Salivary Gland Disorders Important Notes
1. Classification Of Salivary Gland Disorders
- Developmental Anomalies:
- Agenesis
- Atresia
- Hypoplasia
- Ectopia
- Obstructive Lesions:
- Mucocele
- Sialolithiasis
- Infective Lesions:
- Bacterial sialadenitis
- Viral sialadenitis
- Immune Disorders:
- Sjogren’s syndrome
- Mikulicz’s disease
- Functional Disorders
- Ptyalism
- Xerostomia
- Tumors:
- Epithelial Tumours:
- Adenomas
- Plemic adenoma
- estadenoma Sasa cel adenom
- Warthin’s tumour
- Carcinoma:
- Adenocarcinoma
- Epidermoid carcinoma
- Non Epithelium Tumours:
- Fibroma
- Lipoma
- Lymphoma
- Malignant lymphoma
- Secondary Tumours
- Unclassified Tumours
- Tumour Like Lesions
- Sialadenitis
- Oncocytosis
- Necrociting sintometaplasia
- Epithelial Tumours:
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
2. Composition Of Sialolith:
- Calcium phosphate
- Calcium carbonate
- Saints of Mg. Zmec
- Glycoproteins
- Mucopolysaccharides
- Cellular debris’
3. Stalolith Is Common In The Submandibular Gland Due To:
- Due to viscous secretion
- Higher concentration of calcium & phosphate
- Tortuous anatomy of the ducts
- Dependent position of the gland
Salivary Gland Disorders Long Essays
Question 1. Describe clinical features & treatment of salivary calculus of Wharton’s duct and Etiology
Or
Sialolithiasis.
Answer:
Deffiniton Of Sialolithiasis:
Sialolithiasis is an obstructive disorder of the salivary gland. It is a pathological condition characterized by the presence of one or more calcified stones within the salivary gland itself or within its duct
Clinical Features Of Sialolithiasis:
- Age: Middle-aged adults
- Sex: Common in males
- Site: Common in the submandibular gland due to the following:
- Due to viscous secretion
- Higher concentration of calcium & phosphate
- Tortuous anatomy of the ducts
- Dependent position of the gland
Features Of Sialolithiasis:
- Recurrent swelling of the gland region
- Recurrent episodes of sialadenitis
- Tense & tender gland
- Aggregates at mealtime
- Type Of Pain: Pulling or drawing sensation
- Severe, stabbing type
- Enlarged gland
- Location: Unilateral
- In Chronic Cases: Formation of fistulas, sinus tracts & ulcerations in the area
- Necrosis of the gland acini
- Lobular fibrosis
- Complete loss of secretion of the gland
- So there is an increased risk of infections
Diagnosis Of Sialolithiasis:
- Manual palpation
- Occlusal radiograph in case of submandibular gland
- Sialography
Treatment Of Sialolithiasis:
- For Submandibular Gland:
- Locate the sialolith radiographically
- Suture behind & below the duct to prevent the spillage of stone
- If sialolith is present posteriorly, an incision is given medially
- If sialolith is present anteriorly, an incision is placed medial to plica sublingual is
- Locate the duct
- Locate the stone
- Incise over the stone
- Remove it through the forceps
- For parotid Gland Of Sialolithiasis:
- Locate the sialolith
- Semilunar incision given anterior to the opening of the duct
- Reflection of gland
- Locate the stone
- Incise over the stone
- Remove it
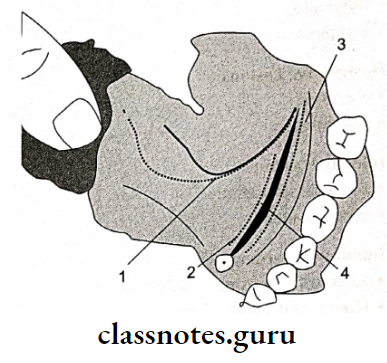
- Lingual nerve-superficial course
- The incision for anterior stone
- The incision for posterior stone
- Sub- mandibular duct
Question 2. Classify salivary gland disorders. Describe in detail about pleomorphic adenoma.
