Amalgam Important Notes
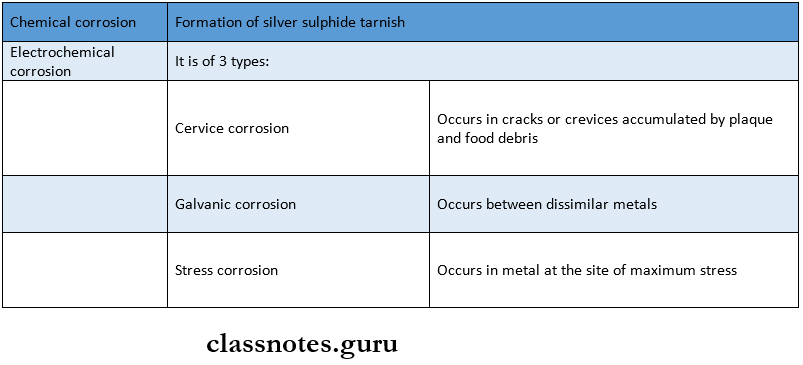
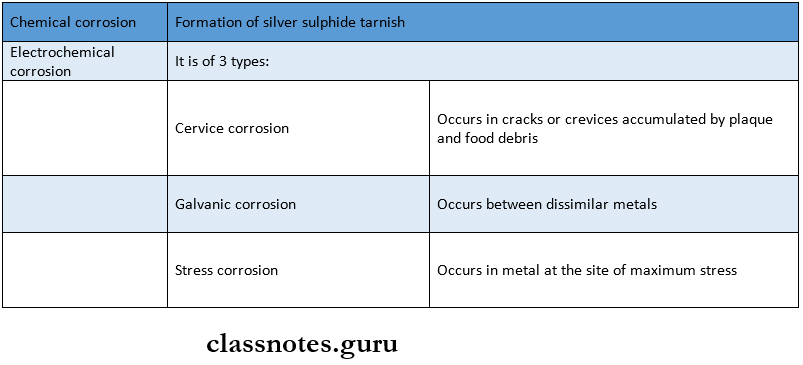
1. Types Of Corrosion
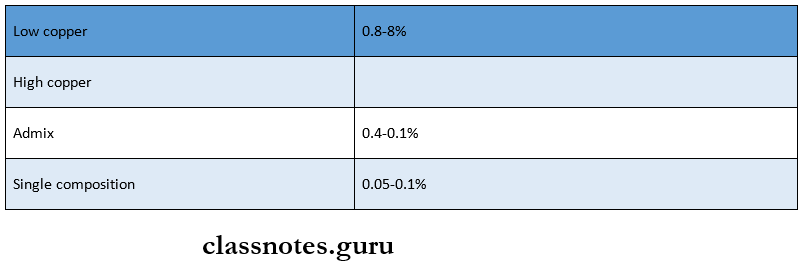
2. Creep Values
3. Mercury Toxicity
- The maximum level of occupational exposure considered safe is 50 pg of mercury/m3 of air
- Mercury vapors may be released from the Ag-Hg phase which is melted during the polishing and amalgam removal process
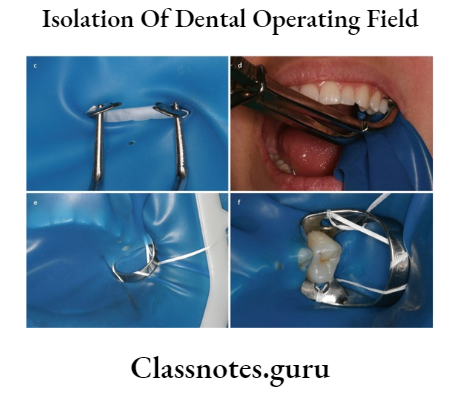
- Rubber dam, high volume evacuation, and water cooling unit are used during the removal of amalgam
- Masks can’t filter mercury vapors
- Mercury toxicity results in acrodynia or Pink’s disease
- It is characterized by pinkish discoloration of the skin, profuse salivation, ulceration of the mucosa, and premature shedding of teeth
- Mercury has an average half-life of 55 days for transport through the body to the point of excretion
- Spent capsules and mercury-contaminated cotton rolls or napkins should be stored in tightly capped pressure containers
4. Forms Of Mercury
- Elemental mercury – vapor is inhaled and absorbed through the lungs at 80% efficiency
- Inorganic mercury – exists mainly as sulfide and is absorbed easily by GIT
Read And Learn More: Operative Dentistry Short And Long Essay Question And Answers
- Organic mercury in the form of methylmercury mercury – mainly carried through food
5. Failures Of Amalgam Restorations
- Bulk fractures of restorations
- Corrosion
- Excessive marginal fractures
- Sensitivity or pain
- Secondary caries
- Fracture of tooth structure
Amalgam Question and Answers
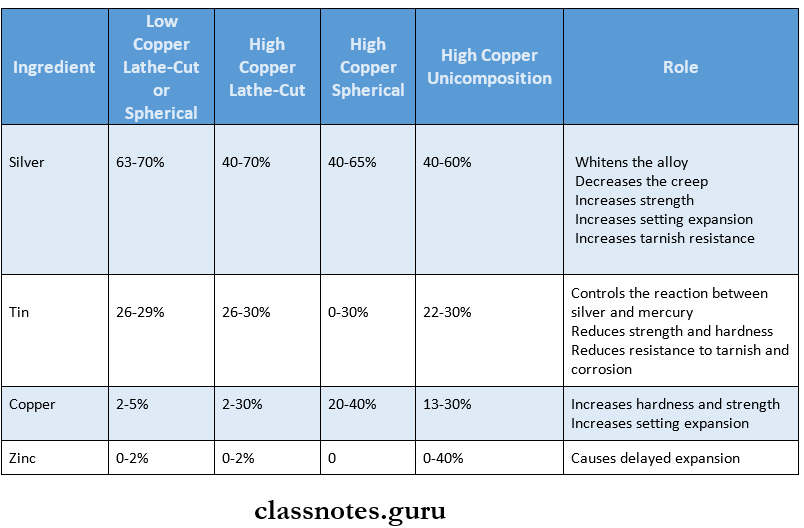
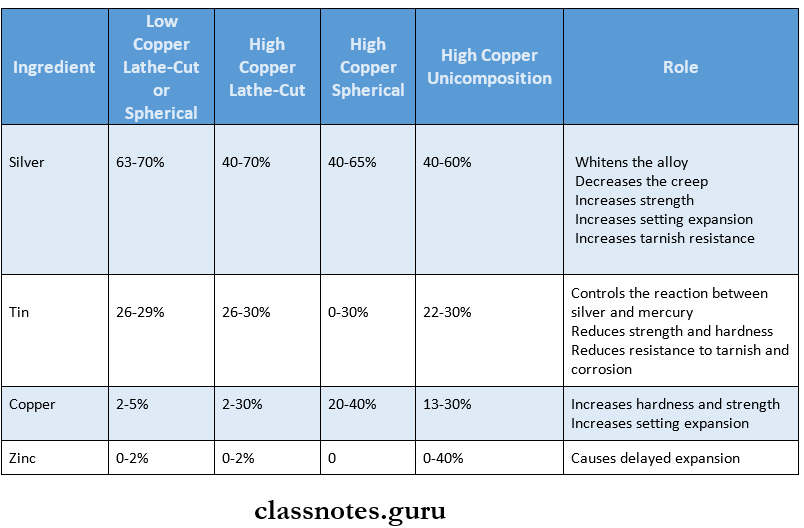
Question 1. Classify silver alloys. Give the role of each ingredient of silver alloy. Add a note on zinc alloys
(or)
Classify amalgam alloys, write the role of each ingredient, and add a note on gamma 2 phase
Answer:
Amalgam:
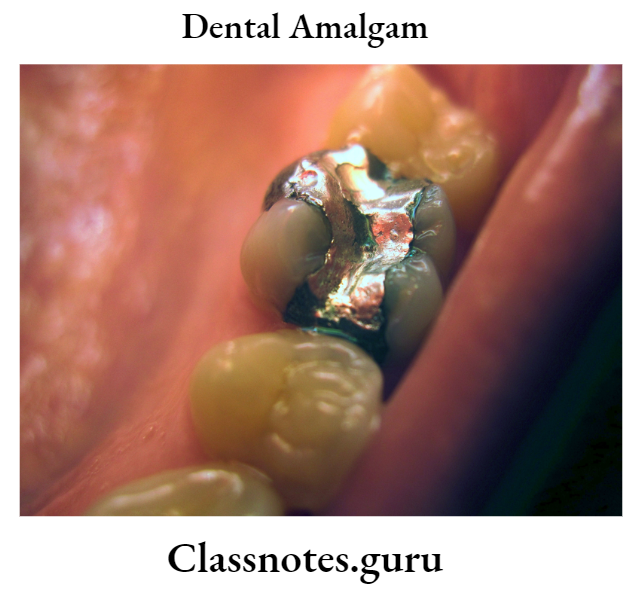
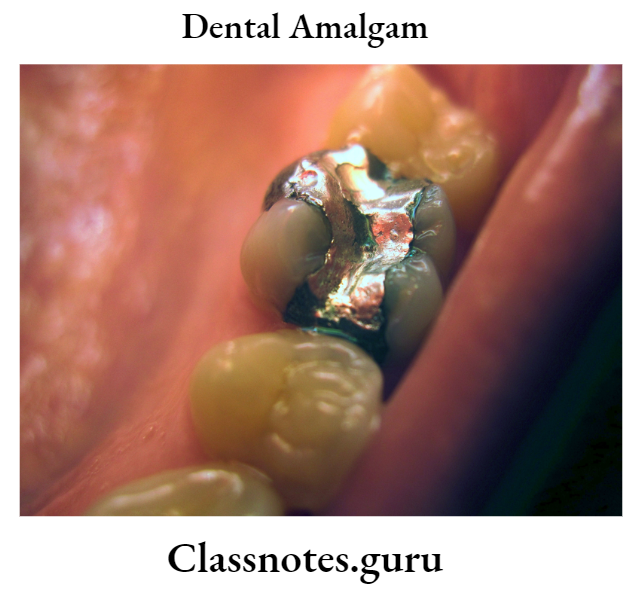
Dental amalgam is an alloy of mercury, silver, copper, and tin which may also contain palladium, zinc, and other elements to improve handling characteristics and clinical performance
Amalgam Classification:
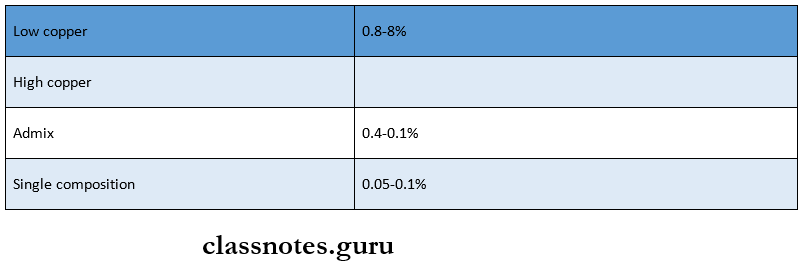
1. Based On Copper Content
- Low copper alloys- contain less than 6% copper
- High copper alloys- contain between 13-30% cop-per
2. Based On Zinc Content
- Zinc containing alloys
- Zinc free alloys
3. Based On The Shape Of AThe Alloy Particle
- Lathe cut alloys
- Spherical alloys
4. Based On The Number Of Alloyed Metals
- Binary alloys
- Tertiary alloys
- Quaternary alloys
5. Based On The Size Of The Alloy
Amalgam Composition:
Mercury:
- Mercury is added to the alloy
Platinum:
- Hardens the alloy
- Increases resistance to corrosion
Palladium:
- Hardens and whitens the alloy
Indium:
- Reduces mercury vapor and improves wetting
Zinc Free Alloys:
- Contains less than 0.01% zinc
- It avoids the delayed expansion of the amalgam which occurs in zinc-containing alloys
- This results in the prevention of dimensional change in the restoration
- Prevents micro-leakage and secondary caries formation
Gamma 2 Phase:
- Gamma 2 phase is Sn and Hg (Sn8Hg)
- Weakest component
- Hardness is 10% that of Gammal
- Least stable in a corrosive environment;
Question 2. Discuss in detail the manipulation of silver amalgam. Add a note on high copper amalgam.
