Maxillofacial Surgery Miscellaneous Short Essays
Question 1. TNM Staging.
Answer:
TNM Staging
- T Size of the tumor
- N lymph node involvement
- M distant metastasis
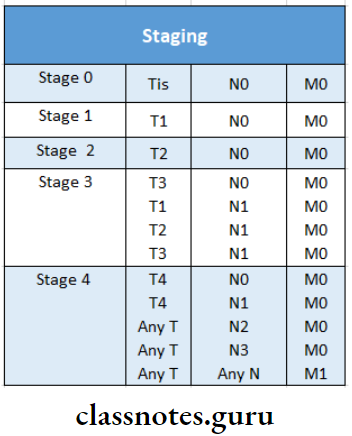
- T0N0 tumor present
- This carcinoma in situ
- T1 Tumour 2 cm or less
- T2 Tumour between 2-4 cm
- T3 Tumour more than 4 cm
- T4 Tumour invading adjacent structures
- N0 No node involvement
- N1 ipsilateral lymph node involvement of 3 cm or less
- N2 ipsilateral lymph node involvement of more than 3 cm or less than 6 cm
- N3 Contralateral node involvement
- M0 no metastasis
- M1 metastasis present
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
Question 2. Cryosurgery.
Answer:
Cryosurgery
- Introduced by Barnard
- Temperature: 20 degrees to -180 degrees
Apparatus Of Cryosurgery:
- Cylinder carrying gases No or CO2
- Probe
- The cord connecting the above two
Technique Of Cryosurgery:
- Anesthetize the area
- Freeze the exposed nerve for 2 min
- Thaw it for 5 min
- Freeze is next for 3 minutes
Effects Of Cryosurgery:
- Dehydration
- Denaturation pf lipid molicules
- Necrosis of tissues, capillaries, small arterioles and venules
Question 3. Champy’s osteosynthesis lines.
Or
Champy’s Lines
Answer:
Champy’s Osteosynthesis Lines
Introduced by Champy et al in France
- He advocated the use of small, thin malleable stainless steel plates used with monocortical screws, placed in specific areas in the mandible.
- The masticatory forces that are produced during the functional loading of the manciple produce a natural strain of compression along the lower border of the mandible
- Champy found that these are ideal osteosynthesis lines of the mandible
- Miniplates with monocortical screws must be placed only along these lines in the region of fracture to achieve maximum stability.
Factors Considered Of Champy’s Osteosynthesis:
- Thickness of bone
- Position of the inferior alveolar canal
- Root apices
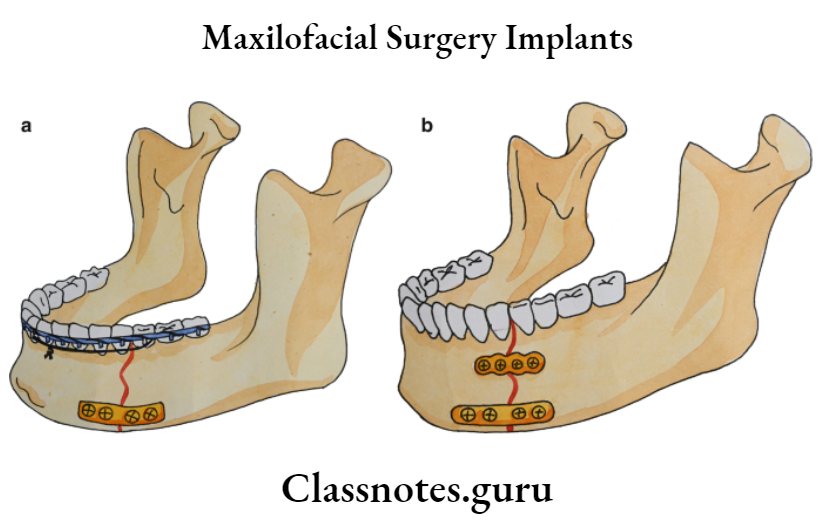
Lines Of Champy’s Osteosynthesis:
- Superolateral aspect along the external oblique ridge
- Inferior border of the mandible
Question 4. Antibiotics for oral infection.
Answer:
Antibiotics For Oral Infection:
Question 5. Antiseptics.
Answer:
Antiseptics: Antiseptics is a chemical that is applied to living tissues such as mucous membranes to reduce the number of microorganisms present, through inhibition of their activity
Requirements Of Antiseptics:
- A broad spectrum of activity
- Fast acting
- Not affected by physical factors
- Nontoxic
- Surface compactable
- Easy to use
- Odourless
- Economical
Agents Of Antiseptics:
- Alcohols: Ethyl alcohol
- Iodophorspovidone iodine
- The hepatitis virus is not susceptible to it
- Formulated as 1% iodine solution
- Not stable at high temperature
- Hexachlorophene
- Toxic
- Used in patients who are sensitive to iodine
- Chlorhexidine0.075%
Question 6. Syncope diagnosis and management.
Answer:
Predisposing Factors Of Syncope:
- Pain
- Anxiety
- Fatigue
- Fasting
- Upright position
- Sight of instruments
- Sight of blood
Presentation Of Syncope:
- Feeling of warmth
- Sweating
- Dilated pupils
- Cold extremities
- Bradycardia
- Dizziness
- Loss of consciousness
Management Of Syncope:
- Loosening of clothes
- Monitor vital signs
- Place cotton soaked in ammonia near the patient’s nose
- Reassure the patient
- Discharge the patient on that day
Question 7. Indication for blood transfusion.
