Oral Medicine Red And White Lesions Long Essays
Question 1. Classify red and white lesions of the oral cavity. Write etiology, clinical features, and management of oral submucous fibrosis and candidiasis.
Answer.
Oral Cavity Classification:
- Red lesions:
- Inflammatory Conditions:
- Inflammation associated with traumatic injury
- Mechanical- cheek biting, ill-fitted denture
- Chemical- aspirin, formoterol
- Thermal- hot food, hot beverages
- Radiation- mucositis
- Infection
- Bacterial
- Scarlet fever
- Gonococcal stomatitis
- Vincent infection
- Fungal
- Atrophic candidiasis
- Angular cheilitis
- Viral
- Measles
- Herpes simplex infection
- Herpes zoster
- Herpangina
- Chickenpox
- Allergic
- Pyogenic granuloma
- Giant cell epulis
- Pregnancy tumor
- Congenital:
- Hemangioma
- Sturge-Weber syndrome
- Median rhomboid glossitis
- Geographic tongue
- Vascular Diseases:
- Purpura
- Polycythemia
- Agranulocytosis
- Leukemia
Read And Learn More: Oral Medicine Question and Answers
- Dermatological:
- Pemphigus
- Erythema multiforme
- Steven Johnson’s syndrome
- Lichen planus
- Psoriasis
- Other Diseases:
- Uremic stomatitis
- Diabetes stomatitis
- Scurvy
- Pernicious anemia
- Premalignant And Malignant Lesions:
- Atrophic leukoplakia
- Erythroplakia
- Carcinoma in situ
- Kaposi’s sarcoma
2. White Lesions:
- Variation In Structure And Appearance Of Normal Mucosa
- Leukoedema
- Fordyce’s granules
- Linea alba
- A White Lesion With Precancerous Potential
- Leukoplakia
- Erythroplakia
- Lupus erythematous
- Carcinoma in situ
- Lichen planus
- White Lesion Without Precancerous Potential
- Traumatic lesions
- Focal epithelial dysplasia
- White sponge nevus
- Stomatitis nicotine
- Hairy leukoplakia
- Nonkeratotic Lesion
- White hairy tongue
- Burns
- Pemphigus
- Desquamative gingivitis
- Candidiasis
- Koplik’s spots
Oral Submucous Fibrosis:
- An insidious chronic disease affecting any part of the oral cavity and sometimes the pharynx.
- Although occasionally preceded by and /or associated with vesicle formation, it is always associated with juxtaepithelial inflammation reaction followed by fibroelastic changes of lamina pro¬pria with epithelial atrophy leading to stiffness of oral mucosa and causing trismus and inability to eat
Etiology:
- Use of chilies due to the presence of capsaicin in it
- Tobacco- acts as a local irritant
- Lime used along with betel nut
- Nutritional deficiency- Vitamin B complex deficiency
- Defective iron metabolism
- Bacterial infections
- Collagen disorders like scleroderma, rheumatoid arthritis
- Immunological disorders like raised ESR and globulin levels
- Altered salivary composition- Increase salivary pH, Increase salivary amylase, low levels of calcium, increase in alkaline phosphatase
- Genetic susceptibility
Oral Submucous Fibrosis Clinical Features:
- Age and sex: fourth-decade males are more affected
- Initially patient complaints of a burning sensation on having spicy and hot food
- It is followed by vesicle formation
- There may be excessive or reduced salivation
- Gradual stiffness of the mucosa occurs
- Oral mucosa becomes blanched
- Palpation of the mucosa reveals many vertical fibrous bands
- There may be difficulty in deglutition
- Referred pain in the ear
- Depapillation of tongue
- Restricted movement of the floor of the mouth
- Shrunken uvula
- Restricted mouth opening
Oral Submucous Fibrosis Management:
- Quit the habit
- Antioxidant- Oxyace-1 capsule/ day
- Multivitamin therapy