Answer:
Manipulation Of Amalgam
1. Selection Of Materials:
- Alloy Selection:
- For restorative purposes- high resistance amalgam is selected
- For strength- High copper alloys are selected
- If moisture control is difficult- non-zinc-containing alloys are selected
- Mercuryattoy Ratio:
- To achieve smooth and plastic amalgam an amount of mercury in excess is desirable
- But because of the harmful effects of excess mercury, it is necessary to reduce the amount of mercury
- One of the methods for it is to reduce the original mercury/alloy ratio
- This is called the Eames technique
- Sufficient mercury must be present in the mix and it should be as low enough so that mercury content is acceptable during condensation
- Ratio is 1:1
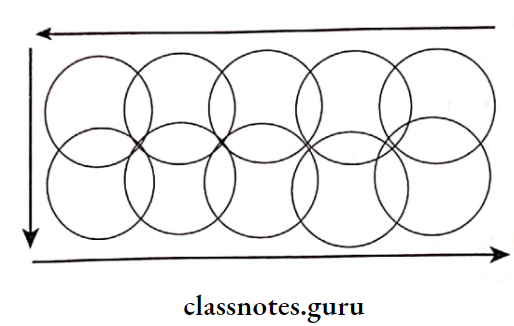
2. Trituration:
- Objective:
- To wet all the surfaces of the alloy particles with mercury
- The film should be rubbed off to obtain a clean surface of alloy for mercury
- Manual Mixing:
- A glass mortar with a roughened inner surface and a pestle with a round end is used for mixing
- It depends on
- Number of rotations
- Speed of rotations
- Pressure placed on pestle
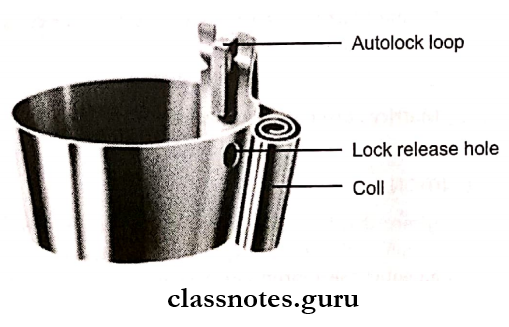
- Mechanical mixing
Alloy and mercury are dispensed into the capsule
↓
The capsule is secured in the machine
↓
The machine is turned on
↓
The automatic timer is set
↓
Trituration is accompalished
3. Mulling:
- Mulling is continuation of trituration
- Mulling causes the mix to cohere so that it can be readily removed from the capsule
- Achieved by vigorously rubbing between first finger and thumb for 2-5 sec
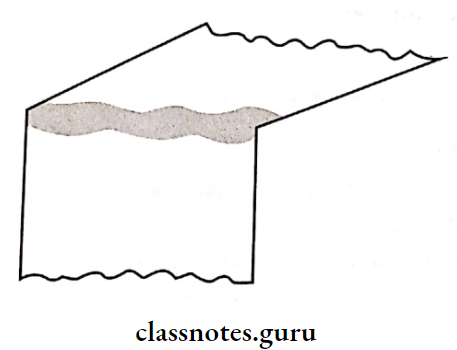
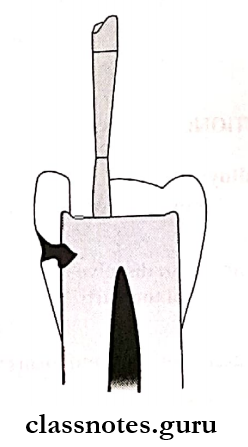
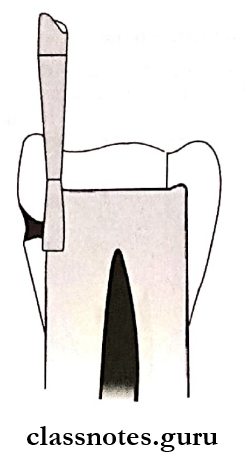
4. Condensation:
- Amalgam is placed in a prepared cavity and condensed using suitable condensers
- Aims
- To compact alloy into a prepared cavity
- To remove any excess mercury in each increment
- Reduces voids
5. Carving And Finishing:
- Carved to reproduce proper tooth anatomy
- Smoothen through burnishing with a ball bur¬nisher
- Final smoothening can be achieved by rubbing with a moist cotton pellet
- Polishing minimizes corrosion and prevents adherence to plaque
- It is delayed for 24 hours
- Wet polishing is desirable
High Copper Alloys:
- Contains 13-30%, weight copper
- They are preferred because of
- Improved properties
- Resistance to corrosion
- Better marginal integrity
- Improved performance in clinical trials
High Copper Alloys Types:
1. Admixed Alloys
- Regular type
- Unicomposition alloy
2. Single-Composition Alloy
Composition
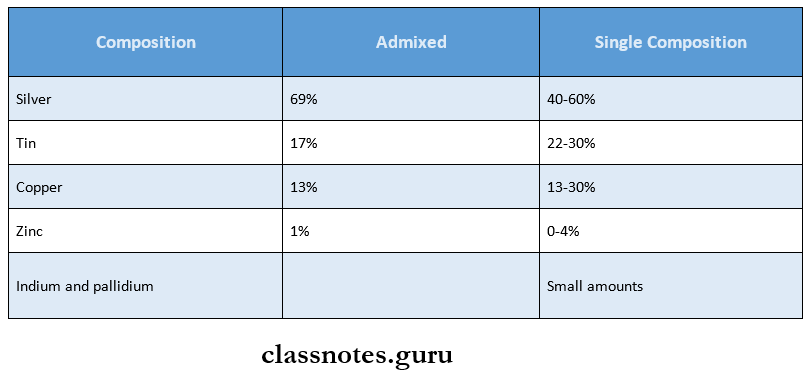
High Copper Alloys Setting Reaction:
1. Admixed Alloy:
Components are mixed
↓
Mercury begins to dissolve the outer portion
of the particle
↓
Silver enters mercury and forms the yx phase
↓
Tin dissolved in mercury reacts with copper
and forms Cu6 Sn8
2. Single Composition:
Each particle contains Ag3 Sn, AgSn, and Cu3 Sn
↓
Silver and tin dissolve in mercury form the Yj phase
↓
Later a layer of Cu6 Sn8 is formed at the surface of the alloy
particles
High Copper Alloys Advantages:
- Sets fasts
- Low residual mercury
- Faster finishing
- High strength
- Low condensation pressure
High Copper Alloys Disadvantages:
- Less working time
- Condensation pressure is not sufficient
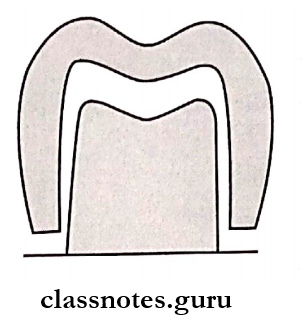
Question 3. Define class 2 cavity and enumerate various retention, resistance, and convenience forms in class 2 restoration.
