Haemodynamic Derangements Of Body Fluids Important Notes
1. Oedema
- It is an abnormal and excessive accumulation of fluid in the interstitial tissue spaces and serous cavities
- Causes
- Decreased plasma oncotic pressure
- Increased capillary hydrostatic pressure
- Increased capillary permeability
- Lymphatic obstruction
- Sodium and water retention
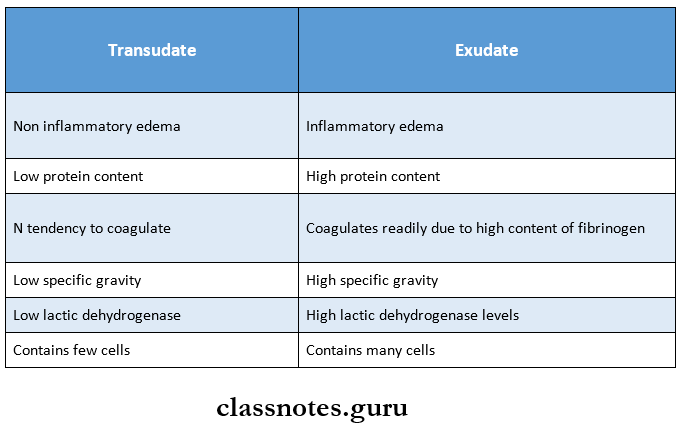
2. Transudate and exudate
Derangements Of Body Fluids Long Essays
Question 1. Define oedema. Discuss pathogenesis and causes of oedema,
(or)
Discuss etiopathogenesis of oedema.
Answer:
Oedema: Oedema may be defined as abnormal and exces¬sive fluid accumulation in interstitial tissue spaces and serous cavities.
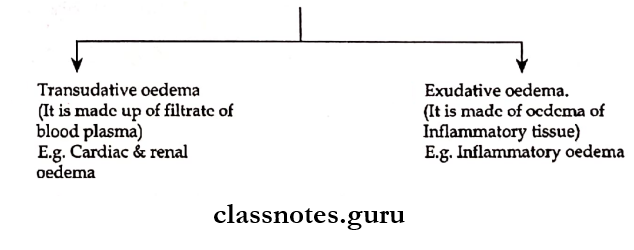
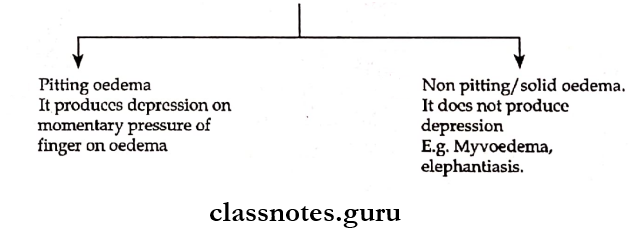
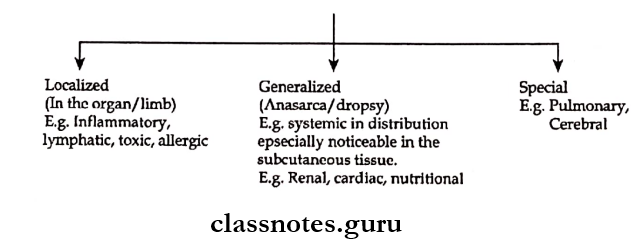
Types of Oedema:
1. Three main types of oedema:
2. Subcutaneous oedema is of 2 types.
Read And Learn More: Pathology Questions and Answers
3. Depending on oedema fluid.
Etiopathogenesis:
Oedema is the result of an increase in the forces that tend to more fluids from the intravascular compartment to the interstitial space
The following six mechanisms may be operating singly/in combination to produce oedema.
1. Decreased plasma oncotic pressure:
- Plasma oncotic pressure exerted by the total amount of plasma proteins tends to draw fluid into the vessels normally.
- A fall in the total plasma protein level/hypoproteinemia less than 5g/dl lowers plasma oncotic pressure and thus it cannot effectively counteract the hydrostatic pressure of blood.
- This results in Tsed outward movement of fluid from the capillary wall and anodised inward movement of fluid from the interstitial space causing oedema.
- Example: Oedema of renal disease: Nephrotic syndrome, acute glomerulonephritis.
- Ascites of liver disease: cirrhosis.
2. Increased capillary hydrostatic pressure:
- Capillary hydrostatic pressure is the force that normally tends to drive fluid through the capillary wall into interstitial space by counteracting the force of plasma oncotic pressure.
- A rise in the hydrostatic pressure at the venular end to a level more than the plasma oncotic pressure results in minimal/no reabsorption of fluid at the venular end consequently leading to oedema.
- Example: Oedema of cardiac diseases→ Congestive cardiac failure, constrictive pericarditis.
- Passive congestion → Mechanical obstruction due to thrombosis of veins of lower limbs, varicosities, pressure by interns, and tumours.
3. Lymphatic obstruction:
Normally the interstitial fluid in the tissue space escapes through lymphatic and thus obstruction to the outflow of the lymphatics causes localized oedema known as lymphoedema.
4. Tissue factors:
They can cause oedema when the oncotic pressure of the interstitial fluid is elevated due to increased vascular permeability and inadequate removal of proteins by lymphatics.
5. Increased capillary permeability:
- Intact capillary endothelium acts as a semipermeable membrane permitting free flow of water and crystalloids and allowing only a minimal passage of tissue proteins.
- Sometimes, capillary endothelium may be injured, in such cases there is development of gaps increasing the capillary permeability to plasma proteins.
- Thus, the oncotic pressure of plasma is reduced and that of interstitial fluid is elevated producing oedema.