Answer:
Indication For Blood Transfusion
- Acute hemorrhage
- Major road accidents
- Chronic blood loss
- Preoperatively
- Intraoperatively
- In severe malnutrition
- In erythroblastosis fetal
- In anaemic patients
- Postoperatively
- During chemotherapy in malignancies
Question 8. Medical emergency drug tray.
Answer:
Primary Emergency Drugs:
1. Injectable:
- Anaphylactic: Epinephrine 0.3-0.5 ml of 1: 1000 IM
- Antiallergic: Chlorpheramine malate10 mg/ml
2. Noninjectable:
- Oxygen 1-liter cylinder
- Vasodilator
- Nitroglycerine 0.4 mg sublingually
- Antihyperglycemic
- Dextrosebolus form
Secondary Emergency Drugs:
1. Injectable:
- Anticonvulsant: Diazepam5 mg/ml
- Analgesic: Meperidine 10 mg/ml
- Vasopressor: Phenylephrine 10 mg/ml
- Corticosteroid: Dexamethasone50 mg/ml
2. Non Injectable:
- Respiratory stimulant
- Ammonia 0.3 ml/vaprole
Question 9. Cardiac arrest.
Answer:
Cardiac Arrest
Cardiac Arrest is an emergency
Management Of Cardiac Arrest:
- Cardiac arrest includes ABC
1. Airway Maintenance:
- The airway is kept patent
- Steps
- Head Tilt:
- Place the palm on the patient’s forehead
- Other to support the patient’s neck
- Tilt the head backward
- Chin Lift:
- Place hand over the bony chin
- Pull the mandible forward
- Jaw Thrust:
- Head Tilt:
2. Breathing:
- Mouth-to-mouth respiration Mouth-to-nose respiration
- To inflate the lungs
- Monitor vital signs
- Check carotid pulse
- If absent, cardiac massage
3. Circulation:
- Through external cardiac compression
- Apply pressure over the lower half of the adult sternum
Effects Of Cardiac Arrest:
- Increased pressure within the thorax
- Increased cardiac output
Question 10. Significance of liver failure.
Answer:
Significance Of Liver Failure
- Drugs play an important role in surgery
- They are either preoperatively intraoperatively or postoperatively
- These undergoes metabolism
- Thereby reaching the target site
- Many drugs are synthesis in the liver
- Thus liver plays an important role
- If the patient is suffering from liver failure drugs cannot reach the target site
- Hence its action is hampered
- Also, the liver plays an important role in the synthesis of many Vitamins
- As vitamins are essential nutrients in our diet, the liver plays an important role in
Question 11. Radiolucent lesions of angle of mandible.
Answer:
Radiolucent Lesions Of Angle Of Mandible
It includes
1. Ameloblastoma:
Clinical Features Of Ameloblastoma:
- Swelling & pain in the region
- Inflammation
- Tension.
- Dental trauma
- Ulceration of mucosa
- Loosening of teeth
- Epistaxis
- Nasal obstruction
Radiological Features Of Ameloblastoma:
- Unilocular or multi locular radiolucency
- Soap bubble appearance of the lesion
- Border is clear
- Resorption of the teeth
2. Dentigerous Cyst:
Clinical Features Of Dentigerous Cyst:
- Sex: Common in males
- Age: 1st& 3rd decade
- Site: Mandibular 3rd molar, maxillary canines, maxillary 3rd molar
- Expansion of bone
- Facial asymmetry
- Displacement of adjacent teeth.
- Resorption of adjacent teeth
Radiological Features Of Dentigerous Cyst:
- The unilocular, well-defined radiolucency
- Marginssclerotic
Types Of Dentigerous Cyst:
- Centralcovering the crown of an unerupted tooth
- Circumferentialcovering the crown from all sides
- Lateralcovering crown from side
Odontogenic Keratocyst:
1. Clinical Features Of Odontogenic Keratocyst:
- Asymptomatic
- If secondary infected, causes expansion of cortical plates
- Mobility of teeth
- Pain & tenderness of the site
2. Radiological Feature Of Odontogenic Keratocyst:
- Unilocular or multilocular radiolucency
- Margins: Well-defined sclerotic margins
- Expansion of cortical plates
- Soap bubble appearance
Question 12. Dry socket.
Answer:
Definition Of Dry Socket:
Dry socket is focal osteomyelitis of the tooth socket in which the blood clot has disintegrated or been lost
Other Names Of Dry Socket:
- Fibrinolytic alveolitis
- Alveolar osteitis
- Alveolar osteomyelitis
Etiology Of Dry Socket:
1. Born’s Hypothesis:
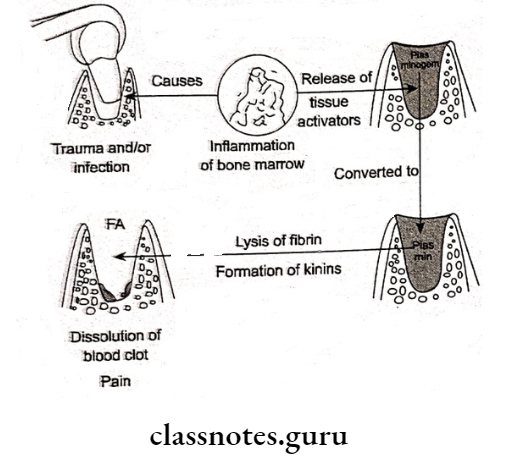
2. Nitzan’s Theory:
- States that there is a possible relationship between the fibrinolytic activity of anaerobic bacteria & dry socket
Pre-Disposing Factors Of Dry Socket:
- Infection
- Decreased blood supply
- Debilitating conditions
Clinical Features Of Dry Socket:
- Loss of blood clot
- Bare of granulation tissue
- Radiating pain
- Foul odor
- Metallic taste
Management Of Dry Socket:
- Irrigation of socket
- Smoothening of bony margins
- Packing with pom pom
- Analgesics
- Hot saline mouth bath
- Chemical cauterization Regular follow-up
Question 13. Indications of laser therapy.
