Question 1. Bence Jones proteins
Answer:
Bence Jones Proteins
- Bence-jones proteins are light chain proteins produced by tumour cells
- Due to it serum protein level raises
- Its presence in urine detects multiple myeloma
- Serum and urinal protein Immunoelectrophoresis is done to detect it
- Bence-Jones protein coagulates when the urine is heated to 42 degrees C to 60 degrees C
- It disappears when the urine is boiled and finally reap¬pears again as urine is cooled
- It is also present in patients with polycythemia or leu¬kemia
Question 2. Vitality Tests
Answer:
Vitality Tests
- Vitality tests are the most useful diagnostic tool used to diagnose an endodontic case
Vitality Tests Types:
1. Heat Test:
- It is usually done using
- Hot gutta percha stick
- Hot burnisher
- Hotcompond
- Hot water
- Hotair
- Hot gutta percha stick
- Gutta-percha is heated over the flame until it becomes shiny and then it is placed on the middle third of the facial surface of the crown
- At first, a normal contralateral tooth should be tested and then the affected tooth is tested
Read And Learn More: Oral Medicine Question and Answers
2. Cold Test:
- Cold Test is done using ethyl chloride spray, pencil sticks of ice, and carbon dioxide snow at -78 degrees C
3. Electric Pulp Test:
- Isolate the area of the tooth to be tested with cotton rolls and air dry all the teeth
- Apply an electrolyte on the tooth electrode and place it against the dried enamel of the crown
- Retract the patient’s cheek away from the tooth
- Turn the rheostat slowly and increase the current gradually
- Record the response of the patient
Question 3. Significance of PST medical history
Answer:
Significance Of PST Medical History
A Complete medical history must be obtained to
- Determine systemic factors or diseases that will require special considerations before, during or after the treatment
- A complete list of meditations most he obtained In order to Identify the drugs or medications that could adversely interact with drugs used in dental treatment
Question 4. Pathergy test
Answer:
Pathergy Test Types:
1. Oral Pathergy Test:
- Site: lower lip.
- The Procedure Of Oral Pathergy Test:
- Prick the mucous membrane of the lower lip to the submucosa using a 20 gauge blunt dispos¬able needle
- Readings are taken after 48 h, and the test is considered positive if a pustule or ulcer is seen
2. Skin Pathergy Test:
- Site: A hairless area on the flexor aspect of the forearms is usually chosen as the test site.
- The Procedure Of Skin Pathergy Test:
- It can be performed using 1-16 needle pricks.
- Generally, the needle is inserted vertically or diagonally at an angle of 45° to a depth of 3-5 mm.
- The needle should reach the dermis for a proper response.
- Readings are taken after 48 hrs of the needle prick.
- An l-2mm papule that is usually felt by palpation and which is surrounded by an erythematous halo is formed on the skin.
- The papule may remain as a papule or transform into a l-5mm pustule.
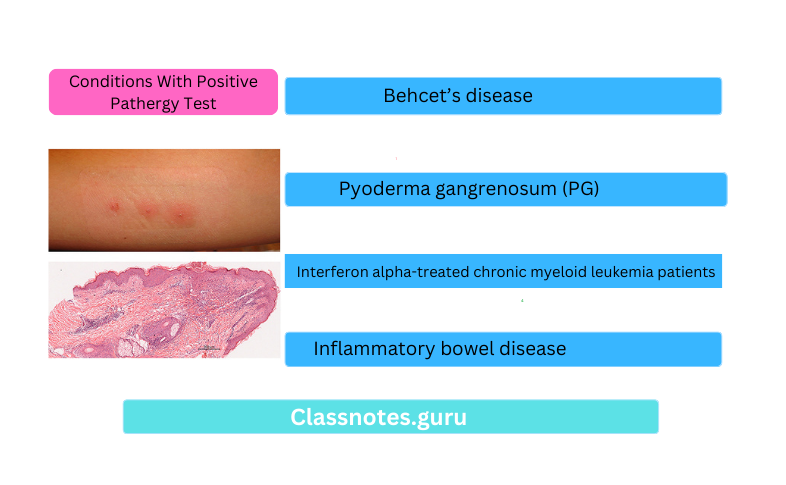
Conditions With Positive Pathergy Test:
- Behcet’s disease
- Pyoderma gangrenosum (PG)
- Interferon alpha-treated chronic myeloid leukemia patients
- Inflammatory bowel disease
Question 5. Oral brush biopsy
Answer:
Oral Brush Biopsy:
- The oral brush biopsy was introduced to the dental profession in 1999.
- This biopsy method utilizes an improved brush to obtain a complete transepithelial biopsy specimen with cellular representation from each of the three layers of the lesion: the basal, intermediate, and superficial layers.
- When used properly and rubbed against an area of suspect tissue aggressively (to the point of minor bleeding) the biopsy brush penetrates to the basement membrane, removing tissue from all three epithelial layers of the oral mucosa
- The oral brush biopsy does not require topical or local anesthetic and causes minimal bleeding and pain.
- The brush biopsy instrument has two cutting surfaces, the flat end of the brush and the circular border of the brush.
- Either surface may be used to obtain the specimen.
- Brush biopsies are utilized routinely in the detection of precancer and cancer in other organ systems.
Question 6. Schimmer’s test.
