Non Steroidal Anti Inflammatory Drugs Important Notes
1. Non-Steroidal Anti-Inflammatory Drugs Classification
2. Non-Steroidal Anti-Inflammatory Drugs Aspirin
- Non-Steroidal Anti-Inflammatory Drugs Aspirin Actions
- Inhibits prostaglandin synthesis with resultant analgesic and antipyretic action
- Reduces fever by promoting heat loss
- At high doses, it has anti-inflammatory action
- Stimulates respiration
- Causes dyspepsia, peptic ulceration with GIT hemorrhage
Read And Learn More: Pharmacology Question and Answers
- Non-Steroidal Anti-Inflammatory Drugs Aspirin Adverse effects
- Mucosal damage and peptic ulceration
- Induces asthma by inhibition of prostaglandin synthesis
- Prevent platelet aggregation
- In children causes Reye’s syndrome
- Prolonged intake causes salicylism characterized by
- Tinnitus
- Vertigo
- Drowsiness
- Impairment of vision and hearing
- Non-Steroidal Anti-Inflammatory Drugs Aspirin Contraindications
- Diabetics
- Heart failure patients
- Peptic ulcers
- Pregnant
- Patients receiving oral anticoagulants
- Should be stooped 1 week before elective surgery
- Non-Steroidal Anti-Inflammatory Drugs Aspirin Uses:
- As analgesic, antipyretic, and anti-inflammatory
- The first drug of choice in acute rheumatic fever and rheumatoid arthritis
- In post-myocardial infarction and post-stroke patients
- For local application as keratolytic, fungistatic, and antiseptic
3. Non-Steroidal Anti-Inflammatory Drugs Paracetamol
- Exerts analgesic, antipyretic action
- Has negligible anti-inflammatory action
- Has a high therapeutic index
- Acute Paracetamol poisoning causes
- Skin reactions
- Liver tenderness
- Hepatotoxicity
- Centrilobular hepatic necrosis, renal tubular necrosis, and hypoglycemia
- Haemolysis
- Methemoglobinemia
4. Non-Steroidal Anti-Inflammatory Drugs Phenylbutazone
- Causes
- Bone marrow depression
- Agranulocytosis
- Sodium and water retention
- Precipitates congestive cardiac failure
5. Non-Steroidal Anti-Inflammatory Drugs Diclofenac
- Analgesic, antipyretic, and anti-inflammatory drug
- Accumulates in synovial fluid
- Has a longer duration of action
- Uses:
- Rheumatoid arthritis
- Osteoarthritis
- Renal colic
Non-steroidal anti-inflammatory drugs questions and answers
6. Non-Steroidal Anti-Inflammatory Drugs Mefenamic acid
- Has weaker analgesic action
- Useful in
- Chronic and dull aching pain
- Dysmenorrhea
7. Non-Steroidal Anti-Inflammatory Drugs Ibuprofen
- Has the analgesic and mild anti-inflammatory effect
- Produces less gastric irritation
- Inhibits platelet aggregation
- Prolongs bleeding time
- Contraindicated in
- Pregnant
- Peptic ulcer patients
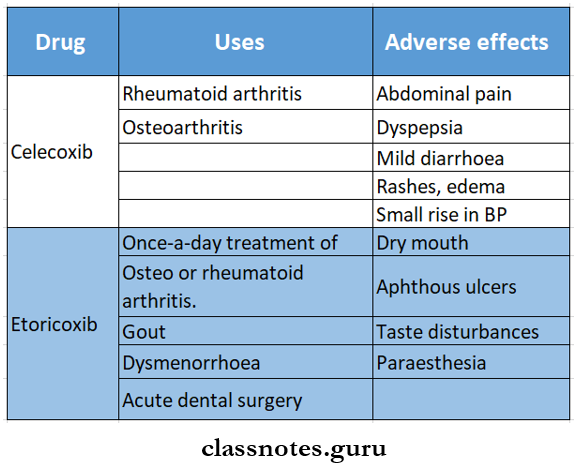
8. Non-Steroidal Anti-Inflammatory Drugs Uses of selective COX-2 inhibitors
- Osteoarthritis
- Rheumatoid arthritis
- Dental and post-operative pain
Non Steroidal Anti Inflammatory Drugs Long Essays
Question 1. Classify nonsteroidal anti-inflammatory drugs. Explain the mechanism of action and uses of ibuprofen.
