Actinomycosis
- Actinomycosis is a chronic granulomatous disease
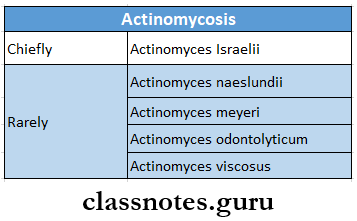
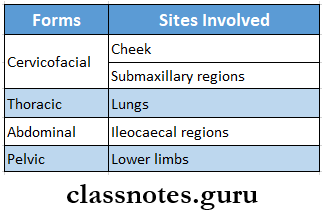
Actinomycosis Causative Organisms:
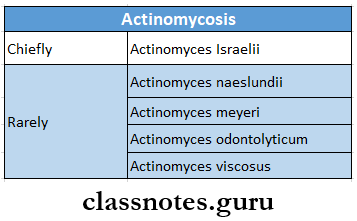
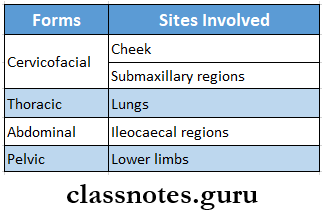
Actinomycosis Forms:
Actinomycosis Clinical Features:
- Actinomycosis is characterized by
- Multiple abscesses
- Tissue destruction
- Fibrosis
- Formation of multiple sinuses
- Painless indurated swelling
- Gingivitis
- Periodontitis
Actinomycosis Treatment:
- Draining of abscess
- Excision of sinus tract
- Use of antibiotics- penicillin and tetracyclines
Question 6. Pyogenic Granuloma
Answer:
Pyogenic Granuloma
- Pyogenic granuloma represents an over-exuberant tissue reaction to some known stimuli or Injuries
Pyogenic Granuloma Clinical Features:
- Age-at early age
- Sex- common in females
- Presence of small, pedunculated or sessile, painless, soft, tabulated growth on gingiva
- Pyogenic Granuloma gets ulcerated and bleeds profusely
- Covered by yellow fibrinous membrane
- Size-upto 1 cm in diameter
- This leads to fibro-epithelial polyp
- Pyogenic Granuloma is common in pregnancy, so it is known as a “pregnancy tumor”
Pyogenic Granuloma Histopathology:
- Pyogenic Granuloma consists of lobular masses of hyperplastic granulation tissue containing multiple proliferating fibroblasts, blood capillaries, and chronic inflammatory cells
- There is the proliferation of endothelial cells
- The overlying epithelium is thin and ulcerated
- Connective tissue shows intercellular edema
- There is the presence of areas of hemorrhage and hemosiderin pigments
Pyogenic Granuloma Treatment: Surgical excision
Bacterial Infections Of Oral Cavity Short Question And Answers
Question 1. Gumma
Answer:
Gumma
- Syphilitic gumma is a lesion caused by tertiary syphilis
- Gumma is a solitary, localized rubbery lesion with central necrosis seen in the original like the liver, testis, bone, and brain-associated scarring of hepatic parenchyma.
- Histologically, the structure of gumma shows the following:
- Qintral coagulative necrosis resembles caseation but is less destructive so that outlines of necrotic cells can still be seen.
- Surrounding zone of palisaded macrophages with lymphocytes, plasma cells, giant cells, and fibroblasts.
Question 2. Hutchison’s Triad
Answer:
Hutchison’s Triad
- Hutchison’s Triad is a feature of congenital syphilis
- Hutchison’s Triad includes:
- Interstitial keratitis
- Hutchison’s Triad results from opacification of the corneal surface with resultant loss of vision
- Enamel hypoplasia of permanent incisors and 1st permanent molars
- Eight nerve deafness
Question 3. Condyloma Lata
Answer:
Condyloma Lata
- Condyloma Lata is a feature of secondary syphilis
- Condyloma Lata is a skin lesion occurring in the form of nodular, flat, or papillary form
- Condyloma Lata resembles viral papilloma
Question 4. Treponema pallidum
Answer:
Treponema pallidum
- Treponema pallidum is a causative organism of syphilis
- Treponema pallidum is a thin, delicate spirochaete with tapering ends having about ten regular spirals
- Treponema pallidum is actively motile showing rotation around the long axis, backward and forward movements, and flexion of the whole body
- Treponema pallidum can be seen by dark ground microscopy
- Treponema pallidum enters the body through minute abrasions on the skin and mucosa
Question 5. Kveim-Siltzbatch test
Answer:
Kveim-Siltzbatch Test
- Kveim-Siltzbatch Test is an intracutaneous test for the diagnosis of sarcoidosis
- Kveim-Siltzbatch Test utilizes suspension of human-known sarcoid tissues test antigen
- Kveim-Siltzbatch Test has a high degree of specificity
- Kveim-Siltzbatch Test is important to aid in the early and accurate diagnosis of disease
Question 6. Noma or cancrum oris
Answer:
Noma Or Cancrum Oris
- Noma is a rapidly spreading and extremely severe granulomatous infection of orofacial tissues
Noma or Cancrum Oris Causative Organisms:
- Fusobacterium necrophorum
- F.nucleatum
- Prevotella intermedia
Noma Or cancrum Oris Clinical Features:
- Age-1-10 years of age
- There is a formation of painful, red, indurated papule over the gingiva
- It gets ulcerated and spreads to mucosal surfaces called necrotizing ulcerative mucositis
- A small, dark, reddish-purple area appears on the skin over the cheek
- Later large hole of a few inches develops on the cheek
- Severe sore mouth
- Increased salivation
- Diffuse edema of the face
- Foul smell from mouth
Question 7. Histopathology of Tuberculosis ulcer
Answer:
Histopathology of Tuberculosis Ulcer
- Tuberculosis ulcer consists of central areas of caseous necrosis surrounded by lymphocytes, epithelioid cells, and multinucleated Langerhans giant cells
- Epitheloid cells are altered macrophages
- Area of caseous necrosis appears eosinophilic
- Presence of tubercle bacilli
- Tuberculosis Ulcer is surrounded by fibrous tissue and lymphocytes
Question 8. Ghon’s Complex
Answer:
Ghon’s Complex
- Primary complex/Ghons complex/childhood tuberculosis/ is primary tuberculosis.