- Steroid- Betnovate 0.12%
- Tumeric application
- Intralesional injection of Hyaluronidase- 1500 U
- Physiotherapy
- Splitting of fibrous bands
- Laser
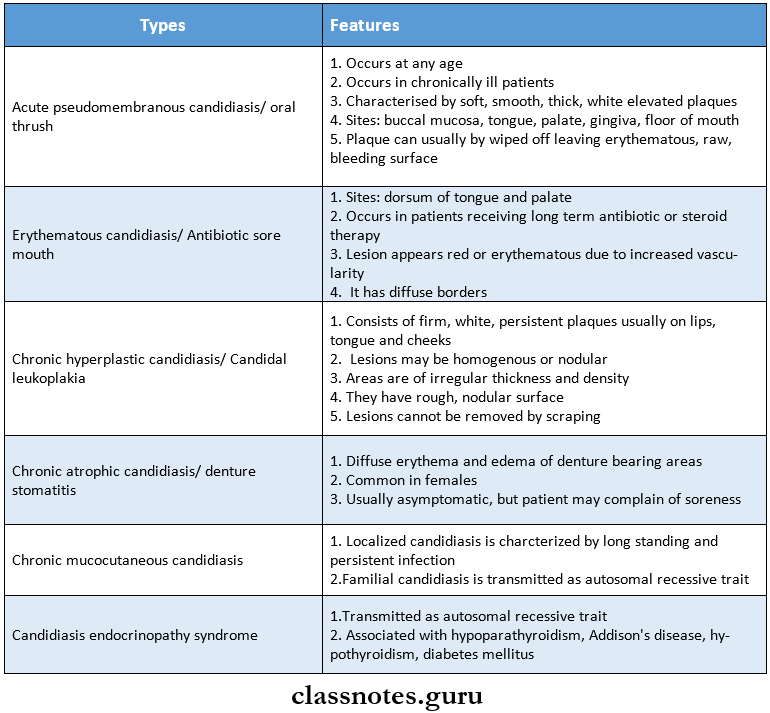
Oral Submucous Fibrosis Candidiasis:
- Candidiasis is the most common fungal infection of the oral cavity
Etiology/Causative Organisms:
- Candidiasis is caused by
- Mainly Candida albicans
- Other species- C.tropicalis, C.glabrata, C. Krusie, C.pscudotropicalia
Causative Organisms Clinical Features:
Candidiasis may range from mild superficial mucosal involvement to severe, fatal, disseminated form
Causative Organisms Management:
1. Removal Of Causative Agents
- Replacement or relining of denture
2. Topical Applications
- Clotrimazole- oral troche- 10 mg tablet dissolved in mouth five times daily
- 1% gentian violet
- Nystatin preparations
- Vaginal tablets- one tablet, 1,00,000 units dissolved in mouth 3 times a day
- Oral pastilles 2,00,000 units dissolved slowly in mouth 5 times a day
- Oral suspension- 1,00,000 units/cc, 1 teaspoon is mixed with 1/4 cup of water, used as an oral rinse
- Amphotericin B- 0.1 mg/ml used as rinse
- Mycostatin cream- 1 lac unit or lactose-containing vaginal tablet
3. Systemic Treatment
- Nystatin- 250 mg TDS for 2 weeks followed by 1 troche per day for the third week
- Ketoconazole- 200 mg tablet once daily
- Fluconazole-100 mg tablet once daily for 2 weeks
- Itraconazole-100 mg capsules for 14 days.

Question 2. Enumerate oral precancerous lesions and discuss differential diagnosis of oral leukoplakia
Answer:
Precancerous Lesions:
- It is defined as morphologically altered tissue in which cancer is more likely to occur than its normal counterparts
- For example,
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowens disease
- Actinic keratosis
Differential Diagnosis Of Leukoplakia::
1. Lichen Planus
- There is the presence of Wickham’s striae
2. Chemical Burn
- Gives a history of burn
- Painful lesion
- Appears as an irregularly shaped, white pseudonym-brane-covered lesion
- Gentle lateral pressure causes the white material to slide away exposing painful central red ulceration
3. Syphilitic Mucous Patches
- Presence of split papule or condyloma latum
4. White Sponge Nevus
- White Sponge Nevus occurs soon after birth or at least by puberty
- White Sponge Nevus is widely distributed over the oral mucous membrane
- The familial pattern is seen
5. Discoid Lupus Erythematosus
- Central atrophic area with a small white dot and slightly elevated border zone or radiating white striae
6. Psoriasis
- Positive Au spitz’s sign
- Skin lesions are present
7. Leukoedema
- Occurs on buccal mucosa covering most of the oral surface of the cheek and extending onto labial mucosa
- The presence of a faint milky appearance with a folded and wrinkled pattern
8. Hairy Leukoplakia
- Associated with AIDS patients
- Corrugated leukoplakic lesions occurring on the lateral and ventral surface of the tongue
9. Verruca Vulgaris
- Commonly occurs in the oral cavity as a small,, raised white lesion, more than 0.5 cm in diameter
10. Verrucous Carcinoma
- Lesions are elevated
11. Cheek Biting Lesion
- The presence of local irritants as a causative factor
- Removal of cause relieves the condition
12. Electrogalvanic White Lesion
- Disappears when different metal restorations are replaced with composite restorations
Question 3. Define premalignant lesion conditions. Describe oral lichen planus in detail.
