Periodontics Normal Periodontium Important Notes
1. Parts of the Gingiva
- Marginal Gingiva
- Border of the gingiva surrounding the teeth in the collar-like fashion
- Demarcated apically by a shallow depression called “free gingival groove”
- Attached Gingiva
- Part of the gingiva that is firm, resilient, and tightly bound to the underlying periosteum of the alveolar bone
- Interdental Gingiva
- Occupies gingival embrasure
2. Layers of Gingival Epithelium
- Basal layer – Cells are cylindrical/cuboidal Attach to the basement membrane
- Cells have the ability to divide
- Stratum Spinosum
- Large cells with short processes called spines
- Cells have a prickled appearance
- Cells are attached to one another with the help of desmosomes
- Stratum Granulosum – Keratohyalin granules are seen
- Stratum Corneum
- The cytoplasm of cells in this layer is filled with keratin
- It can be
- Orthokeratinized
- Parakeratinized
Read And Learn More: Periodontics Question and Answers
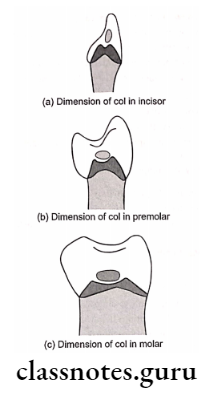
3. Interdental col is an area with more susceptibility to infection because
- It is non-keratinized
- Non accessible area
- Area with food lodgement
4. Blood Supply of Gingiva
- Supraperiosteal arteries
- Arises from above alveolar bone
- Branches and supplies facial and lingual surfaces
- Vessels of the periodontal ligament
- Anastomoses with the capillaries
- Arterioles emerging from the crest of the interdental septa
5. Gingival Fibers
- Dentogingival – From cervical cementum to lamina propria
- Alveologingival – From bone to lamina propria
- Circular – Around the neck of a tooth
- Dentoperiosteal – From cementum to alveolar process
- Transeptal – Runs interdentally
6. Blood supply to a periodontal ligament is through
- Apical vessels
- Transalveolar vessels
- Gingival vessels
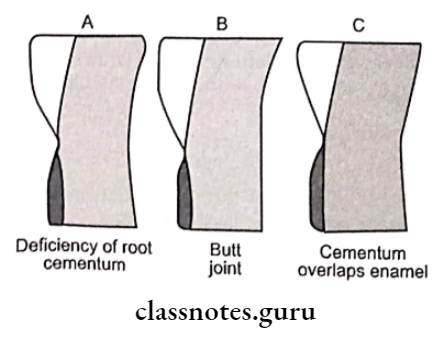
7. Types of the cementoenamel junction
- 60-65%-Cementum overlaps enamel
- 30% End-to-end relationship
- 5-10%-Cementum and enamel fail to meet
8. Principal fibers of periodontal ligament
- Trans-septal group
- Connects cementum of one tooth with that of other
- Alveolar crest
- Extends from cementum to alveolar crest
- Function – Retains tooth in the socket, Retains lateral tooth movement
- Horizontal group – Extends from cementum to alveolar bone
- Oblique group
- Extends coronally from the cementum to the bone
- Function – Resist axially directed forces
- Apical group
- From the cementum to the bone of the alveolar fundus
- Function – Prevents tipping movement, Resists luxation
- Inter-radicular fibers
- Presents between the cementum of a multi-rooted tooth.
- Function – Resists luxation, Resists tipping and torquing
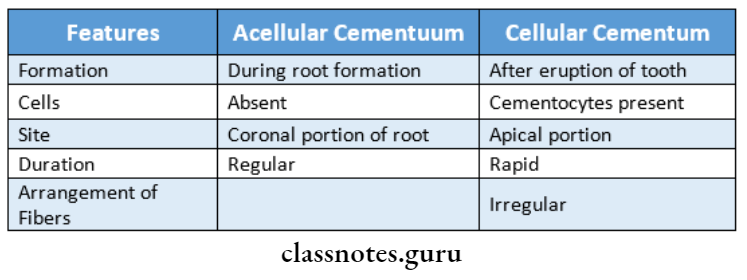
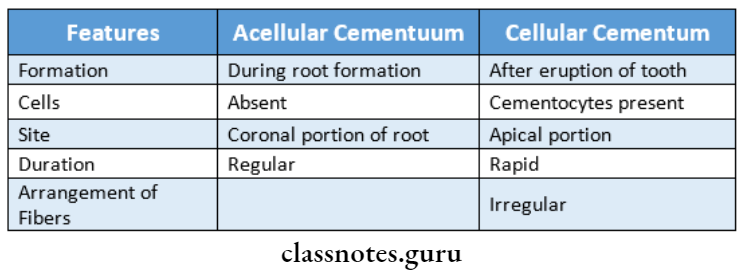
9. Difference between acellular and cellular cementum.

Periodontics Normal Periodontium Short Answers
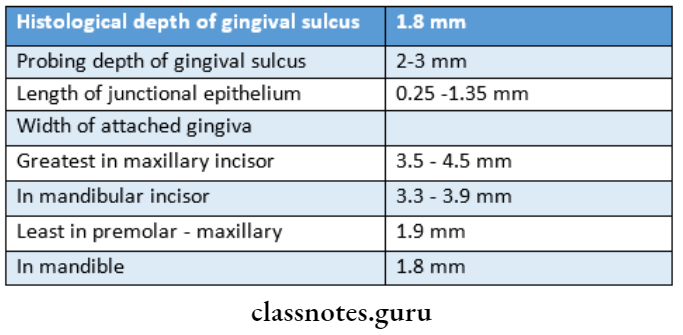
Question 1. Junctional Epithelium.
Answer:
- Junctional Epithelium is the tissue that joins the tooth on one side and the oral sulcular epithelium and connective tissue on the other
- Junctional Epithelium forms the base of the sulcus
Junctional Epithelium Attachment:
- Attach to the tooth surface
- By internal basal lamina
- Reinforced by the gingival fibers
- Consists of lamina dens and lamina lucida
- Attach to gingival connective tissue By external basal lamina
Junctional Epithelium Features:
- Consists of non-keratinizing epithelium
- Thickness
- Early life- 3-4 layers
- Later Increases
- Length- 0.25-1.35 mm
Question 2. Lamina dura.
Answer:
- Lamina dura is the wall of the tooth socket that surrounds the tooth
- Lamina dura is made up of dense cortical bone
- A thin radiopaque line surrounds the root of the tooth
- Lamina dura is continuous with the shadow of the cortical bone at the alveolar crest
- Lamina dura is slightly thicker than the trabeculae of the cancellous bone in the area
- The thickness and density of the lamina dura will vary. with the number of occlusal stresses
- Lamina dura wider and more dense around the roots of teeth. By alternate protruberances and depression heavy occlusion
- Lamina dura thinner and less dense around teeth not subjected to occlusion function
- The presence of intact lamina dura around the tooth indicates a vital pulp.
Question 3. Gingival Sulcus.
Answer:
The gingival sulcus is defined as the shallow crevice or space around the tooth bounded by the surface of the tooth on one side and the epithelium lining the free margin of the gingiva on the other side.
Gingival Sulcus Boundaries:
- Tooth side- bounded by tooth surface
- Tissue side- Bounded by marginal gingiva
- Lateral wall- Formed by sulcular epithelium
- Bottom of sulcus- Formed by junctional epithelium
Gingival Sulcus Depth:
- It is a V-shaped crevice
- The depth of the gingival sulcus is determined by estimating the depth of penetration of the periodontal probe
- In normal or ideal conditions, the depth of the gingival sulcus is 0 mm
- The probing depth of clinically normal gingival sulcus is 2 to 3 mm.