- Is the infection of an individual who has not been previously infected/immunized.
- Ghon’s Complex consists of 3 components:
- Pulmonary component
- Lymphatic vessel component
- Lymph node component.
- The most commonly involved tissues for the primary complex are the lung and hilar lymph nodes.
- Tubercle bacilli, either free/within phagocytes drain the regional lymph nodes, which often causes.
- This combination of the parenchymal lesion and nodal involvement is referred to as Ghons complex
Question 9. Sarcoidosis
Answer:
Sarcoidosis
- Sarcoidosis is a multi-system chronic granulomatous disease
Sarcoidosis Clinical Features:
- Age- 20-40 years of age
- Sex- common in females
- The organs involved are:
- Lymph nodes
- Salivary glands
- Skin
- Bone
- Fever, malaise
- Dry cough
- Weight loss
- Chest pain, dyspnea
- The presence of multiple, slow-growing, red patches over the skin which may ulcerate
Sarcoidosis Oral Manifestations:
- Keratoconjunctivitis
- Enlargement of parotid gland
- Xerostomia
- Small nodular submucosal growth appears over soft palate, gingiva, floor of mouth, or cheek
- Multiple erythematous nodules develop over the cheek, labial mucosa, and hard palate
Question 10. Mantoux Test Or Tuberculin Test
Answer:
Mantoux Test Or Tuberculin Test
- It is a routinely used method for tuberculin testing
Mantoux Test Or Tuberculin Test Method:
- 0.1 ml of purified protein derivative/ PPD containing 51D, tuberculin unit is injected intradermally into the flexor aspect of the forearm
- Mantoux Test is given between layers of the skin
- The site is examined after 48-72 hours for induration
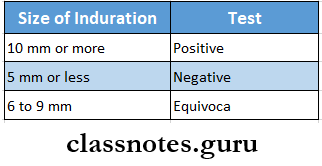
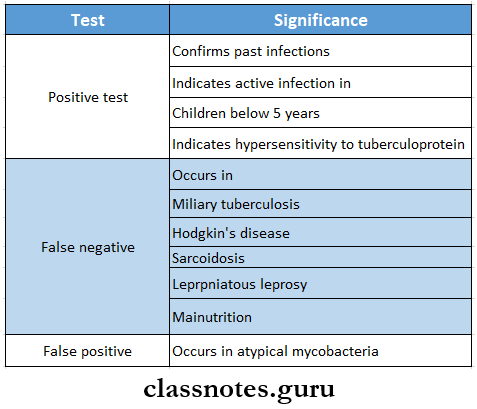
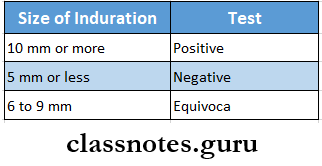
Mantoux Test Or Tuberculin Test Result:
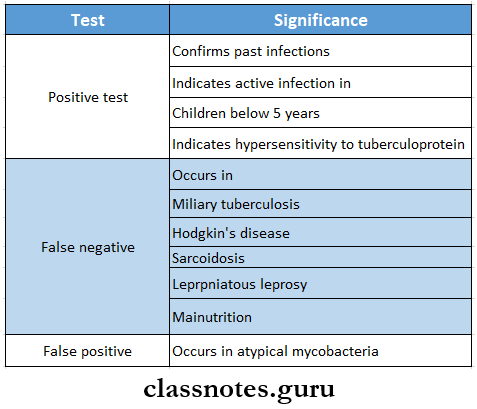
Mantoux Test Or Tuberculin Test Significance:
Question 11. Lumpy Jaw
Answer:
Lumpy Jaw
- Lumpy Jaw is a cervicofacial form of actinomycosis
- Lumpy Jaw is caused by Actinomyces israelii
- It is soft tissue swelling developing in the mandibular anterior region
- Develops abscess with discharge of pus containing sulfur granules
- The skin overlying the abscess is purplish red, indurated, and fluctuant
- Abscess may perforate the skin surface
Question 12. Chancre
Answer:
Chancre
- Chancre is one of the clinical findings of primary syphilis
- Incubation period 3-90 days
- Site
- Penis in males
- Vulva or cervix in females
- Chancre is slightly raised over the surface
- Chancre becomes ulcerated
- Chancre is a non-tender, non-bleeding firm plaque
- Shape- round and indurated
- Size- varies from 5 mm to several centimeters
- Edges- rolled raised edges are seen
- Chancre disappears without treatment
Bacterial Infections Of Oral Cavity Viva Voce
- The causative organism of syphilis is Treponema pallidum
- DOTS therapy is used in tuberculosis patients
- Clostridium tetani causes tetanus
- Raspberry tongue and strawberry tongue are peculiar features of scarlet fever
- Diphtheria is caused by Corynebacterium diphtheria
- Scarlet fever is caused by streptococcus B- hemolytic
- The Kim-Siltzbatch test is used for the diagnosis of Sarcoidosis
- Bull neck is a condition -seen in diphtheria
- Diphtheria may lead to death due to airway obstruction
- Asteroid bodies or Schaumann bodies are a histological feature of Sarcoidosis
- Pyogenic granuloma leads to fibroepithelial polyp
- Intercellular edema is seen in connective tissue in the case of pyogenic granuloma.