Dental Caries Important Notes
- Dental Caries – It is an irreversible microbial disease of the calcified tissues of the teeth, characterized by demineralization of the inorganic part and destruction of the organic substance of the tooth which often leads to cavitation
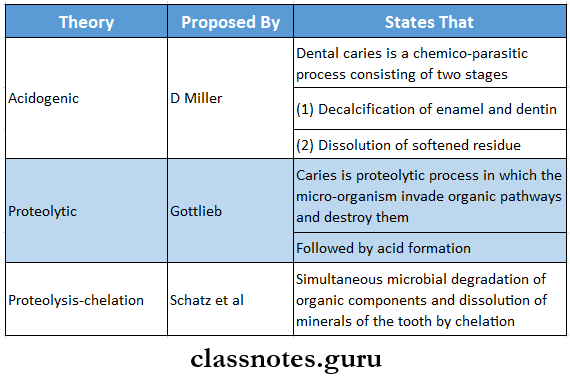
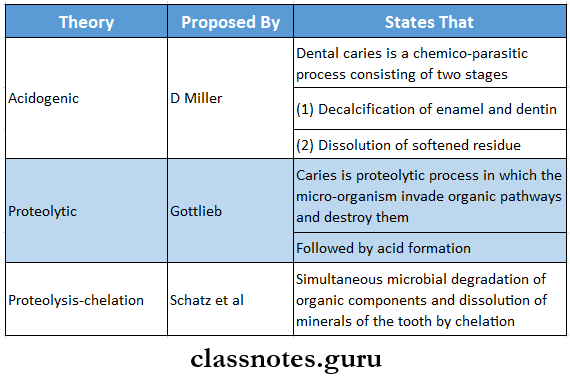
- Caries Theory Regarding Etiology
- Classification Of Caries:
- Based on the anatomical site
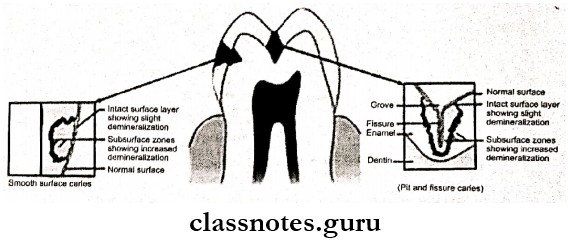
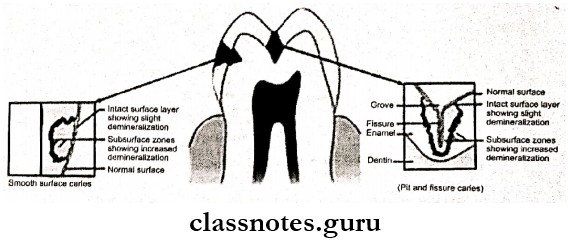
- Pit and fissure caries develops on
- Occlusal surfaces of molars and premolar
- Buccal and lingual surfaces of molar
- Palatal surfaces of maxillary incisor
- Smooth surface caries
- Proximal surfaces of teeth or
- On the gingival third of buccal and lingual surfaces
- Cervical caries
- Extends from the area opposite to the gingival crest occlusal to the convexity of the tooth surface
- Root caries
- Found anywhere on root surfaces
- Based on severity and rate of progression
- Acute caries
- Runs rapidly and results in early pulp involvement
- Chronic caries
- Progresses slowly and involves pulp much later
- Other
- Rampant caries
- Characterised by sudden, severe destruction of teeth affecting surfaces that are relatively caries-free
- Nursing caries
- Affects deciduous dentition due to prolonged use of nursing bottles containing milk or milk formula
- Caries Activity Tests
- Lactobacillus colony test
- Snyder test
- Swab test
- Buffer capacity test
- Salivary reductase test
- Salivary s.mutans level test
- Dip slide test
- Caries Vaccine
- Caries Vaccine is a suspension of an attenuated or killed micro-organism administered for the prevention, amelioration, or treatment of infectious diseases
Route Of Administration
- Oral route
- Increases stimulation of IgA antibodies
- Systemic route
- Subcutaneous administration of s.mutans leads to an increase in IgG, IgM, and IgA antibodies
- Active gingivosalivary route
- Localizes the immune response by using gingival crevicular fluid as a route
- Active immunization
- Synthetic peptides
- Derived from glucosyl transferase enzyme Coupling with cholera toxin subunits
- Coupling of the protein with a nontoxic unit of cholera toxin suppresses colonization of S. mutans
- Fusing with avirulent strains of salmonella
- Liposomes- increases IgA antibodies
- Passive immunization
- External supplements are included
- Bovine milk and whey
- Egg yolk
- Transgenic plants
Dental Caries Long Essays
Question 1. Define and classify dental caries. Describe clinical and histopathologic features of dentinal caries.
