Impression And Mouth Preparation Short Answers
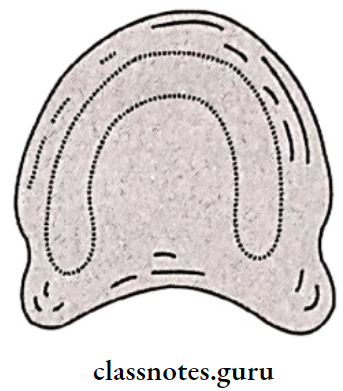
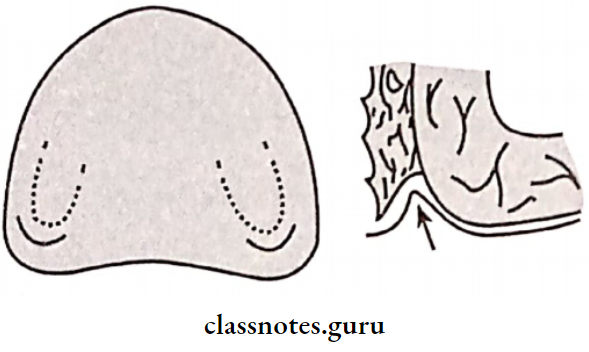
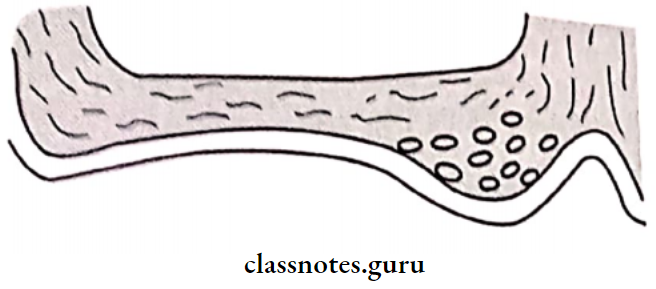
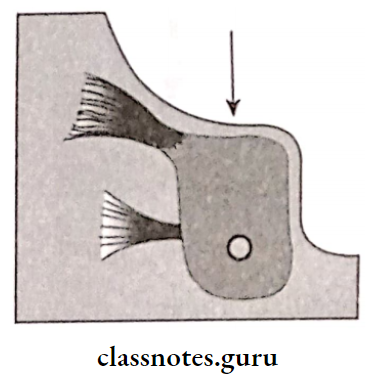
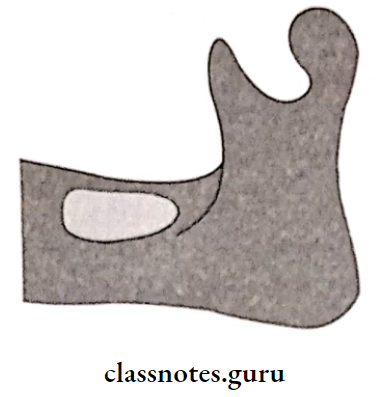
Question 1. Buccal shelf area
Answer:
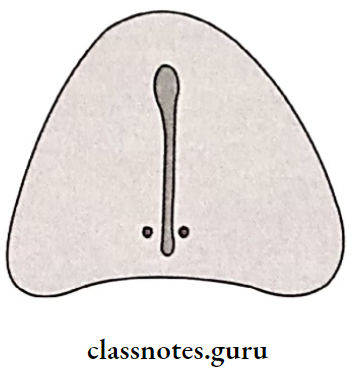
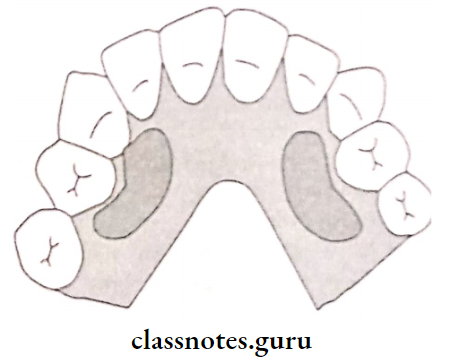
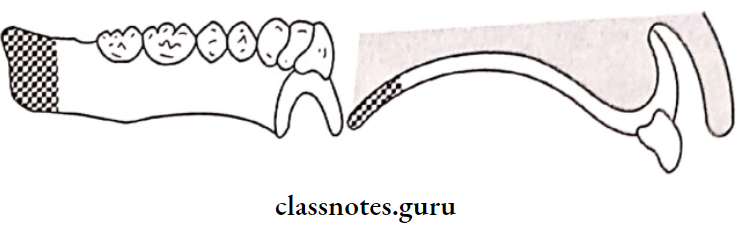
Area Of Buccal Shelf :
Between the buccal frenum and the anterior border of the masseter
Boundaries of Buccal Shelf :
- Medial crest of the ridge
- Distal Retromolar pad
- Lateral external oblique ridge
Significance Of Buccal Shelf :
- Primary stress-bearing area of the mandible
- The width of it increases as resorption continues
Read And Learn More: Prosthodontics Question And Answers
Impression and Mouth Preparation in Complete Dentures
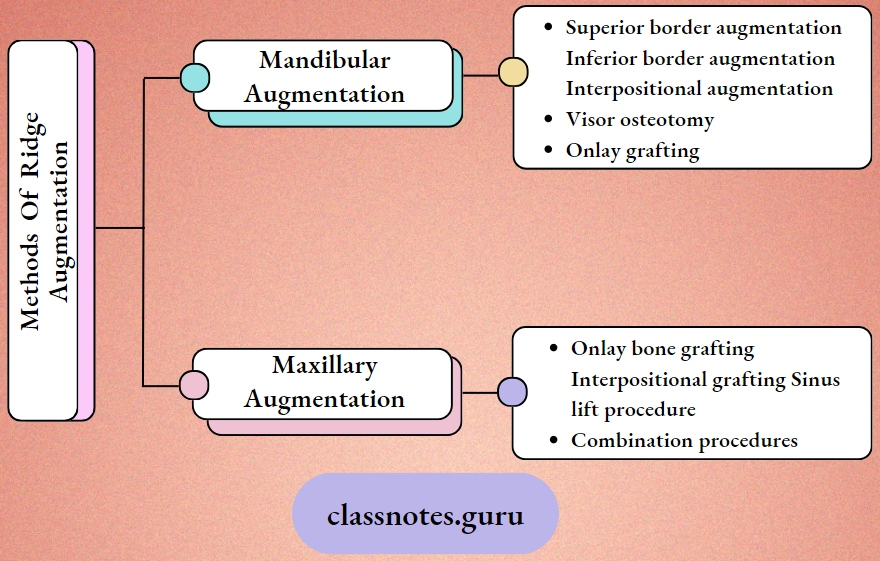
Question 2. Ridge Augmentation
Answer:
Ridge Augmentation Definition:
Any procedure designed to enlarge or increase the size, extent, or quality of a deformed residual ridge is referred to be ridge augmentation procedures