Answer:
Non-steroidal Anti-inflammatory drugs:
- These are non-opioid analgesics.
- They have anti-inflammatory, antipyretic, and uricosuric properties.
Non-steroidal Anti-inflammatory drugs Classification:
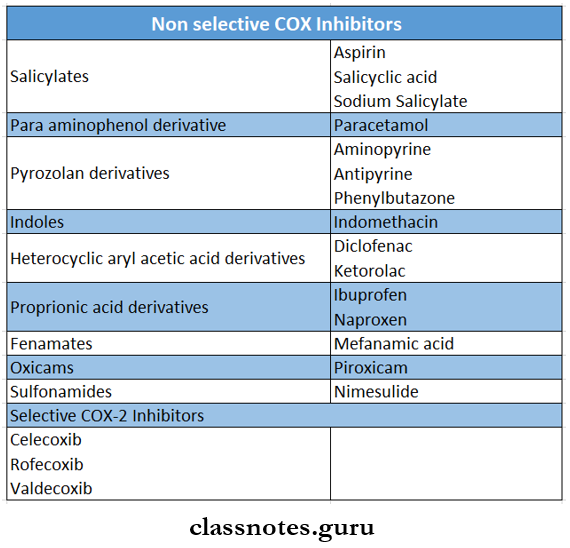
1. Non-selective COX inhibitors.
- Salicylates – aspirin.
- Propionic acid derivatives.
- Ibuprofen, naproxen, ketoprofen.
- Anthranilic acid derivative – mefenamic acid.
- Aryl-acetic acid derivatives – diclofenac, ace- clofenac.
- Oxicam derivatives – perioxicam, tenoxicam.
- Pyrrolo – pyrrole derivative – ketorolac.
- Indole derivative – indomethacin.
- Pyrazolone derivatives – phenylbutazone.
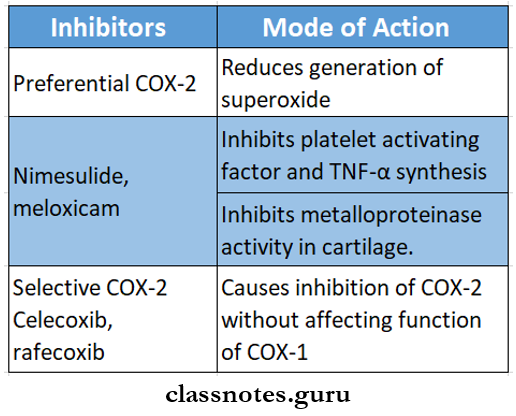
2. Preferential COX-2 inhibitors.
- Nimesulide, meloxicam, nabumetone.
3. Selctive COX-2 inhibotors.
- Celecoxib, etoricoxib, parecoxib.
4. Analgesic – antipyretics with poor anti-inflammatory action.
- Para-aminophenol derivative – paracetamol.
- Pyrazolone derivative – metamizol.
- Benzoxazocine derivative – nefopam.
Ibuprofen:
- Ibuprofen is propionic acid derivative.
Ibuprofen Mechanism of action:
Inflammation
↓
Liberation of arachidonic acid from phospholipids
↓
Cyclo-oxygenase enzyme
↓
Prostaglandin.
↓
Ibuprofen inhibits cyclo-oxygenase enzyme.
↓
Inhibits prostaglandin synthesis.
Ibuprofen Uses:
- As analgesic – in a painful condition.
- As antipyretic – in fever.
- Used when pain is more prominent than inflammation in rheumatoid arthritis, osteoarthritis, and musculoskeletal disorders.