Answer:
Dental Caries Definition:
- Dental caries is an infectious, microbiologic disease of the teeth that results in localized dissolution and destruction of the calcified tissues of the teeth
- Dental Caries leads to weakening of tooth structure, cavity formation, and eventual loss of tooth
Dental Caries Classification:
- Based on occurrence
- Primary caries- affects the intact surface
- Secondary caries- Occurs around margins of restoration
- Based on the anatomical site
- Pit and fissure caries
- Smooth surface caries
- Linear enamel caries
- Cervical caries
- Root caries
- Based on the rate of progression
- Acute caries
- Chronic caries
- Rampant caries
- Nursing bottle caries
- Recurrent caries
- Arrested caries
- Incipient caries
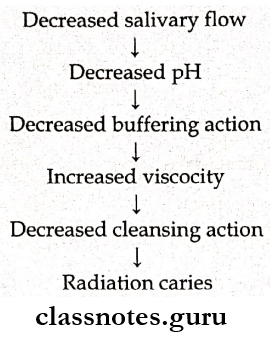
- Radiation caries
Dental Caries Clinical Features:
- Dental Caries occur on pit and fissures/smooth surfaces and roots of teeth
- Initially brown or black in color
- Soft and examined through a catch by tip of the explorer
- The enamel bordering it appears opaque bluish-white
- Due to undermining enamel, caries spreads laterally at DEJ
Histopathologic Features Zones in Dentinal Carles:
- Zone 1- Normal dentin
- Zone of fatty degeneration of odontoblast process
- Represents the innermost layer of carious dentin
- No crystals are present in the lumen of tubules
- No bacteria present in tubules
- Intertubular dentin has normal collagen
- Zone 2- Sub-transparent dentin
- Zone of dentinal sclerosis characterized by deposition of calcium sails in dentinal tubules
- The superficial layer shows areas of demineralization and damage to odontoblastic processes
- It is capable of remineralization
- No bacteria is present in tubules
- Zone 3- Transparent dentin
- Zone of decalcification of dentin, a narrow zone preceding bacterial invasion
- It is softer than normal dentin
- Large crystals are present within the lumen of dentinal tubules
- No bacteria is present in tubules
- It is capable of self-repair and remineralization
- Zone 4- Turbid dentin
- Zone of bacterial invasion of decalcified but intact dentin
- Widening and distortion of dentinal tubules
- Cannot undergo self-repair or remineralization
- Must be removed before restorative treatment
- Zone 5- Infected dentin
- Zone of decomposed dentin
- Infected is the outermost zone of carious dentin
- Characterised by the complete destruction of dentinal tubules
- Areas of decomposition of dentin occur along the direction of dentinal tubules called liquefaction foci of Miller
- Transverse clefts are seen due to the decomposition of dentin
- Bacteria invade and destroy peri and intertubular dentin.
Question 2. Write about the theories of dental caries.
Answer:
Theories Of Dental Caries:
- Acidogenic theory
- Postulated by WD Miller in 1889
- Dental Caries states that
- Acids formed due to the fermentation of dietary carbohydrates by oral bacteria lead to progressive decalcification of the tooth structures with subsequent disintegration of organic matrix
- Dental Caries states that process of dental caries involves two stages
- Initial stage
- Acid production due to fermentation of carbohydrates by plaque bacteria
- Late stage
- Decalcification of enamel followed by dentin by acids
- This causes total destruction of enamel and dentin
- According to Miller, the process of caries involves four factors
- Dietary carbohydrates
- Micro-organisms
- Acids
- Dental plaque
- Proteolytic Chelation Theory
- Proteolytic Chelation Theory states that there is simultaneous microbial degradation of the organic components and the dissolution of the minerals of the tooth by the process known as chelation
- The chelating agent is negatively charged
- Proteolytic Chelation Theory releases the positively charged calcium ions from the enamel or dentin
- Sucrose chelation theory
- Sucrose chelation theory proposes the sucrose itself and not the acid derived from it can cause the dissolution of enamel by forming ionized calcium saccharate
- Autoimmune theory
- Autoimmune theory suggests that few odontoblast cells at some specific sites within pulp are damaged by an autoimmune mechanism
