Fractures General Principles Short Essays
Question 1. Compound fracture
Answer:
Compound Fracture
- Compound fracture or open fracture involves wounds that communicate with the exterior and gets contaminated
Compound Fracture Classification:
- Type 1
- The wound is smaller than 1 cm
- It is clean wound
- Type 2
- The wound is longer than 1 cm
- It is clean and without any soft tissue damage
- Type 3
- The wound is longer than 1 cm with extensive soft tissue damage
Compound Fracture Management:
- Aims
- To prevent infection
- To allow tire fracture to heal
- To restore function
- Treatment
- Control of hemorrhage
- Antibiotic administration
- Cefazolin or clindamycin is preferred for type 1 and type 2
- Metronidazole is preferred for type 3
- Tetanus vaccination
- Irrigation and debridement of the wound
- Incision and drainage in case of type 3
Read And Learn More: General Surgery Question and Answers
Question 2. Pathological fractures
Answer:
Pathological Fractures
- Pathological fracture is one that occurs due to underlying diseases like
- Tumors:
- Giant cell tumour
- Bone cysts
- Infections:
- Acute osteomyelitis
- Metabolic bone diseases
- Hyperparathyroidism
- Osteoporosis
- Paget’s disease
Pathological Fractures Common Sites Involved:
- Vertebral fractures
- Fractures of the neck of femur
- Colles fracture of the wrist
Pathological Fractures Diagnosis:
- Laboratory investigation
- To rule out the systemic diseases present
- ESR estimation
- Total blood count
- A comminuted bone scan is done
- Biopsy
Types of fractures short essay
Question 3. Fracture healing
Answer:
Stages Of Fracture Healing:
- Stage of inflammation
- Occurs soon after the fracture
- Trauma to the blood vessels of the periosteum, endosteum, bone marrow, and Haversian system occurs
- As a result hematoma formation occurs
- This causes hypoxia and necrosis of the fragment ends
- There is acute inflammatory reaction with edema at the site
- Pleuripotent cells produce osteoblast, fibroblast, and chondroblasts
- Granulation tissue is formed
- Hematoma gets organized
- Soft callus formation
- There is formation of subperiosteal fibrous tissue with fibrocartilagenous and cartilagenous components
- This is called callus
- It is soft at this stage
- Hard callus formation
- The endosteal and periosteal blood supply improves
- The callus gets converted into woven bone
- This immature bone is called hard callus
- Stage of remodeling
- There is a continuous process of deposition and resorption of bone
- The immature bone gets converted into mature lamellar bone
Question 4. Nonunion
Answer:
Nonunion
Lack of bony fusion of fractured ends
Nonunion Etiology:
- Inadequate fixation
- Infection of the fracture
- Lack of adequate blood supply
- Excessive periosteal stripping
- Pathological fractures
Nonunion Features:
- Pain
- Difficulty in occlusion
- Difficulty in mastication
- Abnormality mobility of fractured fragments
Nonunion Management:
- Expose the site
- Graft the space
- Stabilize the fractured ends
- Fixation
- Immobilization
Short note on bone fractures
Question 5. Dislocation and subluxation
Answer:
Dislocation And Subluxation
- Dislocation refers to the condition in which the condyle is placed anterior to the articular eminence with collapse of the articular space
- Subluxation is the partial dislocation
Dislocation And Subluxation Clinical Features
- Pain
- Inability to close the mouth
- Tense masticatory muscles
- Difficulty in speech
- Excessive salivation
- Open bite
- Protruding chin
- Deviation of the lower jaw
Dislocation And Subluxation Management:
- Reassure the patient
- Sedative drugs
- Pressure and massage the area
- Manipulation
- The operator grasps the patient’s mandible
- The thumb is placed over the occlusal surfaces of the lower molars
- Fingertips are placed below the chin
- Downward pressure is placed over posteriors
- This overcomes spasms of muscles
- Backward pressure is applied which pushes the entire mandible posteriorly
- Immobilization is done
Classification of bone fractures
Question 6. General Management Of Patient With Head Injury
Answer:
General Management Of Patient With Head Injury
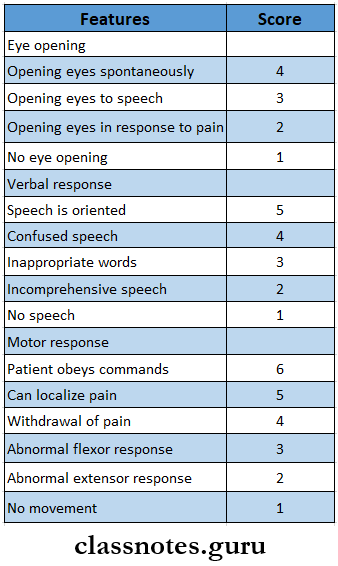
- Management of the head injury depends on Glasgow Coma Scale
- Less than 8 score- indicate severe injury
- Score 9-12- moderate injury
- Score 13-15- mild injury
- Measures includes
- Examination of the wound
- Continued ventilation
- Intensive care unit management of intracranial pressure
- Oxygenation
- Frequent neurological examination
- CT scan