Answer:
Schimmer’s Test
- Schimmer’s Test is a diagnostic test for Sjogren’s syndrome
- A strip of filter paper is placed in between the eye and eyelid to determine the degree of tears measured in mm
- If it is < 5 mm in 5 min, it is positive
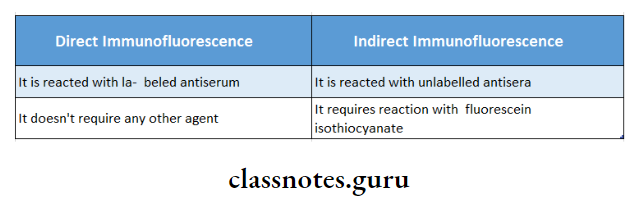
Question 7. Two differences between direct & indirect im- munofluorences
Answer:
Differences Between Direct And Indirect Imunofluorences
Question 8. Toluidine blue staining.
Answer:
Toluidine Blue Staining
- Toluidine Blue Staining is used as an aid in the diagnosis of oral cancer and potentially malignant lesions
Toluidine Blue Staining Mechanism:
- Toluidine Blue Staining is an acidophilic, nuclear dye
- Toluidine Blue Staining selectively stains the nucleic acid, especially DNA and RNA
- Toluidine Blue Staining penetrates into the intracellular canals present in the malignant epithelium
Toluidine Blue Staining Effects:
- It stains the epithelium surfaces to blue
- However, this stain is lost after the application of 1% acetic acid
- This occurs only to the normal epithelium or the be¬nign lesions
- But in malignant lesions, the stains remain as it is
KIT:
- KIT It Contains:
- 1% toluidine blue 10 ml solution « 1% acetic acid
- Absolute alcohol
- Distilled water
- pH is adjusted to 4.5
- KIT Method Of Use:
- Make the patient rinse the mouth with water twice for 20 seconds each
- Next, rinse with 1% acetic acid for 20 seconds
- Dry the area with the help of a gauze piece
- Apply 1% toluidine blue solution with a cotton swab
- Rinse again with acetic acid and water
- Observe the staining if present
- KIT Advantages:
- Good sensitivity
- Very low false negative results
- It is effective in demonstrating dysplasia and early malignant lesions which is not clinically recognizable
Question 9. Tzanck test.
Answer:
Tzanck Smear:
Rub the lesion surrounding the area
↓
Puncture the lesion
↓
Absorb the secretion over cotton
↓
Collect this overslide and stain it
↓
Observe under microscope
Tzanck Smear Result: lesion shows acantholysis
Question 10. Auspitz sign.
Answer:
Auspitz Sign
- Auspitz Sign is seen in psoriasis
- If the deep scales on the surface of the lesion are removed, one or two tiny bleeding points are often dis-closed
- This phenomenon is known as the “Auspitz sign”
Question 11. Patch test.
Answer:
Patch Test
- Patch Test is used to evaluate drug allergy
- The suspected allergen is placed on normal non-hairy skin i.e. on the upper portion of the back
- Patch Test remains in contact with the skin for 48 hours
- Then the patch is removed
- Next, the area is examined after 2-4 hours for persistent erythema
Question 12. Examination of ulcer.
Answer:
1. Examination Of Ulcer Inspection:
- Size And Shape:
- Oval: In tuberculosis
- Circular/ Semilunar: In syphilis
- Irregular: In carcinoma
- Number: Number of the ulcer is examined
2. Examination Of Ulcer Position:
- Different ulcers are located at a different position
- This gives a clue about the diagnosis
- Rodent ulcer: confined to the upper part of the face
- Malignant ulcers: present over lips, tongue, breast, and penis
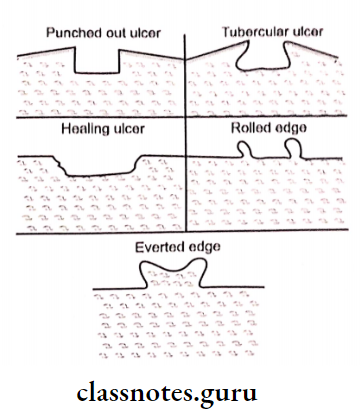
3. Examination Of Ulcer Edges:
- Spreading ulcers have inflamed and edematous edges
- Tuberculosis ulcers have undermined edges
- Gummatous ulcers have punched-out edges
- Healing ulcers have sloping edges
- Rodent ulcers have raised edges
4. Examination Of Ulcer Surrounding Areas:
- Examination Of Ulcer may be glossy, red, and edematous
5. Examination Of Ulcer Palpation:
- Tenderness over the ulcer is palpated
- The temperature of the ulcer is felt
6. Examination Of Ulcer Edges:
- Edges are palpated for induration
7. Examination Of Ulcer Base:
- The depth of the ulcer is measured in millimeters
- Bleeding of the ulcer is examined
- Relation to the deeper structures is examined
Question 13. Paul Bunnell test.
Answer:
Paul Bunnell Test
Paul Bunnell Test is a diagnostic test for infectious mononucleosis
Paul Bunnell Test Procedure:
- Collect sheep’s RBCs and human’s RBCs
- Agglunate both
Paul Bunnell Test Result:
- The normal titer is 1:8
- But in a diseased person, titer becomes 1:4096
- Agglutination is observed
Oral Medicine Investigations Viva Voce
- Paul Bunnel test is for infectious mononucleosis
- A patch test is for drug allergy
- Schimmer test is for Sjogren’s syndrome
- Schilling test is for vitamin B12 deficiency
