Diseases Of The Respiratory System Long Essays
Question 1. Describe the causes of bronchitis and chronic bronchitis and their clinical features, complications, and management.
Answer:
Bronchitis:
- Bronchitis is an inflammation of the bronchi leading to increased bronchial secretions and airway obstruction
Bronchitis Causes:
- Smoke, atmospheric, and industrial pollutants
- These are atmospheric pollutants
- They damage the protective mucosal barrier of the nose
- Results in hypertrophy of mucus-secreting glands
- Infection
- It acts as a precipitating factor
- Physical factors
- Sudden change in temperature and exposure to fog leads to acute attacks of bronchitis
- Genetic and familial
- Alpha 1 antitrypsin deficiency leads to bronchitis
Bronchitis Management:
- Removal of etiological factors
- Avoid smoking
- Avoid exposure to pollutants
- Treatment of infection
- Antibiotics used are:
- Oxytetracycline or ampicillin 250-500 mg after every 6 hours for 5-7 days
- Cotrimoxazole- 960 mg tablets for 5-7 days
- Antibiotics used are:
- Bronchodilators
- Oral theophylline- 150 mg BID is used
- Inhaled beta-2 adrenoreceptor stimulants- salbutamol 200 mg every 6 hours is used
- In severe cases, ipratropium bromide- 40-80 meg every 6 hours is used
- Mucolytic agents
- These include bromhexine and carbocystein
- Corticosteroids
- Prednisolone 30 mg/day for 2 weeks is used
- Oxygen therapy
Respiratory system disorders long answer
Chronic Bronchitis:
- Chronic Bronchitis is defined as a cough with expectoration on most days at least three consecutive months in a year for more than two consecutive years
Bronchitis Clinical Features:
- Productive cough
- Dyspnoea
- Wheezing
- Occasionally chest pain, fever, and fatigue
- Hemoptysis- the presence of blood streaks in sputum
- Complications:
- Type 1 and 2 respiratory failure
- Pulmonary arterial hypertension and corpulmonale
- Secondary infections
- Secondary polycythemia
Question 2. Describe clinical features and management of bronchial asthma.
(or)
Discuss the etiology, clinical features, investigations, and management of bronchial asthma.
Answer:
Bronchial Asthma:
- Bronchial Asthma is a disease of the airway in which there is chronic inflammation and increased responsiveness to a variety of stimuli leading to reversible airway obstruction.
Etiology:
- Etiology is caused by various allergens, which are
- Most common
- Pollens, house dust, feathers, animal dander, insect web, fungal spores, etc.
- Less common
- Ingestion in predisposed individuals like fish, meat, milk, yeast, and wheat
Bronchial Asthma Clinical Features:
- Symptoms may be episodic or persistent
- Episodic asthma
- Sudden in onset
- Triggered by allergens, exercise
- Attacks may be spontaneous
- Duration varies from a few hours to days and even two weeks
- Characterized by wheezing, cough, and dyspnoea
- Between attacks, the patients are usually asymptomatic
- Acute severe asthma
- It is a severe life-threatening attack of asthma
- The patient may have tachycardia, cyanosis, and active accessory respiratory muscles
- Chronic asthma
- Triad of symptoms- chest tightness, wheeze or cough, and exertional dyspnoea occurs
- Cough is productive
- A prominent wheeze is audible
- Breath sound is harsh vesicular with prolonged expiration
Pathophysiology of respiratory diseases essay
Read And Learn More: General Medicine Question and Answers
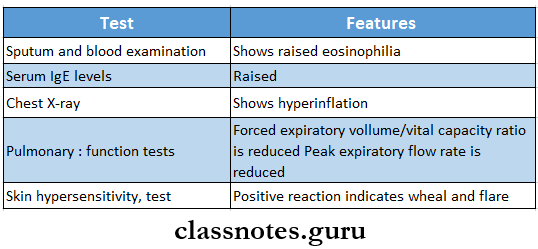
Bronchial Asthma Investigations:
Bronchial Asthma Management:
- Management Of Acute Asthma
- Avoidance of allergens
- Avoid allergens that may aggravate asthmatic attack
- Avoidance of allergens
- Hyposensitisation
- Prevention of mediators of bronchoconstriction
- Sodium cromoglycate is administered by inhalation
- Useful in some cases of non-atopic asthma
- Drug treatment
- Use of salbutamol or terbutaline 100-200 meg is used
- Use of beclomethasoneupto 800 meg twice a day is used along with it
- A high dose of corticosteroids is used along with bronchodilators.