Answer:
Indications Of Laser Therapy
- Incision
- Excision
- Biopsy of cystic lesions
- Vaporise excess tissue
- Frenectomy
- Remove/reduce hyperplastic tissues
- Hemostatic
- In the treatment of Hemangioma
Question 14. Von Willebrands disease.
Answer:
Von Willebrands Disease
Deficiency of Factor VIII von Willebrand factor
Clinical Features Of Von Willebrands:
- Epitaxis
- Menorrheoa
- Bleeding followed by minor trauma
Lab Investigations Of Von Willebrands:
- Bleeding time increased
- Prothrombin time – normal
- 8th Creduced
- ve reduced
Treatment Of Von Willebrands:
- Administration of vasopressin
- 6th infusion of factor 8th
- Administration of von Willebrand factor
- Avoid cryoprecipitate
Question 15. Root in the antrum.
Answer:
Root In antrum
Commonly Affected Teeth: Maxillary first molar
Causes Of Root In Antrum:
- Improper grip over force
- Excessive application of forces
- A sudden movement of the patient
- Slippage of root
Pathogenesis Of Root In Antrum:
- The root piece slips as an orange seed
- An attempt to remove it leads to deep penetration of it
Treatment Of Root In Antrum:
- If it small piece, it exhales out
- If a large root piece is fractured, it leads to oro antral fistula
Management Caldwell Luc Operation:
- Procedure:
- Anesthetized
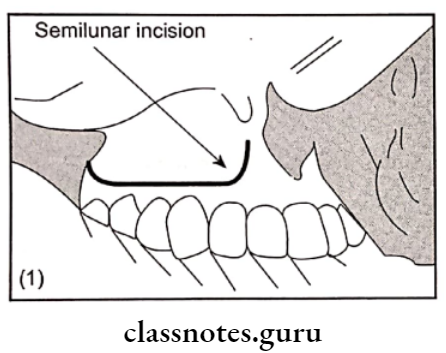
- The semilunar incision is given in the mesiobuccal fold in the canine region
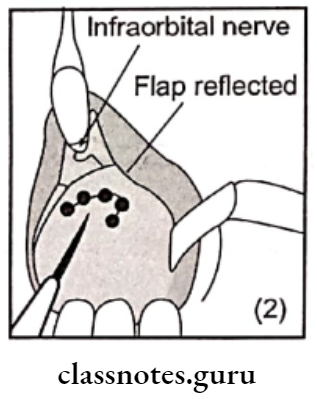
- Reflection of flap
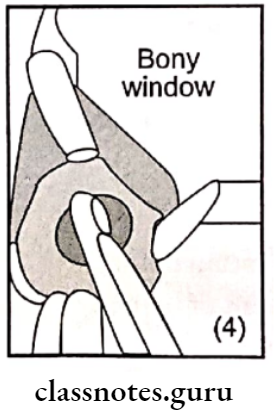
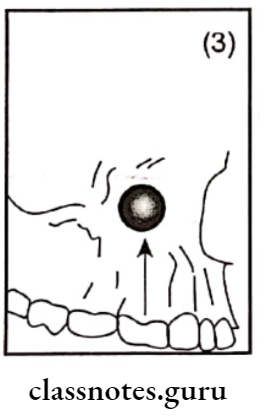
- Creation of window
- Removal of sinus lining for biopsy
- Antrostomy
- Packing the sinus cavity through ribbon gauze pregnant in benzoin
- Smoothening of bony margins
- Replace the flap
- Suturing
Question 16. Analgesics.
Or
Opioid Analgesics
Answer:
Analgesics
- Analgesics is a drug which relieves pain without loss of consciousness
- Analgesics only affords symptomatic relief from pain without affecting the cause
Classes of Analgesics:
1. Opioids Example: Morphine:
- Opioids is abused
Actions Of Opioids:
- Analgesic
- Sedative
- Hypnotic
- Respiratory depressant
- Depresses cough center
- Emetic
- Miotic
- Stimulates vagal center
- Produces convulsants
Contraindications Of Opioids:
- COPD
- Branchial asthma
- Head injuries
- Hypovolaemic shock
2. Nonopioids Example: Aspirin:
Actions Of Nonopioids:
- Analgesia
- Antipyretic
- Anti-inflammatory
- Antiplatelet action
Uses Of Nonopioids:
- Toothache
- Arthralgia
- Fever
- Anti-inflammatory
- Osteoarthritis
- Post myocardial infarction
- Locally as a keratolytic agent
Question 17. Hemophilia.
Answer:
Hemophilia
Bleeding disorder occurring due to X-linked genetic disorder
Types Of Hemophilia:
- Hemophilia A
- Hemophilia B
- Von Willebrand disease
Clinical Features Of Hemophilia :
- Easy bruising
- Prolonged bleeding
- Soft tissue hemartoma
- Epistaxis
- Gastric hemorrhage Recurrent hemarthrosis
- Joint deformity
- Spontaneous hematuria
- Intracranial hemorrhage
Oral Manifestation Of Hemophilia:
- Bleeding gums
- Bleeding followed by nerve block
- Recurrent subcutaneous hematoma
- High caries index
- Oropharyngeal bleeding
Lab Investigation Of Hemophilia:
- Prolonged clotting time
- Prothrombin consumption decreased
- Thromboplastin generation increased
Complications Of Hemophilia:
- Airway obstruction
- Intestinal obstruction
- Intracranial bleeding
- Paralysis
- Death
Treatment Of Hemophilia:
- Immediate transfusion of factor 8 or 9 Transfusion of packed RBC
- Control bleeding with the help of fibrin foam
- Analgesics & corticosteroids
- Joint immobilization
- Local chilling
- Use of 4 desmopressin
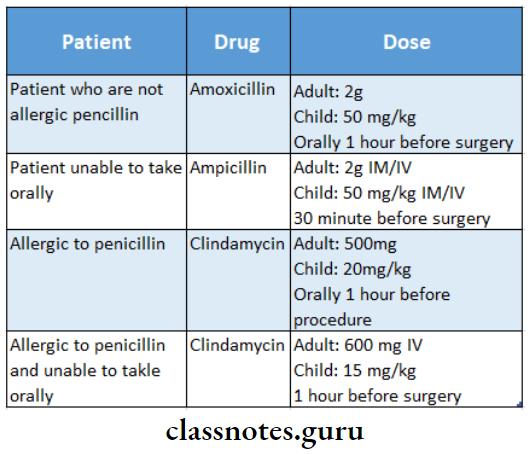
Question 18. Antibiotic prophylactic.
Or
OpharyngealEndocarditis prophylaxis.
Answer:
Prophylaxis Required For:
- Dental extraction
- Periodontal surgeries
- Endodontic procedures beyond the apex
- Dental implant placement
- Subgingival placement
- Intraligamentary injections
Prophylactic Not Required For:
- Restorative dentistry
- Non intraligamentary injection
- Placement of rubber dam
- Placement of removable appliances
- Suture removal
- Making impressions
- Shedding of primary teeth
Question 19. Blood groups.
Answer:
Major Blood Groups:
- ABO system
- Rh system
- ABO system
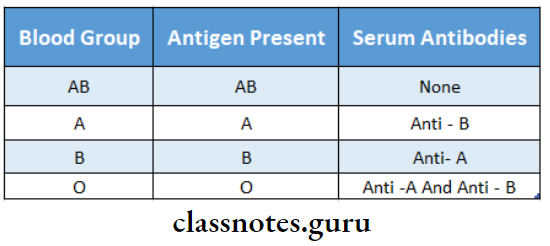
Rhesus System:
- This blood group contains the D antigen
- Individuals who are D-positive are considered Rh-positive
- Individuals with D negative are Rh-negative
Minor Blood Groups:
- Lewis system
- P system
- I system
- MNS system
- Kell & Duffy system
- Luthern system
Question 20. Tooth Transplantation.
Answer:
Tooth Transplantation
Tooth Transplantation is the removal of a tooth from one socket & transplanting into another socket
The Technique Of Tooth Transplantation:
- Asepsis should be followed
- The socket of the transplanted site is curetted & irrigated with saline
- The tooth is placed gently in the socket with light finger pressure
- Check with a radiograph
- Placement of splint
- Prescribe analgesic & antibiotic
- Check after 24 hours
Question 21. Post-injection hematoma.
Answer:
Post-Injection Hematoma
- Injury to any blood vessel may result in the escape of blood into extravascular spaces resulting in a hematoma
- Occurs after inferior alveolar nerve block & posterior superior alveolar nerve block
Features Of Post Injection:
- Intraoral swelling, trismus after inferior alveolar nerve block
- Extraoral swelling After posterior superior alveolar nerve block
Management Of Post Injection:
- Immediate Management: Pressure application
- It resolves itself within 7 – 14 days
- Antibiotics for a large hematoma
- After 1-2 days of fomentation
Question 22. Shock-septic.
Answer:
Definition Of Shock-Septic:
When acute cardiovascular failure is superimposed on bacteremia, it is called septic shock
Clinical Features Of Shock-Septic:
- Fever
- Tachycardia
- Tachypnea
- Respiratory alkalosis
- Hypoxaemia
- Hypotension
- Oliguria
- Icterus
Pathogenesis Of Shock-Septic:
- Low cardiac filling
- Decreased vascular resistance
Results Of Shock-Septic:
- Hypovolaemia
- Myocardial depression
- Abnormal distribution of blood flow
Management Of Shock-Septic:
- Administration of oxygen
- Removal of the septic nidus
- Empirical antibiotics
- Vasoactive Drugs: Phenoxybenzamine
- Inotropic Agents: Dopamine
- Corticosteroids: Prednisolone15 mg/kg
- Mechanical ventilation
- Fluid replacement
Question 23. Anaerobic antimicrobial.
Answer:
Anaerobic Antimicrobial
- Metronidazole is the drug of choice
- Anaerobic Antimicrobial is nitromidazole deravitive
Mechanism Of Anaerobic Antimicrobial:
Micro-organism reduces its nitro group & converts it into a cytotoxic drug which damages DNA & inhibits protein synthesis
Uses Of Anaerobic Antimicrobial:
- Orodental infection
- AUG
- Periodontitis
- Pericoronitis
- Peptic ulcer
- Amoebiasis
- Liver abscess
Adverse Reactions Of Anaerobic Antimicrobial:
- Anorexia
- Metallic taste
- Headache, dizziness
- Glossitis
- Dryness of mouth
- Peripheral neuropathy
Contraindications Of Anaerobic Antimicrobial:
- Neurological disease
- Blood dyscrasias
- The first trimester of pregnancy
- Chronic alcoholism
- Dose: 200-400 mg TDS
Question 24. Diclofenac sodium.
Answer:
Diclofenac Sodium
- Diclofenac Sodium is an aryl acetic acid derivative
- Diclofenac Sodium is an analgesic antipyretic & anti-inflammatory drug
Mechanism Of Diclofenac Sodium:
- Inhibits PG synthesis
- Short-lasting anti-platelet action
- Neutrophil chemotaxis & superoxide production at
- Inflammatory sites are reduced
Uses Of Diclofenac Sodium:
- Rheumatoid & osteoarthritis
- Toothache
- Bursitis
- Ankylosing spondylitis
- Dysmenorrhea
- Post-traumatic & post-operative inflammatory conditions
Adverse Reactions Of Diclofenac Sodium:
- Epigastric pain
- Headache
- Dizziness
- Rashes
- Dose: 50 mg TDS
Trade Name:
- Voveran
- Diclonac
- Movonac
Question 25. Penicillin.
Answer:
Penicillin
Lactum Antibiotic
Mechanism Of Penicillin:
- Inhibit cell wall synthesis
- Inhibit transpeptidase thus inhibiting the synthesis of peptidoglycan
Classification Of Penicillin:
- NaturalPenicillin G
- Semisynthetic
- Acid resistant – Penicillin 5
- Penicillin resistant Methicillin
- Aminopenicillin Ampicillin
- Antipseudomonal penicillin Carbenicillin
Uses Of Penicillin:
- Orodental infections
- Syphilis
- Gonorrhea
- Streptococcal infections
- Tetanus
- Prophylactic Gangrene
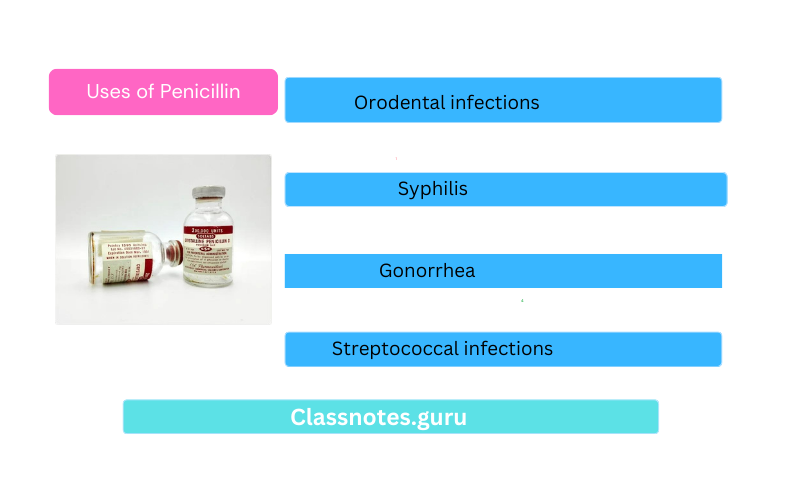
Adverse Reaction Of Penicillin:
- Hypersensitivity
- Anaphylaxis
- Local pain at the site of injection
- Suprainfection
- Jarish Herxheimer reaction
Question 26. CSF Rhinorrhoea.
Answer:
CSF Rhinorrhoea
CSF Rhinorrhoea is typically a high level of Lefort III fracture
Causes Of CSF Rhinorrhoea:
- Dislocation of nasal bone
- Disruption of cribriform plates
- Tear of durometer
- This leads to leakage of CSF
Etiology Of CSF Rhinorrhoea:
- Congenital encephalocele
- Acquired Traumatic
- Infection
- Iatrogenic
- Tumors
- Spontaneous Increased intracranial pressure
Sites Of CSF Rhinorrhoea:
- Cribiform plate of ethmoidal roof
- Sphenoidal sinus
- Frontal sinus
Clinical Features Of CSF Rhinorrhoea:
- Unilateral watery nasal discharge
- Headache
- Visual disturbance
- Salty taste
- Positional variation
- Inflammatory paranasal sinus discharge
Clinical Examination:
- Tram line effect on the face
- Clear fluid stream
- A halo sign is seen in blood fluids
- Glistening moist nasal mucosa
Diagnosis Of CSF Rhinorrhoea:
- Biochemical test
- Low protein
- High glucose
- Beta trans protein
- Intratracheal fluorescin
- Nasal endoscopy Imaging
Treatment Of CSF Rhinorrhoea:
- Conservative
- Bed rest
- Head elevation
- Laxatives
- Antitussives
- Subarachnoid drainage
- Surgical
- Composite graft
Complications Of CSF Rhinorrhoea:
- Pneumocephalus
- Tension cephalus
- Infection
- Intracranial hypertension
- Persistent & recurrent CSF leak
- Post-traumatic CSF cyst
Question 27. Aspirin.
Answer:
Aspirin
Salicylic acid derivative
Actions Of Aspirin:
- Analgesia
- Anti pyretic
- Anti-inflammatory
- Antiplatelet action
Adverse Reactions Of Aspirin :
- GIT upset
- Allergic reactions
- Hemolysis
- Nephrotoxicity
- Hepatotoxicity
- Reye’s syndrome
Uses Of Aspirin:
- Toothache
- Arthralgia
- Fever
- Anti-inflammatory
- Osteoarthritis
- Post myocardial infarction
- Locally as a keratolytic agent
Question 28. Healing of extraction wound.
Answer:
Immediate Reaction Of Extraction Wound:
- Coagulation of blood
- Entrapment of RBC into fibrin mesh
- Vasodilation & engorgement of blood vessels
- Mobilization of leukocytes
- Presence of areas of contraction of clot
First Week Of Extraction Wound:
- Growth of fibroblast into the wound
- Formation of granulation tissue
- The proliferation of epithelium at the periphery
- The osteoblastic activity of alveolar bone
- Organization of blood clot
Second Week Of Extraction Wound:
- Penetration of new capillaries into the center of the clot
- Degeneration of remnants of PDL
- Fraying of the bony socket
- Epithelium proliferation at the periphery
- Fragments of necrotic bone
Third Week Of Extraction Wound:
- Complete formation of granulation tissue
- Presence of young trabeculae Early bone formation
- Remodeling of cortical bone
Fourth Week Of Extraction Wound:
- Bone filling
- Healing of crest of the bone
Question 29. Minor oral surgeries in hemophilic & diabetic
Answer:
Hemophilic Patients:
- Laboratory Investigations
- Immediate transfusion of factor 8 or 8 Transfusion of packed RBC
- Control bleeding with the help of fibrin foam Analgesics & corticosteroids
- Joint immobilization
- Local chilling
- Use of 4 desmopressin
Diabetic Patients:
- Monitor blood & urine glucose
- Risks:
- Hyperglycemia
- Hypoglycemia
- Delayed wound healing
- Infection
Management:
- Check fasting sugar
- Advice from physician
- Normal meal before surgery
- Routine medication before treatment
- Prophylactic antibiotic to prevent infection
- Antibiotics are also prescribed after treatment
Question 30. Blood transfusion reactions.
Answer:
Blood Transfusion Reactions
- Simple pyrexial reactions
- Allergic reactions
- Sensitization to leukocytes & platelets
- Major incompatibility
- Hematuria
- Pain in loins
- Fever with chills
- Oliguria
- Transmission of diseases
- Thrombophlebitis
- Inflammation of superficial veins
- Tender cord-like vein
- Fever
- Congestive cardiac failure
- In chronic anemic patients
- DIC
- Disseminated intravascular coagulation
- Adult respiratory distress syndrome
Reactions Caused By Massive Transfusion:
- Acid-base imbalance
- Hyperkalaemia
- Citrate toxicity
- Hypothermia
- Failure of coagulation
Question 31. Squamous cell carcinoma of Lip.
Answer:
Clinical Features Of Lip:
- Age/sex: Elderly males
- Nonhealing ulcer
- Edge is everted
- Induration present
- The floor is covered with slough
- Bleeding spots present
- Fix to underlying subcutaneous tissue
- Cervical lymphadenopathy
Differential Diagnosis Of Lip:
- Keratoacanthoma
- Ectopic salivary gland tumor
- Pyogenic granuloma
- Leukoplakia
Treatment Of Lip:
- Surgery
- Abbe flap
- Estlander flap
- Radiotherapy
- Dose: 4000-6000 cGy units
Question 32. Management of patient on long-term steroid therapy.
Answer:
Management Of Patient On Long-Term Steroid Therapy
- Prevention of infection by encouraging the patient to maintain good oral hygiene
- Advice frequent dental visit
- Aggressive treatment for acute infections
- Consult the patient’s physician if adrenal suppression is suspected
Mild Surgeries Of Steroid Therapy:
- Double the dose of steroids on the day of treatment
- Return to normal dose on the next day
Moderate Surgeries Of Steroid Therapy:
- 100 mg of Hydrocortisone before the procedure
- Half the dose on the following day
Severe Surgeries Of Steroid Therapy:
- 200 mg Hydrocortisone
- Half the dose on the following day
Question 33. Ibuprofen.
Answer:
Ibuprofen
Propionic acid derivative
Mechanism Of Ibuprufen:
- Inhibit PG synthesis
- Inhibit platelet aggregation
- Prolongs bleeding time
Uses Of Ibuprofen:
- Analgesia
- Tooth extraction
- Fractures
- Postoperative swelling
- Dose: 400-600 mg TDS
Trade Name Ibuprufen:
- Brufen
- Ibugesic
Question 34. Hemostatic agents.
Answer:
Mechanical Of Agents:
- Pressure pressure through gauze piece
- Use of hemostat
- Sutures & ligation
- Embolization of the vessels
- Through steel coils
- Alcohol foam
- Gel foam
- Silicon spheres
Thermal Of Agents:
- Cautery: Transmission of heat by conduction of tissues
- Electrosurgery: Through induction from electric current
- Cryosurgery: Temperature used (-20°C) (180°C)
- Argon Beam Coagulator: Flow of argon gas is used
- Laser
Chemical Agents:
- Local Agents:
- Astringents
- Bone wax
- Thrombin
- Gel foam Oxycel
- Surgicel
- Systemic Agents:
- Whole blood transfusion
- Platelet-rich plasma
- Fresh frozen plasma
- Cryoprecipitate
Question 35. Nerve supply to maxillary teeth.
Answer:
Nerve supply To Maxillary Teeth
- Incisors central, lateralAnterior superior alveolar nerve
- Canine Anterior superior alveolar nerve
- Premolar – Middle superior alveolar nerve
- Molars Posterior superior alveolar nerve
Question 36. Cancrum oris.
Answer:
Cancrum Oris
- Cancrum Oris is an extensive ulcerative disease of cheek mucosa occurring in malnourished children
- Precipitating Factors:
- Malnutrition
- Major diseases like diphtheria
- Vincent’s organism
Treatment Or Cancrum Oris:
- Ryle’s tube-feeding
- Improve the nutrition
- Antibiotics: Metronidazole-400 mg TID for 7-10 days
- Reconstructive surgery
Complications Of Cancrum Oris:
- Fibrosis
- Septicaemia
- Restricted jaw movement
- Death
Question 37. Principles of antibiotic therapy.
Answer:
Principles Of Antibiotic Therapy Can Be Divided Into The Following Groups:
- Clinical evaluation and diagnosis for antimicrobial-biological etiology
- Antibiotics specific for particular organisms should be used
- Study of Culture and Sensitivity
- Causative organisms are cultured and tested against a range of antibiotics for maximum sensitivity
- Age of the patient
- Certain drugs like chloramphenicol may cause serious toxic effects in infants
- Pregnancy and neonatal period
- Many antibiotics cross the placental barrier
- They should be used only when extremely necessary
- Severity of disease
- Antimicrobial therapy should be considered for patients with established orofacial infections
- Initially, a bacteriostatic agent should be used
- Nature of the drug
- Preferable to use bacteriocidal drug
- Possibility of drug resistance
- Alternative drugs should be used in such cases
- History of previous allergic reaction
- Alternative drugs should be used in such cases
- Risk of toxicity of the drug
- Patients should be informed about the side effects of the drug
- Cost
- Proper selection of suitable drugs is done
- Use of narrow-spectrum antibiotic
- It minimizes the risk of superinfection
Miscellaneous Short Question And Answers
Question 1. Idiosyncracy.
Answer:
Idiosyncrasy
- Idiosyncrasy is genetically determined abnormal reaction
- Example: Patients with G6PD deficiency
- In some cases, a person may be sensitive to low doses
- While in some patients even high doses don’t produce any reactions
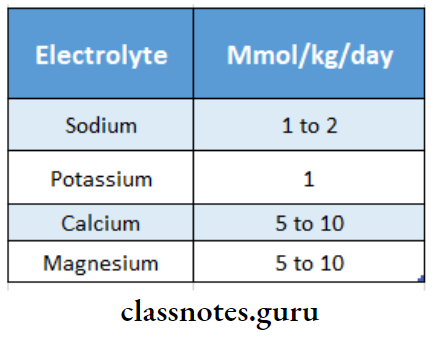
Question 2. Fluid & electrolytes.
Answer:
Fluid & Electrolytes
- Body consists of 50-70% liquids & 30-50% solids by weight
- Liquid varies with age, sex & body habits Infants > adults 80% Vs 60%
- Males > Females 60% Vs 50%
- Thin > Obese
- Out of the total liquid
- Intracellular water 40%
- Extracellular portion 20%
- 5% plasma
- 15% interstitial fluid
Fluid & Electrolytes Water Regulation:
- Water ingested by regulation of thirst center
- Water excreted by regulation of ADH
Fluid & Electrolytes Replacement:
- Fluid requirement during starvation 2ml/kg/hour
- Maintenance requirement 2mg/kg/hour of surgery
- Minor surgery 4ml/kg/hour
- Moderate 6ml/kg/hour
- Severe -8ml/kg/hour
- Blood loss is replaced by blood transfusion
Fluid & Electrolytes Electrolytes:
Question 3. Neurogenic shock.
Answer:
Pathophysiology Of Neurogenic Shock :
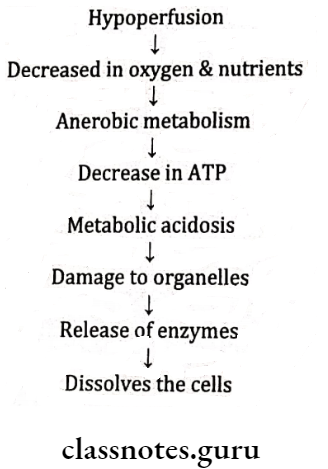
Damage To Organs:
- Increase in myocardial contractibility
Question 4 . Hyperventilation.
Answer:
Clinical Features Of Hyperventilation:
- Age: 15-40 years
- Sex common in females
Features Of Hyperventilation:
- Anniery
- Paim
- Increased depth of respiration
- Excessive exchange of gases in lungs
- Decreased level of carbon dioxide
- Increased pH
- Decreased cerebral blood flow – Hypotension
Management Of Hyperventilation:
- Stop the dental procedure
- Make the patient comfortable
- Caver the mouth & nose with a paper bag
- Ask the patient to breathe
Question 5. Carcinoma in situ.
Answer:
Carcinoma In Situ
Carcinoma In Situ is the most severe stage of epithelial dysplasia, which involves the entire thickness of the epithelium with the basement membrane intact
Clinical Features Of Carcinoma:
- Age: Elderly patients
- Sex: Common in males
Presentation Of Carcinoma:
- Appears as white plaques or ulcerated areas
- Site: The floor of the mouth, tongue, lip, etc
- Appears as leukoplakia or erythroplakia
Treatment Of Carcinoma:
- Surgery
- Radiotherapy
- Electrocautery
Question 6. Classification of NSAID/NSAIDs.
Answer:
Nonsteroidal anti-inflammatory drugs are aspirin-type or non-opioid analgesics
Classification Of NSAID:
- Nonselective COX inhibitors
- Salicylic acid derivatives
- Aspirin, sodium salicylate, diflunisal
- Para-aminophenol derivatives
- Paracetamol
- Pyrazolone derivative
- Phenylbutazone, azapropazone
- Indole acetic acid derivative
- Indomethacin. etodolac
- Arylacetic acid derivative
- Diclofenac, aciclofenac, ketorolac
- Propionic acid derivative
- Ibuprofen, carprofen, naproxen, ketoprofen
- Anthranilic acids
- Flufenamic acid, mefanamic acid
- Oxicams
- Piroxicam tenoxicam
- Alkanones
- Nabumetone
- Salicylic acid derivatives
- Selective COX-2 inhibitors
- Nimesulide, celecoxib, rofecoxib
Mechanism Of Action:
- NSAIDs inhibit prostaglandin synthesis by inhibiting the enzyme cyclo-oxygenase
Question 7. Submucous fibrosis.
Answer:
Submucous Fibrosis
Submucous Fibrosis is a pre-cancerous condition
Submucous Fibrosis is characterized by juxta epithelial inflammatory reaction in the oral mucosa followed by a fibro elastic transformation of the lamina propria leading to mucosal atrophy, rigidity & trismus
Etiology Of Fibrosis:
- Consumption of red chilies
- Consumption of areca nuts Nutritional deficiencies Immunological factors
- Genetic factors
Features Of Fibrosis:
- Burning sensation
- Difficulty in mastication Referred pain in the ear
- Depapillation of tongue
- Restricted movement of floor of mouth
- Shrunken uvula
- Fibrous bands
- Restricted mouth opening
- Stiffness of buccal mucosa
Management Of Fibrosis:
- Quit the habit
- Antioxidant Oxyace1 capsule/ day
- Multivitamin therapy
- Sterold Betnovate 0.12%
- Tumeric application
- Intralesional injection of Hyaluronidase 1500 U
- Physiotherapy
- Splitting of fibrous bands
- Laser
Question 8. Cherubism.
Answer:
Clinical Features Of Cherubism:
- Painless, bilateral swelling of the mandible
- Maxillary swelling
- Pressure on orbit
- Heavenward look
- Increased cheek fullness
- Expansion & widening of the alveolar ridge.
- Flattening of palatal vault
- Chronic lymphadenopathy
- Premature exfoliation of deciduous
- Delayed eruption of permanent
- Hypodontia of teeth
- Difficulty in mastication, speech, swallowing
- Associated with Noonan syndrome
- Affects young children
Treatment Of Cherubism:
- Self-limiting disease
Question 9. Diazepam.
Answer:
Diazepam
Diazepam is benzodiazepine
Actions Of Diazepam:
- Sedation & hypnosis Reduction in anxiety
- Muscle relaxant
- Anticonvulsant
- Amnesia
Mechanism Of Diazepam:
- Binds to GABA receptor
- Increases frequency of chloride channel opening Increases flow of chlorine
- Hyperpolarization
Adverse Reactions Of Diazepam:
- Drowsiness
- Blurred vision.
- Amnesia
- Lethargy
- Ataxia
- Tolerance & dependence
Uses Of Diazepam:
- Insomnia
- Anxiety
- Anticonvulsants
- Muscle relaxant
- Pre-anesthetic medicament
- During alcohol withdrawal
Question 10. Dead space management.
Answer:
Dead Space Management
Dead space is a space left in the body as a result of a surgical procedure
Management Of Dead Space:
- Dead Space Management depends on size, location, and cause
- Treatment options are
- No treatment
- External bandage compression
- Involves the application of mildly compressive bandages to compress
- Suture closure
- Can avoid post-surgical care and overall cost factors associated with the use of surgical drains
- Use of drainage systems
- Protects wounds
- Penrose drains are used to control small to moderate-sized areas of dead space
- Normally used to manage dead space for 3-5 days
- Aspiration
- Hypodermic needle aspiration may be used alone or in combination
Question 11. Enbloc resection.
Answer:
Enbloc Resection
- Dead Space Management is the resection of a large bulky tumor virtually without dissection surgery
- Dead Space Management is used in certain cancers to remove
- Primary lesion
- Contagious draining lymph nodes
Question 12. Papilloma.
Answer:
Papilloma
- Papilloma is a common benign neoplasm of the oral cavity arising from epithelial tissue
- Papilloma is characterized by exophytic growth with a typical cauliflower-like appearance
Clinical Features Of Papilloma:
- Age- Third, fourth, and fifth decade of life Sex-both sexes are equally affected
- Site involved
- Tongue
- Lips
- Buccal mucosa
- Gingiva
- Hard and soft palate
- Present as slow growth, exophytic, soft, pedunculated, painless, nodular growth with a cauliflower-like appearance
- Have numerous finger-like projections over the surface
- It appears as ovoid swelling with a corrugated surface
- Size- a few mm to 1 cm in diameter
- The base of the lesion may be pedunculated or sessile
- Color-white in color
- Surface- highly keratinized
- Superficial ulceration and secondary infection occur
- Rarely papilloma grows inward
Question 13. Eburnation.
Answer:
Eburnation
- Eburnation describes a degenerative process of bone commonly found in patients with osteoarthritis or non-union of fractures
- It is an ivory-like reaction of bone occurring at the site of cartilage erosion
- Osteoarthritis is a degenerative disease of the joints characterized largely by central loss of cartilage and compensatory peripheral bone formation
- Over time, as the cartilage wears away and subchondral bone is revealed
- Eburnation describes the bony sclerosis that occurs in the areas of cartilage loss
Question 14. Nutrition for post-surgical patients.
Answer:
Nutrition For Post-Surgical Patients
Nutrition requirements for post-surgical patients increase than normal requirements
- Calorie:
- Increases to 30-40 kcal/kg
- Patients on ventilators usually require fewer calories- 20-25 kcal/kg
- Protein:
- Increases to 1-1.8 grams/kg
- Fluids:
- Start clear liquids when signs of bowel function return
- Clear liquids are intended for short-term use due to inadequacy
- Vitamin Supplements:
- Vitamin supplements promote healing Avoid long-term supplements due to the high risk of toxicity
Minerals Of Post-Surgical Patients:
- Zinc loss occurs due to large wounds, chest tubes, and wound drains
- Prolonged zinc supplementation interferes with copper absorption