Question 3. “Cohesion” in complete dentures.
Answer:
- Cohesion is the physical attraction of like molecules to each other
- Acts within the film of saliva
- Normal quality and adequate quantity of saliva are cohesive
- When the quantity of saliva is excessive and the quality is watery, cohesion is decreased
- When the quantity of saliva is decreased and its viscosity is increased, cohesion is decreased due to an increase in the thickness of saliva
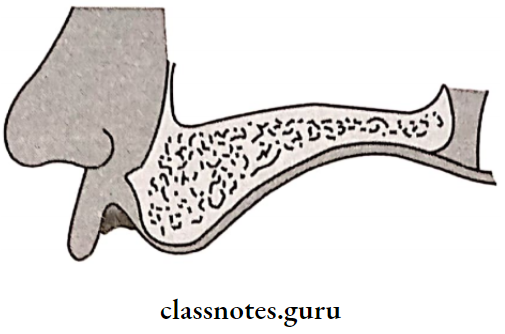
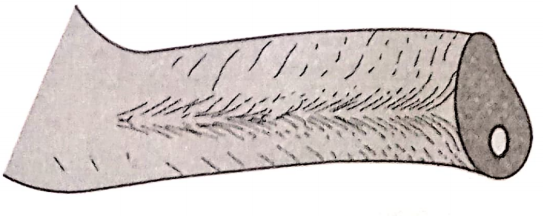
Question 4. Mylohyoid ridge importance
Answer:
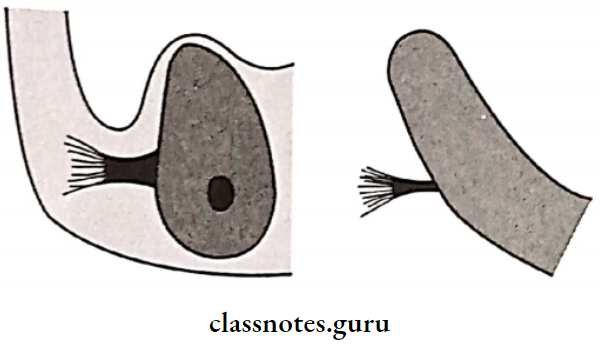
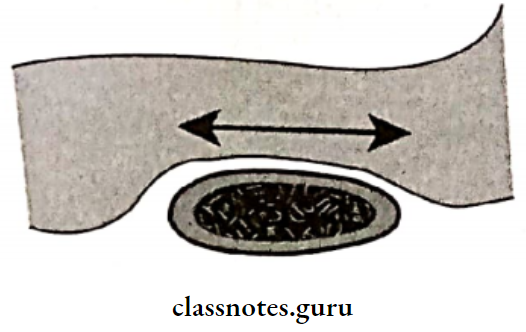
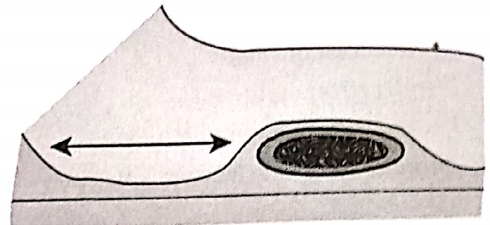
- The mylohyoid Ridge is a rough bony crest extending from the third molar to the second bicuspid region
- The mylohyoid muscle is attached to the mylohyoid ridge
- In the anterior region, the mylohyoid ridge with attached mylohyoid muscle lies close to the inferior border of the mandible
