Disorders Of White Blood Cells Important Notes
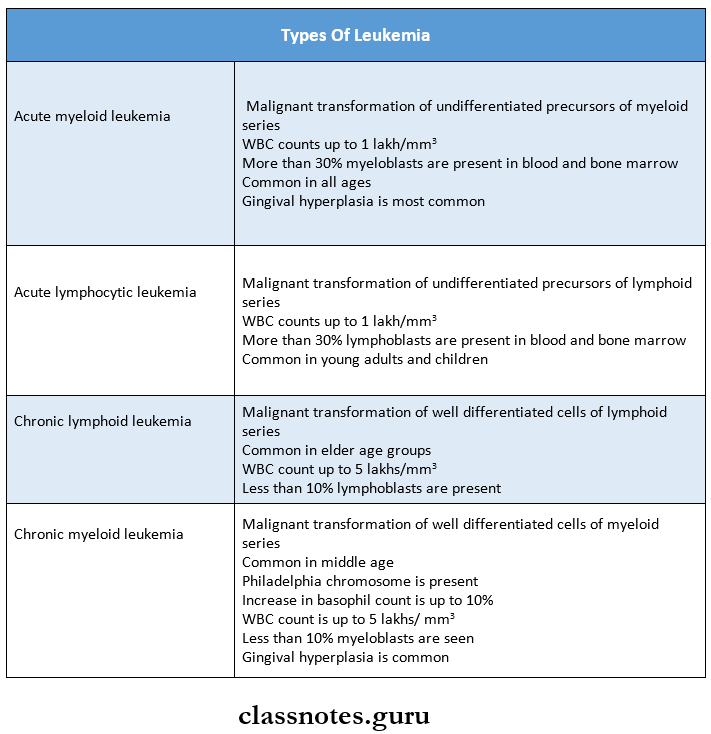
1. Types of leukemia
2. Syndromes associated with leukemia
- Down’s syndrome
- Bloom’s syndrome
- Klinefilter’s syndrome
- Wiskott-Aldrictis syndrome
- Fanconi’s anemia
3. Infectious mononucleosis or glandular fever
- Caused by Epstein Barr virus
- Characterized by atypical leukocytes consisting of
- Oval or horseshoe nuclei
- Irregular nuclear chromatin
- Basophilic foamy or vacuolated cytoplasm
Read And Learn More: Pathology Question And Answers
- Diagnostic tests
- Monospot test
- Paul Bunnel test
- The normal titer of agglutinin and hemolysin in human blood against sheep blood cells does not exceed 1:8
- In a positive Paul Bunnel test, the titer may rise to 1:4096
4. Agranulocytosis
- Mostly occurs due to the ingestion of drugs like
- Amidopyrine
- Barbiturates
- Chloramphenicol
- Quinine
- Sulfonamides
- Features
- Presence of infection in the oral cavity, GIT, genitourinary tract, respiratory tract, and skin
- Oral manifestation
- Necrotizing ulcerations of the oral mucosa, pharynx, tonsils
- Rapid destruction of supporting tissues of the teeth
5. Cyclic neutropenia
- It is characterized by periodic cyclic diminution of leukocytes
- Cycle commonly occurs at every 3 weeks
- Loss of alveolar bone around the teeth is an important oral manifestation
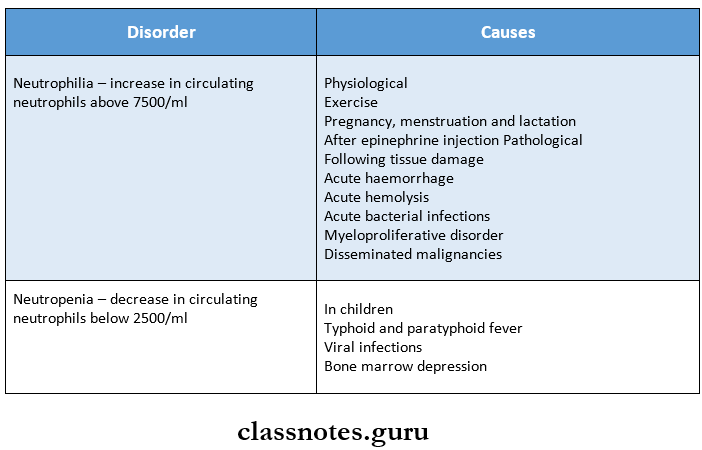
6. Disorders of neutrophil count
7. Leukaemoid reactions
- It is defined as a reactive excessive leucocytosis in the peripheral blood resembling that of leukemia
- It may be myeloid or lymphoid
- The myeloid type is a more common form
- Myeloid leukemoid reactions are seen in
- Infections like staphylococcal pneumonia, TB, meningitis, diphtheria, sepsis, endocarditis
- Intoxication
- Malignant diseases like multiple myeloma
- Severe hemorrhage and hemolysis
- Lymphoid leukemoid reaction are seen in
- Infections like infectious mononucleosis, cytomegalovirus infection, pertussis
- Malignant diseases rarely produce it
8. Most commonly affected bones in multiple myeloma are:
- Skull
- Spine
- Ribs
- Pelvis
Disorders Of White Blood Cells Long Essays
Question 1. Classify leukemia. Describe the clinical picture, blood, and bone marrow findings in acute leukemia.
