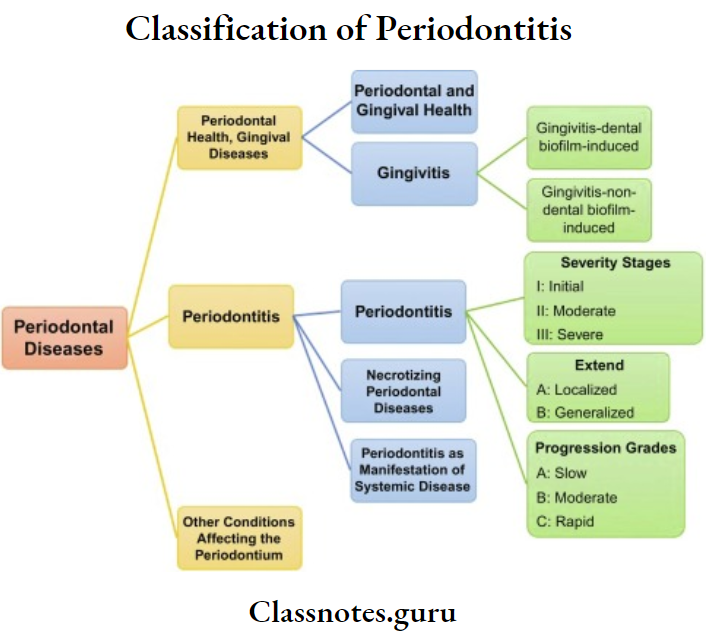
Gingival Enlargements
Gingival Enlargements Definitions
Periodontal Abscess: The periodontal abscess is a localized accumulation of pus within the gingival wall of the periodontal pocket
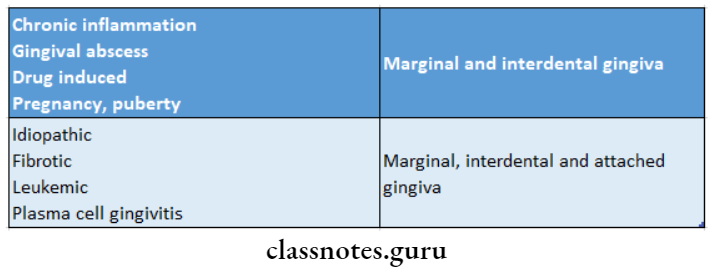
Gingival Enlargements Important Notes
1. Gingival enlargement
- Based on etiology
- Inflammation – Acute
- Chronic
- Drug-induced
- Systemic diseases
- Conditioned enlargements
- Puberty
- Pregnancy
- Non-specific
- Systemic diseases
- Neoplastic
- Benign tumors
- Malignant tumors
- False enlargements
- According to location
- Localized-limited to one/more teeth
- Generalized- involves the entire mouth
- Papillary-confined to interdental papilla – Marginal- confined to marginal gingiva – Diffuse-involves entire gingiva
- Discrete-isolated lesions
- According to the degree
- Grade 0- Normal gingiva
- Grade 1- Involves interdental gingiva
- Grade 2- Involves marginal and interdental papilla
- Grade 3- Covers 3/4th of the crown of teeth
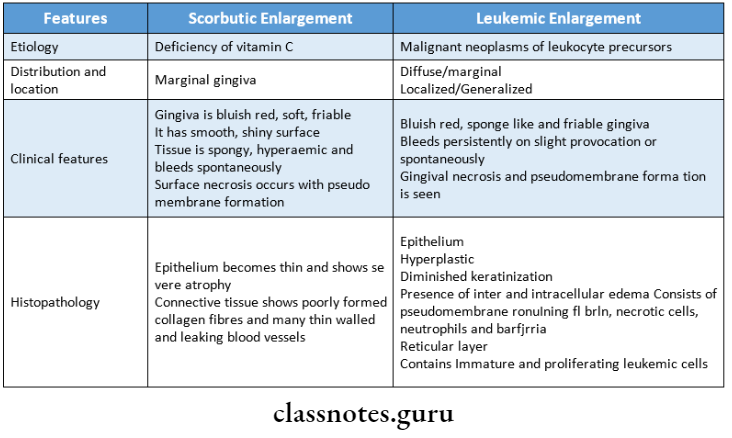
2. Leukemic gingival enlargement
- Occurs only in the acute type and not in the chronic type
- Mostly occurs in acute monocytic leukemia
- The gingival connective tissue is infiltrated with immature leukocytes
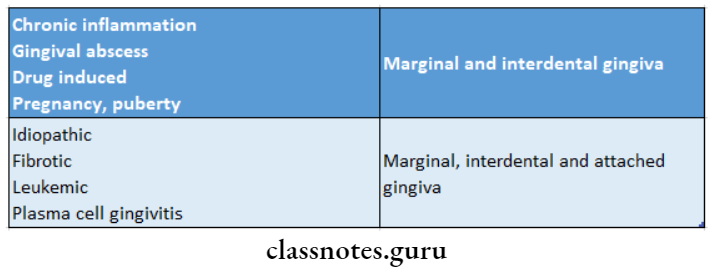
3. Gingival enlargements and their locations
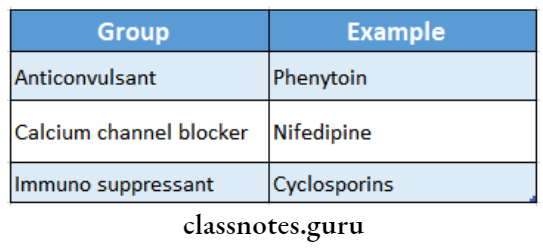
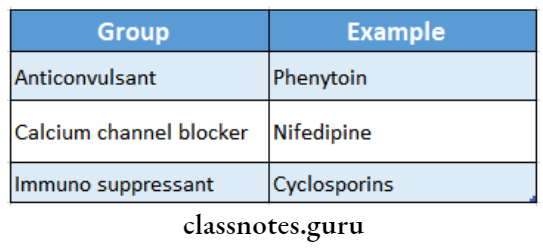