- Posteriorly, it is superior in position and the lingual flange of the denture may extend below the mylohyoid ridge if it drops vertically or slopes at 45 degrees towards the tongue
Short Questions on Mouth Preparation and Impressions
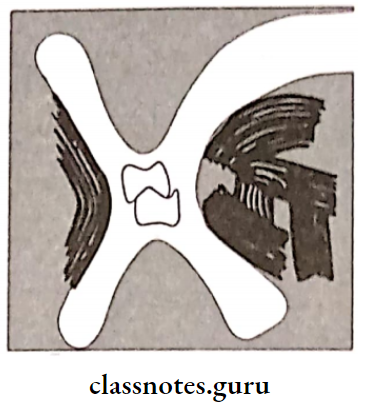
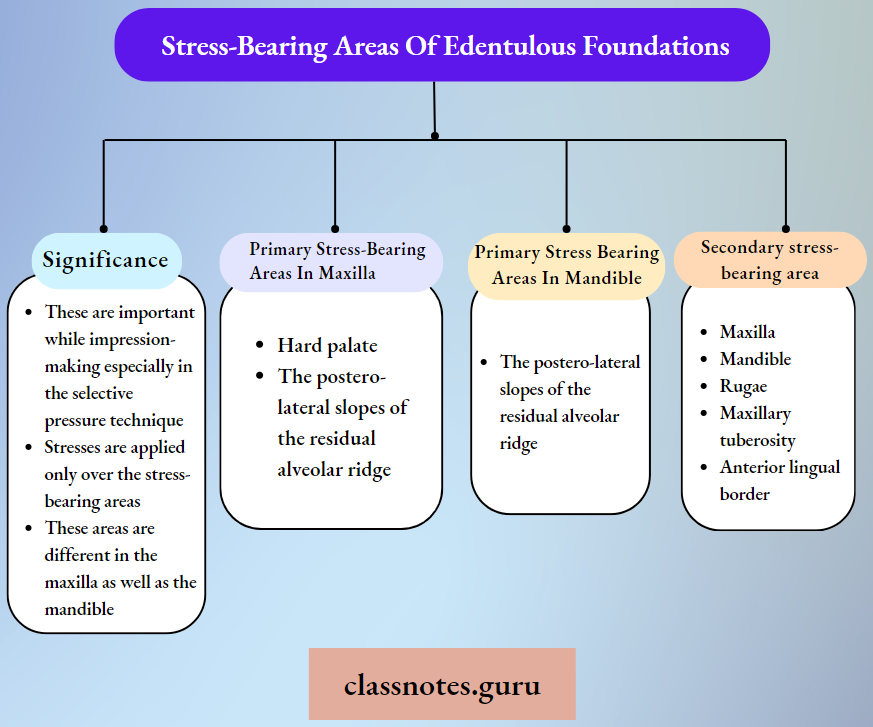
Question 5. Stress-bearing areas of edentulous foundations
Answer:
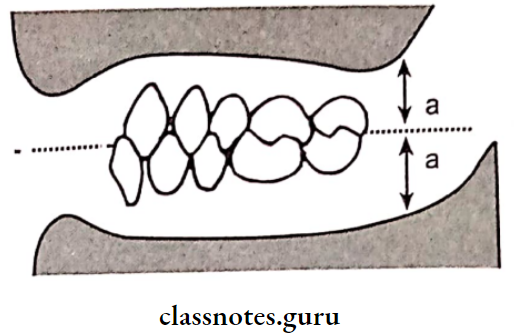
These are those areas where stresses are directed at are right angle
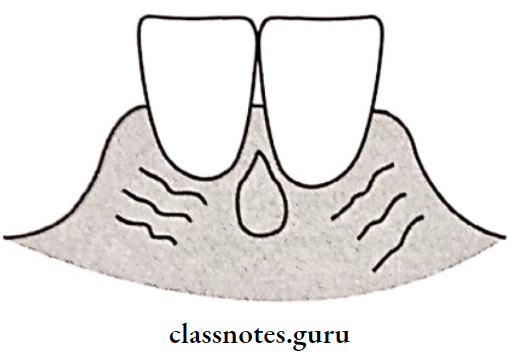
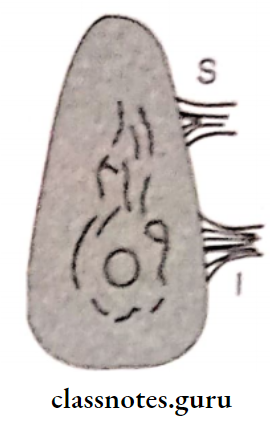
Question 6. Retromolar papilla
Answer:
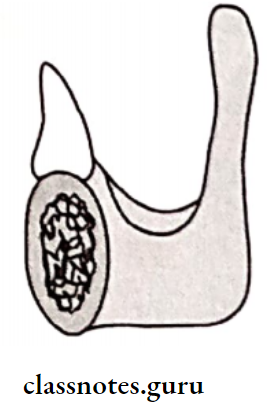
- Retromolar Papilla is described as a pear-shaped papilla. It is a small elevation
- Retromolar Papilla is a residual scar formed after the extraction of the third molar
- Retromolar Papilla lies along the line of the ridge
- The denture should terminate at the distal end of the pear-shaped papilla
- Being in this area improves retention
