Healing Of Tissues Important Notes
1. Sequence of events of wound healing
- Formation of a blood clot
- Acute inflammatory response
- Organization
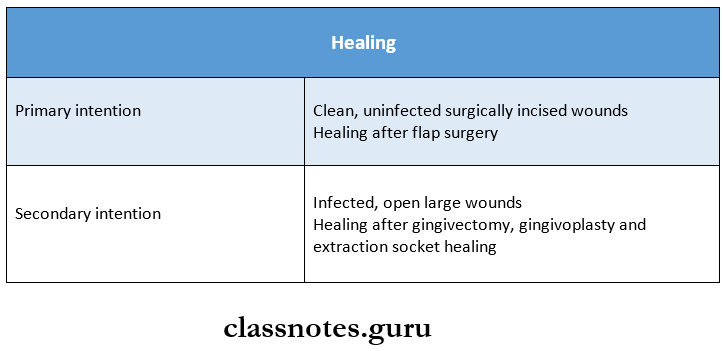
2. Primary and secondary intention of healing and their examples
3. Factors inhibiting wound contraction
- Infection
- Foreign bodies
- Poor blood supply
- Ionizing radiation
- Vitamin C deficiency
- Glucocorticoids
- Uncontrolled diabetes
4. Complications of fracture healing
- Fibrous union
- Nonunion
- Delayed union
5. Factors influencing healing
- Local factors
- Infection – reduces healing
- Poor blood supply – reduces healing
- Foreign bodies – reduce healing
- Movement-reduces healing
- Ionizing radiation – reduces healing
- UV light – facilitates healing
- Systemic factors
- Age-healing is rapid in young
- Nutrition- vitamin deficiency delays healing
- Uncontrolled diabetes reduces healing
- Hematologic abnormalities reduce healing
- Glucocorticoids reduce healing
Read And Learn More: Pathology Question And Answers
Healing Of Tissues Long Essays
Question 1. Describe the healing of a fracture. Enumerate the causes for nonhealing of fracture
Answer:
- Healing: Is the body’s response to injury in an attempt to restore normal structure and function. Healing involves 2 distinct processes:
1. Regeneration:
- When healing takes place by the proliferation of parenchymal cells and usually results in the complete restoration of the original tissues.
2. Repair:
- When healing takes place by the proliferation of connective tissue elements resulting in fibrosis and scarring at times, both processes take place simultaneously.
Healing of fracture: Healing of fracture by callus forma¬tion depends upon whether the fracture is
- Traumatic/pathological
- Complete/incomplete like green stick fracture and
- Simple, comminuted/compound.
- Healing of fractures takes place by.
1. Primary union:
- Occurs in special situations when the ends of fracture are approximated by the application of compression clamps.
- Here, the bony union takes place with the formation of medullary callus without periosteal callus forma¬tion.
2. Secondary union:
More common type. Takes place in the following manner.
- Procallus formation:
- Hematoma – Bleeding from torn blood vessels surrounding the fracture.
- Local inflammatory response – Occurs at the site of injury with exudation of fibrin, polymorphs, and macrophages.
- In the growth of granulation tissue – With neovascular- polarisation and proliferation of mesenchymal cells from periosteum and endosteum.
- Calluses formed – composed of woven bone and cartilage.
- This stage is called provisional callus/precalculus formation.
- Osseous callus formation:
- Procallus acts as a scaffolding on which an osseous callus composed of lamellar bone is formed.
- Woven bone is cleared away by osteoclasts, in their place, newly formed blood vessels and os¬teoblasts invade, laying down osteoid which is calcified and lamellar bone is formed by developing a haversian system concentrically around the blood vessels.
- Remodeling:
- Osteoblastic laying and osteoclastic removal take place during the formation of lamellar bone remodeling the united bone ends.