- The histological depth of the sulcus is 1.8 mm with variations of 0 to 6 mm.
Pathological variations:
- A sulcus depth of about 3 mm leads to the appearance of pocket epithelium with irregular ridges and ulcerations
- Sulcus depth of more than 3 to 5 mm results in the period- dentists
- It is characterized by active bone resorption
Gingival Sulcus Significance:
- The soft tissue wall of the gingival sulcus is prone to infections.
- As the sulcus depth deepens it leads to the periodontal pocket
- which acts as a reservoir for the gingival crevicular fluid
Question 4. Stippling.
Answer:
Stippling It is a form of adaptive specialization or reinforcement for function
Stippling Significance:
- Sign of healthy gingiva
- Loss or reduction – Denotes diseased condition
Stippling Formation:
- By alternate protruberances and depression
- A papillary layer of connective tissue projects into the epithelium
Stippling Diagnosis:
- By drying the gingiva
Question 5. Attached gingiva.
Answer:
Attached Gingiva Definition:
Attached gingiva is defined as that part of the gingiva that is firm, resilient & tightly bound to the underlying periosteum of the alveolar bone
Attached are Gingiva Features:
The surface of the attached gingiva is stippled like an orange peel
- This appearance is most prominent in the facial aspect
- On the facial aspect, the attached gingiva extends upto the alveolar mucosa
- It is demarcated here by the mucogingival junction
- On the Lingual aspect of the mandible, the attached gingiva terminates at the junction of the lingual alveolar mucosa
- The palatal surface of the attached gingiva in the maxilla blends with the palatal mucosa
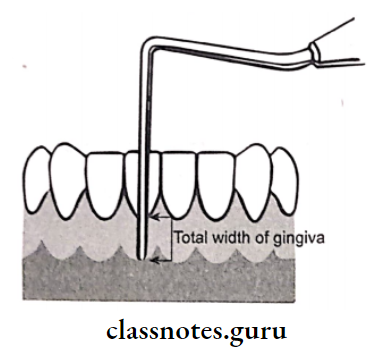
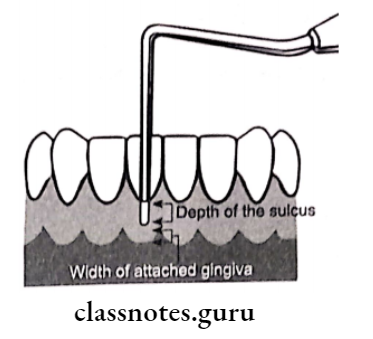
Question 6. How to measure attached gingiva?
Answer:
1. Histological test:
- Schiller’s potassium iodide solution stain
- In this test, Schiller’s potassium iodide solution is applied over gingiva
- This stains the total gingiva.
- Total gingiva is thus measured
- Next measure the pocket depth
- The attached gingiva is calculated by subtracting pocket depth from the total width of the gingiva
2. Anatomical test:
- It includes a measurement approach
- It first, the pocket depth is measured by probing
- Next, the total width of the gingiva is measured
- The attached gingiva is calculated by
- Total width-pocket depth
3. Functional tests:
Tension test:
- Initially, the lip/cheek is stretched
- Observe for the movement of marginal or free gin- give
- Movement of free gingiva indicates inadequate at-attached gingiva
Roll test:
- In this test, adjacent mucosa is pushed coronally
- If the gingiva moves along with it, it donates inadequate attached gingiva
Question 7. Roll test.
Answer:
- In this test, adjacent mucosa is pushed coronally
- If the gingiva moves along with it, it donates inadequate attached gingiva
Question 8. Periosteum.
Answer:
- The periosteum is the tissue covering the outer surface of the bone
- Periosteum consists of
- Inner layers- cells differentiating into osteoblasts
- Outer layer- Blood vessels, nerves, fibers
- Collagen fibers- penetrate the bone
Question 9. Functions of the gingiva.
Answer:
1. Attached gingival:
- Attached gingival braces marginal gingiva
- Attached gingival allows for proper deflection of food
- Attached gingival provides room for proper placement of toothbrush
- Attached gingival is important for the overall maintenance of gingival health
2. Gingival Crevicular Fluid:
- Gingival Crevicular Fluid cleanses material from the sulcus
- Gingival Crevicular Fluid improves the adhesion of the epithelium to the tooth by plasma proteins
- Gingival Crevicular Fluid possesses antimicrobial properties
- Gingival Crevicular Fluid exerts antibody activity to defend gingiva
- Gingival Crevicular Fluid transports a variety of molecules
3. Gingival Fibers:
- Provides support to the gingiva and attaches it to the bone
- Gingival Fibers anchors the tooth to the bone
- Maintains relationship of adjacent teeth
- Secures alignment of teeth in the arch
Question 10. Functions of Gingival Fibers.
Answer:
- Adapts marginal gingiva to tooth
- Withstands forces of mastication
- Unites marginal gingiva to cementum
Question 11. Trans-septal fibers.
Answer:
Trans-septal fibers Location:
- Connects the cementum of one tooth to the cementum of the adjacent tooth
Trans-septal fibers Functions:
- Protect interproximal bone
- Maintain tooth tooth-to-tooth contact
Trans-septal fibers Significance:
- Trans-septal fibers Significance are the last to get destroyed due to disease condition
- Trans-septal fibers Significance are the first to degenerate
Question 12. Blood supply to the gingiva.
Answer:
1. Supraperiosteal arteries:
- Arises from above alveolar bone
- Branches and supplies facial and lingual surfaces
2. Vessels of the periodontal ligament:
- Anastomoses with the capillaries
3. Arterioles emerging from the crest of the interdental septa:
Question 13. Fibroblasts.
Answer:
- Fibroblasts are spindle-shaped cells
- Synthesizes chondroitin sulfate, heparin sulfate, and hyaluronic sulfate
- Synthesizes connective tissue matrix
- Fibroblasts produce
- Collagen fibers
- Reticulin fibers
- Oxytalalan fibers
- Elastin fibers
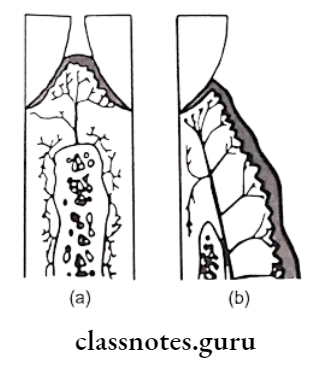
Question 14. Epithelial cell rests on molasses.
Answer:
- It is a remnant of Hertwig’s epithelial root sheath
- Present near and parallel to root surfaces
- Attached to one another by desmosomes
- During disease conditions they undergo proliferation
- Persists as a network strand, island, or tubule
- Exhibits tonofilaments
Question 15. Gingival col.
Answer:
- Col is the depressed central concave area, which fits below the contact point
Gingival col Features:
- Gingival col lies directly below the contact points of the teeth
- Gingival col connects the facial and Lingual papilla
- Gingival col is derived from reduced enamel epithelium
Gingival col Histology:
- The epithelium of the col is non keratinized
- This epithelium is continuous with junctional epithe- lium on each side
- The connective tissue contains xylan fibers
- Its potential as a stagnant site makes it highly susceptible to inflammatory diseases
Question 16. Osteoclast.
Answer:
- Osteoclast are multinucleated giant cells
- Precursor- Blood-borne monocytes
Osteoclast Functions:
- Resorption of bone
- Secretes hydrolytic enzymes
Question 17. Mechanism of tooth Support.
Answer:
1. Tensional theory:
Application of forces
↓
Straightening of principal fiber
↓
Transmission of forces to alveolar bone
↓
Causes elastic deformation of socket
2. Viscoelastic theory:
Transmission of forces to tooth
↓
Transportation of extracellular fluid into marrow spaces
↓
Bundle fibers absorb shock and tighten
Question 18. Difference between acellular and cellular cementum.
Answer:
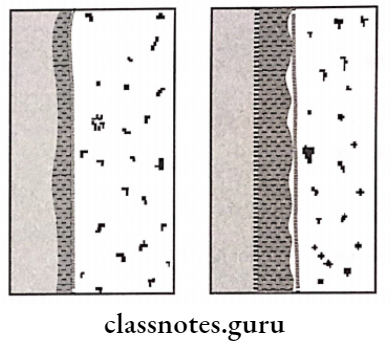
Question 19. Sharpey’s fibers.
Answer:
- Sharpey’s fibers are contained in bundle bone
- Arranged parallel to the root
- Some fibers are completely calcified while most contain an uncalcified central core within a calcified outer layer
Question 20. Bundle Bone.
Answer:
- Bundle Bone is a bone adjacent to the periodontal ligament con- training a great number of Sharpey’s fibers
- Thin lamellae are arranged in layers parallel to the root
- Bundle bone occurs throughout the skeletal system wherever ligaments and muscles are attached
Question 21. Interdental Septum.
Answer:
Interdental Septum Consists of:
- Socket walls
- Facial and lingual plates
Interdental Septum Significance:
- Factors Affecting Its Dimensions:
- Size of adjacent teeth
- Convexity of crowns of adjacent teeth
- Position of teeth in the jaw
- Degree of the eruption of teeth
Question 22. Hypercementosis.
Answer:
- Prominent thickening of cementum
Hypercementosis Types:
- Localized
- Generalized
Hypercementosis Types Localized:
- Excessive tension
- Excessive occlusal forces
Hypercementosis Types Generalized:
- Periapical infections
- Paget’s disease
Question 23. Cemento enamel junction.
Answer:
Cemento Enamel Junction is a junction of the enamel of the crown and the cementum of the root
Cemento Enamel Junction Types:
- 60-65%-Cementum overlaps enamel
- 30%-End to end a relationship
- 5-10%-Cementum and enamel fail to meet
Question 24. Acellular cementum.
Answer:
- Acellular Cementum is first formed cementum
- Acellular Cementum is formed during root formation
- Covers approximately the cervical third or half of the root
- Acellular Cementum does not contain cells
- If interdental space is narrow, the septum may consist
- Acellular Cementum is formed before the tooth reaches the occlusal plane
- Acellular Cementum thickness ranges from 30-230 micrometers
Acellular cementum contains:
1. Sharpey’s fibers:
- Sharpey’s fibers support the tooth
- Inserted at an approximately right angle into root surfaces
- Sharpey’s fibers are completely calcified
2. Intrinsic collagen fibrils:
- Calcified fibers
- Irregularly arranged or parallel to the surface
Question 25. Mast cells.
Answer:
- Mast Cells are small, round, or oval cell
- Contains cytoplasmic granules
- These granules contain heparin and histamine
- During an inflammatory response, these cells release their- time causing the antigen-antibody formation
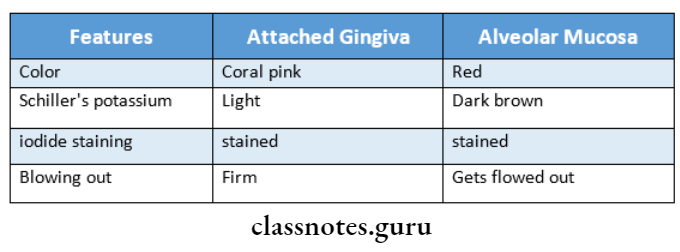
Question 26. Differences between attached gingiva and al-volar mucosa.
Answer:
Question 27. Palatogingival groove.
Answer:
- Palatogingival groove is found primarily on maxillary incisors
- Palatogingival groove is associated with increased plaque accumulation, clinical attachment, and bone loss
- Palatogingival groove are developmental grooves that sometimes appear in maxillary lateral incisors
- Palatogingival groove leads to accessibility problems
Question 28. Define and classify embrasures.
Answer:
Embrasures:
- When two teeth in the same arch are in contact, their curvature adjacent to the contact areas forms spillway spaces called embrasures
Embrasures Functions:
- Provides spillway for food during mastication
- Prevents food from being forced through the contact area
- Make the teeth more self-cleansing
Embrasures Types
- Interproximal embrasure
- Embrasure with no gingival recession
- Larger spaces with exposed root surfaces
Question 29. Functions of cementum.
Answer:
1. Anchorage:
Provides anchorage to the tooth in its alveolus
2. Occlusal maintenance:
Continuous deposition helps in achieving the crown length lost due to attrition
3. Reparative:
- Reparative serves as major reparative tissue for root surfaces
- Reparative maintains the integrity of root surfaces
Question 30. Define periodontal ligament. What does it? Are there small collagen fibers associated with the lar- comprised of?
Answer:
Periodontal Ligament:
Periodontal Ligament is the specialized connective tissue that forms the inter. face between the tooth and the alveolar bone
1. Cellular components:
- Synthesizing cells:
- Fibroblasts
- Cementoblasts
- Osteoblasts
- Resorptive cells:
- Fibroblasts
- Cementoclasts
- Osteoclasts
- Epithelial cells:
- Cell rests of Malassez
- Progenitor cells:
- Undifferentiated mesenchymal cells
- Defense cells:
- Mast cells
- Macrophages
2. Extracellular components:
- Fibers:
- Collagen fibers
- Elastic fibers
- Oxytalan fibers
- Elaunin fibers
- Ground substances:
- Protein polysaccharides
- Glycosaminoglycans
- Proteoglycan
- Glycoprotein
- Fibronectin
3. Connective tissue component:
- Blood vessels
- Nerves
- Lymphatics
Question 31. Define intermediate plexus.
Answer:
- Intermediate Plexus are small collagen fibers associated with the larger principal collagen fibers
- Intermediate Plexusfiber run in all directions forming a plexus called the intermediate plexus
- Intermediate Plexus are reticulate fibers which are fine, immature collagen fibers with a lattice-like arrangement
Question 32. Parts of the alveolar bone
Answer:
The alveolar bone contains two parts
1. Alveolar bone proper
- It is 0.1-0.4 mm thick
- It surrounds the root of the teeth
- Gives attachment to principal fibers of PDL
- Parts
- Lamellated bone
- Contains osteon which contains blood vessel
- Bundle bone
- The bone directly lining the socket is referred to as bundle bone
2. Supporting alveolar bone
- The bone that surrounds the alveolar bone proper and gives support to the socket is called the supporting alveolar bone
- It consists of:
- Cortical plate
- It forms the outer and inner plates of the alveolar processes
- Spongy bone
- It is bone occupying the central part of the al-alveolar process
Question 33. Factors affecting the color of gingiva
- The color of the gingiva normally appears coral pink.
- It depends on
- Degree of keratinization
- Thickness of epithelium
- Degree of pigmentation
- Amount of circulation
Periodontics Normal Periodontium Viva Voce
- The gradual increase occurs in GCF amount from 6:00 am to 10:00 pm and decreases afterward.
- Non-keratinocytes present in the gingival epithelium are: melanocytes, Langerhans cells, Merkel cells
- The junctional epithelium is collar like a band of non-keratinizing epithelium
- Values:
- Stippling is seen in the attached gingiva and central core of the interdental papilla.
- It is absent in marginal gingiva
- Sulcular epithelium is non-keratinized and without recipes
- The junctional epithelium is widest in the coronal portion and thin towards the center
- The turnover rate of junctional epithelium is about 5 days
- The attachment apparatus of the tooth includes the periodontal ligament, cementum, and alveolar bone
- Progenitor cells are undifferentiated mesenchymal cells.