Question 7. Objectives of complete denture impressions
Answer:
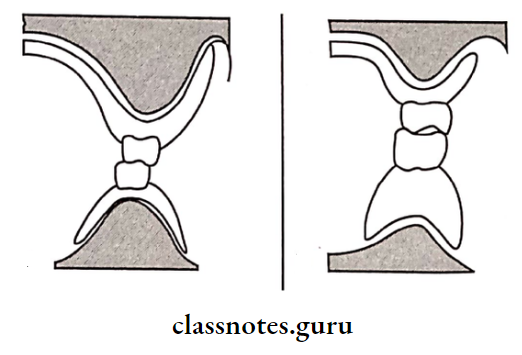
- Retention: It is the resistance to displacement away from the tissue surface. It is a mucosa-borne phenomenon.
- Support: It is the resistance to the occlusal forces in the vertical direction. It is a bone-borne phenomenon.
- Stability: It is resistant to lateral shifting.
- Preservation of remaining structures.
BDS Prosthodontics Viva on Impressions
Question 8. Diagnostic casts.
Answer:
Diagnostic Casts Requirements:
- Diagnostic Casts Should Be:
- Free of voids
- Smooth surface
- Provide good denture support
- Walls should be tapering outward
- Smooth tongue space
- Free of moisture
- The occlusal table is parallel to the floor.
Diagnostic Casts Uses:
- Measure the undercuts. Determine the path of insertion
- Treatment planning
- Perform mock surgery, evaluate the arch
- Assess retention & stability
- Determine secondary retentive forms
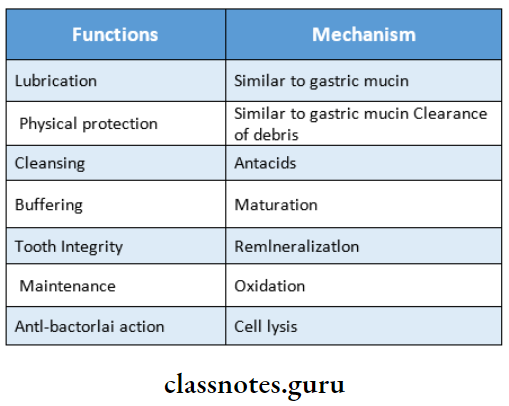
Question 9. Saliva’s influence on denture retention & stability.