Respiratory diseases long questions with answers
Question 3. Describe the etiology, clinical features, and management of ARDS.
Answer:
Acute Respiratory Distress Syndrome- ARDS:
- It describes the acute, diffuse pulmonary inflammatory response to either direct or indirect blood-borne insults.
Etiology:
- Direct-Inhalation
- Aspiration of gastric contents
- Toxic gases/ bum injury
- Pneumonia
- Blunt chest trauma
- Indirect-Blood Borne
- Necrotic tissue
- Multiple trauma
- Pancreatitis
- Severe bums
- Drugs
- Major blood transfusion reacion
- Anaphylaxis
- Fat embolism
Acute Respiratory Distress Syndrome Clinical Features:
- Neutrophil sequestration in pulmonary capillaries
- Increased capillary permeability
- Protein-rich pulmonary edema
- Alveolar collapse
- Progressive pulmonary fibrosis
- Multiple organ failure
Acute Respiratory Distress Syndrome Management:
- General
- Mechanical ventilation through
- Oro-tracheal intubation
- Tracheostomy
- Antibiotic therapy to treat infection
- Mechanical ventilation through
- Mechanical ventilation
- For it, three parameters are used
- Positive end-expiratory pressure- to maintain maximal recruitment of alveolar units
- Mean airway pressure- to promote recruitment and predictor of hemodynamic effects
- Plateau pressure- predictor of alveolar overdistention
- For it, three parameters are used
- Fluid management
- By diuresis or fluid restriction
- Corticosteroids
- Methylprednisolone 2 mg/kg daily is used for 3-5 days
- The dose is then tapered to 0.5-1 mg daily
Question 4. What is pneumothorax? What are the causes of pneumothorax? How do you manage tension pneumothorax?
Answer:
Pneumothorax:
- The presence of air in the pleural cavity is known as pneumothorax
Pneumothorax Causes:
- Rupture of subpleural blebs at the lung apices
- Rupture of emphysematous bullae
- Rupture of a subpleural tuberculous focus
- Rupture of lung abscess
- Pulmonary infarction
- Bronchial asthma
- Acute respiratory distress syndrome
- Sarcoidosis
Pneumothorax Management:
- Introduction of a wide-bore plastic cannula, one end is attached to a long rubber tubing, and the other is placed underwater in a bottle
- Another method is the introduction of an intercostal catheter connected to a water seal drainage system
Respiratory diseases classification long form
Question 5. Describe pneumonia, Bacterial Pneumonia, complications, clinical features, and treatment of community-acquired pneumococcal pneumonia.
Answer:
Pneumonia:
- Pneumonia is defined as an inflammation of the parenchyma of the lung.
Pneumococcal Pneumonia
- Pneumococcal Pneumonia is characterized by the homogeneous consolidation of one or more lobes or segments
Bacterfial Pneumonia:
- Etiology:
- Streptococcal pneumonia Staphylococcal Aureus
- Mycoplasma
- Streptococcus pyrogens
Bacterial Pneumonia Complications:
- Para pneumonic pleural effusion or Empyema
- Lpbar collapse
- Pneumothorax
- Lung abscess
- Hepatitis, meningitis
- Pericarditis
- Myocarditis
- Septicaemia
Bacterial Pneumonia Clinical Features:
- It is sudden in onset
- Fever with chills and rigors occurs
- Vomiting
- Convulsions
- Loss of appetite
- Headache
- Breathlessness
- Chest pain
- Central cyanosis
- Haemoptysis
- Weakness
- Tachycardia, tachypnoea
- Productive cough
- Rust-colored sputum
- Rapid and shallow breathing
Bacterial Pneumonia Management:
- Oxygen therapy
- Delivered in high concentration through masks
- Analgesics
- Pethidine-50-100 mg or morphine 10-15 mg is given intramuscularly
- Antibiotics
- Oral amoxicillin 500 mg 8 hourly or
- Erythromycin 500 mg 6 hourly or
- Oral cephalosporin 250 mg 8 hourly
- Cotrimoxazole 960 mg 2 times daily orally
- Physiotherapy
- The patient is encouraged to cough and take a deep breath
Respiratory tract infections long answer questions
Question 6. Describe etiopathology, clinical features, complications, diagnosis, and treatment of lobar pneumonia
Answer:
Lobar Pneumonia:
- Lobar pneumonia is a radiological and pathological condition referring to the homogenous consolidation of one or more lung lobes associated with pleural inflammation
Etiopathology:
- Etiopathology is caused by viruses, bacteria, fungi and parasites
Lobar Pneumonia Clinical Features:
- Sudden or insidious onset
- Fever with chills and rigors
- Headache
- Productive cough
- Breathlessness
- Chest pain
- Nausea, vomiting, diarrhea
- Myalgia, arthralgia
Lobar Pneumonia Complications:
- Para pneumonic pleural effusion
- Emphysema
- Lung abscess
- Acute Respiratory
- Distress Syndrome
- Pneumothorax
- Hepatitis
- Multiorgan failure
- Formation of ectopic abscess
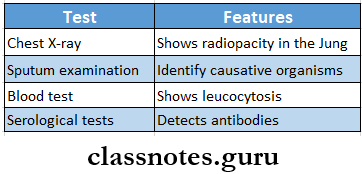
Lobar Pneumonia Diagnosis:
Lobar Pneumonia Treatment:
- Oxygen therapy
- High-concentration oxygen is delivered through masks
- Intravenous fluid administration
- Antibiotic therapy
- Duration of treatment-10-14 days
- Drugs used are:
- Ceftriaxone 1-2 g/day plus macrolide or fluoroquinolone
Pneumonia – etiology, clinical features and management
Question 7. Define and classify pneumonias. Describe the investigations, complications, and treatment of community-acquired pneumonia.
Answer:
Definition: Pneumonia is defined as an inflammation of the parenchyma of the lung.
Community-Acquired Pneumonia Classification:
- Pneumonia is classified into four types
- Lobar pneumonia
- Generally, the entire lobe of the lung is involved
- Bronchopneumonia
- There is neutrophilic exudate in the bronchi and bronchiole with the peripheral spread of infection to alveoli
- Interstitial pneumonia
- There is predominant involvement of the in-interstitium, alveolar wall, and connective tissue around the broncho-vascular tree
- Military pneumonia
- Occurs due to the homogenous spread of pathogens to the lungs
Community-Acquired Pneumonia:
- It is acquired by inhalation of infected oropharyngeal secretions
- Caused specifically by highly virulent organisms
Community-Acquired Pneumonias Classification Investigations:
Community-Acquired Pneumonia Classification Complication:
- Persistent fever
- Emphysema
- Proximal bronchial obstruction
- Recurrent aspiration
Pulmonary tuberculosis long essay
Question 8. Describe the clinical features of pulmonary tuberculosis, and write short-term chemotherapy.
