RNA Viruses Important Notes
1. Inclusion Bodies
Read And Learn More: Microbiology Question and Answers
2. Infections Caused By Human Papillomavirus
- Verruca Vulgaris
- Focal epithelial hyperplasia
- Condyloma acuminatum
RNA Viruses Virology Short Essay Questions and Answers
3. Types Of Rabies Vaccine
- Semple vaccine
- BPL (Beta propriolactone) vaccine
- Infant brain vaccine
RNA Viruses: Short Essays
Question 1. Polio Vaccine
(or)
Immunoprophylaxis for Poliomyelitis
Answer:
The two types of polio vaccines are as follows
1. Salk’s Polio Vaccine:
- It was developed by Salk in 1953.
- It is a formalin-activated preparation of the three types of poliovirus grown in monkey kidney tissue cultures.
- Viral pools of adequate titre are filtered to remove the cell debris and clumps and inactivated with formalin at 37°C for 12-15 days.
Router of Administration:
The vaccine is given by deep subcutaneous or muscular injection.
Salk’s Polio Vaccine Doses:
Three doses are given 4-6 weeks apart, followed by a booster dose that should be given six months later.
- The first dose should be given after the age of six months so that antibody response is not impaired by the residual maternal antibodies.
- Immunity can be sustained by booster doses every 3-5 years thereafter.
Salk’s Polio Vaccine Mechanism:
- This vaccine produces long-lasting immunity to all three poliovirus types.
- Induces serum antibodies
2. Sabin’s Vaccine:
- It was developed by Sabin in 1962
- It contains live attenuated strains of poliovirus types 1, 2, and 3 grown either in monkey kidney cells or human diploid cell cultures.
Sabin’s Vaccine Route of Administration:
- It is administered orally, so known as the oral polio vaccine (OPV).
Sabin’s Vaccine Mechanisms:
- It stimulates both local secretory Iga antibodies in the intestine as well as humoral antibodies (Igm and Igg).
- When the virus is excreted in the faeces, it may spread to close contacts
- Thus, it protects the individual and the community
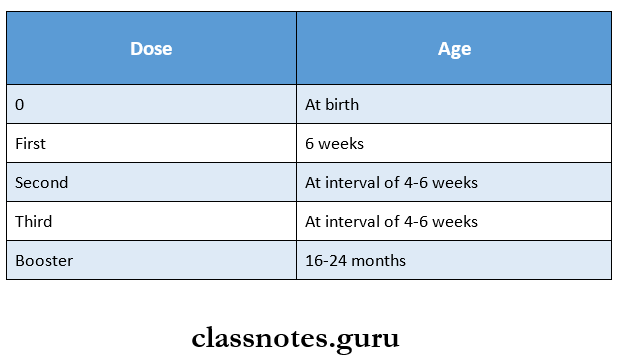
Sabin’s Vaccine Doses:
- Three doses are given
- All doses are generally given along with DPT.
- In addition to it, the following doses are given
Question 2. Mumps:
Answer:
- Mumps is an acute viral infectious disease character¬ised by unilateral (or bilateral nonsuppurative enlargement of the salivary glands, usually the parotid gland.
- Submandibular and sublingual glands are occasionally involved.
- Usually, children are affected. It may also occur in adults.
- Also known as epidemic parotitis
Mumps Causative organism:
- Organisms involved in paramyxovirus.
Mumps Route of infection:
- Infection is acquired by inhalation or direct contact, or through the conjunctiva.
- The incubation period is 12 – 18 days.
RNA Viruses: Important Essay Topics for Medical Students
Mumps Clinical Features:
- Unilateral or bilateral swelling of the parotid glands.
- Fever, malaise
- Local pain and tenderness
- The involvement of extra parotid sites can cause more serious problems as follows.
- CNS involvement may lead to
- Meningitis,
- Meningoencephalitis
- Orchitis
Mumps Complications:
- Orchitis
- Oophoritis
- Arthritis
- Nephritis
- Pancreatitis
- Thyroiditis and myocarditis.
Mumps Laboratory Diagnosis:
- Isolation of viruses from CSF, saline (or urine.
- Serological tests with paired serum samples are tested for the rise in the titer of antibodies by complement fixation test ELISA, and haemagglutination tests.
- Serum amylase levels are elevated in both parotitis and acute pancreatitis.
- Mumps Treatment: Treatment is conservative, maintaining hydration.
- Prevention is the use of the MMR vaccine.
