Periodontal Pocket
Periodontal Pocket Definition: Pathological deepening of the gingival sulcus
Periodontal Pocket Important Notes
1. Classification Of Pocket
- Depending upon its morphology
- Gingival/false pocket
- Periodontal/true pocket
- Combined pocket
- Depending upon its relationship to crustal bone
- Suprabony pocket
- Infrabony pocket
- Depending upon the no. of surfaces involved
- Simple
- Compound
- Complex
- Depending upon the nature of the soft tissue wall
- Edematous
- Fibrotic
- Depending upon disease activity
- Active
- Passive
Read And Learn More: Periodontics Question and Answers
Depending on depth:
- Deep pocket
- Shallow pocket
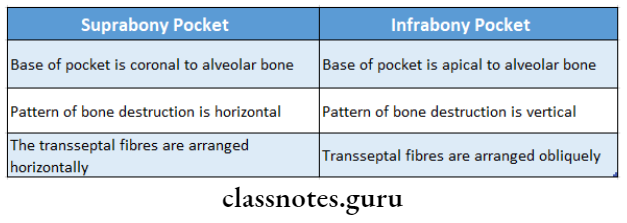
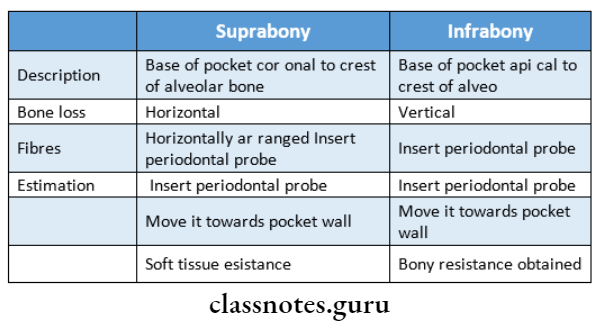
2. Suprabony And Infrabony Pockets
3. Periodontal Cyst
- Periodontal Cyst is an uncommon lesion occurring most often in the mandibular canine-premolar region
- Periodontal Cyst may develop from a dentigerous cyst, a primordial cyst of supernumerary tooth germ from stimulation of epithelial rests f periodontal ligament
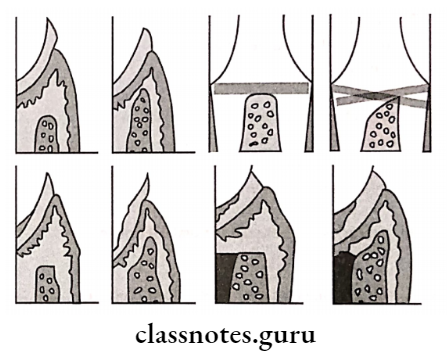
4. Simple, Compound, And Spiral Pocket
5. Acute Periodontal Abscess
- Purpose of treatment
- To alleviate pain
- Control the spread of infection
- Establish drainage
- Drainage can be establish
- Through pocket
- Through incision from the external surface
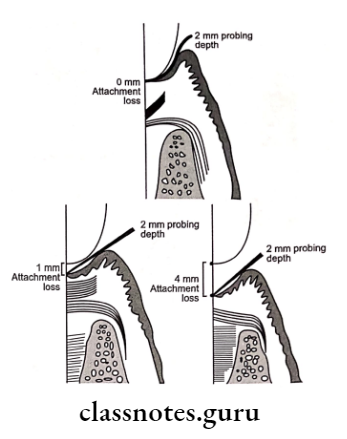
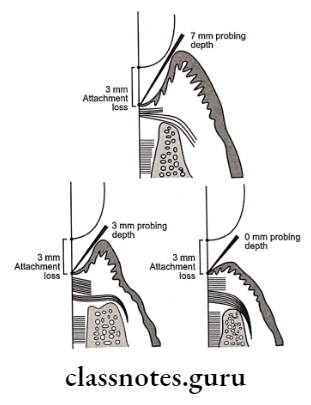
6. Types Of Pocket Depth
- Biologic/histologic depth
- The distance between the gingival margin and the base of the pocket
- Can be measured only in carefully prepared histologic sections
- Clinical/probing depth
- The distance to which the probe penetrates into the pocket
- The probing force is 25 pounds or 0.75 N.