Read And Learn More: Oral Pathology Question And Answers
Question 3. Discuss the role of carbohydrates in caries. Describe and histopathologic features of enamel caries
Answer:
Role Of Carbohydrates In Caries:
- Fermentable dietary carbohydrates play an important role in the causation of caries
- Glucose, sucrose, and fructose are rapidly diffused and fermented by cariogenic bacteria in the oral cavity to produce acid
- This causes the dissolution of hydroxyapatite crystals of enamel
- Risk of caries occurrence increases if dietary sugar is sticky and adheres to the tooth surface for a longer time
- Following its ingestion, the pH of plaque falls to 4.5-5 within 1-3 minutes and neutralization occurs after 10-30 minutes
Enamel Caries Histopathology:
- Early enamel caries
- Loss of interprismatic or inter-rod substances with an increase in prominence of enamel rods
- Appearance of transverse striations of enamel rods
- Dark lines often appear at right angles to the enamel rods
- Accentuation of incremental striate of Retzius
- Advanced enamel caries
- Advanced enamel caries presents several zones in tissues
- Zone 1- Translucent Zone
- Advanced enamel caries are the deepest zone
- Advanced enamel caries is slightly more porous
- Contains 1% by volume
- Pores are larger than usual pores seen in normal enamel
- Dissolution of mineral occurs at the junction of prismatic and interprismatic enamel
- Zone 2-Dark zone
- Located superficial to the translucent zone
- Excessive demineralization of enamel occurs
- Dark zone is narrow in rapidly advancing caries and wide in slowly advancing caries
- Contains 2-4% pore volume
- Pores are smaller than those of the translucent zone
- There is some degree of remineralization present
- Zone 3- Body of lesion
- Present between the dark zone and the surface layer of enamel
- Represents the area of greatest demineralization
- Pore volume is between 5-25%
- Contains larger apatite crystals
- Reprecipitation of minerals occurs
- Dissolution of minerals occurs
- Lost minerals are replaced by unbound water and organic matters
- There is increased prominence of the striate of Retzius
- Zone 4- Surface zone
- The surface zone remains unaffected
- The surface zone is 40 micrometers thick
- Surface remineralization occurs due to active precipitation of mineral ions
Question 4. Describe the immunology of dental caries. Give a brief account of caries activity tests.
Answer:
Immunology of Dental Caries:
- Salivary immunoglobulin IgA protects the tooth from oral pathogenic bacteria by acting as specific agglutinin
- Dental Caries binds and agglutinates specific oral bacteria
- Prevents their adherence to the tooth
- Removes it from the mouth
- Inactivates surface glycosyltransferase
- Reduces synthesis of extracellular glucans
- Reduces plaque formation
- Increases opsonization
Caries Activity Tests:
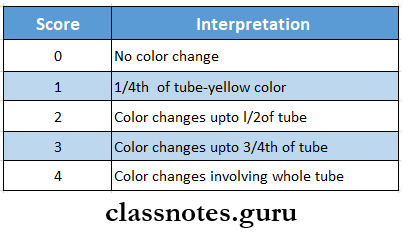
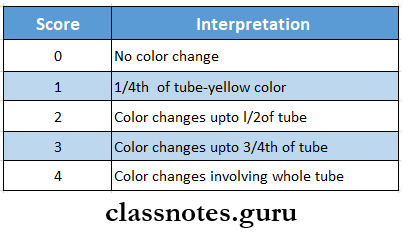
1. Synder’s Test
- Used for lactobacillus count
Synder’s Test Procedure:
- Paraffin-stimulated saliva is collected in test tubes
- Synder test is inoculated into glucose and agar media
- pH-4.7-5 is maintained along with color indicator bromocresol green
- Color change indicates pH change and is compared to the standardized color chart and scored
- Recordings are carried out at the end of 24 hours, 48 hours, and 72 hours
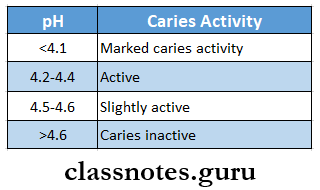
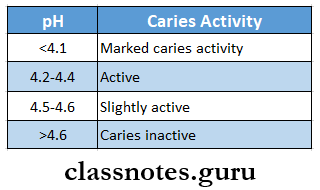
Synder’s Test Result
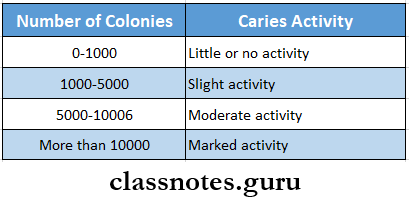
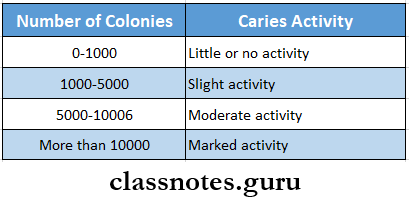
2. Lactobacillus Test
- Described by Hadley in 1933
Lactobacillus Test Procedure:
- Collect paraffin-stimulated saliva
- Dilute to 1:10 dilution by pipetting 1 ml of saliva into a 9 ml tube of sterile saline solution
- Similar again to 1:100 dilution using a 1:10 diluted sample
- Mix thoroughly
- Spread 0.4 ml of each dilution over agar plates
- Incubate for 3-4 days at 37 degrees C
- Count the number of colonies
Lactobacillus Test Result:
3. Swab Test
Swab Test Procedure:
- The oral flora is sampled by swabbing the buccal surfaces of the teeth with a cotton applicator
- Incubate it in media
- The change in pH following 48 hours incubation period is read by pH meter
Swab test Interpretation:
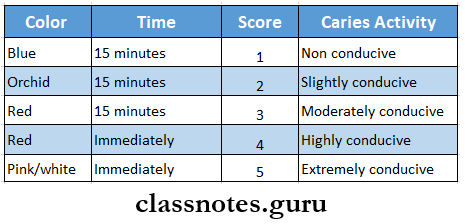
4. Salivary Reductase Test
Salivary Reductase Test Procedure:
- Paraffin-stimulated saliva is collected in a collection tube
- Salivary Reductase Test is then mixed with dye diazo-resorcinol
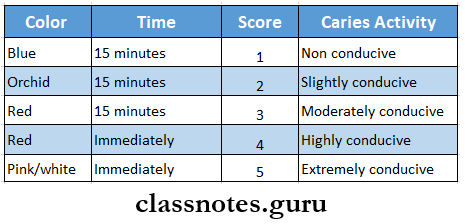
- Caries conduciveness reading or color change is done after 15 minutes
Salivary Reductase Test Result
Dental Caries Short Essays
Question 1. What is plaque? Describe its role in the pathogenesis of dental caries
Answer:
Plaque: Plaque is a soft non mineralized deposit of bacteria present on the tooth surface and other hard surfaces of the oral cavity
Role Of Plaque:
- Plaque harbors the cariogenic bacteria on the tooth surface
- Rapid production of high amounts of acids within the plaque occurs through fermentation of carbohydrates by cariogenic bacteria
- Plaque helps to hold these acids onto the tooth surface for a long duration
- Increased thickness of plaque does not allow the salivary buffers to enter into it to neutralize the acids produced by the cariogenic bacteria
- Plaque protects the acids produced by the cariogenic bacteria from getting neutralized in two ways
- Plaque has diffusion limiting property that does not allow acids to escape
- Does not allow the buffering agents from saliva to enter into it and cause neutralization of acids
- Continued sugar production from bacterial intracellular polysaccharides helps to maintain a low pH and facilitates more tooth decay
Question 2. Describe the etiology of dental caries
Answer:
Etiology of Dental Caries: There are four etiological factors in dental caries
- Tooth
- Composition
- Highly mineralized-less caries formation
- High solubility leads to more caries formation
- Increased permeability of enamel surfaces causes increased caries
- An increase in mineral content leads to increased resistance to caries
- Morphology
- The presence of deep, narrow, and retentive pits and fissures leads to high caries incidence
- Position
- MolaHgned, rotated teeth Are more prone to caries due to more plaque accumuiulkm
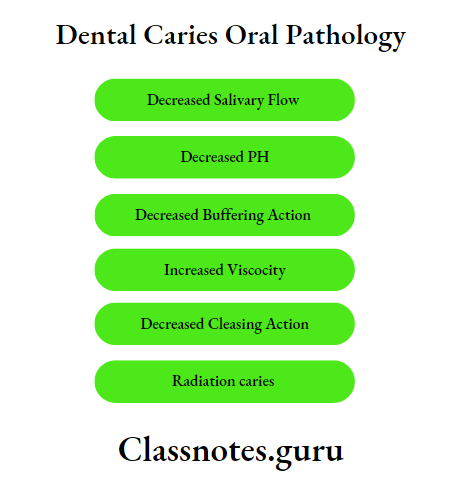
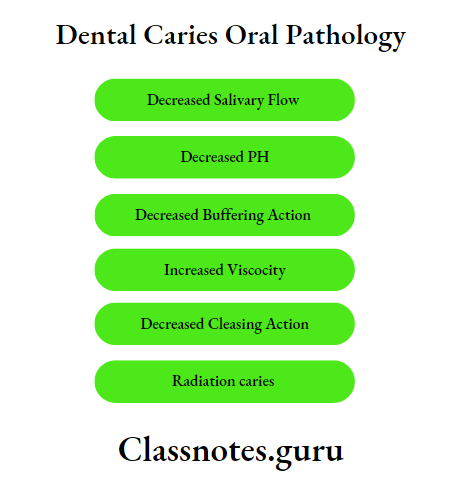
- Saliva
- pH
- A rise in pU neutrally adds attacks on the tooth surface during carle progression
- Composition
- Bicarbonateionscauses neutrailiftalton
- Ammonia- causes a rise in pH
- Quantity
- Reduction of saliva leads to
- Rampant caries
- Exacerbation of caries
- Viscosity
- Extremely viscous saliva leads to carle-free mouth
- Abundant, thin, watery saliva exhibits rampant caries
- Antibacterial properties
- Lysozyme-lyses endogenic and non-cariogenic bacteria
- Salivary peroxidase- inactivates bacterial enzymes
- Immunoglobulin- IgA protects against caries
- Diet
- Fibrous food
- Keep teeth clean
- Stimulates salivary flow
- Reduces caries incidence
- Soft and sticky food increases caries incidence
- Dietary constituents that reduce the incidence of caries are
- Phosphates
- Traces of molybdenum and vanadium
- Vega tables
- Vitamins
- Minerals
- Fats
- Systemic conditions
- Hereditary
- Pregnancy
- Lactation
Question 3. Acidogenic theory of dental caries
Answer:
Acidogenic Theory Of Dental Caries
- Populated by WD Miller In 1889
- Dental caries stales that
- Acids formed due to Ilia fermentation of dietary carbohydrates by oral Itadurla load to progressive decalcification of the tooth structures with subsequent disintegration of organic matrix
- Dental caries states that process of denial Carles Involves two stages
- Initial stage
- Add production due to fermentation of carbohydrates by plaque harder
- Late stage
- Deealdflcalkm of enamel followed by dentin by adds
- This causes total destruction of enamel and dentin
- According to Miller, process of caries Involves four factors
- Dietary carbohydrates
- Micro-organisms
- Adds
- Dental plaque
Question 4. Microbiological aspects of dental Caries
Answer:
Microbiological Aspects Of Dental Caries