Answer:
Premalignant Lesion:
- It is defined as morphologically altered tissue in which cancer is more likely to occur than its nor¬mal counterparts
- For example,
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen’s disease
- Actinic keratosis
Preremalignant Condition:
- It is defined as a generalized state or condition associated with a significantly increased risk for cancer development
- For example:
- Oral submucous fibrosis
- Syphilis
- Sideropenic dysplasia
- Dyskeratosis congenital
- Lupus erthymetosis
Oral Lichen Planus:
- Oral Lichen Planus is a relatively common dermatological disorder occurring on skin and oral mucous membranes and refers to lace-like patterns produced by symbolic algae and fun-gal colonies on the surface of rocks in nature
Etiology:
- Cell-mediated immune response:
- It is associated with wadi lymphocyte epidermal interactions
- Autoimmunity:
- The activated T lymphocytes also secrete gamma interferon which induces keratinocytes to increase differentiation
Immune deficiency:
- There is decreased serum levels of IgG, IgA, or IgM in lichen planus
Genetic factor:
- Oral Lichen Planus has a familial trait
Infection:
- Oral Lichen Planus may be caused due to Spirochetes and rod-like bodies
Psychogenic Factor
- Stress may be related to the occurrence of lichen planus
Habits:
- Oral Lichen Planus Is associated with tobacco chewing and betel nut chewing habits
Miscellaneous:
- Oral Lichen Planus Is associated with deficiency of Vitamin HI, HO, and C and also associated with electric potential difference, anemia, and patient with secondary syphilis
Oral Lichen Planus Types:
- Reticular
- Papular
- Plaque
- Atrophic
- Classical
- Erythematous
- Ulcerative
- Hypertrophic
- Erosive
- Bullous
- Annular
- Actinic
- follicular
- Linear
Oral Lichen Planus Clinical Features:
- Site:
- Buccal mucosa
- Tongue
- Lips
- Gingiva
- The floor of the mouth
- Palate
- Presentation
- Initially, there is a burning sensation of the oral mucosa
- It appears as radiating white and grey velvety thread-like papules in a linear, angular or retiform arrange¬ment forming typical lacy, reticular patterns, rings, and streaks
- Wickham’s striae- tiny white elevated dots are present at the intersection of white lines
- It may be superimposed to candidal infections
Oral Lichen Planus Types Explanation:
- Reticular Type:
- It is bilateral
- It consists of slightly elevated fine whitish lines that produce lace-like patterns
- Papular Type:
- Whitish elevated lesions of 0.5-1 mm in size
- It is well seen in keratinized areas
- They are seen at the periphery of the reticular pattern
- Plaque Type:
- It is soon on the dorsum of the tongue and buccal mucosa
- It loads lo disappearance of papillae
- It spreads In concentric peripheral growth
- Atrophic Type:
- It appears a smooth, red, poorly defined area
- The attached gingival is frequently involved
- Patient may complain of pain and burning In the areas of Involvement
- Bullo Us Type:
- It consists of vesicles and bullae which are short-lived
- They rupture leaving an ulcerated surface
- Hypertrophic Form:
- It appears as a well-circumscribed, elevated white le¬sion resembling leukoplakia
- Annular Form:
- It appears as a round or ovoid, white outline with either pink or reddish-pink center
Oral Lichen Planus Differential Diagnosis:
- Leukoplakia:
- Absence of Wickham’s striae
- Candidiasis:
- Pseudomembrane can be rubbed off
- Lupus Erythematous:
- It has the feathery appearance of a lesion
Oral Lichen Planus Management:
- Removal of the causative agent
- Steroid therapy.
- Steroid spray.
- Use of beclomethasone dipropionate spray, triamcinolone acetonide in gel or cream form over small and moderately sized painful lesions
- Steroid coating:
- Some painful lesions are treated with topical application of topical steroids
- Topical delivery
- Prednisolone:
- 30 mg/day for the first week
- 15 mg/day for the second week
- 5 mg/day for the third and final week
- Intralesional injection of methylprednisolone 40 mg/ml
- Topical application of fluocinolone acetonide for 4 weeks
- Nystatin and ketoconazole for treating fungal infections
- Vitamin supplements
- Surgical therapy:
- Cryosurgery and cauterization
- Psychotherapy:
- Tranquilizers are tried to reduce anxiety
- Dapsone therapy:
- To control the lymphocytes-mediated progress of lichen planus
- PUVA therapy
- High-intensity long-wave ultraviolet (PUVA) light is used as a therapeutic agent
- Fluocinonide
- It is used as an adhesive base
- Symptomatic therapy
- As topical analgesic, topical anesthetic, and antihistaminic
Question 4. Classify white lesion. Describe in detail the etiology, classification, clinical features, and management of leukoplakia.
Answer:
White Lesion Classification:
1. Variation In Structure And Appearance Of Normal Mucosa
- Leukoedema
- Fordyce’s granules
- Linea alba
2. White Lesion With Precancerous Potential:
- Leukoplakia
- Erythroplakia
- Lupus erythematosus
- Carcinoma in situ
- Lichen planus
3. White Lesion Without Precancerous Potential
- Traumatic lesions
- Focal epithelial dysplasia
- White sponge nevus
- Stomatitis nicotine
- Hairy leukoplakia
4. Nonkeratotic lesion
- White hairy tongue of Burns
- Pemphigus
- Desquamative gingivitis
- Candidiasis
- Koplik’s spots
Leukoplakia Definition:
- Leukoplakia is a whitish patch or plaque that cannot be characterized, clinically or pathologically, as any other disease and which is not associated with any other physical or chemical causative agent except the use of tobacco.
Etiology:
- Tobacco
- Smokeless tobacco
- Smoking tobacco
- Alcohol
- Chronic irritation
- Candidiasis
- Galvanism
- Vitamin deficiency
- Xerostomia
- Nutritional deficiency
- Hormones: sex hormones
- Drugs: Anticholinergic, antimetabolic
- Virus: herpes simplex and HIV
- Idiopathic
Leukoplakia Clinical Features:
- Age and sex: in older age males it occurs commonly i.e in the age of 35-45 years
- Sites
- Buccal mucosa
- Commissures
- Lip
- Tongue
- Presentation
- Oral leukoplakia often represents solitary or multiple white patches
- They can be nonpalpable, faintly translucent, white areas over the mucosa
- Many lesions can be thick, fissured, indurated, or papillomatous in nature
- The size of the lesion varies from a small well-localized patch measuring about a few mm in diameter to a dif¬fuse large lesion, covering a wide mucosal surface
- The surface of the lesion may be smooth or finely wrinkled or even rough on palpation, and the lesion cannot be removed by scraping
- The lesions are usually white or grayish or yellowish-white in color and in some cases, due to the heavy use of tobacco, they may take a brownish-yellow color
- Some lesions may exhibit a pumice-like surface, which occurs due to the presence of multiple discrete keratotic striae, on the surface of these lesions
- Leukoplakia of the floor of the mouth sometimes has an ebbing tide pattern of appearance
- The thickness of the patch may vary from only faint to considerably thick
- In most of cases, these lesions are asymptomatic, however in some cases, they may cause pain, a feeling of thickness and a burning sensation, etc
- Leukoplakia Types:
- Homogenous leukoplakia
- Ulcerative leukoplakia
- Nodular or speckled leukoplakia
Staging Of Leukoplakia:
According To Size, Clinical Aspect, And Pathological Features
Size: It is denoted by L
- L1: size is less than 2 cm
- L2: size is in the range of 2-4 cm
- L3: size is more than 4 cm
- Lx: size is not specified
Clinical Aspect: it is denoted by C
- C1– homogenous
- C2– nonhomogenous
- Cx-not specified
Pathological Features: It is denoted by P
- P1– no dysplasia
- P2– mild dysplasia
- P3– moderate dysplasia
- P4– severe dysplasia
- Px– not specified
Site: it is denoted by S
- S1– all sites excluding floor of the mouth, tongue
- S2– floor of the mouth and tongue
- S3-not specified
Leukoplakia Management:
- Elimination of etiological factor
- Prohibition of smoking
- Removal of chronic irritants
- Elimination of other etiologic factors like syphilis, alcohol dissimilar metal restoration, etc
- Conservative treatment
- Vitamin therapy:
- Vitamin A: ‘3000 to 300000 H1 tor 3 months
- Vitamin A + Vitamin K therapy to inhibit metabolic degradation
- Nystatin therapy
- it is given o00000 ID twin’ daily pins .’0’V borax glycerol or t ‘V gentian violet or month rinses with chlorogenic solution
- Panthenol
- Lingual tablets and oral sprays may be used against glossitis and glossodynia
- Ksttvgen:
- it can be helpful
Surgical Management:
- Conventional surgery
- The affected area is undermined and disserted from the underlying tissue
- Sliding unusual dap is prepared for covering the wound
- After proper mobilization of the unusual dap, it is advanced, and multiple interrupted Mark silk sutures are used
- Post-operative application of ioehags at the sife is advised to minimize bleeding and swelling:
- Cryosurgery
- Tissue is exposed to extreme cold to produce irreversible cell damage
- Liquid nitrogen or pressurized nitrogen oxide is used at -d0” Celsius
- Fulguration
- It’s a technique in which there is the destruction of tissues by high voltage current and action is controlled by movable electrodes
Leukoplakia Laser:
- CO2 lasers are most commonly used in oral lesions due to their great affinity for any tissue with high water content and their minimum penetration depth. U\ tVd- 0. 3 mm in oral tissue
- It is used in the form of
- Biopsy
- Laser peel
- Ablation
Leukoplakia Miscellaneous:
- Radiation therapy is only used in neoplastic tissues
- Chemotherapeutic agents-
- Bleomycin and human fibroblast interferon are used
Question 5. Classify white lesion. Describe in detail the clinical features, differential diagnosis & management of oral submucous fibrosis.
Answer:
Classification Of White Lesions:
- Variation In Structure And Appearance Of Normal Mucosa
- Leukoedema
- Fordyce’s granules
- Linea alba
- A White Lesion With Precancerous Potential
- Leukoplakia
- Erythroplakia
- Lupus erythematosus
- Carcinoma in situ
- Lichen planus
- White Lesion Without Precancerous Potential
- Traumatic lesions
- Focal epithelial dysplasia
- White sponge nevus
- Stomatitis nicotine
- Hairy leukoplakia
- Nonkeratotic Lesion
- White hairy tongue
- Burns
- Pemphigus
- Desquamative gingivitis
- Candidiasis
- Koplik’s spots
Oral Submucous Fibrosis Clinical Features:
- Age And sex: Third – fourth-decade males are more affected
- Gradual stiffness of the mucosa occurs
- Oral mucosa becomes blanched
- Palpation of the mucosa reveals many vertical fibrous bands
- There may be difficulty in deglutition
- Referred pain in the ear
- Depapillation of tongue
- Restricted movement of the floor of the mouth
- Shrunken uvula
- Restricted mouth opening
Oral Submucous Fibrosis Differential Diagnosis:
- Scleroderma
- Chemical burns
Oral Submucous Fibrosis Management:
- Quit the habit
- Antioxidant- Oxyace- 1 capsule/ day
- Multivitamin therapy
- Steroid-Betnovate 0.12%
- Tumeric application
- Intralesional injection of Hyaluronidase- 1500 U
- Physiotherapy
- Splitting of fibrous bands
- Laser