Answer:
- Thick and ropy saliva, loss of retention
- Thin and watery saliva compromised retention
- Watery serous saliva is more retentive
- In xerostomia there is no adhesion
- Ptyalism leads to gagging
- Xerostomia: Soreness and irritation
Question 10. Retention in the maxilla
Answer:
Retention factors present in the maxilla are
- Large denture-bearing area
- Thick and ropy saliva
- Interfacial surface tension
Impression Techniques in Complete Dentures
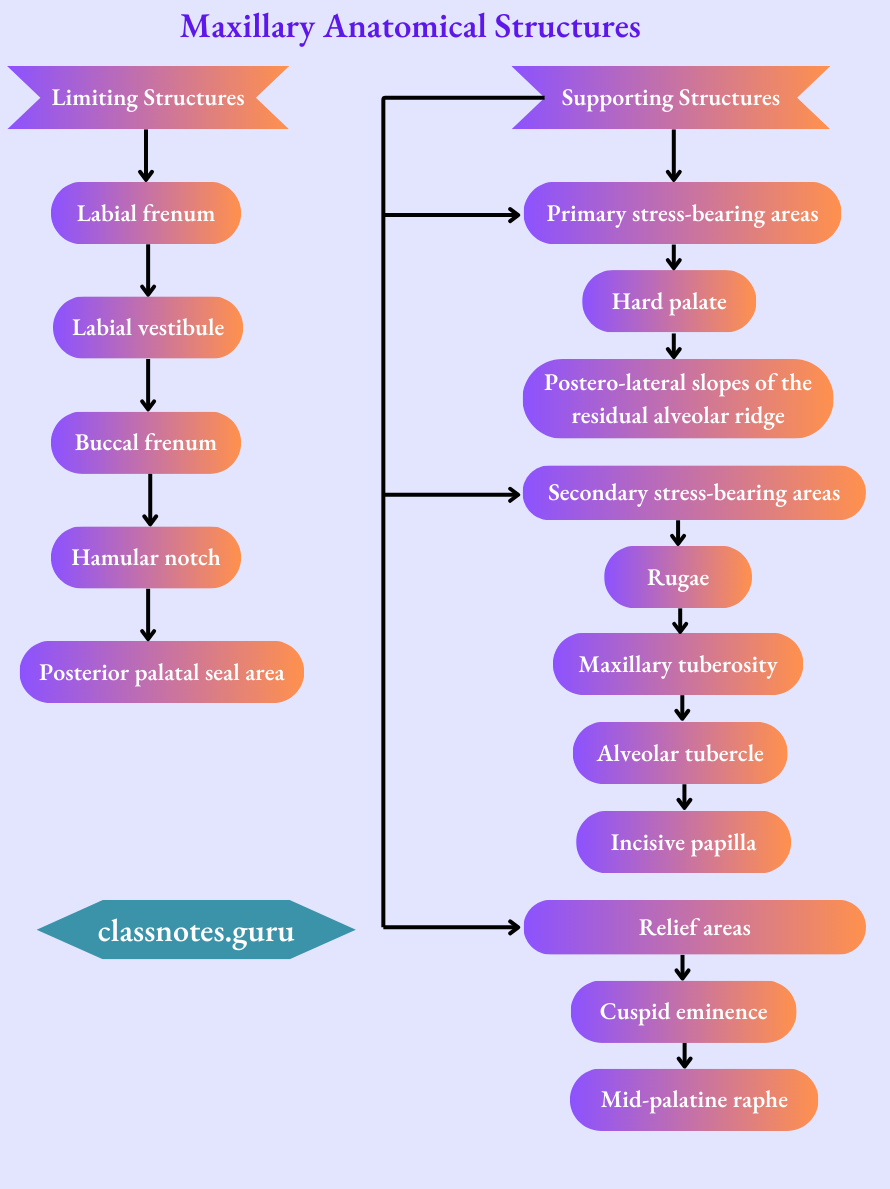
Question 11. Maxillary anatomical structures
Answer:
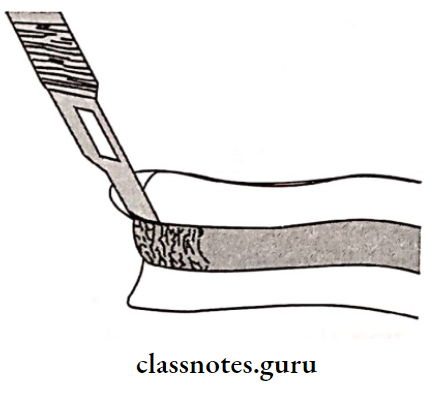
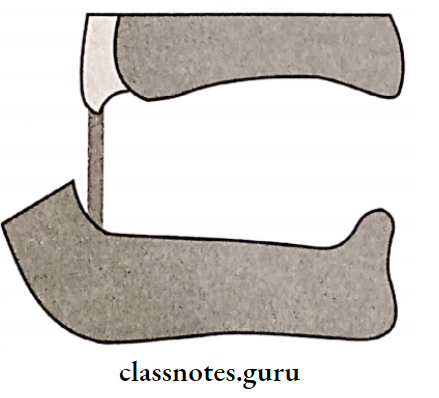
Question 13. Final impression methods in complete denture
Answer:
- Dry gauze is placed on the floor of the mouth to remove the saliva
- It is removed just before making an impression
- Impression material is manipulated and loaded onto the tray
- The tray is rotated in the horizontal plane and inserted into the mouth using the anterior handle
- The tray is seated completely by applying alternating pressure over the posterior handles
- The patient is asked to touch his upper lip with his tongue
- Passive movements are performed
- After the material gets set and examined for any defects
Question 14. Realeff effect