- Soft tissue injuries, fractures.
- Following tooth extraction.
- To relieve postoperative pain.
- Dysmenorrhea.
- Osteoarthritis.
- Gout
- Surgical removal of impacted teeth. It is combined with muscle relaxant
classification of NSAIDs with examples
Question 2. Mention therapeutic uses and adverse effects of aspirin.
(or)
Describe pharmacological actions and therapeutic uses of salicylates.
Answer:
Salicylates/Aspirin:
- Aspirin is acetylsalicylic acid.
Salicylates Actions:
1. Analgesia.
- Aspirin inhibits prostaglandin synthesis and acts as an analgesic.
- It is a weak analgesic.
2. Antipyretic.
- Reduces fever by promoting heat loss.
- It resets the thermostat at a normal level.
3. Anti-inflammatory reaction.
- Aspirin act as an anti-inflammatory at high doses.
- It interferes with the formation of chemical mediators in the kallikrein system.
4. Respiratory.
- Increases consumption of oxygen increases CO2 production.
- This stimulates the respiratory center.
- As a result, the rate, and depth of respiration increase.
5. Acid-base and electrolyte balance.
- At anti-inflammatory doses, salicylates increase CO2 production.
- This results in respiratory alkalosis and pH becomes alkaline.
6. CVS action.
- High doses increase cardiac output
7. GIT action.
- Aspirin is a gastric irritant.
- It causes epigastric distress, nausea, and vomiting.
- At high doses, it stimulates CTZ.
8. Metabolism.
- Aspirin enhances cellular metabolism.
9. Blood.
- It inhibits thromboxane A2 synthesis by platelets.
- Interferes with platelet aggregation.
Salicylates Uses:
1. As analgesic.
- For headache, toothache, backache, joint pain, myalgia, neuralgia, and dysmenorrhoea.
2. As antipyretic.
- Effective in any type of fever.
3. Acute rheumatic fever.
- Aspirin 4 – 6 g/day in 4 – 6 divided doses is given.
- It results in dramatic relief of signs and symptoms in 24 – 48 hours.
4. Rheumatoid arthritis.
- Dose – 3 – 5 g/day.
- Relieves pain, and reduces swelling and redness of joints.
5. Osteoarthritis.
- Provide symptomatic relief.
6. Postmyocardial infarction.
- Aspirin inhibits platelet aggregation and lowers the incidence of reinfarction.
7. Rarely used for.
- Pregnancy-induced hypertension.
- Patent ductus arteriosus in the newborn.
- Familial colonic polyposis.
- Prevention of colon cancer.
- Prevent flushing attending nicotinic acid ingestion.
Salicylates Adverse effects:
- GIT effects – nausea, vomiting, epigastric distress increased occult blood loss in stools.
- Hypersensitivity reactions – rashes, urticaria, rhino-rhea, angioedema, anaphylactoid reaction.
- CNS – headache, dizziness, confusion
- Respiratory system – precipitates asthma.
- Hemolysis – In GPD deficiency patients.
- Hepatotoxicity.
- Nephrotoxicity.
- Reye’s syndrome – a form of hepatic encephalopathy.
- Pregnancy – delays onset of labor.
Salicylates Acute Salicylate Poisoning:
- More common in children.
- Fatal dose -15 – 30 g in adults.
- Symptoms are:
- Vomiting, dehydration, electrolyte imbalance, hyperpyrexia, GI irritation, restlessness, delirium, hallucinations, convulsions, tremors, and death.
- Treatment – symptomatic:
- Gastric lavage.
- Correction of acid-base balance and dehydration by IV fluids.
- Control of temperature by external cooling.
- Blood transfusion and vit K. Administration.
- Use of Vv fluids with Na+, K+, HCo3–, and glucose.
Mechanism of action of NSAIDs
Question 3. Describe pharmacological actions, uses, and adverse effects of propionic acid derivatives.