7. Pus
- Pus is a common feature of periodontal disease
- Pus is not an indication of the depth of pocket or severity of periodontal destruction
- Pus reflects the nature of inflammatory changes in the pocket wall
Periodontal Pocket Long Essay
Question 1. Define and classify pocket. Describe its clinical features pathogenesis and treatment.
Answer:
Pocket Definition: Pathological deepening of the gingival sulcus
Pocket Classification:
1. Depending upon its morphology:
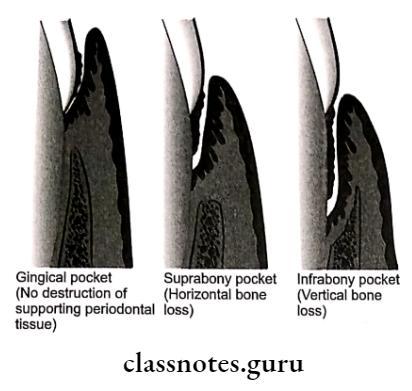
- Gingival/false pocket:
- Due to the bulk of gingiva
- No destruction of underlying periodontal tissues
- Periodontal/true pocket:
- Leads to the loosening and exfoliation of tissues
- Combined pocket:
2. Depending upon its relationship to the crustal bone:
- Suprabony pocket:
- The bottom of the pocket is coronal to the underlying bone
- Infrabony pocket:
- The bottom of the pocket is apical to the underlying bone
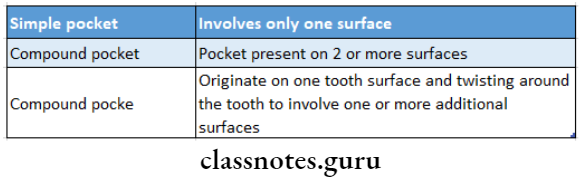
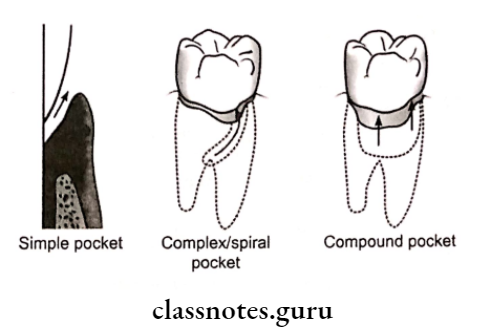
3. Depending upon the no. of surfaces involved:
- Simple: Involving one tooth surface
- Compound: Involving two/more tooth surfaces
- Complex: The base of the pocket is not in direct communication with the gingiva margin
4. Depending upon the nature of the soft tissue wall:
- Edematous: Due to inflammation
- Fibrotic
5. Depending upon disease activity:
- Active
- Passive
6. Depending on depth:
- Deep pocket
- Shallow pocket
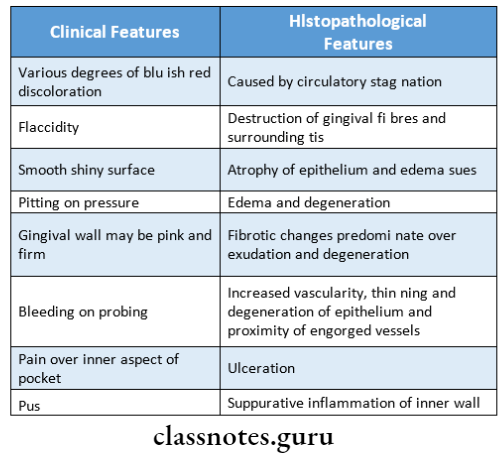
Pocket Features:
Gingiva:
- Color – bluish red
- Size – enlarged
- Surface – shiny, discolored
- Consistency-puffy
- Bleeding – Positive
- Purulent exudates – positive
- Bluish red vertical zone extending from marginal gingiva to alveolar mucosa
- Break in faciolingual continuity of gingiva
Teeth:
- Mobility
- Extrusion from socket
- Pathological migration
- Toothache
- Sensation of pressure
- Foul taste
- Radiating pain, gnawing feeling
- Thermal sensitivity
- Stickness of food
- Urge to dig
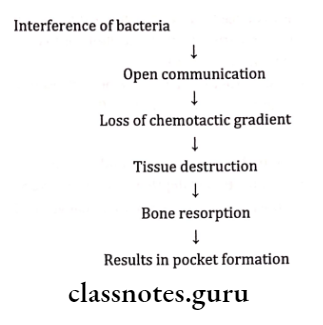
Pocket Pathogenesis:
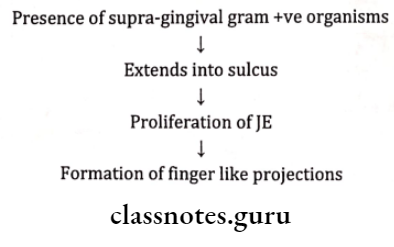
- Collagenase released by bacteria, phagocytes, and fibro-blast
- Forces by bacteria
- Exudation
Pocket Treatment:
1. Gingival pocket/False pocket:
- Scaling and root planning
- Recall
- If required gingivectomy/gingivoplasty
2. Periodontal pocket:
- Scaling and root planning
- Removal of pocket wall-Gingivectomy
- Hemisection
3. Suprabony pockets:
- Scaling and root planning
- Flap surgery
4. Infrabony pockets:
- New attachment procedures
- Nongraft associated
- Graft associated
- Combinations
Question 2. Discuss the contents of the periodontal pocket.