- External callus is cleared away compact bone (cortex) is formed in place of intermediate callus, and the bone marrow cavity develops in in¬ternal callus
Causes of nonhealing of fracture :
- Local factors:
- Infection – the presence of infection delays wound healing.
- Poor blood supply – delays wound healing
- Foreign bodies like sutures – delay healing
- Movement of the injured area – delays healing
- Exposure to ionizing radiation delays granulation tissue formation.
- Exposure to UV light – facilitates healing
- The type, size, and location of injury determine whether healing takes place by resolution/organization.
- Systemic factors:
- Age-wound healing is rapid in young and slow in aged and debilitated people.
- Nutrition – nutritional deficiency delays healing
- Systemic infection – delays wound healing.
- Uncontrolled diabetes – delay in healing.
- Haematologic abnormalities – delay wound healing.
Question 2. Describe the healing of a wound by the primary union. Mention the differences between primary and secondary unions.
Answer:
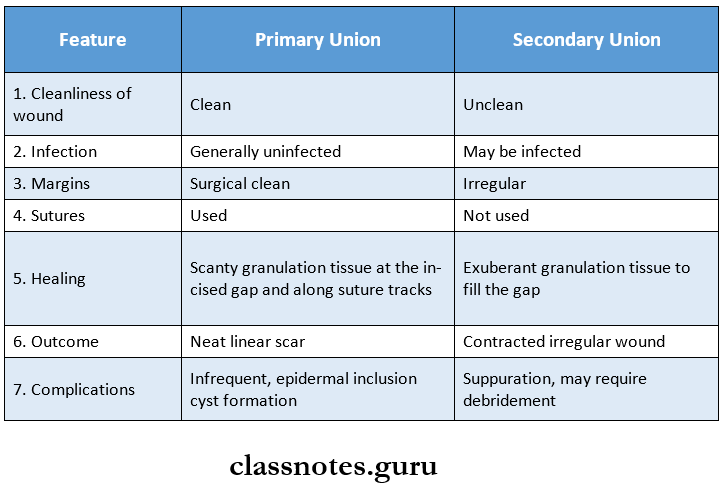
Primary union: Primary union is defined as the healing of a wound which is
- Clean and uninfected
- Surgically incised
- Without much loss of cells and tissue
- Edges are approximated by surgical sutures.
The sequence of events in primary union:
1. Initial hemorrhage:
- Immediately after injury, the space between the surfaces of the wound is Filled with blood which later clots and seals the wound against dehydration and infections.
2. Acute inflammatory response:
- Within 24 hours, polymorphs appear from the margin. By 3rd day, they are replaced by macrophages.
3. Epithelial changes:
- Within 48 hours basal cell layer of the epidermis starts proliferating and forms a layer which separates the viable dermis from the overlying clot and necrotic material. This forms a scab which is cast off. By the 5th day, a new multi-layered epidermis is formed.
4. Organisation:
- Fibroblasts invade the wound area and by the 5th day new collagen fibrils start forming.
- In 4 weeks, scar tissue is with scantly cellular and vascular elements, a few inflammatory cells, and epi trellised surface is formed.
5. Suture tracks:
- Each suture track is a separate wound and incites the same phenomena as in the healing of the primary wound.
- When sutures are removed around 7th day, much of the epithelioid suture track is avulsed and the remaining epithelium tissue in the track is absorbed
- Sometimes, the suture track gets infected (stitch abscess) or the epithelial cells may persist in the track (implantation or epidermal cysts).
Differences between primary and secondary union.
Healing Of Tissues Short Essays
Question 1. Granulation tissues
Answer:
- Granulation tissue is a newly proliferated tissue that is formed during the healing of a wound by secondary inten¬tion.
- It takes place in 3 steps:
1. Inflammation:
- After the injury, blood clot forms at the site. There is an acute inflammatory response with exu¬dation of plasma, neutrophils, and some monocytes within 24 hours.