Answer:
Proprionic Acid Derivatives:
- Proprionic acid derivatives – ibuprofen, naproxen, ke- toprofen, flurbiprofen.
- Proprionic Acid Derivatives Actions:
- Analgesia.
- Anti-pyretic.
- Anti-inflammatory.
- Proprionic Acid Derivatives Uses:
- As analgesic in painful conditions.
- Fever.
- Soft tissue injuries, fractures.
- Following tooth extraction.
- Gout
- Used when pain is more prominent than inflammation in rheumatoid arthritis, osteoarthritis, and musculoskeletal disorders.
- To relieve postoperative pain.
- Dysmenorrhoea.
- Surgical removal of impacted teeth – combined with a muscle relaxant.
Proprionic Acid Derivatives Adverse effects:
- GIT effects – Nausea, vomiting, gastric discomfort
- CNS effects – headache, dizziness, blurring of vision, tinnitus, depression.
- Hypersensitivity reactions – rashes, itching.
- Fluid retention.
Question 4. Compare morphine and aspirin. Write contraindications of morphine.
Answer:
Morphine and aspirin:
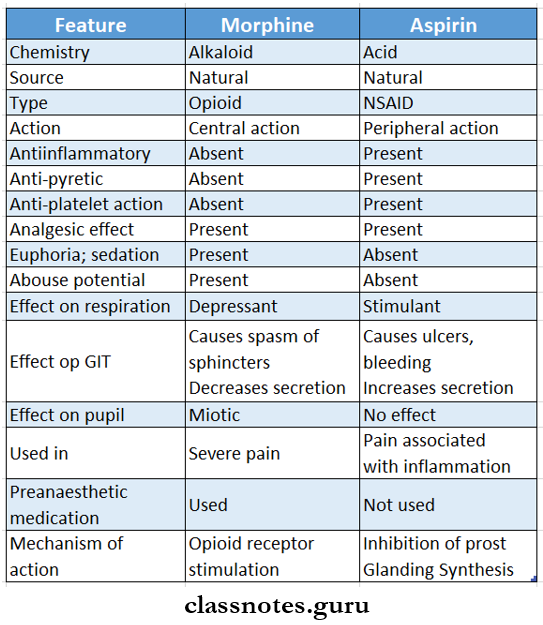
Contra-indication of morphine:
- In extremes of age.
- In patients with respiratory insufficiency.
- In bronchial asthma.
- Elderly males.
- Head injury.
- Hypovolemic shock.
- Undiagnosed acute abdominal pain.
- Unstable personalities.
- Hypothyroidism, renal and liver diseases?
Question 5. Mention two contraindications to morphine.
Answer:
Contraindications of aspirin:
1. Aspirin is contraindicated in patients who are sensitive to aspirin.
2. In peptic ulcers – because.
- It irritates gastric mucosa.
- Stimulates CTZ.
- Inhibits PG synthesis, delays, healing reduces platelet aggregations.
- Decreases gastric acid secretion
- Promotes bleeding in ulcer
3. In children suffering from chickenpox or influenza.
- Develops Reye’s syndrome.
4. In chronic liver disease.
- Causes hepatic necrosis.
5. In bronchial asthma – precipitates attacks.
6. In diabetes.
- Aspirin causes hyperglycemia due to central sympathetic stimulation.
7. Pregnancy
- Delays onset of labor
- Leads to premature closure of ductus arteriosus.
- Increase postpartum bleeding.
8. In Lactating mothers.
9. In G6PD deficiency patients.
- Leads to hemolysis.
NSAIDs contraindications and precautions
Question 6. Define analgesics. List four non-steroidal antiinflammatory drugs belonging to four different chemical groups. Mention therapeutic uses of aspirin. Explain the pharmacological basis of anyone.
Answer:
- Analgesic:
- Analgesic is a drug that selectively relieves pain by acting in the CNS or on peripheral pain mechanisms without significantly altering consciousness.
Non-steroidal anti-inflammatory drugs:
- Salicylates – aspirin.