Answer:
Leukemia Classification:
1. Based on cell types predominantly involved.
- Myeloid
- Lymphoid.
2. Based on the natural history of the disease:
- Acute
- Chronic.
WHO classification of myeloid neoplasm:
1. Myeloproliferative Diseases:
- Chronic myeloid leukaemia (CML], {Ph chromo¬some t(9;22) (q34;ll), BCR/ABL-positive}
- Chronic neutrophilic leukemia
- Chronic eosinophilic leukemia/ hypereosinophilic syndrome
- Chronic idiopathic myelofibrosis
- Polycythaemia vera (PV]
- Essential thrombocythaemia (ET)
- Chronic myeloproliferative disease, unclassifiable
2. Myelodysplastic/Myeloproliferative Diseases: Chronic myelomonocytic leukemia (CMML)
3. Myelodysplastic Syndrome (MDS):
- Refractory anemia (RA)
- Refractory anemia with ring sideroblasts (RARS)
- Refractory cytopenia with multilineage dysplasia (RCMD)
- RCMD with ringed sideroblasts (RCMD-RS)
- Refractory anemia with excess blasts [RAEB-1)
- RAEB-2
- Myelodysplastic syndrome unclassified (MDS-U)
- MDS with isolated del 5q
4. Acute Myeloid Leukaemia (AML):
- AML with recurrent cytogenetic abnormalities
- AML with t(8;21)(q22;q22)
- AML with abnormal bone marrow eosinophils {inv(16][pl3q22]}
- Acute promyelocytic leukaemia {tC15;17](q22;ql2)}
- AML with llq23 abnormalities (MLL)
- AML with multilineage dysplasia
- With prior MDS
- Without prior MDS
- AML and MDS, therapy-related
- Alkylating agent-related
- Topoisomerase type 2 inhibitor-related
- Other types
- AML, not otherwise categorized
- AML, minimally differentiated
- AML without maturation
- AML with maturation
- Acute myelomonocytic leukemia (AMML)
- Acute monoblastic and monocytic leukemia
- Acute erythroid leukemia
- Acute megakaryocytic leukemia
- Acute basophilic leukemia
- Acute panmyelosis with myelofibrosis
- Myeloid sarcoma
5. Acute Biphenotypic Leukaemia
Acute Leukemia: It is a leukemia characterized by predominant undifferentiated leucocytes precursors
Acute Leukemia Clinical Features:
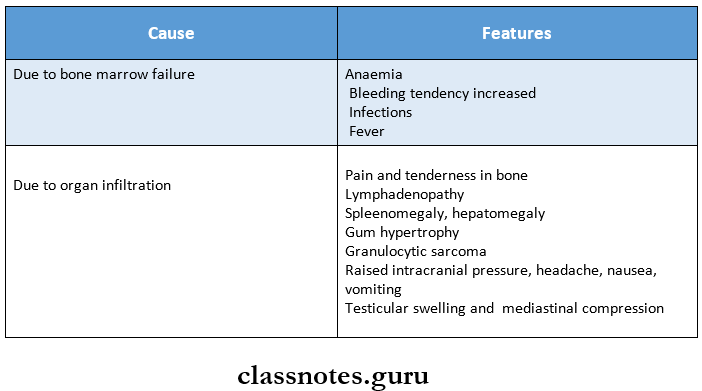
Acute Leukemia Blood Picture:
- Moderate reticulocytosis
- Normochromic anemia
- Increased platelet count
- WBCs count is more than 100000 per microlitre
Acute Leukemia Bone Marrow Examination:
- Cellularity- Bone marrow is hypercellular
- It shows predominantly myeloblasts and premyelo¬cytes
- Leukemic cells are demonstrated by Romanowsky stains
- Erythropoiesis shows
- Reduced erythropoietic cells
- Dyserythropoiesis,
- Megaloblastic features
- Ring sideroblasts
- Megakaryocytes
Question 2. Define leukemia. Describe the etiology, clinical features, blood, and bone marrow picture of chronic myeloid leukemia.
Answer:
Leukemia: leukemia are a group of disorders arising from the malignant transformation of hematopoietic cells leading to an increased number of white blood cells in blood and/or bone marrow.
Chronic myeloid leukemia:
Chronic myeloid leukemia Etiology: It is a myeloproliferative disorder.
- Occurs as a result of the malignant transformation of plea- potent stem cells leading to the accumulation of a large number of immature leukocytes in the blood.
- Radiation exposure and genetic factors have been implicated in the development of CML
Chronic myeloid leukemia Clinical features:
- Onset is usually slow, initial symptoms are often non-specific example: weakness, pallor dyspnoea, and tachycardia.
- Symptoms due to hypermetabolism such as weight loss, anorexia, and night sweats.
- Splenomegaly is almost always present and is frequently massive. In some patients, it may be associated with acute pain due to splenic infarction.
- Bleeding tendencies such as bruising, epistaxis, menorrhagia, and hematomas may occur.
- Visual disturbance, neurologic manifestations.
- Juvenile CML is more often associated with lymph node enlargement than splenomegaly.
Peripheral blood picture of CML:
- Leucocyte count is elevated often > 1,00,000 cells/pl.
- Circulating cells are predominantly neutrophils, metamyelocytes, and myelocytes but basophils and eosinophils are also prominent.
- A typical finding is an increased number of platelets (thrombocytosis).
- Anaemia is usually of moderate degree and is normocytic, normochromic in type. Normablasts may be present occasionally.
- A small portion of myeloblasts usually < 5% are seen.
Bone marrow examination:
- Cellularity – Hyper cellular with total/partial re-placement of fat spaces by proliferating myeloid cells.
- Myeloid cells -Myeloblasts are only slightly increased.
- Erythropoiesis -Normoblasts but there is a reduction in erythropoietic cells.
- Megakaryocytes – Conspicuous but are usually smaller in size than normal.
- Increase in number of phagocytes.
Disorders Of White Blood Cells Short Essays
Question 1. Leukocytosis
Answer:
Leukocytosis is an increase in the number of white cells & is common in a variety of reactive inflammatory states caused by microbial and non-microbial stimuli.
Leukocytosis Causes: Leukocytosisare relatively non-specific and can be classified on the basis of particular white cell series affected as follows:
Causes of Leukocytosis: Leukocytosis are relatively non-specific and can be classified on the basis of particular white cells series affected as follows:
1. Neutrophilic leucocytosis.
- Cute bacterial infections especially those caused by pyogenic organisms.
- Sterile inflammation caused by tissue necrosis (myocardial infarction, burns)
2. Eosinophylic leucocytosis (eosinophilia)
- Allergic disorders such as asthma, hay fever
- Allergic skin diseases, for example., pemphigus, dermatitis herpetiform.
- Parasitic infestations
- Drug reactions
- Certain malignancies, for example., Hodgkin’s disease and some non-hodking’s lymphomas.
- Collagen vascular disorders and some vasculitis.
3. Basophilic leucocytosis (basophilia): Rare often indicates CML.
4. Monocytosis.
- Chronic infections, ie.g., tuberculosis
- Bacterial endocarditis
- Rickettsiosis and malaria
- Collagen vascular diseases, for example., systemic lupus erythematosus (SLE)
- Inflammatory bowel diseases, for example., ulcerative coli¬tis
5. Lymphocytosis: Usually accompanies monocytosis in many disorders associated with it.
- Chronic immunologic stimulation, for example., tuberculo¬sis, brucellosis and
- Viral infections, for example., hepatitis A, cytomegalovirus, Epstein-Barr virus, and bordetella pertussis infections.
Question 2. Causes of neutrophilic leukocytosis
Answer:
- Acute bacterial infections especially those caused by pyogenic organisms.
- Sterile inflammation caused by tissue necrosis (myocardial infarction, burns)
Question 3. Agranulocytosis
Answer:
- The term agranulocytosis is used to describe a state of severe neutropenia.
- A reduction in the number of granulocytes in the blood is known as neutropenia.
Agranulocytosis Causes: Neutropenia can be caused by the following reasons.
- Drug-induced: Anti-cancer, antibiotics, anticonvulsants, antithyroid drugs
- Hematological disease: Aplastic anemia, acute leukemia, etc.
- Infections: Malaria, TB, typhoid,
- Autoimmune: Systemic lupus erythematosus
- Congenital: Cyclic neutropenia.
Agranulocytosis Clinical features:
- Initially patient develops malaise, chills, and fever, with subsequent marked weakness and fatiguability.
- Massive growth of microorganisms due to inability to produce leukocyte response.
- Infections are usually present as ulcerating, necrotizing lesions of the gingiva, the floor of the mouth, buccal mucosa, and other sites within the oral cavity known as agranulo¬cytic angina.
- Lymphadenopathy and hepatosplenomegaly may be present.
Agranulocytosis Treatment:
- Patients with neutropenia and fever must be sent to the hospital.
- In severe infections, neutrophil transfusion must be done.
- Broad-spectrum antibiotics and antifungal drugs are to be given.
Question 4. Leukemoid reaction
Answer:
- Leukaemoid reaction is defined as the reactive excessive leucocytosis in peripheral blood resembling that of leukemia in the subject who does not have leukemia.
- Leukaemoid reaction may be myeloid or lymphoid.
Myeloid leukemoid reaction:
- The majority of leukemoid reactions involve the granulocyte series.
- It may occur in infection, intoxication, malignant diseases, severe hemorrhages, and severe hemolysis.
Lymphoid leukemoid reaction: It is found in conditions such as infectious mononucleosis, whooping cough, chicken pox, measles, and tuberculosis.
Agranulocytosis Lab diagnosis:
- Leukocytosis
- Infective cases may show toxic granulation and Dohle bodies in the cytoplasm of neutrophils.
Question 5. Peripheral blood picture of acute lymphatic leukemia
Answer: Acute lymphatic leukemia shows
1. Anaemia:
- Normochromic
- Shows few nucleated cells
2. Thrombocytopenia: Platelet count decreases to 100000 cells
3. White blood cells:
- WBC count is variable
- It may exceed 100000 cells or may be less than that
- Leukocytes appear as blasts cells
Disorders Of White Blood Cells Short Questions And Answers
Question 1. Eosinophilia
Answer:
- An increase in the number of eosinophilic leukocytes is referred to as eosinophilia.
- The causes of eosinophilia are as follows:
- Allergic disorders: Bronchial asthma, urticarial, drug hypersensitivity
- Parasitic infestations: Trichinosis, echinococcosis, intestinal parasitism.
- Skin diseases: Pemphigus, dermatitis herpetiformis, erythema parasitism.
- Certain malignancies: Hodgkin’s diseases and some non-Hodgkin’s lymphomas.
- Pulmonary infiltration which eosinophilia syndrome
- Irradiation.
- Miscellaneous disorders: Sarcoidosis, rheumatoid arthritis, polyarteritisnodosa.
Question 2. Blood picture in chronic myeloid leukemia
Answer:
- Leucocyte count is elevated often > 1,00,000 cells/Bll.
- Circulating cells are predominantly neutrophils, metamyelocytes, and myelocytes but basophils and eosinophils are also prominent
- The typical finding is an increased number of platelets (thrombocytosis).
- Anaemia is usually of moderate degree and is normocytic, normochromic in type. Normablasts may be present occasionally.
- A small portion of myeloblasts usually < 5% are seen.
Question 3. Peripheral smear layer findings in acute leu¬kemia
Answer:
1. Anaemia:
- Always present generally severe, progressive, and normochromic.
- A moderate reticulocytosisupto 5% and a few nucleated red cells may be present.
2. Thrombocytopenia:
- Platelet count < 50,000/pl
- When the platelet count is below 20,000/01 serious spontaneous haemorrhagic episodes develop.
- Acute promyelocytic leukemia may be associated with a serious coagulation abnormality called dis-seminated intravascular coagulation.
3. White blood cells:
- In advanced cases, WBC > 1,00,000/pl
- The majority of leucocytes in the peripheral blood are blasts and there is often neutropenia due to mar¬row infiltration by leukemic cells.
Question 4. Burkitt’s lymphoma
Answer:
- Burkitt’s lymphoma is a rare type of non-Hodgkin’s lymphoma (NHL).
- Epstein-Barr virus (EBV) and HIV are associated with the development of Burkitt’s lymphoma.
- This is the most rapidly progressive tumor first described in African children.
- Most patients present with lymphadenopathy and abdominal mass.
- It has a tendency to metastasize to the CNS.
- Treatment should be initiated promptly with intensive chemotherapy. Prophylactic chemotherapy is also given. 70-80% of patients may be cured.
Question 5. Multiple myeloma
Answer: Multiple myeloma is a malignant disease arising from the neoplastic transformation of plasma cells of mono-clonal origin
Multiple Myeloma Clinical Features:
- Age- in older age
- Anaemia
- Bone pain
- Infections
- Pathological fractures
- Renal failure
- Spinal cord compression
Multiple Myeloma Investigations:
- Bence- Jones proteins in urine
- Reversal of serum albumin/globulin ratio
- Increase in total serum proteins
Multiple Myeloma Treatment:
- Radiotherapy
- Biphosphonates
- Autologous peripheral cell transplantation
- Administration of thalidomide and proteasome inhibi¬tors
- Chemotherapy includes:
- Melphalan
- Cyclophosphamide
- Doxorubicin
- Dexamethasone
Diseases Of Cardiovascular Disorders Important Notes
1. Clinical patterns of angina
- Stable or typical angina
- Prinzmetal’s variant angina
- Unstable or crescendo angina
2. Forms of Creatine phosphokinase
- CK-MM-Derived from skeletal muscle
- CK-BB-Derived from the brain and lungs
- CK-MB-Derived from cardiac muscle
3. TypesofischaemicheartdiseaseJHD
- Stable angina
- Unstable angina
- Chronic IHD
- Myocardial infarction
- Sudden ischaemic death
Diseases Of Cardiovascular Disorders Short Question And Answers
Question 1. Hyperlipidemia
Answer:
- Hyperlipidaemia is a major risk factor for atherosclerosis
- It occurs due to
- Diabetes mellitus
- Myxoedema
- Nephritic syndrome
- Von Gierke’s disease
- Xanthomatosis
- Familial hypercholesterolemia
- Dietary regulation and administration of cholesterol-lowering drugs have beneficial effects on reducing the risk of ischaemic heart diseases
Question 2. Atheromatous plaques
Answer: A fully developed atherosclerotic lesion is called atheromatous plaque
Atheromatous plaques Appearance:
1. Gross appearance
- Appear as white to the yellowish-white lesion
- Size-1-2 cm in diameter
- Appears raised on the surface
2. Cut surface
- Shows luminal surface as a firm, white fibrous cap
- The central core is composed of yellow to yellow-white soft material called atheroma
3. Microscopic
- The fibrous cap is covered by endothelium
- It is composed of smooth muscles, dense connective tissue, and extracellular matrix
- The cellular area contains macrophages, foam cells, lymphocytes and smooth muscle cells
- The deeper central soft core consists of extracellular lipid material, cholesterol cleft, Fibrin, neurotic debris, and lipid-laden foam cells