Answer:
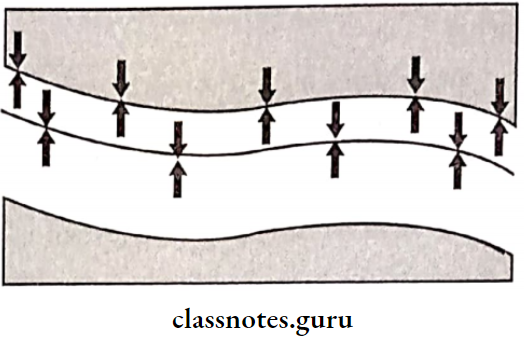
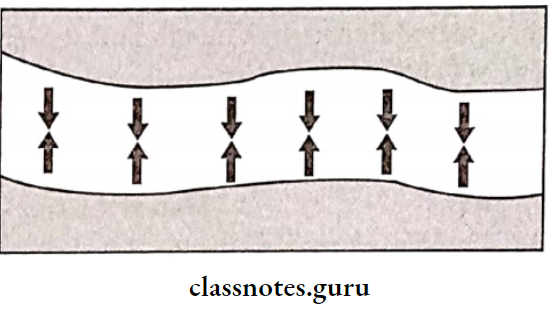
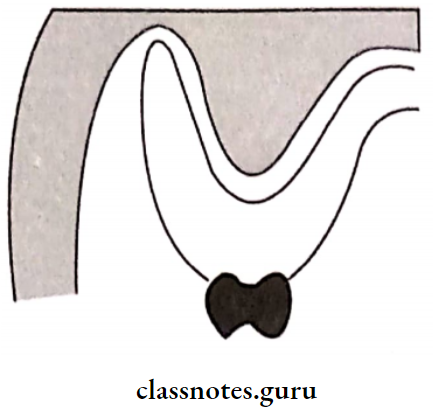
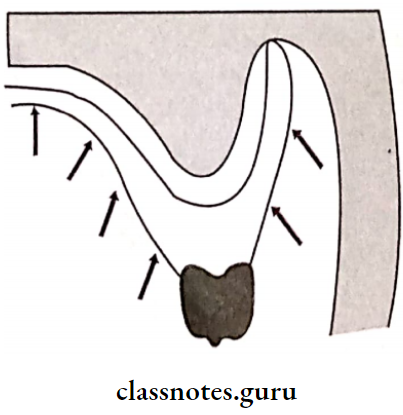
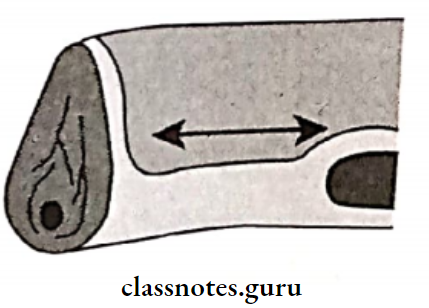
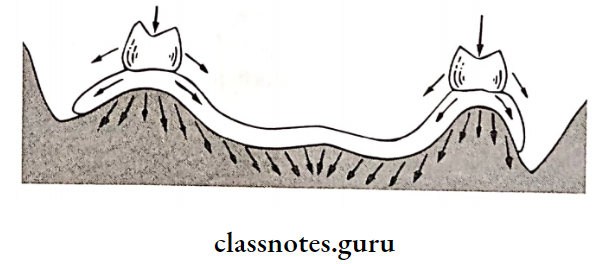
Complete dentures rest on the basal seat area, which is primarily the oral mucosa and the residual alveolar ridge
- The oral mucosa is displaceable and compressibl.e Hanau described this factor as “resiliency and like effect”- Realeff effect
- It plays an important role in all steps of complete denture fabricate,on as in
- Primary impression
- Border moulding
- Final impression
- Jaw relation
- Try in
- Remount
- Follow up
- Mechanical or pathological reasons cause fibrous changes in the residual ridge, making it resilient
- It is more commonly seen in Mandibular residual ridges
- Maxillary anterior ridges
Factors Affecting the Real Effect
- Consistency of mucosa
- Excess bone loss during extraction
- A person’s general health
- Elderly tissues
- Smaller forces produce distinct compression
- Parafunctional habits
- Single complete denture
Question 15. Materials used for the master impression.
Answer:
Master Impression Requirements:
- Low viscosity
- Form a thin layer of impression.