- Proprionic acid derivatives – Ibuprofen.
- Anthranilic acid derivative – mefenamic acid.
- Aryl acetic acid derivative – diclofenac, aceclofenac.
- Oxicam derivative – piroxicam, tenoxicam,
Uses of Aspirin:
1. As analgesia.
Aspirin act on peripheral pain receptors.
↓
Prevent prostaglandin-mediated
sensitization of nerve endings.
↓
Inhibit prostaglandin synthesis.
↓
Causes analgesia.
2. As antipyretic.
Resets hypothalamic thermostat
↓
Promotes heat loss
↓
Reduces fever.
3. Anti-inflammatory.
Inhibits prostaglandin synthesis
↓
Interferes with the formation of chemical mediators.
↓
Decreases adherence of granulocyte.
↓
Decreases migration of macrophages at the site of inflammation.
4. Acute rheumatic fever.
5. Rheumatoid arthritis.
6. Osteoarthritis.
7. Post myocardial infarction.
Non Steroidal Anti Inflammatory Drugs Short Essays
Question 1. Mention an antidote for paracetamol poisoning. How does it act?
Answer:
Paracetamol Poisoning:
- When a large dose of paracetamol is taken serious toxicity can occur.
Manifestations:
- Early manifestations – Nausea, vomiting, abdominal pain, liver tenderness.
- After 12 – 18 hours – Centrilobular hepatic necrosis, renal tubular necrosis, hypoglycemia, coma.
- After 2 days – jaundice.
- Later – Fulminating hepatic failure and death
Mechanism:
1. At normal doses.
Paracetamol.
↓
M etabolite N -acteyl-p-benzoquinoneimine.
↓
Gets detoxified by glutathione.
2. At high doses.
High doses of paracetamol
↓
Increases production of metabolite
↓
Glutathione is depleted
↓
Thus, metabolite covalently binds to
proteins in liver cells.
↓
Causes necrosis.
Antidote:
- N-acetylcysteine is infused by IV or given orally.
- It replenishes hepatic glutathione.
- Prevents binding of metabolite to another cellular constituent
Question 2. Compare paracetamol and aspirin.
Answer:
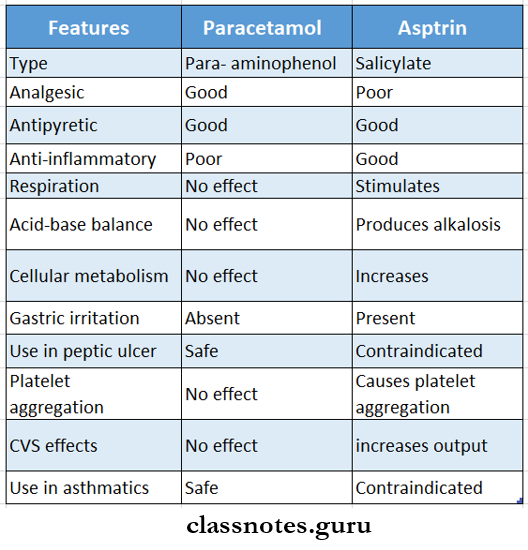
NSAIDs classification and mechanism
Question 3. Selective COX-2 inhibitors.
Answer:
Selective COX-2 inhibitors are coxibs-celecoxib, rofecoxib, parecoxib, etoricoxib and valdecoxib.
Selective COX-2 inhibitors Advantages:
- Less gastric irritation.
- Less occurrence of peptic ulcers.
- Do not depress thromboxane A2 production by platelets.
- Do not inhibit platelet aggregation.
Selective COX-2 inhibitors Disadvantages:
- Increases risk of
- Cardiovascular events
- Cerebrovascular thrombotic events.
- Myocardial infarction.
Selective COX-2 inhibitors Indications:
- Patients who cannot tolerate NSAIDs
- Patients with a high risk of developing.
- Peptic ulcers.
Selective COX-2 inhibitors Contraindications:
- It is avoided in patients with.