Or
Define Pleomorphic adenoma
Answer:
Classification Of Salivary Glands Disorders:
1. Developmental Anomalies:
- Agenesis
- Atresia
- Hypoplasia
- Ectopia
2. Obstructive Lesions:
- Mucocele
- Sialolithiasis
3. Infective Lesions:
- Bacterial sialadenitis
- Viral sialadenitis
4. Immune Disorders:
- Sjogren’s syndrome
- Mikulicz’s disease
5. Functional Disorders:
- Ptyalism
- Xerostomia
6. Tumours:
- Epithelial Tumours
- Adenomas
- Pleomorphic adenoma
- Cystadenoma
- Basal cell adenoma
- Warthin’s tumor
- Carcinoma
- Adenocarcinoma
- Epidermoid carcinoma
- Non-Epithelial Tumours
- Fibroma
- Lipoma
- Lymphoma
- Malignant Lymphoma
- Secondary Tumours
- Unclassified Tumours
- Tumour Like Lesions
- Sialadenitis
- Oncocytosis
- Necrotizing sialometaplasia
Pleomorphic Adenoma:
1. Clinical Features Of Pleomorphic Adenoma:
- Age: 5th & 6th decade
- Sex: Common in females
- Site: Common in the parotid gland
2. Features Pleomorphic Adenoma:
- Slow growing
- Exophytic growth
- Solitary lesion
- Swelling of gland
- The smooth surface of the lesion
- No pain
- Superficial lesions
- Located near the angle of the mandible
- Deeper lesions:
- Over the lateral wall of the oropharynx
- Minor gland neoplasms exhibit firm, nodular swelling
- The palatal lesion causes surface ulceration
- In buccal mucosa, it is present as a small, painless nodular lesion
3. Treatment Pleomorphic Adenoma:
- Surgical excision-parotidectomy
4. Complication Pleomorphic Adenoma:
- Facial palsy
- Frey’s syndrome
Question 3. Write in detail about necrotizing sialometaplasia.
Answer:
Necrotizing Sialometaplasia:
Necrotizing Sialometaplasia is a spontaneous disease of unknown etiology, characterized by necrosis of minor salivary glands of the palate along with the surface epithelium & underlying connective tissue
Etiology Of Necrotizing Sialometaplasia:
- Probably due to local ischemia
- Local trauma from a denture
- Alcohol & tobacco
Clinical Features Of Necrotizing Sialometaplasia:
- Age: Old age, around 47 years on average
- Sex: Common in males
- Site: Common over palate & oral mucosal sites
Features Of Necrotizing Sialometaplasia:
- Appears: As deep-seated punched-out ulceration
- Location: Bilateral
- Borders rolled borders
- Surface: Few granular lobules present
- Size: 2-3 cm in diameter
- Symptoms: Asymptomatic
- Some may complaint of burning sensation Future: heals spontaneously
Treatment Of Necrotizing Sialometaplasia:
- Discontinue the use of dentures till the ulcer heals
- Regular irrigation with dilute hydrogen peroxide
- Antibiotics & analgesic
- The lesion usually heals spontaneously
Salivary Gland Disorders Short Essays
Question 1. Sialolithiasis Or Salolith of Etiology And Pathogenesis and Composition
Answer:
Etiology Of Sialolithiasis:
- Stagnation of saliva
- Ductal epithelial inflammation & injury
- Biological factors
Pathogenesis Of Sialolithiasis:
- Formation of the soft nidus of mucin, protein, bacteria &
- desquamated cells.
- Allows concentric, lamellar crystallization
- Gradually sialolith increases in size
Composition Of Sialolithiasis:
- Calcium phosphate
- Calcium carbonate
- Salts of Mg, Zn, etc
- Glycoproteins
- Mucopolysaccharides
- Cellular debris
Question 2. Bacterial sialadenitis.
Answer:
Etiology Of Bacterial Sialadenitis:
- Staphylococcus aureus
- Streptococcus pyogenes
- Less common Hemophilus & bacteroids
Route Of Infection Of Bacterial Sialadenitis:
- Parotid duct
Predisposing Factors Of Bacterial Sialadenitis:
- After surgery
- Dehydration
- Diabetes
- Malignancy
- Sjogren’s syndrome
- Sialolithiasis
Clinical Features Of Bacterial Sialadenitis:
- Gland involved: Parotid Location: unilateral or bilateral
- Signs: Swelling of the gland Symptoms: Pain
- Fever
- Malaise
- Redness of the skin
- Difficulty in swallowing
- Trismus
- Exudation of pus
Treatment Of Bacterial Sialadenitis:
- Antibiotics penicillin
- Gentle massage over the gland
- Incise to drain the gland
- Remove or cause
Question 3. Sialography.
Answer:
Sialography
Used for investigation of sialolith
The Procedure Of Sialography:
- Identification of duct
- Exploring of the duct
- Introduction of cannula
- Introduce contrasting media
- Lipid soluble or
- Water soluble agents
- Amount of the agent
- Submandibular gland: 0.5-0.75 ml
- Parotid gland 0.76-1ml
- Radiograph is taken
- Occlusal view
- AP view
Interpretation Sialography:
- Parotid gland- Tree in winter appearance
- Submandibular gland – Bush in winter appearance
- Sjogren’s syndrome – Cherry blossom appearance
- Malignant tumor- Ball holding in hand appearance
Question 4. Parotidectomy.