RNA Viruses Short Question And Answers
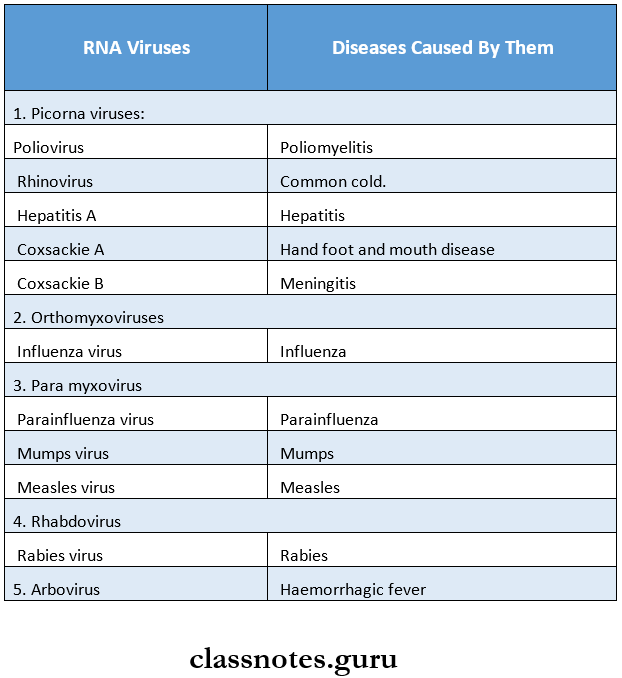
Question 1. Name 3 RNA viruses and diseases caused by them.
Answer:
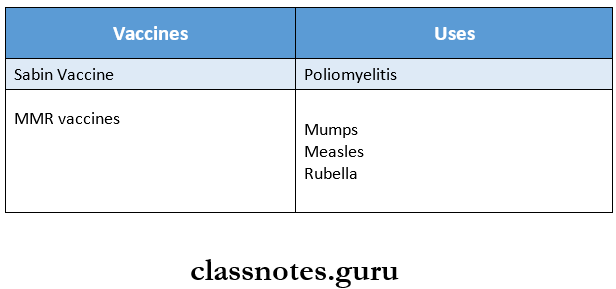
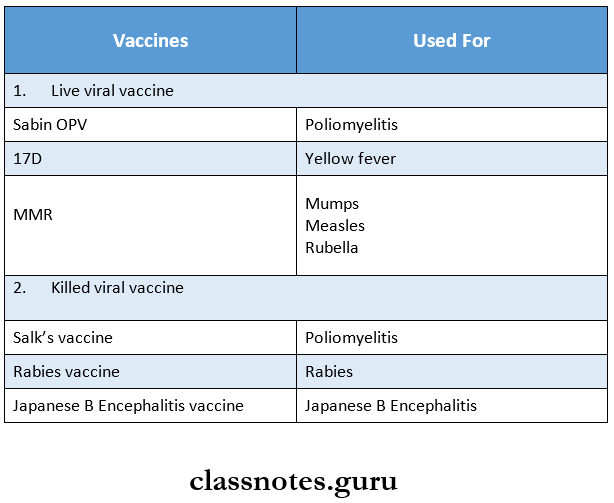
Question 2. Mention two important live viral vaccines.
Answer:
Live viral vaccines are
Question 3. Koplik’s spots?
Answer:
- Koplik’s spots are named after Henry Koplik, who first described them in 1896
- Koplik’s spots are seen in measles or rubella
- Immune reaction to the virus in the endothelial cells of dermal capillaries plays a role in the development of spots.
Koplik’s Spots Appearance:
- These are small, irregularly shaped flecks
- They appear as bluish-white flecks surrounded by a bright red margin.
- The spots disappear after the onset of the rash.
- Orally, they are most commonly observed on the buccal mucosa opposite to the lower molars
- With the decline of acute symptoms,a widespread maculopapular rash over the neck
- It then spreads to the rest of the body
- The rash fades in about a week
- The patient recovers in 10-14 days
RNA Viruses: Structure and Replication Cycle Essay
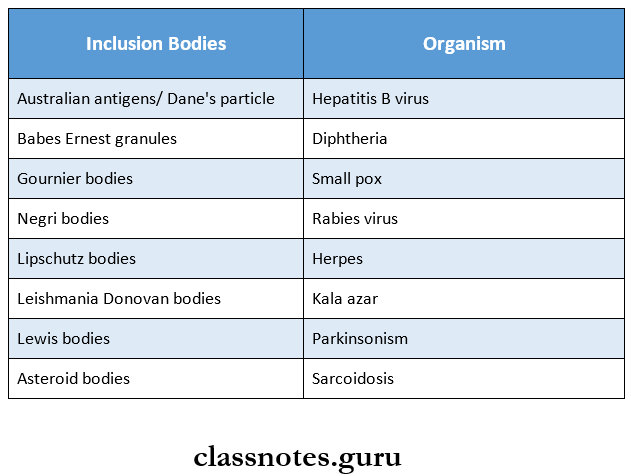
Question 4. Inclusion bodies?
Answer:
- Inclusion bodies are distinctive structures frequently formed in the nucleus or) cytoplasm in cells infected with certain viruses.
- These are 3 types based on location
- Intranuclear
- Intra cytoplasmic
- Both.
- They are also known as cellular inclusions.
- Examples are:
- Intra-cytoplasmic and intra-nuclear
- Negri bodies – rabies
- Intra-cytoplasmic
- Henderson – Peterson bodies – molluscum contagiosum- gypsum
- Intra-nuclear
- Cow dry type A – Herpes, yellow fever
- Cow dry type B – Adenovirus, poliomyelitis.
- Intra-cytoplasmic and intra-nuclear
Question 5. Name four vaccines
Answer:
Question 6. Mumps vaccine?
Answer:
- An effective live attenuated vaccine [Jeryl Lynn strain of mumps virus] grown in chick embryo fibroblast cul¬ture is against mumps.
- The vaccine is given as a single subcutaneous injection either alone or) in combination with the MMR vaccine.
- The vaccine is not protective to individuals already exposed to the virus and who are in the incubation stage of the disease.
- The MMR vaccine provides effective protection for 10 years.
Mumps Vaccine Contraindications:
- Pregnancy
- Immunodeficiency
- Hypersensitivity neomycin or egg protein.
Question 7. Arboviruses
Answer:
- Arboviruses are RNA viruses that are transmitted by blood-sucking arthropods from one vertebrate host to another
- Mosquitoes, ticks and sandflies are the principal vectors
- They are named according to the
- Disease caused by them- example. Yellow fever
- Place of isolation- for example, Kyasanur forest disease
- The local name of the disease, for example, Chikungunya
- They are classified according to their physical and chemical features into five families
- Togaviridae
- Flaviviridae
- Bunyaviridae
- Rheoviridae
- Rhabdoviridae
- They are named according to the
Arbovirus Diseases Caused by Them:
- Encephalitis
- Haemorrhagic fever
Arboviruses Diagnosis:
The diagnosis is made by virus isolation and serologi¬cal tests
Question 8. Rabies vaccine
(or)
Immunisation against rabies
Answer:
Rabies vaccines are of two types
- Neural
- Non-neural
1. Neural Vaccines:
- Semple Vaccine:
- The most widely used vaccine
- Developed by Semple at Central Research Insti¬tute, Kasauli.
- It is a 5% suspension of infected sheep brain and inactivated by 5% phenol at 37°C leaving no re¬sidual live virus.
- Beta Propiolactone (BPL) Vacine:
- Modified semple vaccine
- Instead of phenol, BPL is used as an inactivating agent.
- Infant Brain vaccine:
- Used widely in South America
- Reduce neurological complications.
- Vaccination Schedules:
- Nowadays not used.
- In the past, they were given subcutaneously on the anterior abdominal wall.
- 7 – 14 injections depend on the degree of risk.
2. Non-Neural Vaccines:
- Duck Egg Vaccine:
- BPL is used as an inactivating agent
- It has poor immunogenicity so not used now.
- Tissue Culture Vaccines: Following cell culture vaccines are available in India.
- Human diploid cell strain vaccine [HDCS]
- The HDCS vaccine is prepared by growing rabies virus on human diploid cells and is in¬activated with BPL.
- This vaccine is highly antigenic and free of side effects
- Purified chick embryo cell vaccine [PCEC]
- PCEC is now widely used.
- It is cheaper
- It contains BPL inactivated flurry LEP strain
- Purified Vero cell vaccine [PVC]
- This vaccine is under study
- Human diploid cell strain vaccine [HDCS]
Question 9. Kyasanur forest disease
Answer:
- It is a tick-borne haemorrhagic fever that occurs in Agar and Sorab, Shikarpur talukas of Shimoga district in Karnataka state
- It is locally known as monkey fever as it infects mon¬keys also
- But infection in monkeys is fatal
Kyasanur Forest Disease Causative Organism:
- It is caused by the Russian Spring-Summer Encephalitis ( RSSE) Complex
- Forest birds, and small mammals are the reservoir hosts
- Principal vector is Haemaphysalis spinigera
Kyasanur Forest Disease Clinical Features:
- Sudden onset with fever, headache, conjunctivitis, myalgia and severe prostration
- Some may develop haemorrhages in the skin, mucosa and viscera
Question 10. Japanese Encephalitis
Answer:
Japanese Encephalitis Causative Organism:
- Japanese encephalitis virus causes Japanese B encephalitis.
- The virus in one of the mosquito-borne groups of valve viruses.
- Culex tritaeniorhyncus – Principal vector
- Herons – Reservoir hosts.
- Pigs – Amplifier hosts.
Japanese Encephalitis Clinical Features:
- The disease typically has an abrupt onset with fever, headache and vomiting.
- The fever is high and continuous.
- The majority of infections are asymptomatic.
- After 1-6 days signs of encephalitis set in with nuchal rigidity, convulsions, altered sensorium and coma.
- The majority of infections are asymptomatic.
- After 1-6 days, signs of encephalitis set in with nuchal rigidity, convulsions, altered sensorium and coma.
Japanese Encephalitis Laboratory Diagnosis:
- There is neutrophil leucocytosis in the peripheral blood
- Pleocytosis with normal (or raised sugar and slightly raised protein in the CSF.
Japanese Encephalitis Immunisation:
- A formalin-inactivated mouse brain vaccine produced by using the Nakayama strain has been successfully used for human immunization in Japan and even in India also.
- 2 doses at 2-week intervals, followed by a booster 6 – 12 months later, constitute a full course.
- Subsequent booster doses are recommended every 3 – 4 years as the immunity produced by the vaccine is short-lived.
Medically Important RNA Viruses Notes PDF
Question 11. Human papillomaviruses [HPV]
Answer:
- Human papillomaviruses belong to the papovaviruses.
- These are small, non-enveloped. Icosahedral oncogenic DNA viruses.
- It can cause cutaneous warts, genital warts, recurrent respiratory papillomatosis, and oral papillomatosis.
- These infections are transmitted by indirect or direct contact, including sexual contact.
- An association between HPV infection (HPV types 16 and 18) and cancer of the uterine cervix.
Question 12. Viruses cause diarrhoea.
Answer:
- Diarrhoea is defined as an increase in the frequency, fluidity or volume of bowel movements relative to the usual habits of an individual.
- Viruses causing diarrhoea include.
- Rotavirus
- Norwalk virus
- Adenovirus
- Astrovirus
- Coronavirus
- Calicivirus
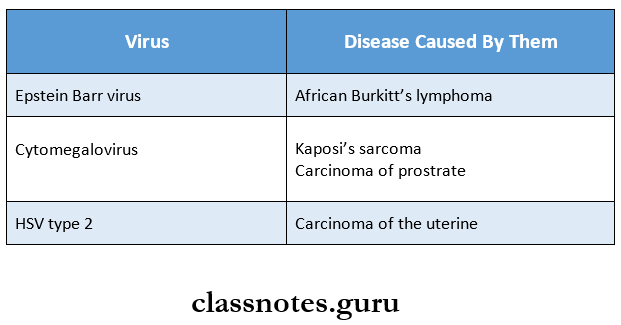
Question 13. Oncogenic herpes viruses
Answer:
Oncogenic herpes viruses cause various malignant diseases.
Question 14. Name oncogenic viruses
Answer:
The various Oncogenic viruses are as follows:
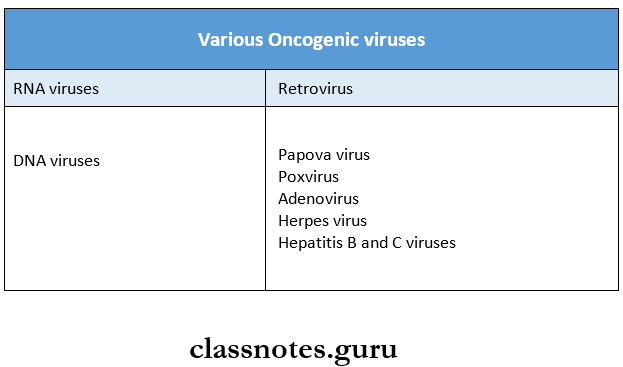
Question 15. Oncogenic RNA viruses
Answer:
- Oncogenic RNA viruses belong to the Retroviruses, which are enveloped, spherical viruses
- They develop by budding through the host cell membrane
- It contains the enzyme RNA-dependent DNA polymerase or reverse transcriptase within the virion
- It is classified into three subfamilies as follows
- Oncovirinae
- Spumavirinae
- Lentivirinae
- These viruses induce tumours by
- Introducing into the cellular genome or by
- Inducing or altering the expression of a pre-existing cellular gene.
Virology Essay on RNA Viruses for NEET PG / AIIMS
Question 16. MMR.
Answer:
- It is a live viral vaccine
- It is used for Mumps, Measles and Rubella
- It provides effective protection for 10 years
- It is recommended for all infants at the age of 15 months, followed by a booster at the age of 4-6 years.
Side Effects Of MMR vaccine:
- Sore arm
- Fever
- Mild rash
- Temporary pain and stiffness in joints