Answer:
Pulmonary Tuberculosis:
- Tuberculosis is a chronic infective disorder produced by mycobacterium tuberculosis characterised by the formation of granulomas and the development of cell-mediated hypersensitivity
- The involvement of the lungs by tuberculosis is called pulmonary tuberculosis
Pulmonary Tuberculosis Clinical Features:
- Loss of weight
- Loss of appetite
- Fever with night sweats
- Tiredness, malaise
- Amenorrhoea
- Cough with purulent sputum
- Haemoptysis
- Chest pain
- Breathlessness
- Finger clubbing
- Distended neck and chest veins
- Pleural effusion
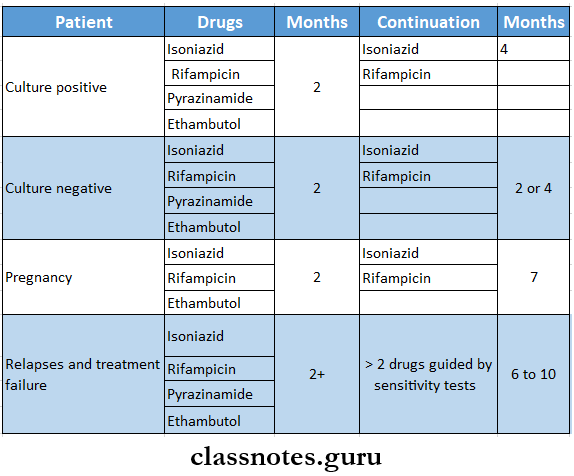
Chemotherapy Of Tuberculosis
Question 9. Describe the diagnosis, complications, and management of post-primary tuberculosis
Answer:
Post-Primary Tuberculosis:
Post-Primary Tuberculosis Complications:
- Haemoptysis
- Pneumothorax
- Secondary infection of the cavity
- Pleural effusion
- Emphysema
- Pulmonary fibrosis
- Scar carcinoma
- Respiratory failure
- Amyloidosis
- Anaemia
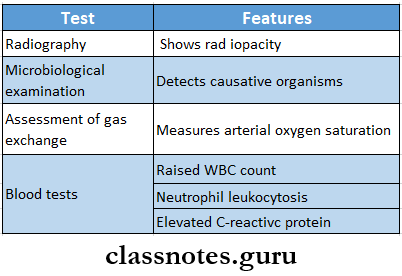
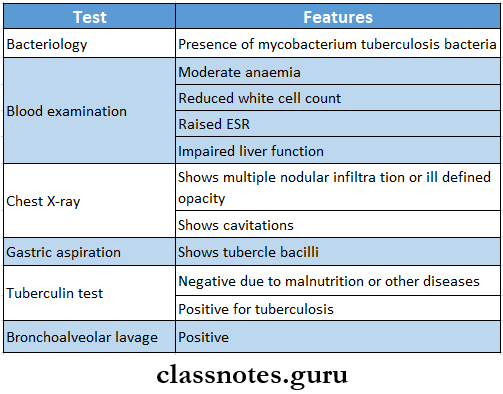
Post-Primary Tuberculosis Investigations:
Lung cancer classification and treatment long answer
Question 10. Describe the etiology, clinical features, and treatment of bronchial obstruction.
Answer:
Bronchial Obstruction:
- Bronchial Obstruction is called bronchiectasis
- Bronchial Obstruction is defined as an abnormal and irreversible dilatation of bronchi
Etiology:
- Infective causes
- Bacterial- H. influenzae, staphylococcus aureus, E. coli, Tuberculosis, mycoplasma
- Viral- measles, adenovirus, influenza virus
- Fungal
- Obstructive causes
- Endobronchial benign neoplasm
- Foreign body aspiration
- Chronic bronchitis
- Enlarged lymph nodes
- Noninfective causes
- Allergic
- Cystic fibrosis
Bronchial Obstruction Clinical Features:
- Chronic cough with massive expectations
- Haemoptysis
- Recurrent pulmonary infection
- Dyspnoea
- Fever, weight loss, anemia, and weakness
- Oedema
- Sepsis
Bronchial Obstruction Treatment:
- Physiotherapy
- To keep bronchi dilated
- Antibiotic therapy
- Ampicillin- 500 mg 8 hourly or
- Amoxycillin 500 mg 8 hourly or
- Oral cefaclor 250 mg 8 hourly
- Bronchodilators and nuicolytics
- Bronchodilators used are theophylline or terbutaline
- Mucolytics used arc bromhexine, carboys- teenie
- Surgery- indications
- Those who do not respond to medical therapy
- Those who have repeated massive hemoptysis
- Young patients
- Unilateral bronchiectasis
Respiratory disorders long essays for nursing students
Question 11. Describe the pathogenesis, clinical features, and diagnosis of lung abscess.