Answer:
Contents Of The Periodontal Pocket
- Micro-organisms and their product sections
- Enzymes
- Endotoxins
- Metabolic products
- Dental plaque, food remnants
- Gingival fluid
- Salivary mucin
- Serum
- Fibrin
- Cells
- Desquamated epithelial cell
- Leukocytes
- Degenerated and necrotic PMNs
- Pus formation
Question 3. Describe histopathology and sequels.
Answer:
Histopathology:
1. Changes in soft tissue wall:
- Blood vessels are engorged and dilated
- Connective tissue is edematous and densely infiltrated with plasma cells, lymphocytes, and PMNs
- Degeneration and necrosis of epithelium leading to ulceration of epithelium
- Bacterial invasion along the lateral and apical areas of the pocket
- The epithelial projection extends deep into the connective tissue
2. Microtopography of a gingival wall of the pocket:
- 7 areas are identified
- Area of relative quiescence
- Area of bacterial accumulation
- Area of leukocytes
- Area of bacterial leukocyte interaction
- Area of epithelial desquamation – Area of ulceration
- Area of hemorrhage
3. Periodontal pocket as healing lesion:
- Characterized by destructive and constructive tissue changes
- Destructive changes are characterized by fluid and cellular inflammatory exudates
4. Changes in root surface wall:
- Structural changes:
- Presence of pathogens
- Areas of increased mineralization
- Areas of root caries
- Chemical changes:
- Increased calcium, magnesium, phosphate, and fluoride
- Cytotoxic changes:
- Bacterial penetration
- Presence of endotoxins
Sequel:
- Inflamed gums with damaged fibers
- Bone destruction
- Exposed root surfaces
Question 4. Define periodontal pocket. Classify periodontal pockets. Discuss briefly the root surface wall of the pocket.
Answer:
Root Surface Wall Changes:
Structural:
- Presence of pathogens
- Areas of increased mineralization
- Areas of root caries
- Chemical – Increased Calcium, Magnesium, Phosphate,
- Cytotoxic – Bacterial penetration, Presence of endotoxin-ins
Zones:
- Cementum
- Attached plaque
- Unattached plaque
- Junctional epithelium
- Partially lysed CT fibers
- Intact CT fibers
- Constant probing depth with different levels of attachment loss
Periodontal Pocket Short Essays
Question 1. Differentiate supra bony and inf ebony pockets.
Answer:
Question 2. Periodontal Cyst.
Answer:
- Localized destruction of the periodontal tissues along the lateral root surface
- Site: Common mandibular canine premolar area
Periodontal Cyst Etiology:
- Odontogenic cyst
- Dentigerous cyst
- Primordial cyst
- The proliferation of epithelial cells rest of molasses
Periodontal Cyst Features:
- Asymptomatic
- Localized
- Tenderness
Periodontal Cyst Radiographic Feature:
- Radiolucent lesion bordered by a radiopaque line
Periodontal Cyst Treatment:
- Scaling and root planning
- Drainage
Question 3. Changes of root surface wall of the pocket.
Answer:
- Structural
- Presence of pathogens
- Areas of increased mineralization
- Areas of root caries
Chemical: Increased Calcium, Magnesium, Phosphate, and Fluoride
Cytotoxic: Bacterial penetration, Presence of endotoxins
Zones:
- Cementum
- Attached plaque
- Unattached plaque
- Junctional epithelium
- Partially lysed CT fibers
- Intact CT fibers
Question 4. Classify periodontal pockets. Treatment of pseudopockets.