Answer:
Parotidectomy
Parotidectomy is a surgical treatment for salivary gland tumors
Types Of Parotidectomy:
- Superficial Parotidectomy:
- Anaesthesize
- Incision over the preauricular crease, curved downward upto tip of the mastoid
- Elevation of skin & superficial fascia
- Preserve the facial nerve
- Dissect the gland away from each branch of the gland
- Hemostasis
- Placement of drains
- Suturing
- Total Parotidectomy:
- Involves the removal of entire parotid gland
- Superficial parotidectomy done
- Then remove tumor deep into the facial nerve
Question 5. How to investigate the of salivary gland
Answer:
Investigation Of Salivary Gland:
- Duration of the lesson:
- Longer duration, malignancy
- Nature of onset
- Gradual & painless, malignant
- Sudden & painful, inflammatory
- Rapidity of growth
- Slow benign
- Rapid malignant
- Associated symptoms
- Discharge of pus
- Dryness of mouth
- Constitutional symptoms
- FNAC to rule out malignancy
- CT Scan for deeper lesions
- FNAC for lymph nodes involvement
- X-ray of bone for resorption
Salivary Gland Disorders Short Question And Answers
Question 1. Mucocele.
Answer:
Etiology Of Mucocele:
- Trauma or obstruction of minor salivary gland
Types Mucocele:
- Mucous Retention Cyst:
- Most common
- Caused by trauma
- Causes leakage of saliva into the submucosal tissue
- Results in inflammation of surrounding tissues
- Mucous Retention Cyst:
- Less common
- Caused due to obstruction
- Results in the dilation of the duct
Features Of Mucocele:
- Asymptomatic
- Superficial lesions:
- Less than 1 cm in size
- Thin-walled bluish lesion
- Deeper lesions:
- Well circumscribed
- Covered by normal mucosa
Treatment Mucocele:
- Surgical excision
Question 2. Frey’s syndrome.
Answer:
Frey’s Syndrome
This is auriculotemporal nerve syndrome
Causes Frey’s Syndrome:
- Iatrogenic causes followed by parotidectomy
Features Of Frey’s Syndrome:
- Pain in auriculotemporal nerve distribution
- Gustatory sweating
- Flushing on the affected side
Diagnosis Of Frey’s Syndrome:
- Positive starch iodine test
Treatment Frey’s Syndrome:
- Topical application of anticholinergic
- Radiation therapy
- Surgical procedures
- Skin excision
- Nerve section
- Tympanic neurectomy
Question 3. Ranula.
Answer:
Ranula:
- A special type of mucocele
- Resembles the belly of a frog
Site Of Ranula:
- The floor of the mouth
- Superficial or deep to mylohyoid muscle
Cause Of Ranula:
- Trauma to duct
Features Of Ranula:
- Slow-growing unilateral lesion
- Soft & freely movable
- Superficial lesions
- Thin-walled bluish lesion
- Deeper lesions
- Well circumscribed
- Covered by normal mucosa.
Types Ranula:
- Simple type
- Plunging ranula
Treatment Ranula:
- Marsupialization
Question 4. Sjogren’s syndrome
Answer:
Sjogren’s Syndrome:
- It is a chronic autoimmune disease
- Characterize by oral & ocular dryness, exocrine dysfunction & lymphocytic infiltration
Types Of Sjogren’s Syndrome:
- Primary: It involves the salivary & lacrimal gland
- Secondary: It also involves other connective tissue disease (rheumatoid arthritis, scleroderma)
Etiology Of Sjogren’s Syndrome:
- Etiology Of Sjogren’s is unknown
Presentation Of Sjogren’s Syndrome:
- Decreased salivary function
- Dry mouth
- Difficulty in chewing, swallowing & speech
- Increased risk of caries
- Altered taste
- Dry, cracked lips
- Angular cheilitis
- Mucosa is painful & sensitive to species
- Mucosa is pale & dry
- Friable or furrowed
- Minimal salivary pooling
- The tongue is smooth & painful
- Increased dental caries & erosion of enamel Susceptible to infection
- Increased risk of developing malignant lymphoma
- Difficulty in wearing dentures
- From one third to one-half of the patients have diffuse, firm enlargement of major salivary glands
- Swelling is usually bilateral
- Maybe non-painful or slightly tender
- May be intermittent or persistent
- Due to decreased salivary flow, there is a high risk of bacterial sialadenitis
Salivary Gland Disorders Viva Voce
- Ageusia refers to loss of taste
- Fordyce’s disease is due to aberrant sebaceous glands
- Sialoliths are most commonly found in the submandibular gland
- Treatment of mucocele is by excision
- Recurrent ranula is best treated by sublingual gland excision
- Stenson’s duct is the drainage duct of the parotid salivary gland
- Sialcangiectasis denotes that the salivary gland and duct system are vastly dilated
- While removing a submandibular gland one encounters the facial artery, facial vein, a cervical branch of the facial nerve, and lingual nerve
- The early manifestation of sialadenitis on a scalogram is terminal acini are dilated
- Warthin’s tumor is a benign parotid tumor
- A mucoepidermoid tumor is malignant