- Ischaemic heart disease.
- Hypertension
- Cardiac failure.
- Cerebrovascular disease.
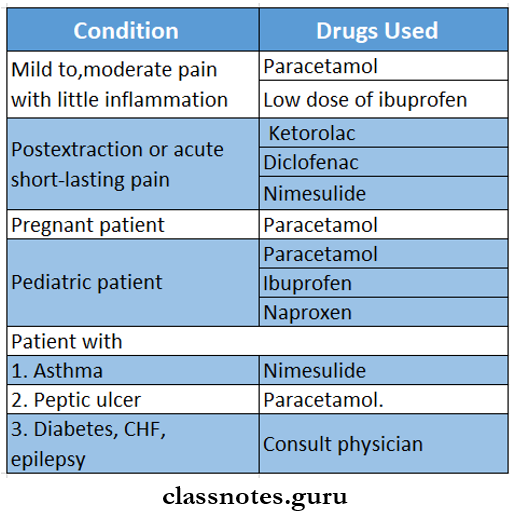
Question 4. Write a brief account of drugs in dental pain.
Answer:
The selection of drugs depends on.
- Nature of pain – acute or chronic.
- Type of pain-mild, moderate, severe
- Cause of pain.
- Risk factors
- Individual preference.
- Presence or absence of inflammation.
Question 5. Explain why nimesulide is preferred over aspirin as an anti-inflammatory agent.
Answer:
Nimesulide:
- It exhibits relative COX-2 selectivity.
- It is completely absorbed orally.
- 99% plasma bounded.
- Exerts reduce the generation of superoxide by neutrophils.
- Acts as a free radical scavenger.
- Inhibits metalloproteinase activity in cartilage.
- Aspirin:
- Produces salicylism.
- In children – may cause liver damage.
- In adults – causes hepatic injury.
- Contraindicated in patients with.
- Peptic ulcer
- Children suffering from influenza
- Chronic liver diseases.
- Diabetes.
- Lactating mothers.
- Thus, nimesulide is superior to aspirin.
Question 6. Aspirin.
Answer:
- It is acetyl-salicylic acid
Aspirin Actions:
- Analgesia – inhibits prostaglandin synthesis
- Antipyretic – promotes heat loss
- Anti-inflammatory – interferes with the formation of chemical mediators of the Kallikeren system
- Respiratory
- Increases consumption of oxygen
- Increases production of carbon dioxide
- Stimulates respiratory center
- Increases rate and depth of respiration
- Acid-base and electrolyte balance
- Causes an increase in the production of carbon dioxide leading to respiratory alkalosis
- CVS action – increases cardiac output
- GIT action
- Stimulates CTZ
- Causes epigastric distress, nausea, vomiting
- Metabolism – enhances cellular metabolism
- Blood
- Inhibits thromboxane A2 synthesis
- Interferes with platelet aggregation
Aspirin Uses:
- As an analgesic for headaches, dental pain, back pain, and joint pain, myalgia
- As antipyretic
- Acute rheumatic fever – dose – 4-6 g/day in 4-6 divided dose
- Rheumatoid arthritis – dose – 3-5 g/day
- Osteoarthritis
- Postmyocardial infarction – inhibits platelet aggregation
- Rarely used in
- Pregnancy induces hypertension
- Patent ductusarteriosus in newborn
- Familial colonic polyposis
- Prevention of colon cancer
Aspirin Adverse Effects:
- GIT effects – nausea, vomiting, epigastric distress, increased occult blood loss in stool
- Hypersensitivity reactions – rashes, urticaria, rhinos-rhea, angioedema, anaphylactic reaction
- CNS – headache, dizziness, confusion
- Respiratory system – precipitates asthma
- Hemolysis
- Hepatotoxicity
- Nephrotoxicity
- Reye’s syndrome
- In pregnancy – delays the onset of labor
Non Steroidal Anti Inflammatory Drugs Short Question And Answers
Question 1. Paracetamol.