4. Cyclosporine
- It is a potent immunosuppressive drug used to prevent organ transplant rejection and treat several autoimmune diseases
- Gingival enlargement, nephrotoxicity, hypertension, etc are its side effects
- Another immunosuppressive tacrolimus exhibits less severe gingival inflammation
- It is used as a substitute for cyclosporine
5. Phenytoin
- It is used to treat all forms of epilepsy
- Gingival enlargements occur in 50% of patients on this drug
- It often occurs in young patients
- Phenytoin stimulates the fibroblasts and reduces collagen degradation
- Ethosuximide, valproic acid, and mephenytoin are other antiepileptic drugs causing gingival enlargements
6. Plasma cell gingivitis
- Gingiva appears red, friable, granular
- It bleeds easily
- It may be associated with cheilitis and glossitis
- It is allergic in origin possibly related to components of chewing gums, denitrifies, or diet.
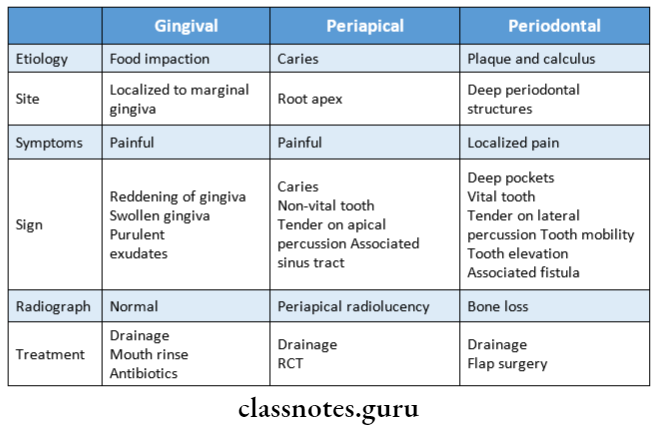
7. Gingival abscess
- It is a localized, painful rapidly expanding lesion of sudden onset
- It is limited to marginal gingiva or interdental papilla
- It is due to foreign substances carried deep into the tissues such as toothbrush bristle, a piece of apple core, or a lobster shell
Gingival Enlargements Long Essays
Question 1. Classify gingival enlargements. Discuss the history- theology and clinical features of drug-induced gingivitis.
Answer:
Gingival Enlargements Classification:
Based on etiology:
- Inflammation:
- Drug-Induced:
Gingival Enlargements Systemic diseases:
- Conditioned enlargements:
- Puberty
- Pregnancy
- Non-specific
- Systemic diseases:
- Neoplastic:
- Benign tumors
- Malignant tumors
- False enlargements:
- Idiopathic:
Read And Learn More: Periodontics Question and Answers
Gingival Enlargements According to the degree:
- Grade 0- Normal gingiva
- Grade 1- Involves interdental gingiva
- Grade 2- Involves marginal and interdental papilla
- Grade 3- Covers 3/4th of the crown of teeth
Drug-Induced Gingivitis:
Drug-Induced Gingivitis Clinical Features:
- It occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in the maxilla
- The site involved- marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion
- Has lobulated surface
- Firm to resilient in consistency
- No tendency to bleed
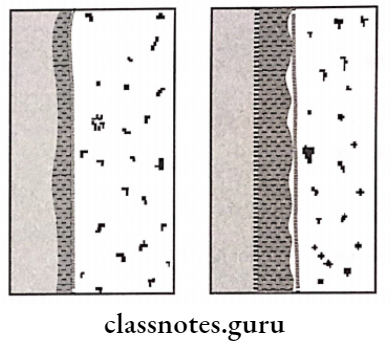
Drug-Induced Gingivitis Histopathology:
1. Epithelium:
- Shows varying degrees of acanthosis
- Elongated, thin rete pegs are present
- Increased epithelial pearls
- Presence of PMNs
2. Lamina propria:
- The proliferation of fibroblasts present
- There is an increase in collagen production
Question 2. Classify different gingival enlargements. Describe in detail acute inflammatory enlargement.
Answer:
Gingival enlargement Classification:
1. According to the etiology:
Inflammation:
Drug-Induced:
- Phenytoin
- Cyclosporins
- CCB’s
Systemic diseases:
- Conditioned Vitamin C deficiency
- Puberty
- Pregnancy
- Non-specific
- Systemic diseases – Leukemia
Neoplastic:
- Benign
- Malignant
- False enlargements
2. According to Location:
Localized: limited to one/more teeth
- Generalized: Involves entire mouth
- Papillary: Confined to interdental papilla
- Marginal: Confined to the marginal gingiva
- Diffuse: involves the entire gingiva
- Discrete: Isolated lesions
3. According to the degree:
- Grade 0: Normal gingiva
- Grade 1: Involves interdental papilla
- Grade 2: Involves marginal and interdental papilla
- Grade 3: Covers 3/4th of the crown of teeth
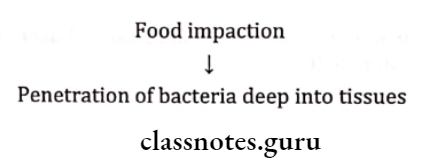
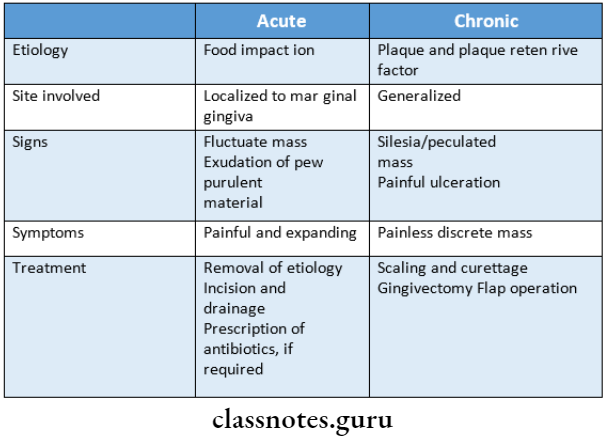
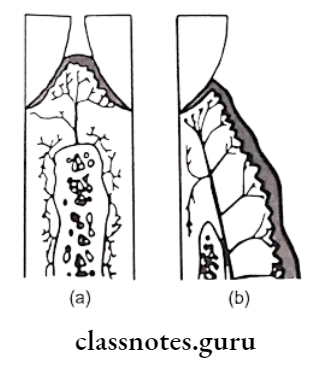
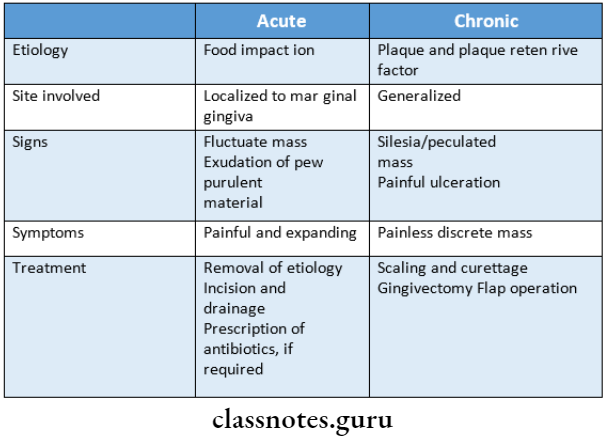
Acute Inflammatory Enlargement:
- Sudden localized painful expanding lesion occurring on biting of hard objects like apple or fish thorns
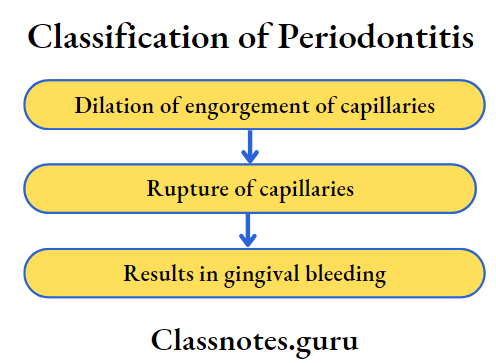
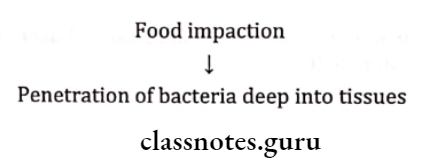
Etio-Pathogenesis:
Gingival enlargement Features:
- Site – Localized to the marginal gingiva
- Color – Reddish
- Surface – Smooth and shiny
- Symptoms – Painful, expanding lesion
- Sign – Bleeding on probing
- Tender on percussion
- Exudation of purulent material
- Size – Swollen gums
Gingival enlargement Treatment:
- Removal of etiological factors
- Incision and drainage of abscess
- In persistent cases, prescribe antibiotics
Gingival Enlargements Short Essays
Question 1. Pericoronal Abscess.
Answer:
Pericoronal Abscess is a localized accumulation of pus covering the crown of unerupted/partially erupted teeth
Pericoronal Abscess Etiology:
- Plaque accumulation around the impacted teeth
Pericoronal Abscess Features:
- Red, swollen, erythematous gingiva around impacted teeth
- Interferes with occlusion
Pericoronal Abscess Radiographic Features:
- Radiograph shows impacted teeth
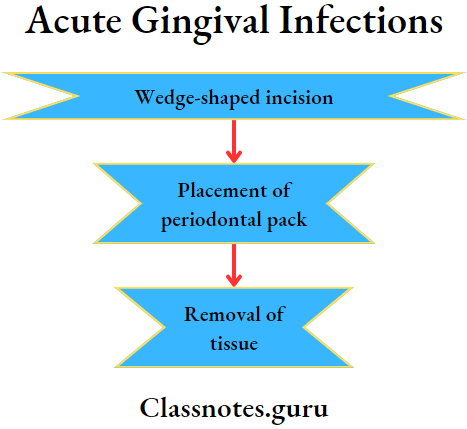
Pericoronal Abscess Treatment:
Question 3. Dilantin sodium-induced hyperplasia.
Answer:
Dilantin Sodium-Induced Hyperplasia Clinical Features:
- Dilantin Sodium-Induced Hyperplasia occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in the maxilla
- Site involved-marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion
- Has lobulated surface
- Firm to resilient in consistency
- No tendency to bleed
Dilantin Sodium-Induced Hyperplasia Histopathology:
1. Epithelium:
- Shows varying degrees of acanthosis
- Elongated, thin rete pegs are present
- Increased epithelial pearls
- Presence of PMNs
2. Lamina propria:
- The proliferation of fibroblasts present
- There is an increase in collagen production
Question 4. Differentiate Acute and Chronic Inflammatory Enlargement.
Answer:
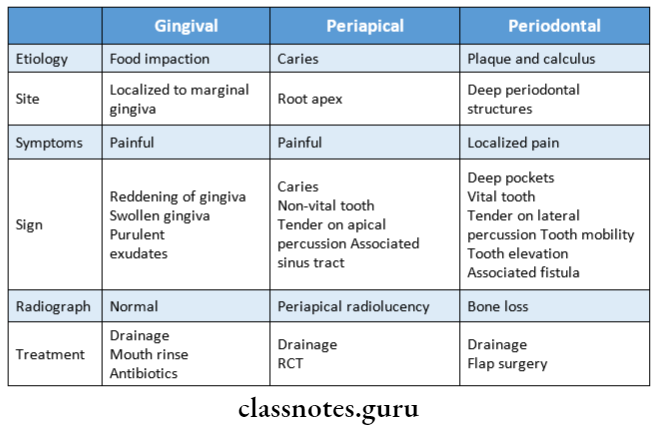
Question 5. Differentiate periapical, periodontal, and gingival abscesses.
Answer:
Question 6. Drug-induced Gingival Enlargement.
Answer:
Drugs Causing Enlargement:
Drugs Causing Enlargement Features:
- Duration – 3 months after initiation of drug therapy
- Location – Generalized
- The site involved – Marginal gingiva and interdental papilla
- Appearance – Painless, bead-like enlargement
- Complication – Interferes with occlusion
- Absence of inflammation
- Mulberry shaped enlargement
- Color-pale pink
- Presence of inflammation
- Color-red/bluish-red
- Presence of increased bleeding
- Consistency – Firm and resilient
- Surface:
- Bleeding:
Drugs Causing Enlargement Pathogenesis:
- The similarity in the structure of phenytoin and sub-population of fibroblasts
- Thus, fibroblasts become sensitive to phenytoin
- Results in increased collagen production
Drugs Causing Enlargement Treatment:
Step 1:
- Oral prophylaxis
- Substitute drug
- Recall
Step 2:
- Mild case – Gingivectomy
- Severe destruction – flap surgery
Question 7. Leukemic Gingival Enlargement.
Answer:
Leukemic Gingival Enlargement Distribution:
- Diffuse/marginal
- Localized/Generalized
Leukemic Gingival Enlargement Appearance:
- It increases in size gradually and covers the tooth crown
- Tumor like enlargement
- Color-bluish red
- Surface-shiny
- Consistency-moderately firm
- Bleeding on probing – positive
- Increased susceptibility to infections Associated symptoms: ANUG
Leukemic Gingival Enlargement Treatment:
- Consult physician
- Monitor hematological values
- Antibiotic prophylaxis
- Incision and drainage
- Cleanse the area with cotton pellets soaked in hydrogen peroxide
- Application of pressure with gauze
Question 8. Classify gingival enlargement. Add a note on idiopathic gingival enlargement.
Answer:
Gingival Enlargement:
Gingival Enlargement is an increase in the size of the gingiva
Gingival Enlargement Classification:
1. Based on etiology:
- Inflammation
- Drug-induced
- Systemic diseases
- Conditioned enlargements
- Puberty
- Pregnancy
- Non-specific
- Systemic diseases
- Neoplastic
- Benign tumors
- Malignant tumors
- False enlargements
- Idiopathic
2. According to the location:
- Localized-limited to one/more teeth
- Generalized- involves the entire mouth
- Papillary-confined to interdental papilla
- Marginal- confined to the marginal gingiva
- Diffuse- involves the entire gingiva
- Discrete- Isolated lesions
Idiopathic Gingival Enlargement:
Idiopathic Gingival Enlargement is a rare condition of unknown etiology
Idiopathic Gingival Enlargement Clinical Features:
- It has diffuse involvement
- Involves attached gingiva, marginal gingiva, and inter-dental papilla
- The affected gingiva is firm, pink, and leathery in consistency and has a pebbled surface
- Facial and lingual surfaces of the mandible and maxilla are generally affected
- Teeth are almost completely covered by the gingival enlargement
- The enlargement projects into the oral vestibule
- Jaws appear distorted
- Secondary inflammatory changes occur
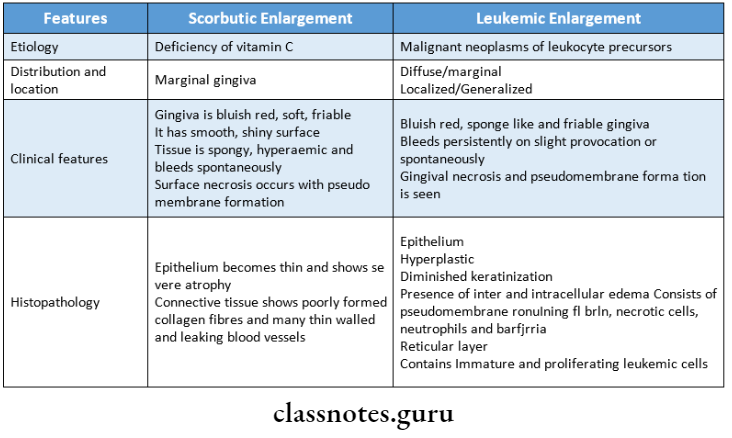
Question 9. How will you differentiate between scorbutic gingival enlargement and leukemic gingival enlargement?
Answer:
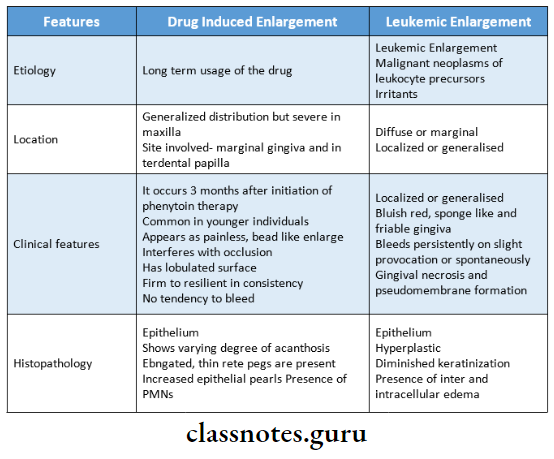
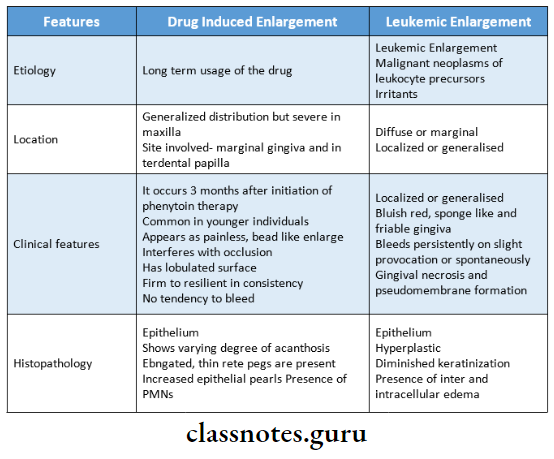
Question 10. Compare drug-induced gingival enlargement and leukemic gingival enlargement.
Answer:
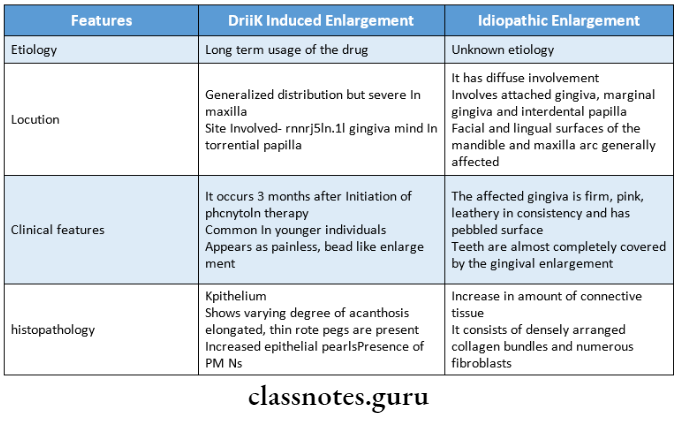
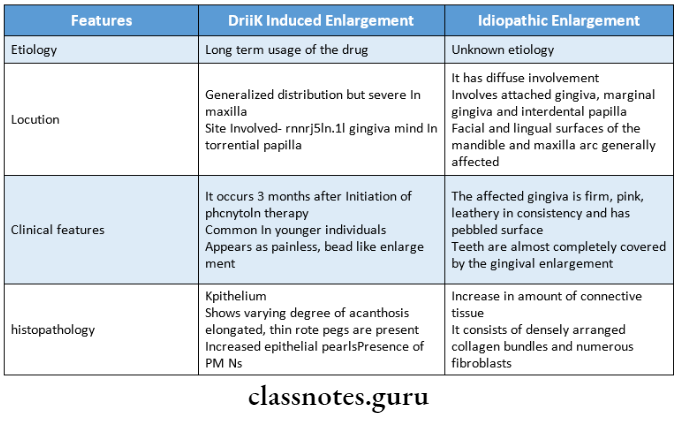
Question 11. Compare drug-induced and Idiopathic gingival enlargement.
Answer:
Question 12. Benign tumors of the gingiva.
Answer:
Benign Tumours Of Gingiva:
1. Focal fibrous hyperplasia:
- Focal fibrous hyperplasia is present often in adults
- Focal fibrous hyperplasia is a nodular lesion
- Has dome-like growth with a smooth surface of normal color
- Surface keratosis occurs
- Focal fibrous hyperplasia is slow progressing lesion
- Focal fibrous hyperplasia may remain the same size for many years
- Focal fibrous hyperplasia is also known as peripheral fibroma
2. Peripheral ossifying fibroma:
Peripheral ossifying fibroma is a gingival nodule consisting of reactive hyperplasia of connective tissue containing focal areas of bone
Peripheral ossifying fibroma Clinical Features:
- Peripheral ossifying fibroma represents a well-demarcated, encapsulated, ex-pantile, central jaw lesion
- Peripheral ossifying fibroma is localized, painless, non-tentered bony hard swelling.
- Peripheral ossifying fibroma is a slow-growing lesion
- Peripheral ossifying fibroma leads to the expansion and distortion of cortical plates
- There may be displacement of regional teeth
3. Peripheral giant cell granuloma:
Peripheral Giant Cell Granuloma is the hyperplastic reaction of gingival connective tissue in which the histiocytic and endothelial cellular components predominate
Peripheral giant cell granuloma Clinical Features:
- Age- during the mixed dentition period
- Sex- common in females
- Site- interdental papilla
- Appears as a small, exophytic, well-circumscribed, pedunculated lesion on the gingival surface
- It is painless, firm, and lobulated
- Surface- smooth or granular
- Size-less than 2 cm in diameter
- Color-purplish-red to dark-red in color
- The overlying epithelium is ulcerated
- Consistency-firm
- Bleeding occurs spontaneously
- Some lesions may develop with hour-glass shapes located between teeth and lobulated extremities projecting both buccally and lingually
4. Gingival cyst: A gingival Cyst is derived from the rest of the dental lamina
Gingival Cyst Clinical Features:
- A gingival Cyst occurs as firm, compressible, fluid-filled swelling on the facial gingiva usually in the anterior or premolar region
- A gingival Cyst usually develops as a solitary lesion
- Color remains normal
- Occurs on attached gingiva or interdental papilla
Question 13. Clinical features of drug-induced gingival enlargement.
Answer:
Drug-Induced Gingival Enlargement :
- Phenytoin
- Cyclosporins
- CCB’s
- It occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in the maxilla
- The site involved- marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion
- Has lobulated surface
- Firm to resilient in consistency
- No tendency to bleed
Gingival Enlargements Short Answers
Question 1. Periodontal abscess.
Answer:
The periodontal abscess is a localized accumulation of pus within the gingival wall of the periodontal pocket
Periodontal abscess Etiology: Presence of plaque and calculus
Periodontal abscess Clinical Features:
- Involves deep periodontal structures
- Localized pain
- Deep pockets
- Vital tooth
- Tender on lateral percussion
- Tooth mobility
- Associated fistula
Periodontal abscess Treatment:
Question 2. Conditioned Gingival Enlargements.
Answer:
Conditioned enlargements are caused by systemic conditions of the patient which exaggerates the usual gingerval response to dental plaque
Conditioned Gingival Enlargements Types:
- Hormonal
- Nutritional
- Allergic
Question 3. Angiogranuloma.
Answer:
- Gingival enlargement in pregnancy is also known as angiogranuloma
- It is an inflammatory response to local irritation
- It is modified by the patient’s condition
- It usually appears after the first trimester
Question 4. Drug-induced gingival enlargements.
Answer:
Drug-Induced Gingival Enlargements Clinical Features:
- It occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in the maxilla
- The site involved- marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion
- Has lobulated surface
- Firm to resilient in consistency
- No tendency to bleed
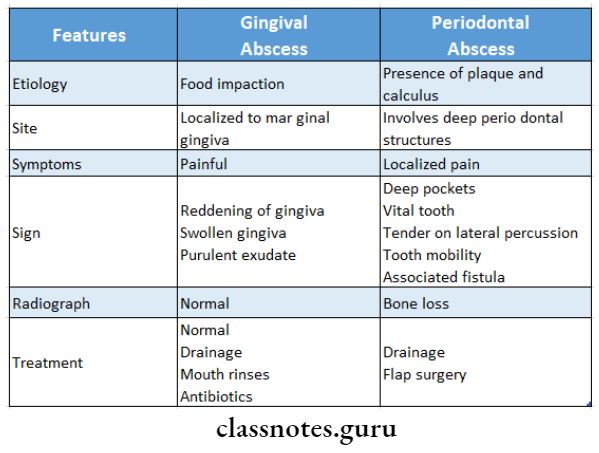
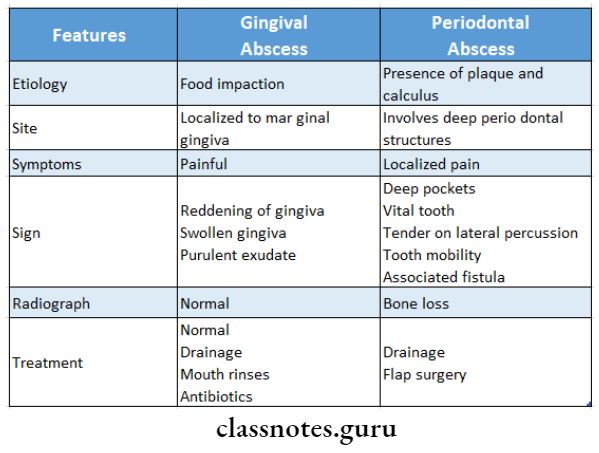
Question 5. Write the difference between gingival and periodontal abscess.
Answer:
Question 6. Wegener’s Granulomatosis.
Answer:
- Wegener’s Granulomatosis is a disease of unknown etiology
- Wegener’s Granulomatosis basically involves the vascular, renal, and respiratory systems
Wegener’s Granulomatosis Clinical Features:
- Occurs at any age
- Common in males
- Initially, there is the development of rhinitis, sinusitis, and otitis
- The patient later develops cough and hemoptysis, fever, joint pain
- Hemorrhagic or vesicular skin lesions are common
Wegener’s Granulomatosis Oral Manifestations
- Affected gingiva is termed strawberry gingiva Gingival lesions may be ulcerations, friable granular lesions
- It starts in the interdental papilla and spreads rapidly
- This leads to bone loss and tooth mobility
Question 7. Developmental gingival enlargements.
Answer:
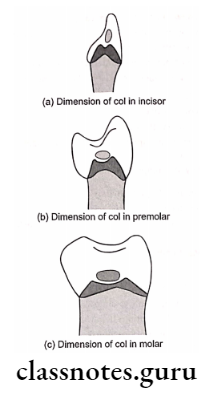
- These enlargements are physiologic
- During various stages of the eruption, the labial gingiva may show a bulbous marginal distortion caused by the superimposition of the bulk of the gingiva on normal enamel
- This enlargement is known as developmental enlargement
Question 8. Differential diagnosis of epulis.
Answer:
- Epulis refers to all discrete tumors and tumor-like masses of the gingiva
- Differential diagnosis of it includes oral fibroma
Question 9. Leukemic gingival enlargement.
Answer:
Leukemic Gingival Enlargement Distribution:
- Diffuse or marginal
- Localized or generalized
- It increases in size and gradually covers the tooth crown
- It appears as a tumor-like enlargement
- Color-bluish red in color
- Surface-shiny surface
- Consistency-spongy-like and friable
- Gingiva bleeds spontaneously
- Increased susceptibility to infections
Gingival Enlargements Viva Voce
- Three types of conditioned gingival enlargements are: hormonal, nutritional, and allergic
- Fibrotic gingival enlargement is a side effect of some anticonvulsants, calcium channel blockers, and immunosuppressant drugs
- Leukemic enlargement is generally bluish-red and has a shiny surface
- Administration of phenytoin may precipitate mega-holoblastic anemia and folic acid deficiency.
- Drug-induced gingival enlargement starts at the interdental papilla
- Cyclosporine causes highly vascularized gingival enlargement
- Systemic administration of phenytoin accelerates the healing of a gingival wound
- Tacrolimus can replace Cyclosporine
- Bacterial plaque is not necessary for the initiation of gingival enlargement in Wegener’s granulomatosis