- Cariogenic bacteria are present in the oral cavity
- They accumulate In plaque and ferment carbohydrates present In the diet
- Produces add and results in dissolution of enamel to cause cavity formation
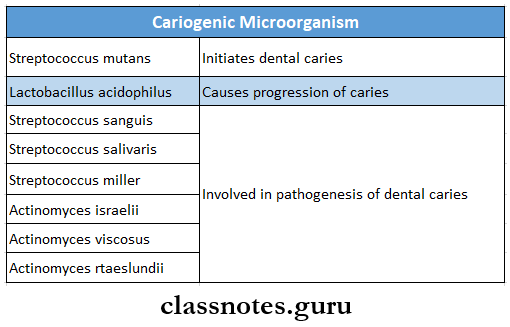
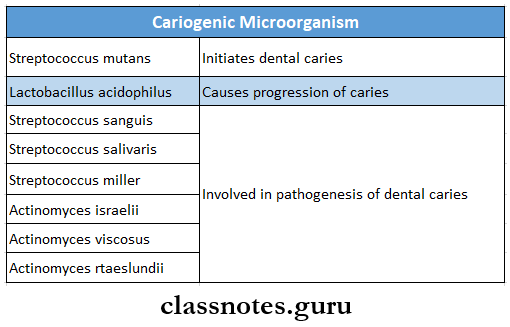
- Microorganisms Involved in the caries process are
- Streptococcus mutans
- Streptococcus mutans are catalase-negative, gram-positive cocci forming short or medium chains
- Streptococcus mutans synthesizes Insoluble polysaccharides from sucrose
- Streptococcus mutans results in production of lactic acid
- This causes a drop in pH favoring caries
- Streptococcus mutans also has the ability to store intracellular glycogen amylopectin
- Provides a reservoir of substrate and enables prolonged periods of increased metabolic activity
- Lactobacillus
- Lactobacillus is long and thin, non-motile
- Lactobacillus may occur singly in the palm or in chain
- Lactobacillus could multiply in low-pH of plaque and carious lesions
- Hence it is an important etiologic agent of dental caries
- Lactobacillus is present in deep fissures and in deep dentinal caries
- Lactobacillus causes progress of caries
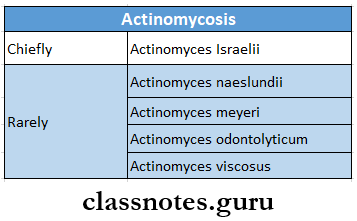
- Actinomycosis
- Lactobacillus cause root caries
Question 5. Preventive measures for carIe’s control
Answer:
Preventive Measures For Caries Control: Preventive measures for caries control include
- Chemical measures
- Chemical includes sub lances that
- Alter tooth surface or tooth structure
- Interfere with carbohydrate degradation
- interfere with bacterial growth and metabolism
- Fluorine
- It decreases microbial acid production
- Enhances remineralization of underlying ename
- Bis-biguandies- Chlorhexidine
- Silver nitrate
- Prevent or arrest dental caries
- Zinc chloride and potassium ferrocyanide
- It seals off Carie’s Invasion pathway
- Vitamin K
- Nutritive measures
- A diet rich in fag low in carbohydrates and free of sugar have low caries activity
- A phosphate-rich diet causes a reduction in caries
- Mechanical measures-includes
- Oral prophylaxis by dentist
- Tooth brushing
- Mouth rinsing
- Use of dental loss
- Pit and fissure sealants
Question 6. Clinical types of caries
Answer:
Clinical Types Of Caries
- Pit and fissure caries
- Carles develops on occlusal surfaces of molars and promoters, buccal and lingual surfaces of motel’s, and palatal surfaces of maxillary Inch sors
- Clinical Types Of Caries Appearance:
- Initially brown or black in color
- Soft and examined through catch by lip of explorer
- Enamel bordering 2 appears opaque bluish-white
- Due to undermining enamel, Caries spreads laterally at DEJ
- Smooth surface caries
- Develops on proximal surfaces of teeth or a gingival third of buccal and lingual surfaces
- Begins just below the contact points
- Incipient caries
- Intact enamel surface
- Destruction of enamel below surface layer
- Appeal’s as chalky while tooth surface
- It Is reversible process
- Cured by remineraiization by salivary Ions
- Prevented by topical fluorides
- Rampant carles
- Present in oil age groups
- Both dentitions are effected
- It involves all teeth Including mandibular incisors
- Rapidly new lesions develop in addition to the present old lesions
- Carious tooth are with pulpal involvement
- Nursing bottle caries
- All teeth except mandibular anteriors are affected
- They are protected by the position of tongue
- Initially, caries appears as dull, white area along gingival margin
- This progresses to the cervical margin to form a ring-like lesion
- Finally, whole crown of Loolh is destroyed
- Chronic caries
- Progresses slowly
- Common in adults
- Dentin is stained dark brown
- Surface destruction occurs with minimal softening of dentin
- Arrested caries
- Caries becomes static
- Affects both dentition
- Occurs on occlusal surfaces
- Recurrent caries
- Occurs in immediate contact of restoration
- Due to inadequate extension of restoration, this favors food lodgement
- Root caries
- Periodontal attachment loss
- Soft, irregular lesion
- Round or oval in shape
- Irregular outline
- Common in males