- Should be uniform
Master Impression Materials Used:
- Zinc oxide eugenol paste impression
- Medium-bodied elastomeric impression materials
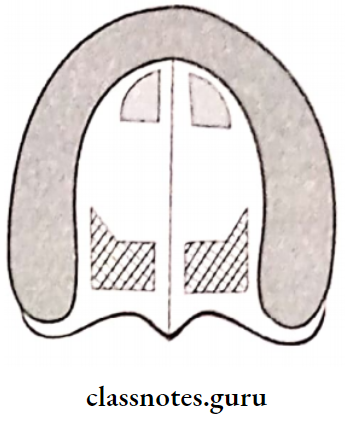
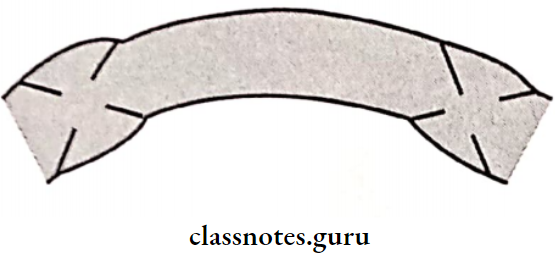
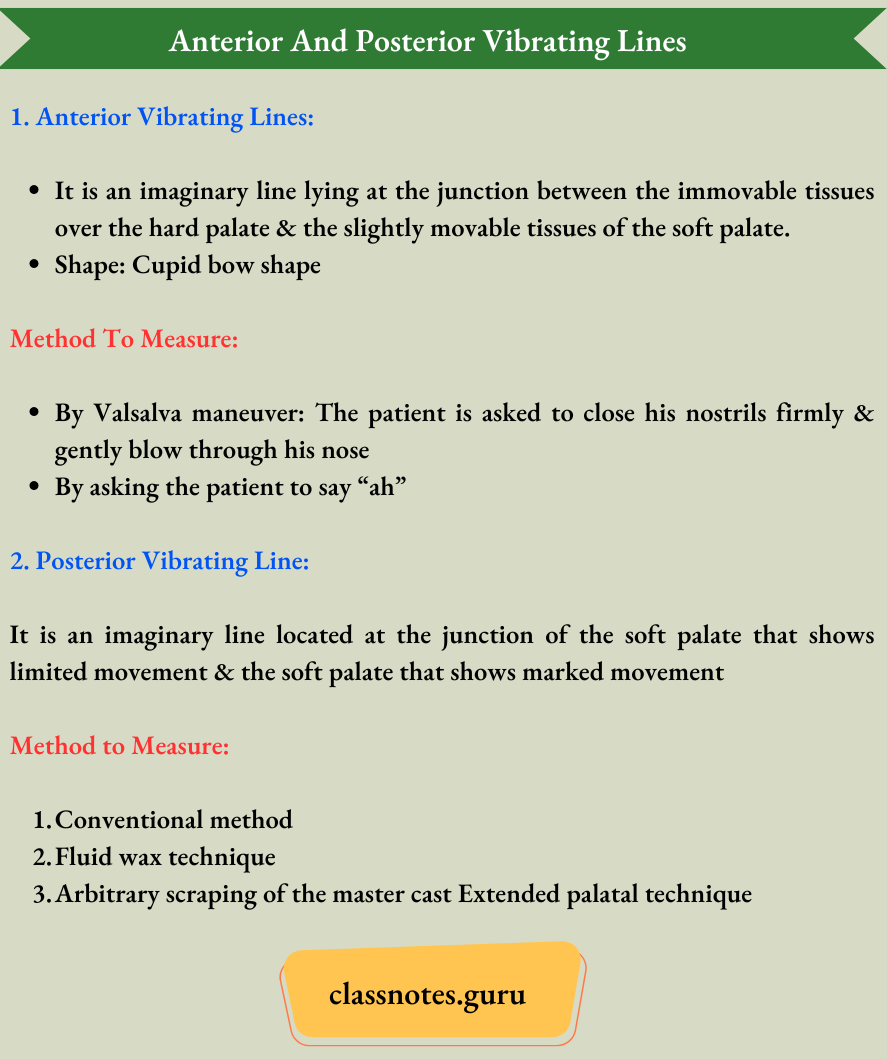
Question 16. Anterior and posterior vibrating lines.
Answer:
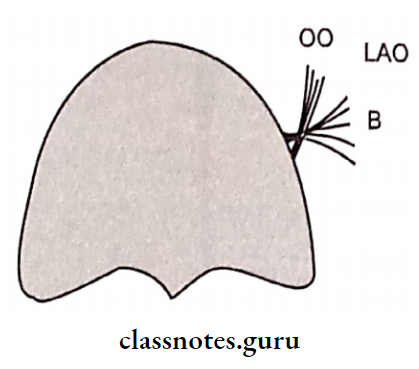
Question 17. Modiolus.