(or)
Define retention form. discuss various methods of retention form in cavity preparation
Answer:
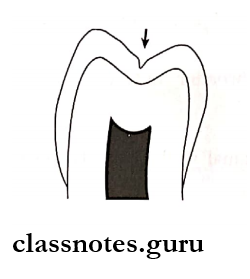
Class 2 Cavity:
- Preparation involving the proximal surface of posterior teeth is termed class 2
Retention
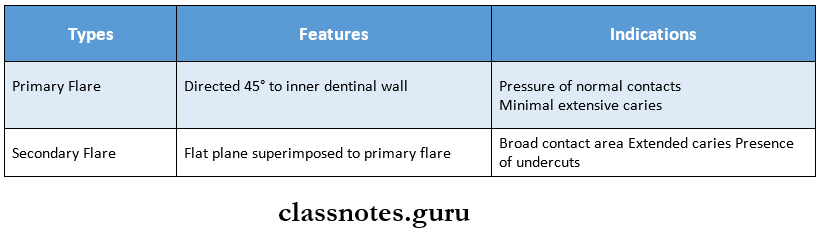
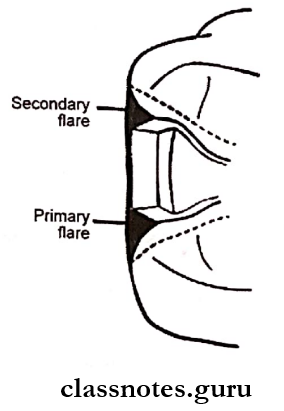
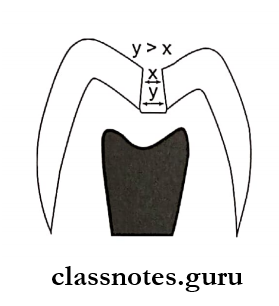
1. Primary Retention Form:
- It is the shape or form of the conventional prepara¬tion that prevents displacement or removal of the restoration by tipping or lifting forces for non-bonded restorations
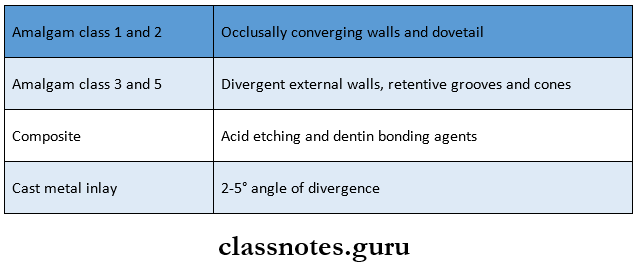
- Primary Retention Form For Amalgam Restoration
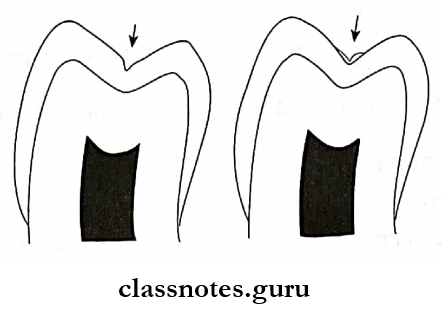
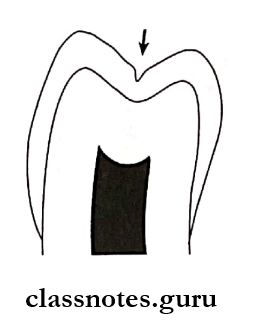
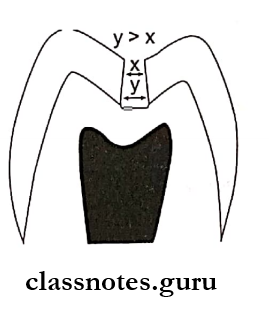
- Occlusal convergence is provided
- Primary Retention Form For Composite Restoration
- Composite restorations are retained by micro¬mechanical bond
- Bonding is increased by bevel and flare in enamel
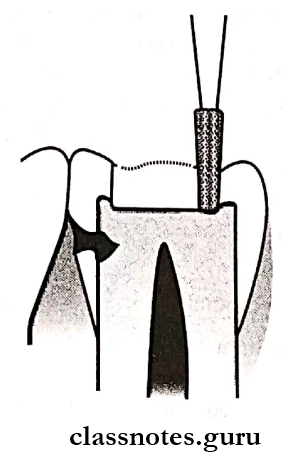
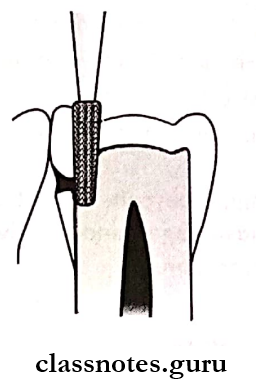
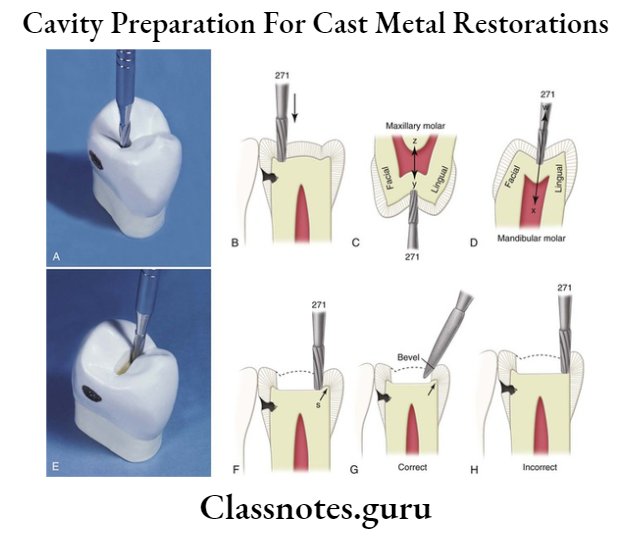
- Primary Retention Form For Cast Metal Restoration
- Obtained by
- Parallel vertical walls
- The small angle of divergence
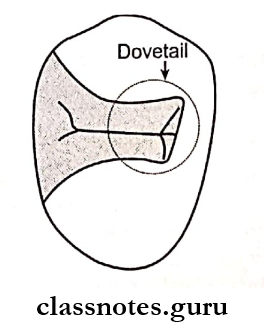
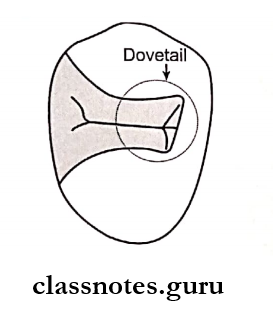
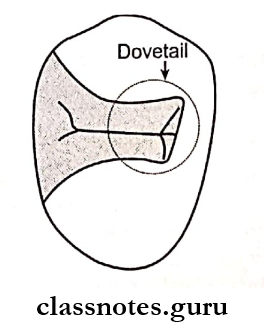
- Occlusal dovetail
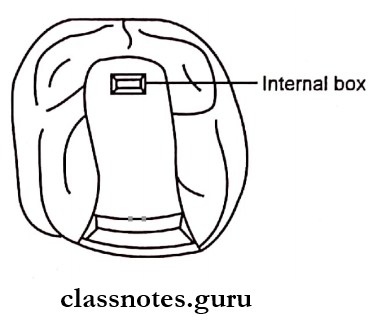
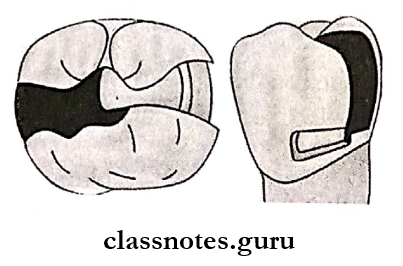
2. Secondary Retention Forms:
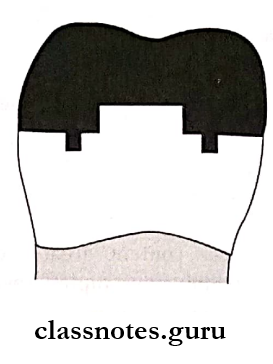
- Grooves And Coves
- At axiofacial and axiolingual line angles
- For cast restoration
- Slots
- In occlusal box, buccoaxial, linguoaxial and gin-gival walls
- For amalgam and cast restoration
- Locks
- In the proximal/occlusal box
- For amalgam
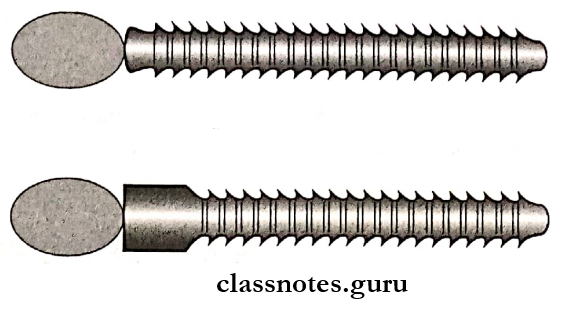
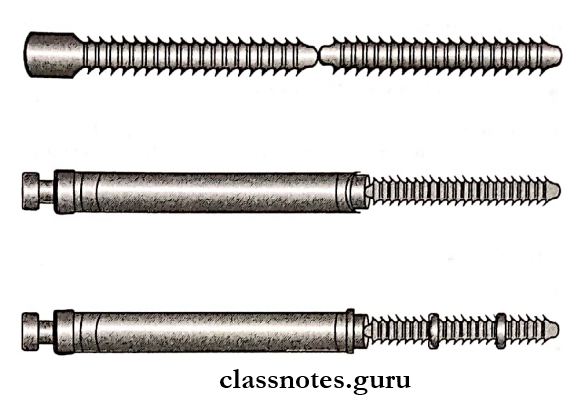
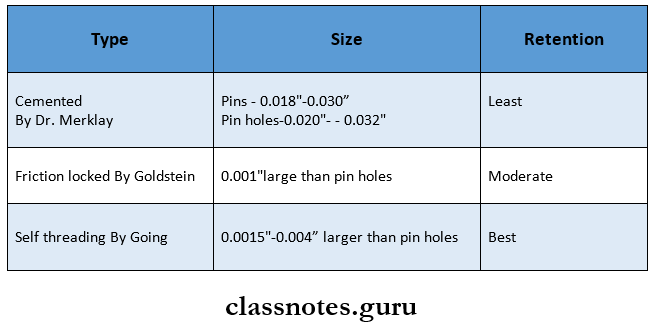
- Pins – For amalgam, composite, and cast restoration
- Skirts
- On all four sides of the preparation
- For cast restoration
- Amalgampins – For amalgam restoration
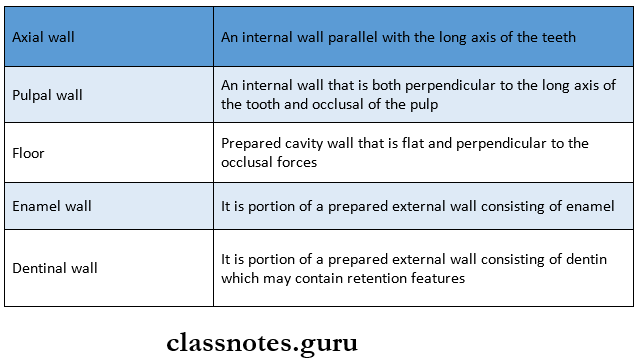
Resistance Form:
- Resistance Form may be defined as the shape and placement of the preparation walls that best enable the remaining tooth structure and the restoration to withstand, without fracture, masticatory forces delivered principally along the long axis of the tooth
Resistance Form Features:
- Relatively horizontal floors
- Box-like shape
- Inclusion of weakened tooth structure
- Prevention of cusps and marginal ridges
- Rounded internal line angles
- The adequate thickness of restorative material
- Reduction of cusps for capping, when indicated
Resistance Form Convenience Form:
- Convenience Form is the shape or form of the preparation that provides for adequate observation, accessibility, and ease of op¬eration in preparing and restoring the tooth
- Convenience Form is obtained by
- Occlusal divergence of vertical walls
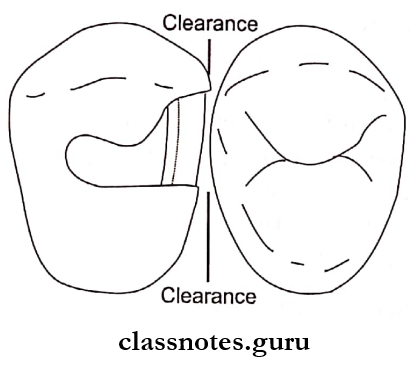
- Extending proximal preparation beyond proximal contacts.