2. Phase of clearance:
- Necrotic tissue, debris, and RBCs are removed from the site by proteolytic enzymes liberated from neutrophils, autolytic enzymes from dead cells, and phagocytic activity of macro¬phages.
3. Phase of ingrowth of granulation tissue: Consists of 2 processes.
- Neovascularisation.
- Fibrogenesis
1. Neovascularisation: Formation of new blood vessels at the site of injury takes place by prolifera¬tion of endothelial cells which develops lumen and start carrying blood. These blood vessels differentiate into muscular arterioles, thin-walled venules, and true capillaries.
2. Fibro genesis: New fibroblasts originate from fibrocytes and by meiotic division of fibroblasts.
- Fibrils begin to appear by about 6th day.
- As maturation proceeds, more and more of collagen is formed, and the number of active fibroblasts and new blood vessels decreases.
- This results in the formation of an inactive-looking scar known as cicatrization.
Question 2. Complications of wound healing
Answer:
Complications of wound healing:
1. Infection:
- Due to the entry of bacteria, wound healing may be delayed.
2. Implantation (epidermal) cyst:
- Due to the persistence of epithelial cells in the wound after healing, cyst formation may occur.
3. Pigmentation:
- Healed wounds sometimes may have rust-like color due to staining with haemosiderin. Some colored pigments may be left behind during healing that imparts color.
4. Deficient scar formation:
- Due to inadequate formation of granulation tissue.
5. Incisional hernia:
- A weak scar, especially after a laparotomy, may be the site of the bursting open of a wound or an incisional hernia.
6. Hypertrophied scars and keloid formation:
- Excessive formation of collagen in healing results in keloid (claw-like) formation. Hypertrophied scars are confined to the borders of the initial wound.
7. Excessive contraction:
- An exaggeration of wound contraction may result in information of contrac¬tures /cicatrization.
8. Neoplasia:
- Rarely, a scar may be the site for the development of carcinoma later.
- Example: Squamous cell carcinoma in Marjolin’s ulcer.
Healing Of Tissues Short Question And Answers
Question 1. Healing of oral structures
Answer:
- Healing is defined as the body’s response to injury in an attempt to restore normal structure and function.
- Healing can take place by.
- Primary union
- Secondary union
1. Primary union:
- Primary healing takes place in clean and uninfected and surgically incised wounds whose edges are approximated by sutures and also where much loss of cells and tissues is not present.
- The sequence of events in primary union are
- Initial hemorrhage
- Acute inflammatory response.
- Epithelial changes
- Organization
- Suture tracks.
2. Secondary union:
- Second healing takes place in wounds with a large tissue defect and where there is extensive loss of cells and tissues
- The sequence of events in secondary union are
- Initial hemorrhage
- Inflammatory phase
- Epithelial changes
- Granulation tissue
- Wound contraction
- Presence of infection.
Question 2. Healing by secondary intention
Answer:
- This is defined as the healing of a wound which is
- Open with large tissue defect.
- Having extensive loss of cells and tissues.
- The wound is not approximated by surgical sutures but is left open.
The sequence of events is as follows:
1. Initial hemorrhage:
- Wound space is filled with blood and fibrin clot which dries.
2. Inflammatory phase:
- An initial acute inflammatory response is seen followed by the appearance of macro-phages which clear off debris.
3. Epithelial changes:
- Epithelial cells proliferate from the wound margins in the form of epithelial spurs till re-epithelialization occurs and the gap is closed completely.
- But, proliferation cells do not cover the gap till granu¬lation tissue from the base starts filling the wound space.
4. Granulation tissue:
- This forms the main bulk of sec¬ondary healing. It is formed by the proliferation of fibro¬blasts and new blood vessels.
5. Wound contraction:
- This is not seen in primary healing due to the action of myofibroblasts, the wound contracts to one-third to one-fourth of its original size.
6. Presence of infection:
- Delays the process of healing due to the release of bacterial toxins that provoke necro¬sis, suppuration, and thrombosis.