- Common in mandibular molars
- Radiation caries
- It is rampant caries in patients undergoing radiotherapy
- Rate of progression is faster
- Encircles entire crown cervical portion
Question 7. Write about nursing bottle syndrome
Answer:
Nursing Bottle Caries: Caries caused by prolonged use of a bottle filled with any liquid other than water
Nursing Bottle Etiology:
- Bovine milk and milk products
- Sweeteners like honey-dipped pacifiers
- Micro-organisms like streptococcus mutans
- Fermentable carbohydrates
- Hypoplasia of teeth
- Decreased salivary flow
- Malnutrition
Nursing Bottle Clinical Features:
- All teeth except mandibular interiors are affected
- They are protected by the position of tongue
- Initially caries appears as the dull, white area along the gingival margin
- This progresses to cervical margin to form ring-like lesion
- Finally, whole crown of tooth is destroyed
Nursing Bottle Treatment:
- Excavate and restore all caries lesions
- Pulpal therapy
- Drainage of abscess
- Topical fluoride application
- Diet counselling
- Extraction of unrestorable teeth
Question 8. Cemental caries
Answer:
Cemental Caries
Cemental caries is soft, progressive lesion that is found anywhere on the root surface that has lost its connective tissue attachment and is exposed to the environment
Cemental Caries Etiology:
- Streptococcus mulans
- Lactobacillus
- Actinobacillus
Cemental Caries Clinical Features:
- Periodontal attachment loss
- Soft/irregular lesion
- Round or oval in shape
- Irregular outline
- Common in males
- Common in mandibular molars
Cemental Caries Prevention:
- Plaque removal
- Diet modification
- Use of topical fluoride
- Soft tissue management
- Use of xylitol-containing chewing gums
Question 9. Smooth surface caries
Answer:
Smooth Surface Caries
- Develops on proximal surfaces of teeth or a gingival third of buccal and lingual surfaces
- Begins just below the contact points
Smooth Surface Caries Appearance:
- Initially, faint white opacity of enamel is seen
- In some cases, it appears yellow or brown pigment
- Later it becomes roughened due to superficial decalcification of enamel
- The enamel surrounding the caries is bluish-white
- Smooth Surface Caries extends both buccally and lingually
- There is formation of cavity
Question 10. Theories of dental caries
Answer:
Acidogenic Theory
- Postulated by WD Miller
- Acidogenic Theory states that acids formed due to fermentation of dietary carbohydrates by oral bacteria lead to progressive decalcification of the tooth structures with subsequent disintegration of organic matrix
Proteolytic Chelation Theory
- Proteolytic Chelation Theory states that there is simultaneous microbial degradation of the organic components and the dissolution of the organic components and the dissolution of the minerals of the tooth by the process known as chelation
Sucrose Chelation Theory
- Sucrose Chelation Theory proposes that the sucrose itself and not the acid derived from it can cause dissolution of enamel by forming ionized calcium saccharate
Autoimmune Theory
- Autoimmune Theory suggests that few odontoblast cells at some specific sites within pulp are damaged by an autoimmune mechanism
Dental Caries Short Question And Answers
Question 1. Lactobacillus
Answer:
Lactobacillus
- Lactobacilli are gram-positive, non-spore-forming rods that grow best under microaerophilic conditions
- Lactobacillus is long and thin, non-motile
- Lactobacillus may occur singly or in pairs or in chains
- Lactobacillus could multiple in low-pH of plaque and carious lesion
- Hence it is important etiologic agent of dental caries
- Lactobacillus is present in deep fissures and in deep dentinal caries
- Lactobacillus can be cultured on agar, in broth, in litmus milk, etc
Question 2. Streptococcus mutans
Answer:
Streptococcus Mutans
- Streptococcus mutans are catalase-negative, gram-positive cocci forming short or medium chains
- On agar media they grow as convex colonies
- Streptococcus Mutans synthesizes insoluble polysaccharides from sucrose
- Streptococcus Mutans results in the production of lactic acid
- This causes drop in pH favoring caries