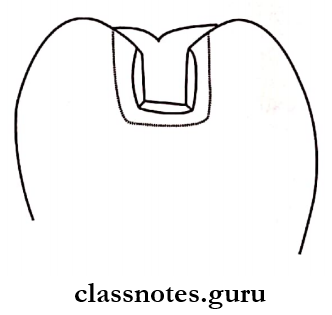
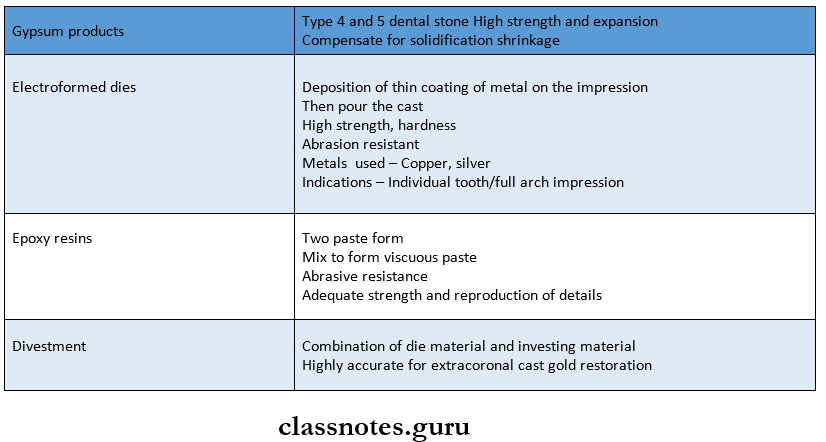
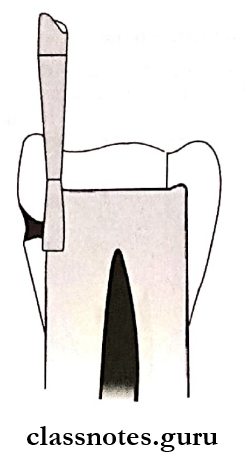
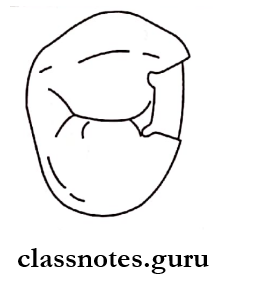
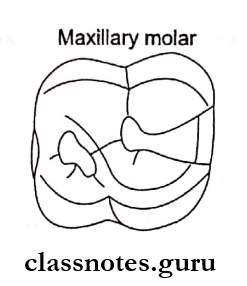
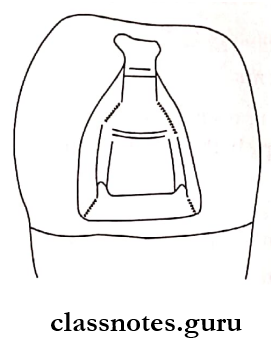
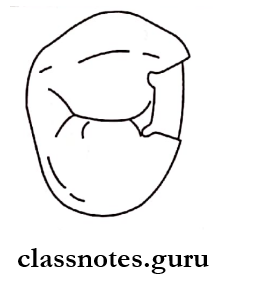
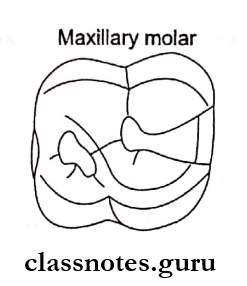
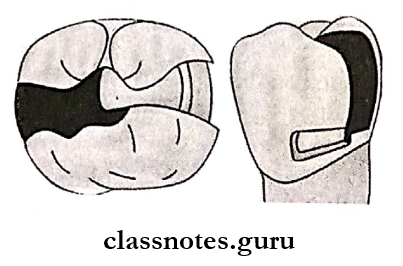
Question 4. Discuss tooth preparation of maxillary first mo¬lar for class 2 mesioocclusal amalgam restoration.
Answer:
Tooth preparation of maxillary first mo¬lar for class 2 mesioocclusal amalgam restora¬tion:
Steps
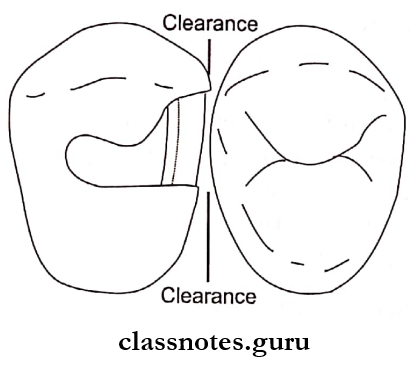
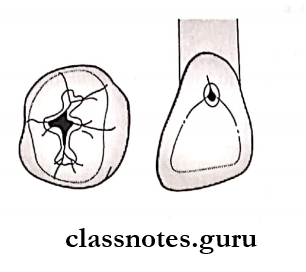
1. Outline Form:
- It means placing the preparation margins in the positions they will occupy in the final preparation except for finishing enamel walls and margins
- Using high-speed bur with air-water spray enter the pit on the occlusal surface area to the mesial surface
- Maintain an initial depth of 1.5-2 mm
- Extend upto central fissure
- Maintain uniformity of pulpal floor
- Enameloplasty is done if required
- Maintain width of the cavity to l/4th of the intercuspal distance
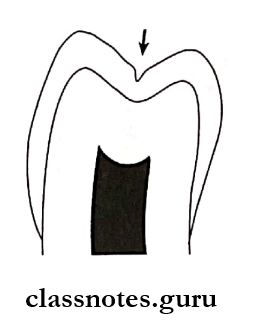
- Occlusal convergence is made
- Widen preparation faciolingually
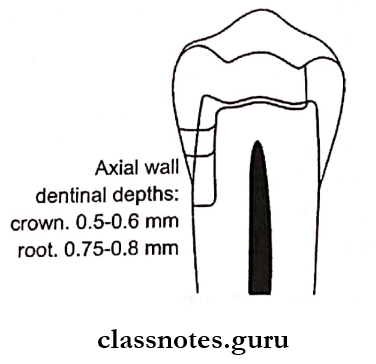
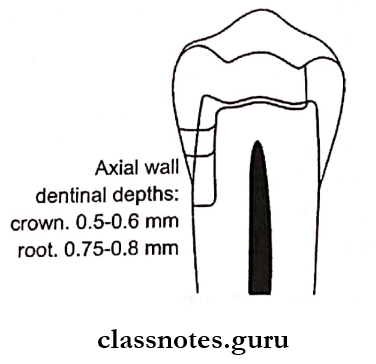
- Proximal cutting upto 0.5-0.6 mm depth
- Make cavosurface angle of 90°
- Ideal clearance 0.3-0.5mm
- Preservation of marginal ridge
- The reverse curve in the case of broader contacts
2. Primary Resistance Rorm:
- Primary Resistance Rorm may be defined as the shape and placement of the preparation walls that best enable the remaining tooth structure and the restoration to with¬stand, without fracture, masticatory forces delivered principally along the long axis of the tooth
Primary Resistance Form Features:
- Box-shaped preparation
- Flat pulpal floor
- Inclusion of all weakened structure
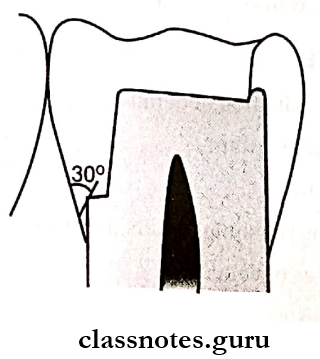
- Cavosurface angle of 90o
- Rounded internal line and point angles
- Cusp. Capping
- Minimal width of preparation
3, Primary Retention Form:
- Primary Retention Form is the shape or form of the conventional preparation that prevents displacement or removal of the restoration by tipping or lifting forces for non-bonded restorations
- It is achieved by
- Occlusal convergence
- Dovetail
4. Convenience Form:
- Convenience Form is the form and shape of the cavity that enables ease of accessibility, visibility, and ease of operation.
5. Final Tooth Preparation:
- Inspect the preparation
- Removal of debris, old restorative material
- Removal of soft caries with a spoon excavator
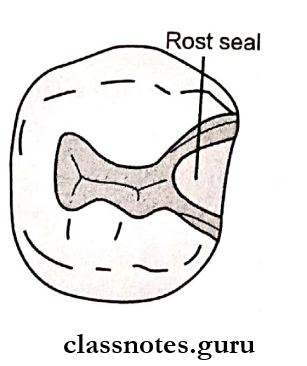
6. Secondary Retention And Resistance Form:
- Retention grooves and locks in the proximal box
- Slots in the gingival floor
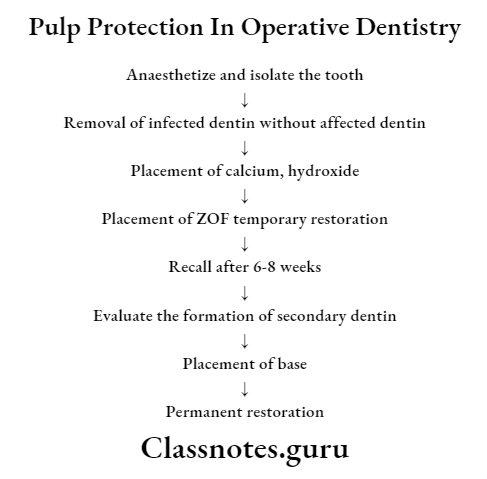
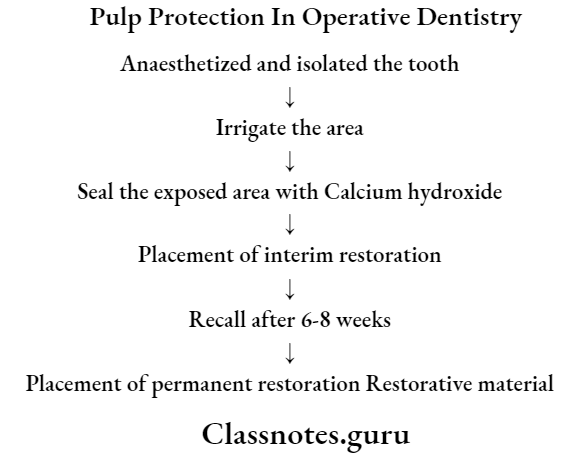
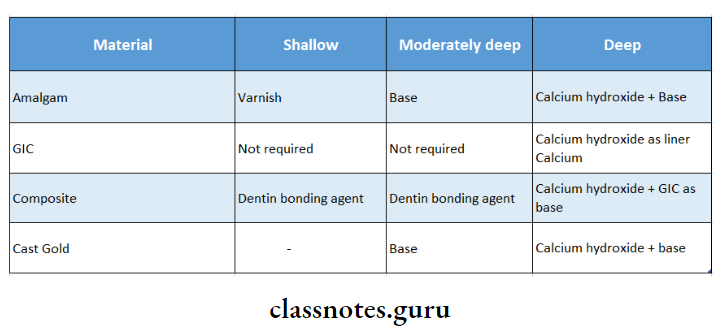
7. Pulp Protection:
- Use of pulp protective materials.
8. Finishing Of External Walls:
- Removal of all unsupported enamel
- Bevelling of the enamel of the gingival wall with GMT
Question 5. Principles of cavity preparation and describe secondary retention form in class 2 for amalgam restoration.
Answer:
Principles Of Cavity Preparation:
1. Cavity Preparation Initial Steps:
1. Cavity Preparation Outline Form:
- Placing the preparation margins to the place they will occupy in the final tooth preparation
Cavity Preparation Factors:
- Extension of all carious lesions
- Caries index
- Old restorative material
- Initial depth 0.2-0.8 mm
- Esthetics
Cavity Preparation Features:
- Preserve cuspal strength
- Preserve marginal ridge
- Minimize extension
- Maintain initial depth to 0.2-0.8 mm
- Enameloplasty wherever required
2. Primary Resistance Form:
- “Primary Resistance Form is that shape and form of the cavity which enables both tooth and restoration to withstand without fracture the stresses of masticatory forces delivered principally along the long axis of the tooth”
Primary Resistance Form Features:
- Box-shaped preparation
- Flat pulpal floor
- The adequate thickness of restorative material
- Preservation of marginal ridge
- Inclusion of weakened tooth structure
- Rounded internal line angles
- Cusp capping
3. Primary Retention Form:
- Primary Resistance Form is the form and shape of the cavity that resists the displacement of restoration from lifting and tipping forces
Primary Resistance Form Features:
- Occlusal convergence
- Dovetail
4. Convenience Form:
- Convenience Form is the form and shape of the cavity that enables ease of accessibility, visibility, and ease of operation
Convenience Form Features:
- Adequate extension
- Cavosurface margin
- Proximal clearance
Question 6. Discuss the causes of failure of amalgam restoration and how you manage them clinically.
Answer:
1. Poor Case Selection:
- Teeth with extensive caries
- Presence of para-functional habits
- Heavy masticatory form
amalgam Management:
- Proper case selection should be done
- Patient’s esthetic concerns, economic status, medical condition, and age should be taken into consideration
- Patients at high risk for dental caries may require an initial treatment plan to limit disease progression until caries risk factors are reduced or eliminated
2. Defective tooth preparation:
- Inadequate Occlusal Extension
- Increased risk of secondary caries
- Under The Extension Of The Proximal Box
- Not upto embrasure
- Interferes with self-cleaning action
- Over-Extended Tooth Preparation
- Tooth fracture
- Need of cusp, capping
- Depth Of Preparation
- Shallow cavity – Inadequate thickness of restorative material
- Deep cavity – Pulpal damage
Defective tooth Management:
- Minimal occlusal thickness for resistance to fracture should be 1.5 mm
- Restrict the buccolingual extension of the external walls to allow strong cusp and ridge areas to remain with sufficient dentin support
- In case of extensive tooth preparation, cusp cap-ping is done
- A pulpal depth of approximately 1.5-2 mm and usually a maximum depth into the dentin of 0.2 mm is maintained
3. Defective Amalgam Manipulation:
- Incorrect Mercury Alloy Ratio
- More the mercury, the less the strength
- Trituration
- Overtriturated – shiny wet and soft
- Under triturated – dry mix
- Improper Condensation
- Faulty Finishing And Polishing
- Excessive heat production during polishing causes pulpal trauma
- Heavy pressure during polishing -overhangs
Defective Amalgam Manipulation Management:
- Use proper mercury: alloy ratio as 1:1
- Use of proper triturated amalgam
- Amalgam should be adapted to all the walls
- Condensation done in small increments
- Use of coolant along with finishing and polishing of restoration
4. Defective Matrix Adaptation:
Defective Matrix Adaptation Management:
- The matrix should be properly contoured
- Use of wedge
- Stabilization of wedge
- Avoid premature removal of matrix band to prevent fracture of restoration
5. Defective Matrix Adaptation Post-Operative Failures:
- Postoperative pain – due to
- High points
- Zinc containing alloys
- Dissimilar restoration
- Thermal changes
Defective Matrix Adaptation Management:
- Use of zinc-free alloys to prevent delayed expansion
- Occlusal correction to reduce high points
- Avoid the use of dissimilar restoration to prevent galvanism
Amalgam Short Question and Answers
Question 1. Control of pain during cavity preparation.
Answer:
- The administration of local anesthesia to all tissues in the operating site is recommended in certain patients to eliminate pain and reduce salivation associated with tooth preparation and restoration
Factors Affecting Cavity Preparation
1. Patient Factors:
- Cardiovascular System
- Before administration of a drug, the condition of the cardiovascular system must be assessed
- Central Nervous And Respiratory Systems
- The central nervous system is affected by an overdose of injected anesthetic drugs
- Allergy
- Allergy is an absolute contraindication for administration of local anesthetic
Cavity Preparation Advantages:
- Patient cooperation
- Salivation control
- Hemostasis
- Operator efficiency
Cavity Preparation Technique:
- Before needle entry, the mucosa at the injection site should be wiped free of debris and saliva with sterile gauze
- After this, a lidocaine topical anesthetic ointment is applied for a minimum of 1-2 minutes to the selected entry site
- Lidocaine 2% with 1:100,000 epinephrine is commonly used in operative dentistry
- 1 ml provides infiltration anesthesia for 40-60 minutes for anterior teeth
- Painless injection is achieved by a combination of the following
- Use of topical anesthetic
- Use of sharp needle
- Slow deposition rate
Question 2. Mercuroscopic expansion.
Answer:
Mercuroscopic Expansion:
- Mercuroscopic expansion is proposed by Jorgensen
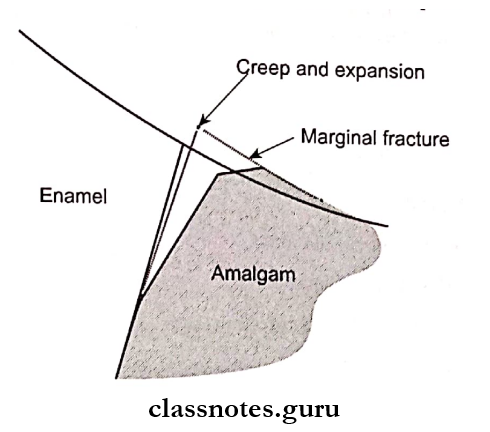
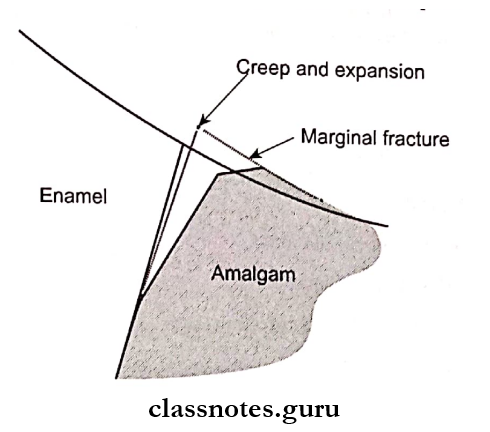
- It occurs due to electrochemical corrosion
- During this corrosion mercury from tin-mercury reacts with silver-tin particles and produces expansion
- Corrosion is due to the oxidation of the tin-mercury phase of amalgam leading to the formation of oxides and oxychlorides in tin
- The oxide precipitates as crystals and tends to fill up the spaces occupied by the original tin-mercury phase
- It can occur anywhere on or within a set amalgam
- This leads to extrusion at margins which has a greater prevalence of marginal fracture associated with occlusal amalgam
- Such expansion is known as macroscopic expansion
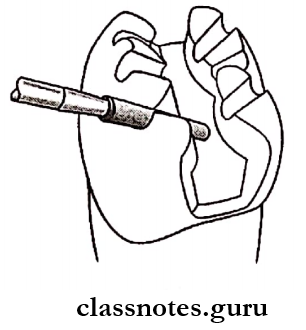
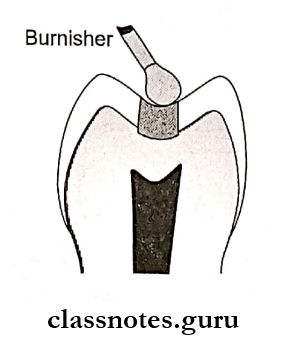
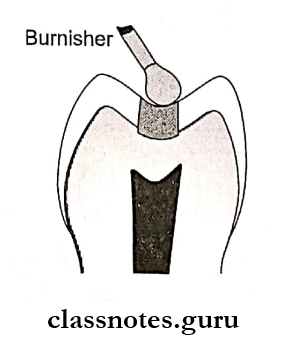
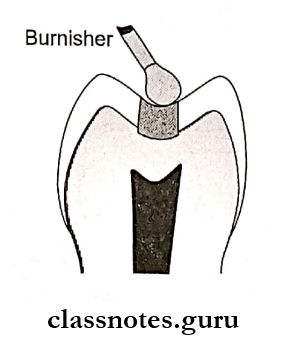
Question 3. Burnishing.
Answer:
Burnishing:
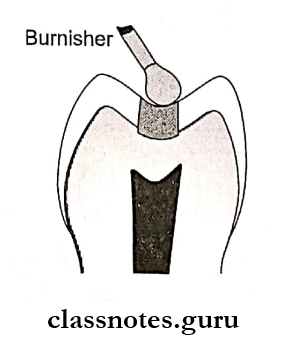
- Done after condensation
- To make the surface shiny
- Amalgam is overfilled and burnished immediately
Burnishing Types:
1. Pre-Carve Burnishing
- Reduce mercuric content
- Creates gross anatomy
- Done with a large burnisher
2. Post-Carve Burnishing
- Done after completion of the carving
- Done with a small-size burnisher
- To remove traces of carving
Question 4. Trituration and condensation of Amalgam.
Answer:
Trituration And Condensation Of Amalgam:
Trituration:
Trituration is the process of removal of the oxide layer from the alloy particles to coat each particle with mercury, resulting in a homogenous mass
Trituration Method:
- Manual
- Mechanical
Trituration Objectives:
- Result in workable mass
- Removal of the oxide layer
- Dissolution of alloy into mercury
- Reduces y1 and y2
Trituration Types:
- Normal – Homogenous mass
- Overtriturated – warm, shiny wet, and soft
- Under triturated – Dry, weak
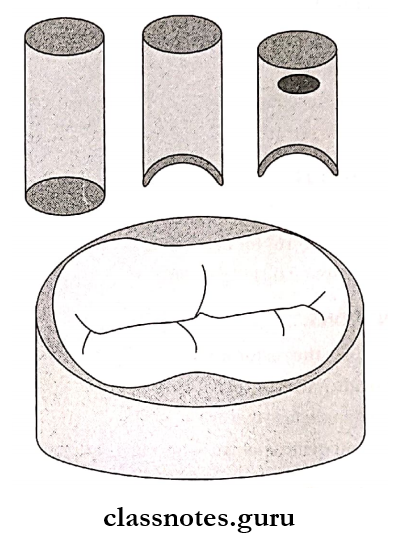
Trituration Condensation:
- Types Of Condensers
- Triangular
- Round
- Elliptical
- Trapezoidal
- Rectangular
- Rules:
- Done in increments
- Condense laterally and apically
- Have a constant supply of amalgam
- Apply adequate force
- Depends on the type of alloy
- Lathe cut alloy – Small condenser
- Blended alloy-Small condenser
- Spherical alloy-Large condenser
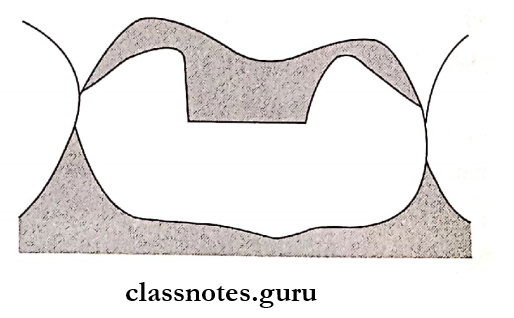
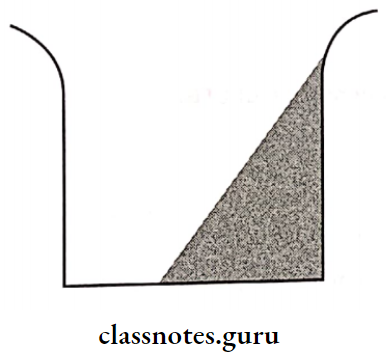
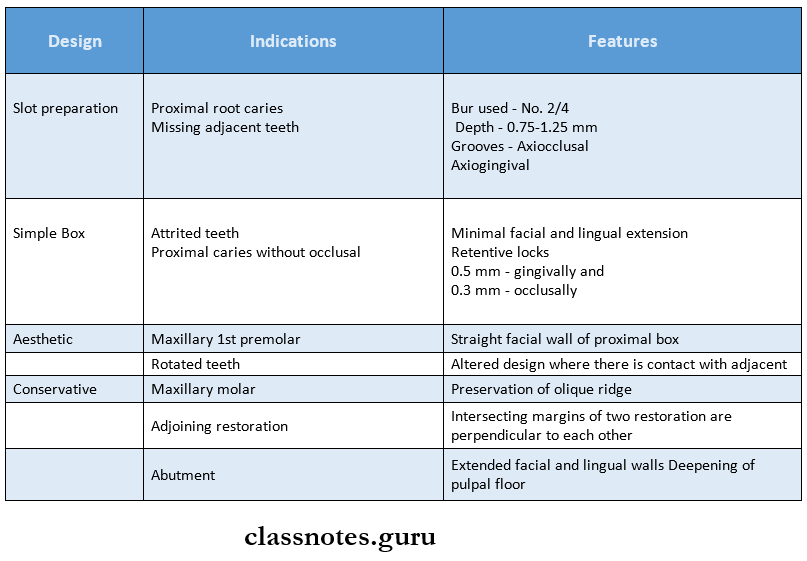
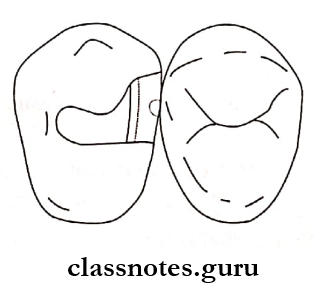
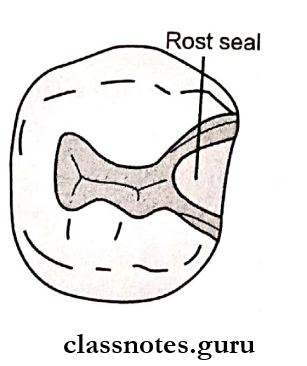
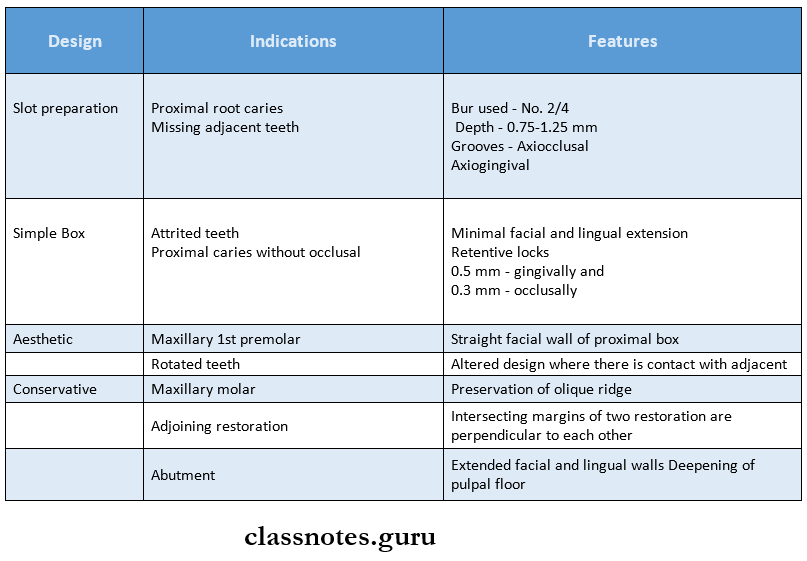
Question 5. Various cavity designs for Class 2.
Answer:
Various Cavity Designs For Class 2:
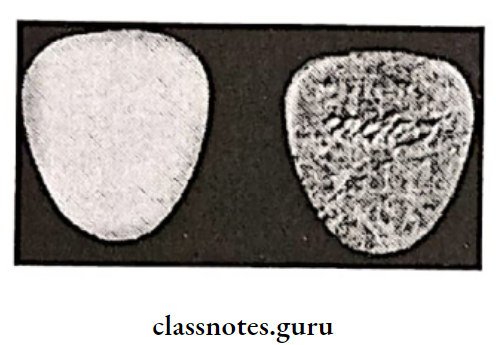
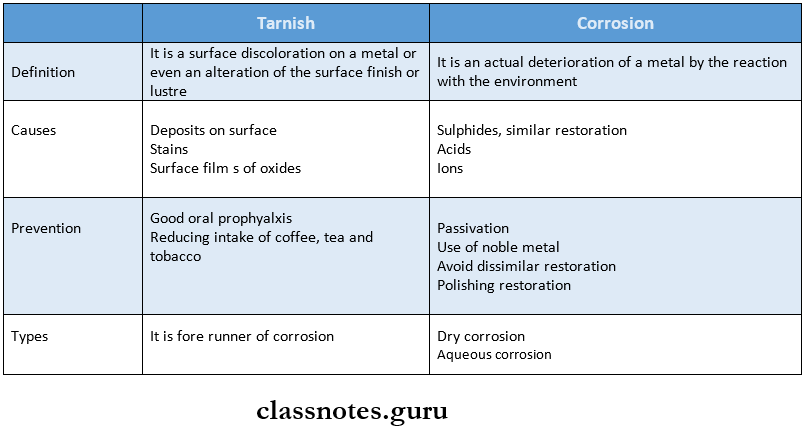
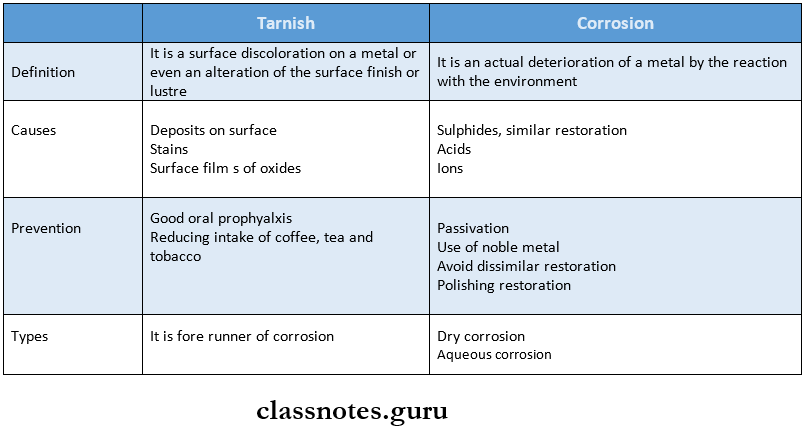
Question 6. Tarnish and Corrosion.
Answer:
Tarnish And Corrosion:
Question 7. Finishing and Polishing of Amalgam.
Answer:
Finishing And Polishing Of Amalgam:
- Involves the removal of marginal irregularities, obtaining proper contours, and smoothening the restoration
- Polishing creates a smooth, shiny luster on the surface of the amalgam
Finishing And Polishing Of Amalgam Time:
- After 24 hours of restoration
- Premature – Interferes with a crystalline structure
Finishing And Polishing Of Amalgam Advantages:
- Marginal adaptation
- Reduce tarnish and corrosion
- Plaque resistance
- Prevent recurrent caries
- Prevent occlusal problems
- Maintain periodontal health
Finishing And Polishing Of Amalgam Steps:
- Evaluate marginal integrity by explorer
- Evaluate occlusal pattern
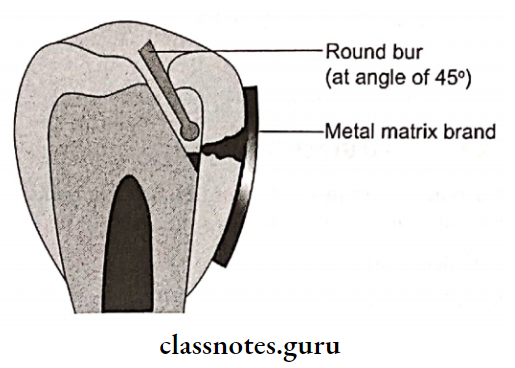
- Smoother margins by round bur
- Eliminate scratches by large round finishing bur
- Smoothen occlusal surface by side of burs
- Smoothen margins by finishing the strip
- Smoothen facial and lingual surfaces with a finishing disk
- Rinse and clean out debris
- Evaluate all margins and surfaces
Question 8. Mercury Hygiene.
Answer:
Mercury Hygiene:
- Follow aseptic technique
- Knowledge about mercury disposal and storage
- Use of proper ventilation
- Checking mercury levels periodically
- Avoid carpet/floor covering
- Storage of mercury in a closed container in an isolated area
- Use of pre-capsulated alloy
- Use of amalgamator
- Polishing, along with coolant
- Avoid direct contact with skin
- Use of evacuators
- Disposal in a closed plastic container
- Clean spilled mercury
- Remove protective clothing before leaving the operating area
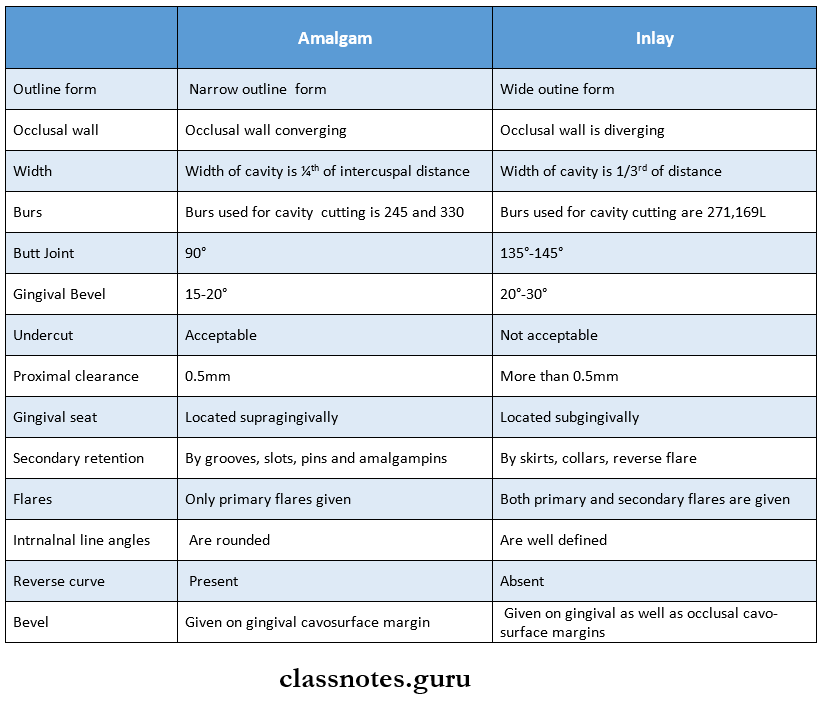
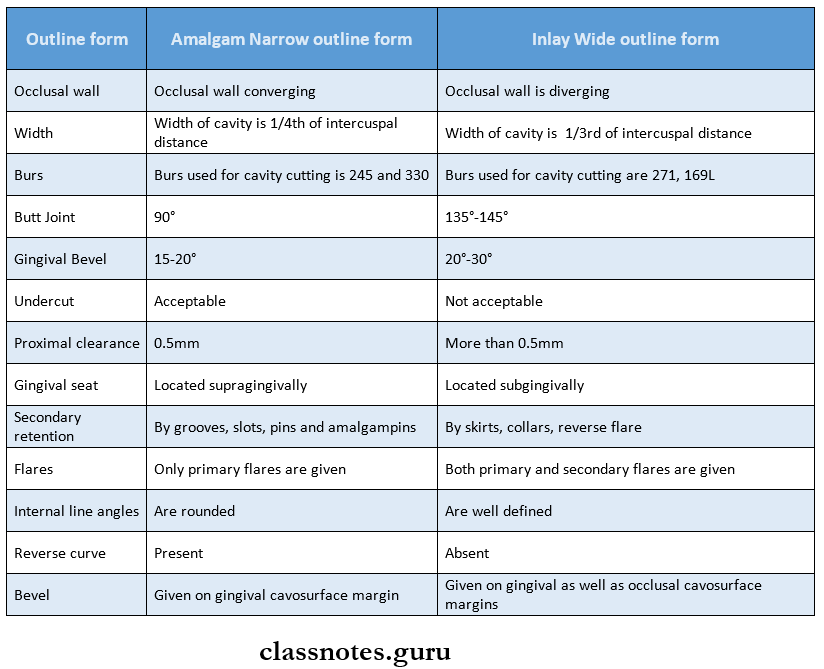
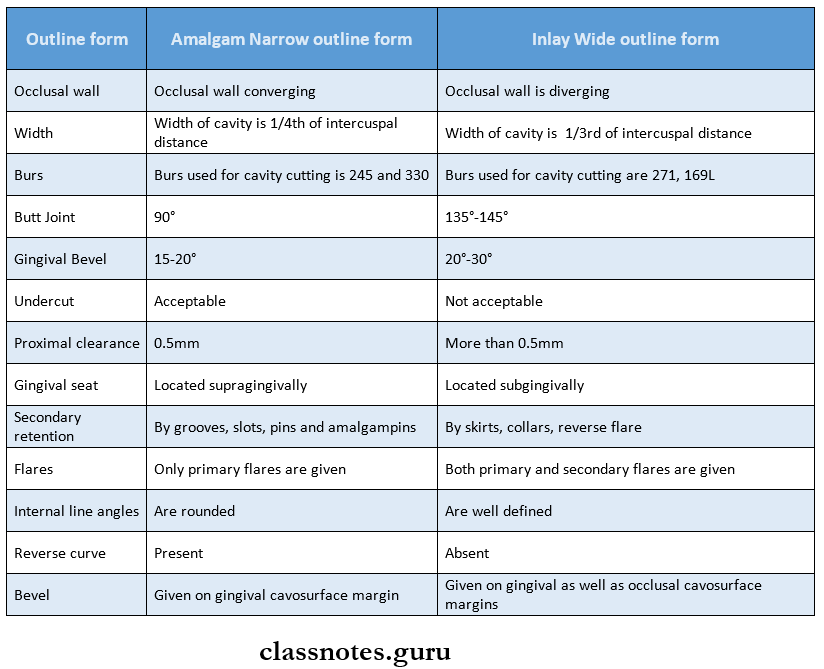
Question 9. Differences between amalgam and inlay cavity
Answer:
Differences BBetween Amalgam And Inlay Cavity
Question 10. Resistance form in cavity preparation
Answer:
Resistance Form In Cavity Preparation:
It may be defined as the shape and placement of the preparation walls that best enable the remaining tooth structure and the restoration to withstand, without fracture, masticatory forces delivered principally along the long axis of the tooth
Resistance Form In Cavity Preparation Features:
- Relatively horizontal floors
- Box-like shape
- Inclusion of weakened tooth structure
- Prevention of cusps and marginal ridges
- Rounded internal line angles
- The adequate thickness of restorative material
- Reduction of cusps for capping, when indicated
Amalgam Short Answers
Question 1. High copper alloy.
Answer:
High Copper Alloy:
- Contains more than 6% copper
High Copper Alloy Types:
- Admixed
- Single composition
High Copper Alloy Advantages:
- Elimination of weakest 72-phase
- Improved mechanical properties
- Corrosion resistance
- Better marginal integrity
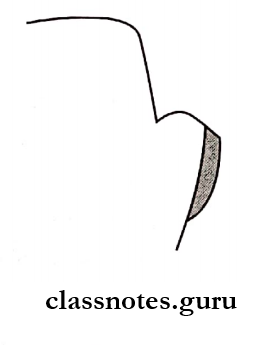
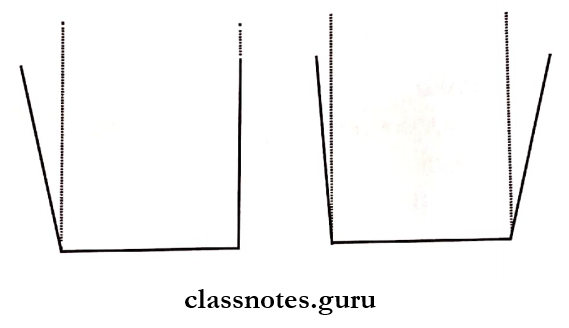
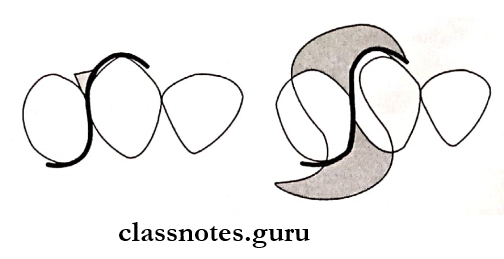
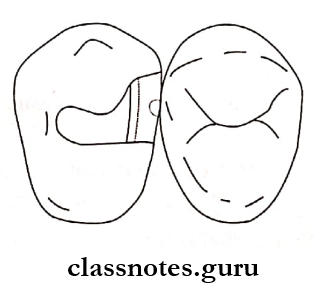
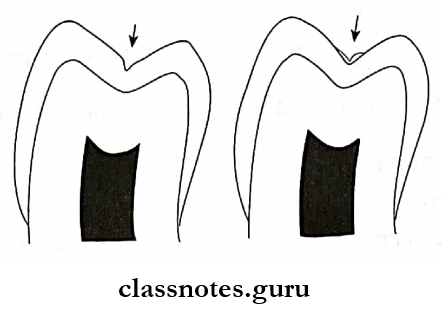
Question 2. Reverse Curve.
Answer:
Reverse Curve:
- Used in proximal preparation for class II amalgam restoration
- Indicated for broader contacts
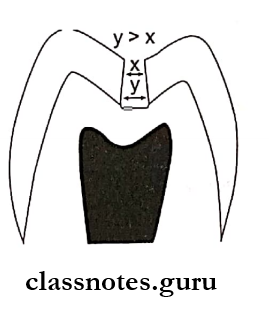
Reverse Curve Features:
- Curving proximal walls inwards towards the contact area
Reverse Curve Importance:
- Useful as if excessive flare is given it results in weakening of tooth structure and fracture of restoration
Reverse Curve Advantages:
- Conserves tooth structure
- Preserves marginal ridge
- Increases resistance for tooth and restoration
Question 3. Convenience form.
Answer:
Convenience Form:
Convenience Form is the form and shape of the cavity that enables ease of accessibility, visibility, and ease of operation
Convenience Form Features:
- Adequate extension
- Cavosurface margin
- Proximal clearance
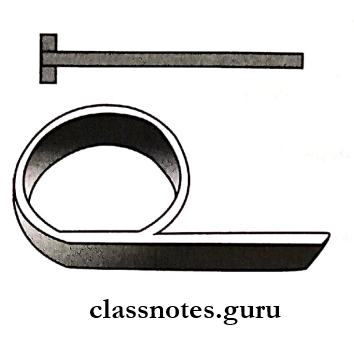
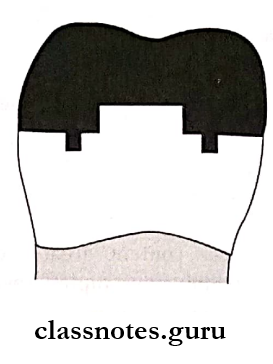
Question 4. Retention locks.
Answer:
Retention locks:
- Retention locks is a secondary retentive form for class 2 cavity preparation
- Used for amalgam restoration
- Placed in the proximal or occlusal box
- Prepared where sufficient vertical tooth preparation permits
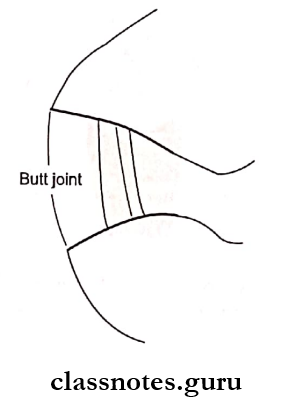
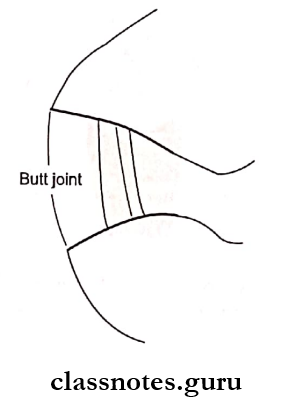
Question 5. Cavosurface angle /Butt joint.
Answer:
Cavosurface Angle:
- The Cavosurface Angle is an angle formed between the preparation wall and the external tooth surface
Cavosurface Angle Factors Effecting:
- Location of tooth
- Type of restorative material
- The direction of enamel rods
Cavosurface Angle Value:
- 90° for amalgam
- 110o-120o for cast
Cavosurface Angle Significance:
- If increased results in restoration fracture
- If decreased results in tooth fracture
Question 6. Delayed expansion.
Answer:
Delayed Expansion:
- If zinc-containing amalgam is contaminated by moisture during trituration or condensation a large expansion can take place
- Delayed expansion usually starts after 3-5 days and continues upto months reaching 400 pm
- This is called “delayed expansion”
- H2O + Zn → ZnO + H2 [gas]
- Effects of Liberated H2 Gas
Produce internal stresses
↓
Expansion of mass
↓
Increased creep
Increased microleakage
Pitted surface and corrosion
↓
Dental pain
Recurrence of caries
Fracture of restoration
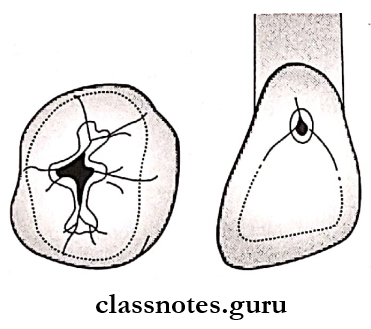
Question 7. Axio-pulpal line angle.
Answer:
Axio-Pulpal Line Angle:
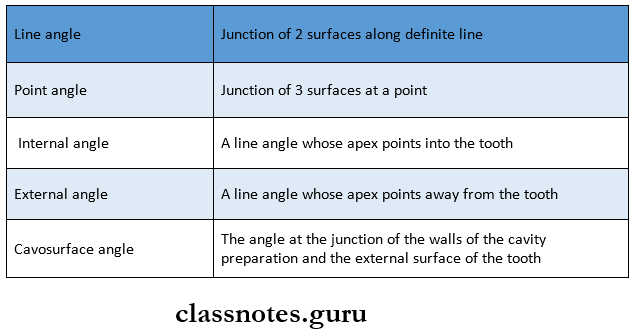
Line Angle:
Axio-Pulpal Line Angle:
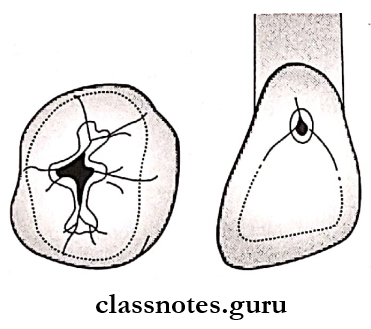
- The junction between the axial wall and pulpal floor
Axio-Pulpal Line Angle Significance:
- In amalgam restoration, there needs to be a curved axio-pulpal line angle
- Straight axio-pulpal line angle results in increased stress concentration over it leading to fracture
Question 8. Enameloplasty.
Answer:
Enameloplasty:
- Enameloplasty is the cauterization of the enamel surface
Enameloplasty Reason:
- In the case of a deep pit and fissure, the bristles of the toothbrush are unable to reach those areas
- By cauterization/enameloplasty these areas are converted to self-cleansable areas
Enameloplasty Features:
- Fissure present <l/3rd of enamel thickness
- Covering only a superficial portion of the enamel
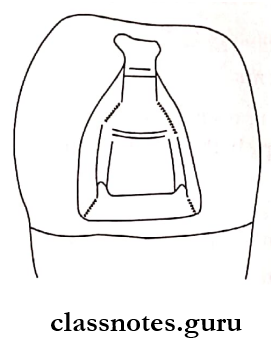
Question 9. Bonded Amalgam restoration.
Answer:
Bonded Amalgam Restoration:
Bonded Amalgam Restoration Mechanism:
Resin liner mixes with amalgam
↓
Forms micromechanical union
↓
Increases retention
↓
The liner acts between hydrophobic amalgam and hydro–Philip’sp tooth
Bonded Amalgam Restoration Indications:
- Weak preparation
- Extensive caries
- Deep bite
- Core foundation
Bonded Amalgam Restoration Advantages:
- Dentin sealing
- Increased resistance
- Increased retention
- Conserve tooth structure
- Improved marginal seal
- Cost-effective
Question 10. Mulling.
Answer:
Mulling:
- Continuation of trituration
- Coat all alloy particles with mercury
Mulling Methods:
- Manually squeezing amalgam in chamois skin
- Mechanical – By increased trituration for 1-2 sec.
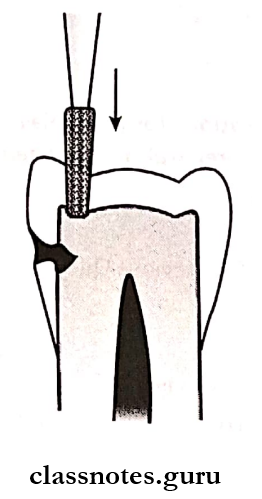
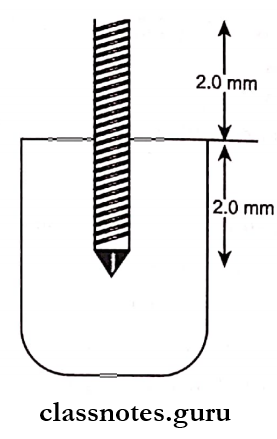
Question 11. Amalgampins.
Answer:
Amalgampins:
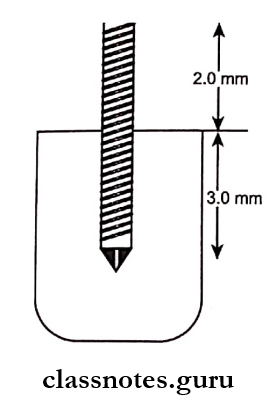
- Vertical posts of amalgam in dentin
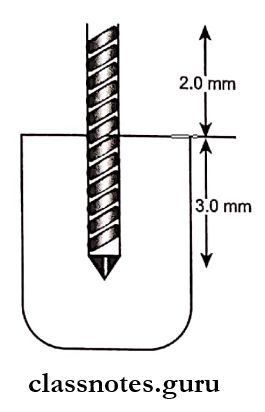
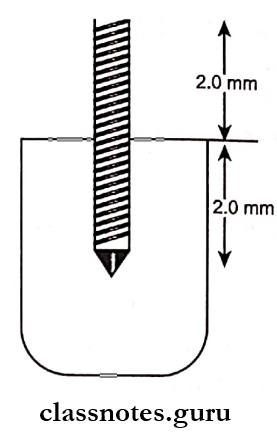
Amalgampins Dimensions:
- Depth on the gingival floor – 1-2 mm
- Width – 0.5 -1 mm
Amalgampins Advantages: Increases resistance and retention
Question 12. Disposal of scrap amalgam.
Answer:
Disposal Of Scrap Amalgam:
- Store all scrap amalgam in a tightly closed container either dry or under a radiographic fixer solution
- Amalgam scrap should not be stored in water
- If the scrap is stored dry, mercury vapor can escape into room air when the container is opened
- If the scrap is stored under a radiographic fixer solution, special disposal of the fixer may be necessary
- Dispose of mercury-contaminated items in sealed bags according to applicable regulations
- Do not dispose of mercury-contaminated items in regulated waste containers or bags or along with waste that will be incinerated
- Clean up spilled mercury properly using trap bottles, tape, or freshly mixed amalgam to pick up droplets and commercial cleanup kits
- Do not use a household cleaner
Question 13. Mercury hygiene
Answer:
Mercury Hygiene:
- Follow aseptic technique
- Knowledge about mercury disposal and storage
- Use of proper ventilation
- Checking mercury levels periodically
- Avoid carpet/floor covering
- Storage of mercury in a closed container in isolated areas of pre-capsulated alloy
- Use of amalgamator
- Polishing, along with coolant
- Avoid direct contact with skin
- Use of evacuators
- Disposal in a closed plastic container
- Clean spilled mercury
- Remove protective clothing before leaving the operating area
Amalgam Viva Voce
- Increasing copper content greater than 12% by weight in amalgam alloy suppresses the formation of more corrosive gamma-2 phase
- High copper amalgamate is more corrosion-resistant than low copper amalgam
- Mercury: alloy ratio in Eames technique is 1:1
- Use of zinc-containing alloys results in delayed expansion
- Tin-mercury gamma-2 phase is the weakest in dental amalgam
- The threshold limit value for exposure to mercury va¬pour for a 40-hour work week is 50pg/m3