(or)
Write etiopathogenesis, clinical features, and treatment of lung abscesses.
Answer:
Bronchial Obstruction Lung Abscess:
- Bronchial Obstruction Lung Abscess is a collection of purulent material ilocalizedised necrotic area of lung parenchyma
Etiopathogenesis:
- Infection without obstruction
- Aspiration of nasopharyngeal contents
- Involvement of various organisms like staphylococcus, Kleibsella, gram-negative and anaerobic organisms
- Formation of abscess
- Metastatic spread of infection
- Obstruction with or without infection
- Bronchus obstruction due to tumor, foreign body, lymph node
- Bronchial collapse
- Abscess formation
Bronchial Obstruction Clinical Features:
- High-grade fever with chills and rigors
- Pleuritic chest pain
- Dry cough
- The presence of copious purulent discharge
- Haemoptysis
- Weight loss, anorexia
- Emphysema
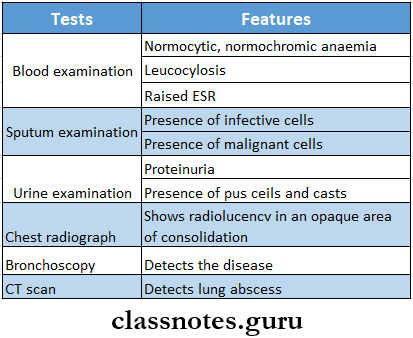
Bronchial Obstruction Investigations:
Bronchial Obstruction Management:
- Postural drainage and chest physiotherapy
- Antibiotic therapy
- Oral amoxicillin 50 mg 8 hourly for 5-7 days
- Cotrimoxazole 960 mg twice daily
- Oral metronidazole 400 mg 8 hourly
- Surgery
- Resection of part of the lung is done
- Indications:
- Massive hemoptysis
- Localized malignancy
- Associated symptomatic bronchiectasis
- Persistent abscess cavity
Obstructive vs restrictive lung disease long essay
Question 12. Describe the etiology, clinical features, investigations, and management of pulmonary eosinophilia.
Answer:
Pulmonary Eosinophilia:
- Pulmonary Eosinophilia is a lesion in the lungs associated with blood eosinophilia
Etiology:
- Parasitic infections- hookworm disease, ascariasis, strongyloidiasis
- Allergic conditions- Hay fever, asthma, drugs like aspirin, aspergillosis
- Skin disorders- eczema, dermatitis herpetiform
- Tumors- lymphoma
- Collagen vascular disorders- rheumatoid arthritis, polyarteritisnodosa
- Hypereosinophilic syndromes- Loeffler’s syndrome, idiopathic
- Miscellaneous- Sarcoidosis, Addison’s disease
Pulmonary Eosinophilia Clinical Features:
- Dyspnoea or orthopnoea
- Wheezing
- Cough with mucoid expectoration
- Haemoptysis
- Types
- Cryptogenic eosinophilic pneumonia
- Idiopathic eosinophilic syndromes- includes
- Loeffler’s syndrome
- Hypereosinophilic syndrome
- Churg Strauss syndrome
- Tropical pulmonary eosinophilia
Pulmonary Eosinophilia Diagnosis:
- Blood examination- High blood eosinophils count
- Sputum shows eosinophilia
- X-ray of the chest shows diffuse miliary mottling of the lungs
Pulmonary Eosinophilia Treatment:
- Diethylcarbamazine- 2 mg/kg three times a day is used
- Allergic reactions are controlled by the use of antichrist-mimics and steroids