- Example: Generalized oedema in systemic infections, poisonings localized oedema. Inflammatory oedema – infections, allergic reactions. Angioneurotic oedema.
6. Sodium and water retention:
- Excessive retention and decreased renal excretion of sodium and water occur in response to hypovoleamia.
- Example: Oedema of cardiac disease – congestive cardiac failure.
- Ascites of liver disease – cirrhosis.
Question 2. What are the types of exudation? Describe the sequelae of pyogenic abscesses.
Answer:
Exudate:
Exudate is inflammatory oedema which is protein-rich with a specific gravity usually greater than 1.020
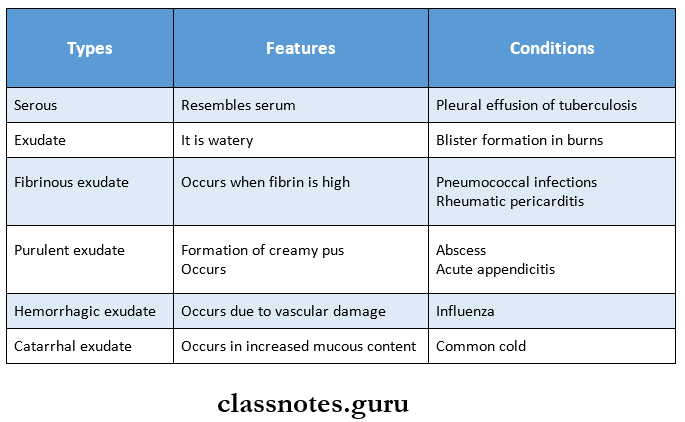
Exudation Types:
Sequence of Pyogenic Abscess:
- Drainage
- Abscess may be discharged to the surface due to increased pressure inside
- Healing by fibrous scarring
- Calcification
- If the abscess is not drained, it gets organized by dense fibrous tissue
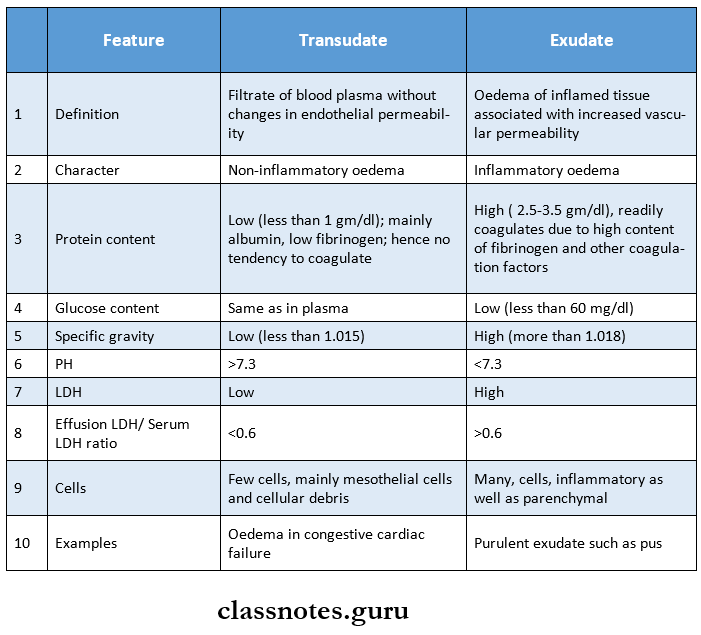
Question 3. Classify inflammatory exudate. Give example. What are the differences between exudate and transudate?
Answer:
Derangements Of Body Fluids Short Essays
Question 1. Angioedema
Answer:
- Angioedema is an autosomal dominant disorder which manifests as a form of local anaphylaxis
- It Is characterised by laryngeal oedema, oedema of eyelids, lips, tongue and trunk
- The response is mediated by humoral antibodies of IgE type
- It involves the release of
- Histamine
- Serotonin
- Leukotrienes
- Prostaglandin
- Platelet-activating factors
- These act as anaphylactic mediators
- They are responsible for changes associated with angioedema
Derangements Of Body Fluid Short Question And Answers
Question 1. Renal oedema
Answer:
Generalised oedema occurs in certain diseases of renal origin such as
1. Nephrotic syndrome:
In nephrotic syndrome, there is persistent and heavy proteinuria, there is hypo-al-buminemia causing decreased plasma oncotic pressure resulting in severe generalised oedema.
2. Glomerulonephritis:
Nephritic oedema is usually mild as compared to nephrotic oedema. Nephritic oedema is due to excessive reabsorption of sodium and water in the renal tubules via the resin angiotensin-aldosterone mechanism.
3. Acute tubular necrosis:
Acute tubular injury following shock/toxic chemicals results in gross oedema of the body.
Question 2. Pulmonary oedema
Answer:
- Pulmonary oedema develops from left heart failure.
- There is fluid accumulation not only in tissue spaces but also in the pulmonary arteriole.
- It causes serious functional impairment
Etiopathogenesis: Can result from either elevation of pulmonary hydrostatic pressure/increased capillary permeability.
- Elevation of pulmonary hydrostatic pressure.
- An increase in hydrostatic pressure of pulmonary capillaries and the resulting imbalance between palm hydrostatic press and plasma oncotic pressure causes excess fluid to move into the interstitium.
- Interstitial oedema develops later with a prolonged elevation of hydrostatic pressure, alveolar lining cells develop and alveolar oedema results.
- This mechanism is seen in left heart failure, mitral stenosis and thyrotoxicosis.
- Increased capillary permeability: Damage to alveolar-capillary membrane causes increased permeability so that excess fluid and plasma proteins leak out, initially into the interstitium and later into the alveoli.
- Example: Fulminant pulmonary infections, radiation injury, inhalation of ototoxic substances.