Answer:
Paracetamol is active metabolite of phenacetin.
Paracetamol Actions:
- Central analgesic action.
- Good antipyretic
- Weak anti-inflammatory.
- Active on cyclo-oxygenase in the brain.
Paracetamol Uses:
- As analgesic – toothache, headache, myalgia.
- As antipyretic – to reduce fever.
- In dentistry – in chronic pulpitis, periodontal abscess, post-extraction – used with ibuprofen.
Paracetamol Adverse effects:
- Nausea.
- Rashes
- Rarely leukopenia.
Question 2. A low dose of aspirin is administered prophylactically.
Answer:
- Aspirin in low doses irreversibly inhibits thromboxane A2 synthesis.
- It produces an antiplatelet effect
- Thus, it is used in the prophylactic treatment of various thromboembolism like myocardial infarction.
- To reduce the incidence of recurrent infarction.
- To decrease mortality in post-MI patients.
Non-steroidal anti-inflammatory drugs questions and answers
Question 3. Uses of aspirin.
Answer:
- As analgesic
- As antipyretic.
- Acute rheumatic fever
- Rheumatoid arthritis.
- Osteoarthritis.
- Postmyocardial infarction.
- Rarely in
- Pregnancy-induced hypertension.
- Patent ductus, arteriosus in newborns.
- Familial colonic polyposis.
- Prevention of colon cancer.
- To prevent flushing attending nicotinic acid ingestion.
Question 4. Contraindications of aspirin.
Answer:
- In patients sensitive to aspirin.
- In peptic ulcers.
- In children suffering from chickenpox or influenza.
- In chronic liver disease
- In bronchial asthma.
- In diabetics
- Pregnancy.
- Lactating mothers.
- In G6PD deficiency patients.
Question 5. Nimesulide.
Answer:
Nimesulide is a sulphonamide compound.
- It is a weak inhibitor of PG synthesis.
Nimesulide Actions:
- Inhibits leukocyte function.
- Prevents release of mediators.
- Has antihistaminic and antiallergic properties.
- Has analgesics, antipyretic and anti-inflammatory actions.
Nimesulide Uses:
- Used primarily for short-lasting painful inflammatory conditions like sports injuries, sinusitis, ENT disorders, dental surgery, bursitis, and dysmenorrhoea.
Adverse Effects:
- GIT effects – heart bum, nausea, loss of stools
- Skin effects – rashes, pruritis.
- Nephrotoxicity.
- Prolonged use causes hepatotoxicity.
Question 6. Phenylbutazone.
Answer:
Phenyl butanone is a pyrazolone derivative.
- It is good anti-inflammatory action.
- But poor analgesic and antipyretic action.
Phenylbutazone Uses:
- Rheumatoid arthritis.
- Ankylosing spondylitis.
- Osteoarthritis.
- Gout
- Musculoskeletal disorders.
Phenylbutazone Adverse Effects:
- GIT effects – dyspepsia, epigastric distress, nausea, vomiting.
- Precipitate CCF, edema.
- CNS effects – insomnia, vertigo, optic neuritis, convulsions.
- Inhibit iodine uptake.
- Hypersensitivity reactions – rashes, serum sickness, stomatitis, dermatitis.
- Hematological complications – bone marrow depression, aplastic anemia, agranulocytosis, thrombocytopenia.
Question 7. The rationale of using aspirin in post-myocardial infarction.
Answer:
Aspirin irreversibly inhibits platelet cyclo-oxygenase
↓
Inhibits thromboxane A2 synthesis by platelets
↓
Interferes with platelet aggregation
↓
Lower incidence of reinfarction.
↓
Decreases incidence of transient ischaemic attacks and stroke.
- Thus, aspirin is used in postmyocardial infarction.
Non-steroidal anti-inflammatory drugs questions and answers
Question 8. Enumerate COX-2 inhibitors. Describe their mode of action.
Answer:
COX-2 inhibitors are: