Hard And Soft Tissue Oral Lesions In Children Important Notes
1. Epulis
- It is a pink, pedunculated, submucosal mass usually arising from the anterior maxillary alveolar ridge Problems:
- Feeding difficulty
- Breathing problems are rare
- Treatment
- Local excision
Read And Learn More: Pedodontics Short Essays Question And Answers
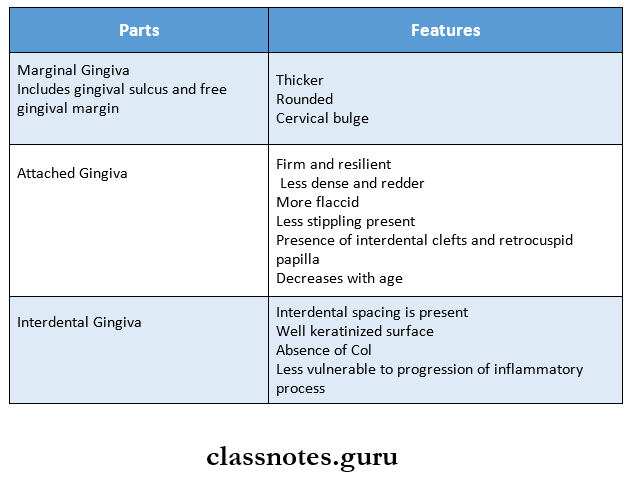
2. Normal gingiva in child
Hard And Soft Tissue Oral Lesions In Children Short Essays
Question 1. ANUG.
Answer:
- It is an inflammatory destructive disease of the gingiva
Anug Etiology:
- Bacteria- fusospirochaetal organisms and bacteroids intermedius
- Predisposing factors
- Local predisposing factors:
- Pre-existing gingivitis
- Injury to gingiva
- Smoking
- Systemic predisposing factors:
- Nutritional deficiency
- Debilitating diseases
- Psychosomatic factors
- Local predisposing factors:
Anug Clinical Features:
1. Intraoral signs:
- Punch out crater-like depression
- Covering of pseudomembranous slough
- Gingival hemorrhage
- Fetid odor
- Increased salivation- pasty saliva
- Sensitive to touch
- Radiating gnawing pain
- Increased pain on having spicy foods
- Metallic foul taste
2. Extraoral signs:
- Lymphadenopathy
- Fever
- Loss of appatite
- Lassitude
- Leucocytosis
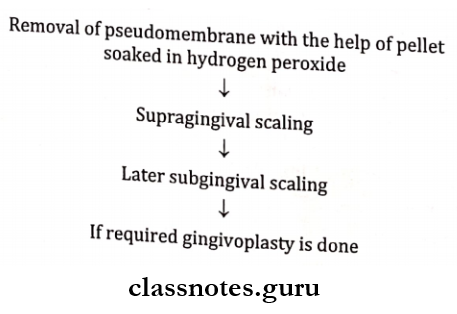
Anug Treatment:
1. Antibiotic coverage:
- Penicillin 500 mgTDS
- Metronidazole-200-400 mg BID
Question 2. Localized Aggressive Periodontitis/Juvenile.
Answer:
An uncommon form of severe periodontitis
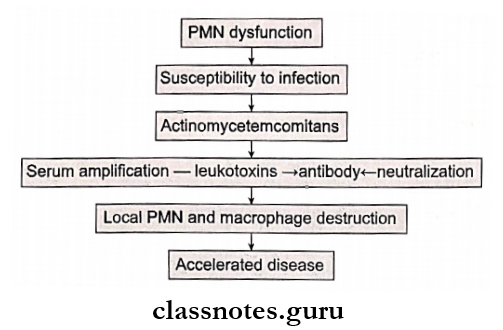
Juvenile Etiology:
- Actinobacillus actinomycetemcomitans
- Capnocytophage
- Defective neutrophil functioning
Juvenile Pathogenesis:
Juvenile Features:
- The teeth involved are permanent incisors and the first molar
- Attachment loss
- Alveolar bone loss
- Lack of inflammation
- Presence of deep pockets
- Excessive mobility
- Regional lymphadenopathy
- The presence of plaque is inconsistent with the disease process
Juvenile Radiographic Features:
- Vertical bone loss
- Arc-shaped bone loss
- Mirror image is formed as a result of bilateral involvement of arch
Juvenile Treatment:
- Scaling and root planning
- Subgingival irrigation
- Administration of tetracyclines
Question 3. Scorbotic Gingivitis.
Answer:
Scorbotic Gingivitis Etiology:
- Vitamin C deficiency
Scorbotic Gingivitis Features:
- Gingiva
- Color – bluish red
- Consistency – soft and friable
- Surface – smooth and shiny
- Size – Increased
- Bleeding on probing present
- Interdental papillae – Ulceration and necrosis
- Foul breath
- Bone loss
- Loosening of teeth
Scorbotic Gingivitis Treatment:
- Ingestion of vitamin C tablets in the form of nutrition
- Oral prophylaxis
Question 4. Classification of Gingival and Periodontal disease in Children.
Answer:
1. Gingival diseases:
- Dental plaque-induced gingival diseases
- Associated with dental plaque only
- Modified by systemic factors
2. Periodontal diseases:
- Incipient chronic periodontitis
- Aggressive periodontitis
- Periodontitis as a manifestation of systemic diseases
- Necrotizing periodontal diseases
Short Question And Answers
Question 1. Acquired Pellicle.
Answer:
- It is thin film derived mainly from salivary glycoprotein which forms over the surface of a cleansed tooth crown.
- It is free from micro-organism
- It cannot be easily removed
- It reforms very quickly on clean tooth surfaces
Question 2. Causes of gingival hyperplasia.
Answer:
1. Inflammation:
- Acute
- Chronic
2. Drug-induced:
- Phenytoin
- Cyclosporins
3. Systemic diseases:
- Conditioned enlargeents
- Puberty
- Regnancy
- Non-specific
- Systemic diseases
- Leukemia
4. Neoplastic:
- Benign tumors
- Malignant tumors
5. False enlargements
6. Idiopathic
Question 3. Phenytoin induced gingival hyperplasia.
Answer:
Phenytoin Clinical Features:
- It occurs 3 months after initiation of phenytoin therapy
- Common in younger individuals
- Generalized distribution but severe in maxilla
- The site involved- marginal gingiva and interdental papilla
- Appears as a painless, bead-like enlargement
- Interferes with occlusion
- Has tabulated surface
- Firm to resilient in consistency
- No tendency to bleed
- Question 4. Acute herpetic gingivostomatitis.
Answer: - It is an acute infection of the oral cavity
- Acute herpetic gingivostomatitis Etiology:
- It is caused by herpes simplex type-1 virus
- Acute herpetic gingivostomatitis Clinical Features:
- Age- occurs during childhood
- Headache
- Fever
- Nausea, anorexia
- Lack of tactile and sensory sensation
- Sore throat
- Drooling of saliva
- Bilateral cervical lymphadenopathy
- Irritability
- Myalgia
- Site involved
- Gingiva
- Hard palate
- Dorsum of tongue
- Lips
- Vermillion border
- Perioral skin
- Nasopharynx
- Present as shiny erythematous gingival swelling
- Reddening of the oral mucosa
- Formation of numerous small, dome-shaped or pinhead-type vesicle
- Size-2-3 mm in diameter
- Vesicles contain clear fluid and rupture to form ulcers
- Ulcers are multiple, small, circular, punctuate, shallow and painful
- Have red margins and yellowish or greyish floor
- Small ulcers fuse to form diffuse, large, whitish ulcers
- They are surrounded by a red halo
- Gingival margins are red, swollen, and painful and have punched-out erosions
- Difficulty in taking food
- Difficulty in mastication
- Difficulty in swallowing
- Increased bleeding
- Soreness of the oral cavity
- Sensitive to touch
- Numerous vesicle formations over the tonsillar area and posterior pharynx
Question 5. Juvenile periodontitis.
Answer:
- Rapid loss of attachment and bone loss occurring in an otherwise clinically healthy patient with the number of microbial deposits inconsistent with the disease severity and familial aggregation of diseased individual
Juvenile periodontitis Etiology:
- Hereditary
- A. actinomycete contains
- Capnocytophaga
Juvenile periodontitis Types:
- Localized aggressive periodontitis
Juvenile periodontitis Clinical features:
- Age- 20 years
- Sex – common in females
- Lack of inflammation
- Deep pockets
- A small amount of plaque
- Mobility of first molars and incisors
- Midline diastema
- Root sensitivity
- Deep dull radiating pain
- Periodontal abscess
- Lymphadenitis
2. Generalised aggressive periodontitis
- Characterised by generalised interproximal attach¬ment loss affecting at least three permanent teeth other than first molar and incisors
Generalized aggressive periodontitis Clinical features:
- Age – puberty to 30 years of age
- Site – all teeth are affected
- Severely inflamed tissue
- Spontaneous bleeding
- Suppuration
- Deep pockets
- Attachment and bone loss
- Weight loss
- Mental depression
- General malaise
Hard And Soft Tissue Oral Lesions In Children Viva Voce
- Unique characteristics of attached gingiva are: inter-dental clefts and tricuspid papilla
- The probing depth of clinically normal gingiva is 2-3 mm
- Chronic marginal gingivitis is more prevalent
- Eruption cyst is most frequently seen in the primary second molar
- Eruption sequestrum is seen in children at the time of eruption of first permanent molar
- Penicillin is drug of choice in ANUG
- Sulcus depth around primary teeth ranges from 1.4 mm to 2.1 mm
- The periodontal ligament is wider in deciduous teeth as compared to permanent