Answer:
Pseudopockets Treatment:
- Scaling
- Oral hygiene instructions are given
- Patients on antiepileptic drugs, calcium channel blockers or immune suppressants should consult a physician for alternative drugs
- Procedures like gingivectomy and gingival curettage are done
Question 8. Correlation of clinical and histopathological features of a periodontal pocket
Answer:
Periodontal Pocket Short Answers
Question 1. Periodontal disease activity
Answer:
According to the concept of periodontal disease activity, periodontal pockets go through periods of exacerbation and quiescence.
1. Period of quiescence:
- Characterized by a reduced inflammatory response
- There is little or no loss of bone and connective tissue attachment
- Presence of unattached plaque with gram-negative bacteria
2. Period of exacerbation:
- Bone and connective tissue attachment loss Pocket deepens
- It lasts for days, weeks, or months
- It is followed by a period of quiescence
- These periods of quiescence and exacerbation are known as periods of inactivity and periods of activity
Question 2. Methods of pocket therapy.
Answer:
1. Gingival pocket/false pocket:
- Scaling and root planning
- Recall
- If required gingivectomy/gingivoplasty
2. Periodontal pockets:
- Scaling and root planning
- Gingivectomy
- Hemisection
3. Suprabony pockets:
- Scaling and root planning
- Flap surgery
4. Infrabony pockets:
- New attachment procedures
- Nongraft associated
- Graft associated
- Combination
Question 3. Treatment of pseudo/edematous/false pocket.
Answer:
- Scaling and root planning
- Recall
- If required gingivectomy/gingivoplasty
Question 4. Complex pocket.
Answer:
- It is also known as a spiral pocket
- It originates on one tooth surface and twisting around the tooth involves one or more additional surfaces
- Here the base of the pocket is not in direct communication with the gingival margin
- It is most common in furcation areas
Question 5. Long junctional epithelium.
Answer:
- During the healing of the periodontal pocket, the area is in- invaded by cells from 4 different sources.
- Oral epithelium.
- Gingival connective tissue
- Bone
- Periodontal ligament
- If epithelium proliferates along the tooth surface before the cells from other tissues reach the area, it results in the long junctional epithelium
Question 6. Suprabony pockets.
Answer:
- Also known as suprarenal or supra-alveolar pocket
- In it, the bottom of the pocket is coronal to the underlying alveolar bone
- A horizontal pattern of bone loss is seen
- Interproximal, trans-septal fibers that are restored during progressive periodontal disease are arranged horizontally in the space between the base of the pocket and the alveolar bone
- On facial and lingual surfaces, periodontal ligament fi- bres beneath the pocket follow their normal horizontal-oblique course between tooth and bone
Question 7. Infrabony pockets.
Answer:
- Also known as subcrustal or intra-alveolar pocket In it the bottom of the pocket is apical to the underlying alveolar bone
- An angular pattern of bone loss is seen
- Interproximal, trans-septal fibers are oblique and extend- ing from the cementum beneath the base of the pocket along also- the bone and over the crest to the cementum of the adjacent tooth
- On facial and lingual surfaces, periodontal ligament fi- bres beneath the pocket follow an angular pattern of adjacent bone
- They extend from the cementum beneath the base of the pocket along the alveolar bone and over the crest to join with the outer periodontium
Periodontal Pocket Viva Voce
- In a pseudo or gingival pocket, there is no attachment loss
- The pocket depth is due to the coronal movement of the gingival margin
- In a true pocket, there is apical movement of the junctional epithelium due to the destruction of the supporting tissues
- In supra bony pocket, the base of the pocket is coronal to the alveolar bone
- Periodontal abscess is usually formed in the supporting periodontal tissues along the lateral aspect of the root or in the soft tissue wall
- The most severe destruction occurs in the lateral surface of the pocket
- The normal distance between junctional epithelium and alveolar bone is about 1.07-1.97 mm
- The normal distance between the apical extent of calculus and the alveolar crest is 1.97 mm
- The pattern of bone destruction in infra-bony pockets is angular
- The pocket formed by gingival enlargement is referred to as a pseudo pocket
- Periodontal abscess is also known as parietal abscess
- Periodontal cyst is commonly seen in mandibular canine and premolar
- The only reliable method of detecting periodontal pockets is probing