Answer:
The modiolus is a point where 8 muscles meet at the angle of the mouth
Modiolus Are:
- Depressor anguli oris
- Levator anguli oris
- Risorius
- Orbicularis oris
- Buccinator
- Zygomatic major
- Quadralus labii superioris
- Quadralus labii inferioris
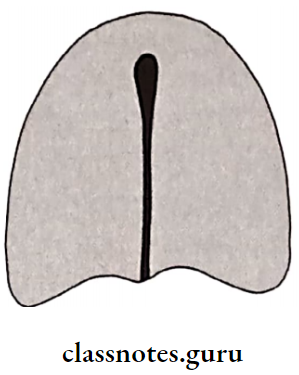
Question 18. Hamular notch.
Answer:
- The Hamular Notch is the depression situated between the maxillary tuberosity and the hamulus of the medial pterygoid plate. It is a soft area of loose connective tissue
- The tissues in this area can be safely displaced to achieve the posterior palatal seal
- The distolateral border of the denture base rests in the hamular notch
Hamular Notch Significance:
- The denture border should extend to the hamular notch
- If the border is located anteriorly near the maxillary tuberosity, the denture will not have retentive properties, as the denture will lie on non-resilient tissues in such cases
Complete Denture Pre-Prosthetic Steps
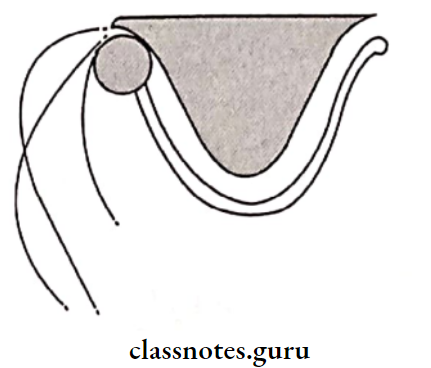
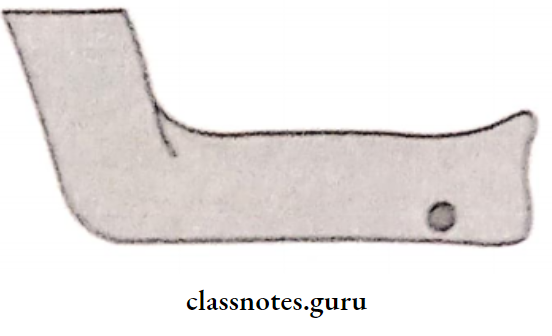
Question 19. Retromylohyoid fossa.
Answer:
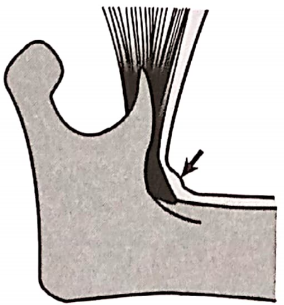
- The Retromylohyoid Fossa belongs to the posterior part of the alveolar lingual sulcus
- Retromy lohyoid Fossa lies posterior to the mylohyoid muscle
Retromylohyoid Fossa Boundaries:
- Anteriorly retro mylohyoid curtain
- Posterolaterally superior constrictor of the pharynx
- Posteromedially palatoglossus and the lateral surface of the tongue
- Inferiorly sub mandibular gland
Question 20. Syneresis and imbibition.
Answer:
- The process of water sorption by hydrocolloids is known as imbibition
- Syneresis is a process where the gel may lose water by exudation of fluid
- Syneresis & imbibition can result in dimensional changes & therefore inaccurate casts
- To avoid this, hydrocolloids should be poured immediately
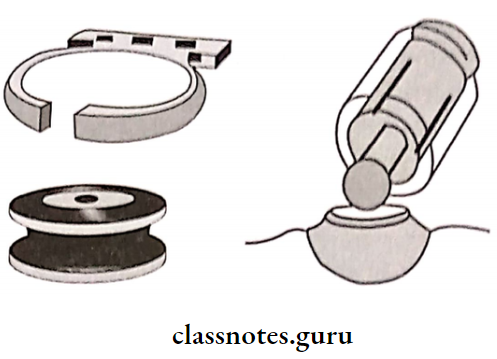
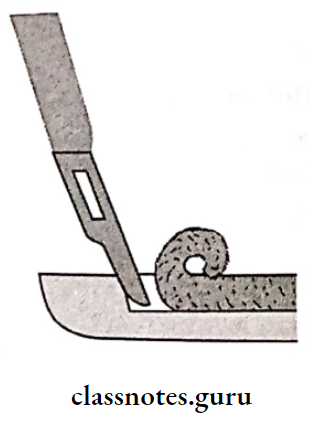
Question 21. Advantages of the perforated stock tray.
Answer:
- Perforated Stock Tray is used for impression materials like alginate
- Holes present in it are advantageous
- Perforated Stock Tray helps in retaining the material while impression-making
- Perforated Stock Tray retains the material by mechanical interlocking