- Streptococcus Mutans also has an ability to store intracellular glycogen amylopectin
- Provides a reservoir of substrate and enables prlonged periods of increased metabolic activity
Question 3. Pioneer bacteria
Answer:
Pioneer Bacteria
- Pioneer bacteria are the first group of bacteria that adheres to the dental plaque
- They are streptococci, Neisseria, Actinomyces and Captocytophaga
- Other bacteria co-adhere to the pioneer bacteria to increase the complexity of the association
- Dental caries results from the metabolism of this association which attacks the tooth enamel
Question 4. Cariogenic micro-organism
Answer:
Cariogenic Micro-organism
Question 5. Name organisms causing cervical caries
Answer:
- Organisms involved in cervical caries are
- Actinomyces
- Nocardia
- Streptococcus mutans
Question 6. Define Caries
Answer:
Caries
- Dental caries is an infectious, microbiologic disease of the teeth that results in localized dissolution and destruction of the calcified tissues of the teeth
- Caries leads to the weakening of tooth structure, cavity formation, and eventual loss of tooth
Question 7. Enamel caries
Answer:
Enamel Caries
- Occurs in pit and fissures, smooth surface, and root
- Initially brown or black in color
- Soft and examined through catch by tip of the explorer
- The enamel bordering it appears opaque bluish-white
- Due to undermining enamel, caries spreads laterally at DEJ
Question 8. Zones in enamel caries
Answer:
Zones In Enamel Caries:
- Zone 1- Translucent zone
- Zone 2- dark zone
- Zone 3- Body of the lesion
- Zone 4- Surface zone
Question 9. Dentinal caries
Answer:
Dentinal Caries
- Dentinal Caries occurs on pit and fissures, smooth surfaces, and root caries
- Initially brown or black in color
- Soft and examined through catch by tip of explorer
- Enamel bordering it appears opaque bluish-white
- Due to undermining enamel, caries spreads laterally at DEJ
Question 10. Zones in dentinal caries
Answer:
Zones In Dentinal Caries:
- Zone 1
- Zone of fatty degeneration of odontoblast process
- Zone 2
- Zone of dentinal sclerosis characterized by deposition of calcium salts in dentinal tubules
- Zone 3
- Zone of decalcification of dentin, a narrow zone preceding bacterial invasion
- Zone 4
- Zone of bacterial invasion of decalcified but in that dentin
- Zone 5
- Zone of decomposed dentin
Question 11. Dental plaque
Answer:
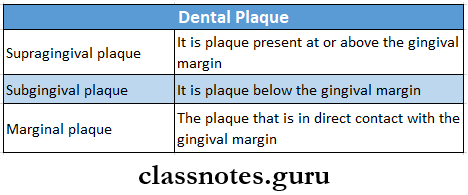
Dental Plaque
Plaque is a soft non mineralized deposit of bacteria present on the tooth surface and other hard surfaces of the oral cavity
Dental plaque Classification:
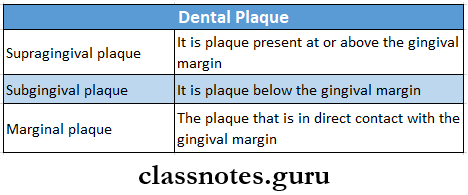
Dental Plaque Composition:
- Dental plaque consists of
- Bacteria
- Epithelial cells
- Macrophages
- Leucocytes
Dental Plaque Effects:
- Calculus formation
- Dental caries
- Periodontal diseases
Question 12. Arrested caries
Answer:
Arrested Caries
- Caries becomes static
- Affects primary and permanent dentition
- Occurs on occlusal surfaces
Arrested CAries Appearance:
- Large open cavity
- Superficially softened and decalcified dentin
- Brown stained
- Sclerosis of dentinal tubules and secondary dentin formation
- It can also occurs on proximal surfaces revealing brown stained at or just below contact point
- Caries is arrested by fluoride application
Question 13. Nursing bottle caries
Answer:
Nursing Bottle Caries: Caries caused by prolonged use of a bottle filled with any liquid other than water
Nursing Bottle Caries Etiology:
- Bovine milk and milk products
- Sweeteners like honey-dipped pacifiers
- Micro-organisms like streptococcus mutans
- Fermentable carbohydrates
- Hypoplasia of teeth
- Decreased salivary flow
Nursing Bottle Caries
- All teeth except mandibular interiors are affected
- They are protected by the position of tongue
- Initially, caries appears as the dull, white area along the gingival margin
- This progresses to the cervical margin to form a ring-like lesion
- Finally, the whole crown of the tooth is destroyed
Question 14. Caries susceptibility
Answer:
Caries Susceptibility
- Caries susceptibility refers to inherent tendency of the host and target tissue to caries process
- Microbiological test helps to measure the number of streptococcus mutants and lactobacillus acidophilus
- Two samples of paraffin-stimulated saliva is collected and diluted 10 times and each is cultivated in two different special media
- After incubation, the number of colonies that develop in two separate media are counted and then are multiplied by 10 to estimate the number of bacteria in 1 ml of saliva
- If the count is more than 10,00,000 S. mutans and more- than 1,00,000 L.acidophilus, then caries susceptibility of the individual is very high
Question 15. Role of Saliva in dental caries
Answer:
Role of Saliva in Dental Caries
Salivary factors that influence dental caries are as follows
- pH
- A rise in pH neutralizes acid attacks on tooth surface during caries progression
- Composition
- Bicarbonate ions- causes neutralization
- Ammonia- causes rise in pH
- Quantity
- Reduction of saliva leads to
- Rampant caries
- Exacerbation of aeries
- Viscosity
- Extremely viscous saliva leads to caries-free mouth
- Abundant, thin, watery saliva exhibit rampant carles
- Antibacterial properties
- Lysozyme- lyses cariogenic and non-cariogenic bacteria
- Salivary peroxidase- inactivates bacterial enzymes
- Immunoglobulin-IgA protects against caries
Question 16. Liquefaction foci of Miller
Answer:
Liquefaction Foci Of Miller
- Liquefaction foci of Miller are present in advanced caries of dentin
- These are formed by focal coalescence and breakdown of few dentinal tubules
- They occur along the direction of dentinal tubules
Question 17. Rampant caries
Answer:
Rampant Caries
Rampant Caries is an acute widespread caries with early pulpal involvement of teeth which are usually immune to decay
Rampant Caries Etiology:
- Multifactorial in nature
- Excessive sticky carbohydrates
- Decreased salivary flow
- Heredia try
Rampant Caries Clinical Features:
- Present in all age groups
- Both dentitions are affected
- Rampant Caries involves all teeth including mandibular incisors
- Rapidly new lesions develop in addition to the present old lesions
- Carious teeth with pulpal involvement
Rampant Caries Treatment: Pulpotomy is done
Question 18. Pit and fissure caries
Answer:
Pit And Fissure Caries
The shape of pit and fissure make it more susceptible to caries
Pit And Fissure Caries Features:
- Initial – Brown/Black in color
- Catch with an explorer
- Decalcification of enamel
- Enamel involvement – in the direction of the rod
- Shape – Triangular, base towards DE
- Progress to the involvement of dentinal tubules
- Result in cavitation
- Undermining of enamel
Question 19. Proteolytic chelation theory
Answer:
Proteolytic Chelation Theory
- Proteolytic Chelation Theory explains the process of dental caries
- According to it
- Initially, all proteolytic breakdown of the organic portion of the enamel matrix takes place
- Formation of a chelating agent by combining proteolytic breakdown products acquired pellicle and food debris
- The negatively charged chelating agent releases positively charged calcium ions from enamel and dentin
- This results in tooth decay
Question 20. Radiation caries
Answer:
Radiation Caries Pathogenesis:
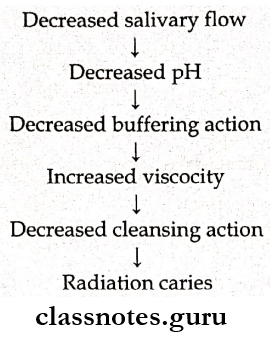
Radiation Caries Types:
- Superficial
- Involving cervical region
- Dark pigmentation
Dental Caries Viva Voce
- The most cariogenic carbohydrate is sucrose
- Clinical significance of sclerotic dentin is that it is resistant to caries
- The most significant organism for pit and fissure caries is Strep. Mutans and lactobacillus
- The most significant organism for root surface caries is A. Viscosus
- The lingual surface of the maxillary lateral incisor is more susceptible to caries
- pH below 5.5 causes demineralization of the tooth surface
- The inorganic phase of enamel consists of crystalline hydroxyapatite
- The critical pH for tooth minerals to act as buffers is 5.5
- Recurrent caries occurs near a restoration
- Brown stains in newly erupted teeth are indicative of underlying decay
- Brown stains in older individuals may be due to arrested lesions