Diseases Of The Nervous System Long Essays
Question 1. Describe the etiology, clinical features, and localization of infra-nuclear facial nerve palsy.
(or)
Describe the etiology, clinical features, and management of facial palsy
Answer:
Facial Palsy
- Idiopathic paralysis of the facial nerve of sudden onset
Etiology: 5 Hypothesis:
- Rheumatic
- Cold
- Ischaemia
- Immunological
- Viral
Facial Palsy Clinical Features:
- Pain in post auricular region
- Sudden onset
- Unilateral loss of function
- Loss of facial expression
- Absence of wrinkling
- Inability to close the eye “ Watering of an eye “
- Inability to blow the cheek
- Obliteration of nasolabial fold
- Loss of taste sensation
- Hyperacusis
- Slurring of speech
Diseases of the nervous system long essays
Facial Palsy Management:
- Physiotherapy
- Facial exercises
- Massaging
- Electrical stimulation a Protection for the eye
- Covering of eye with bandage
- Medical management
- Prednisolone 60-80 mg per day
- 3 tablets for 1st 4 days
- 2 tablets for 2nd 4 days
- 1 tablet for 3rd 4 days
- Surgical treatment
- Nerve decompression
- Nerve grafting
- Medical management
Question 2. Classify epilepsy. Describe clinical features, diagnosis, and management of grand mal epilepsy.
Answer:
Epilepsy:
- Epilepsy is a group of disorders of cerebral functions characterized by chronic, recurrent, paroxysmal, nonsynchronous discharge of cerebral neurons
Grand Mal Epilepsy Classification:
- Partial or focal seizures
- Simple partial seizures
- Motor
- Sensory
- Visual
- Versive
- Psychomotor
- Complex partial seizures
- Temporal lobe
- Frontal lobe
- Secondary generalized partial seizures
- Simple partial seizures
- Primary generalized seizures
- Tonic-clonic
- Tonic
- Absence
- Akinetic
- Myoclonic
- Unclassified seizures
- Neonatal seizures
- Infantile spasms
Grand Mal Epilepsy:
- It is a common type of epilepsy
grand Mal Epilepsy Clinical Features:
- Phases of grand mal epilepsy
- Prodromal phase
- Symptoms are uneasiness or irritability
- It lasts for hours or days before an attack
- Aura
- Occurs when partial seizure becomes generalized
- Symptoms Are:
- Visual disturbances
- Hallucinations
- Nausea
- Epigastric discomfort
- Alteration in psychic functions
- The tonic and clonic phase
- Symptoms Are
- Tonic contraction of muscles
- Flexion of arms
- Extension of legs
- Cry due to spasm of respiratory muscles
- It lasts for 10-30 seconds
- Clonic phase causes:
- Violent jerking of face and limbs
- Biting of the tongue
- Incontinence of urine and feces
- It lasts for 1-5 minutes
- Symptoms Are
- Postictal phase
- Symptoms are:
- Deep unconsciousness with flaccid limbs
- Loss of corneal reflex
- Plantar extensor
- It lasts for a few minutes to several hours
Grand Mal Epilepsy Diagnosis:
- History of patient
- Clinical symptoms
- Blood test to assess metabolic disorders
- Brain imaging
Grand Mal Epilepsy Management:
- Elimination of causative agent
- Protection of patient
- Protected from a hot and sharp object
- Use of padded mouth gag
- Airway maintenance
- 4 administration of Diazepam 5-10 mg
- Long-term drug therapy
- Phenytoin sodium-200-400 mg daily
- Carbamazepine- 600-1800 mg daily in divided dose
- Sodium valproate- 0-2000 mg daily
- Phenobarbitone-60-180 mg daily
- Primidone-750-1500 mg daily in a divided dose
Long essay questions on neurological disorders
Question 3. Describe the etiology and clinical features of meningitis. How would you proceed to establish the diagnosis?
(or)
What are the causes of meningitis? Describe clinical features, complications, and treatment of pyogenic meningitis.
(or)
Discuss the etiology, clinical features, and investigations of pyogenic meningitis.
Answer:
Meningitis:
- Meningitis is defined as inflammation of the pia-arachnoid and the fluid contained in the space
Pyogenic Meningitis:
- Pyogenic Meningitis is bacterial meningitis
Etiology:
- Gram negative bacilli
- Group B streptococci
- Listeria monocytogenes
- H. influenzae
- Neisseria meningitidis
- Mycobacterium tuberculosis
Read And Learn More: General Medicine Question and Answers
pyogenic Meningitis Clinical Features:
- Classical triad- fever, headache, and neck rigidity
- Tachycardia, tachypnoea
- Convulsions in children
- Headache
- Blurring of vision
- Papilloedema
- Ecchymosis
- Associated lung, ear, and sinus infection
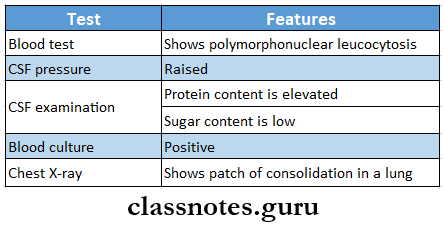
Pyogenic Meningitis Diagnosis
Pyogenic Meningitis Complications:
- Neurological deficiencies- hemiplegia, aphasia, blindness, deafness
- Mental deterioration
- Brain abscess
- Auditory impairment
- Subdural empyema
- Internal hydrocephalous
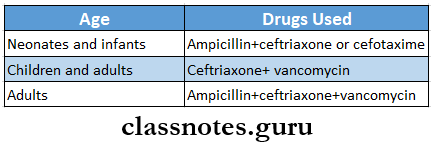
Pyogenic Meningitis Management:
- Ceftriaxone provides adequate coverage against infection
Central nervous system diseases long essays
Question 4. Discuss clinical features, complications, and management of tubercular meningitis.
Answer:
Tubercular Meningitis:
- Meningeal involvement by the mycobacterium tuberculosis causes tubercular meningitis
Tubercular Meningitis Clinical Features:
- Insidious in onset
- Headache
- Vomiting
- Low-grade fever
- Confusion
- Lassitude
- Visual disturbances
- Papilloedema
- Neck rigidity
- Cranial nerve palsies
- Hydrocephalus
Tubercular Meningitis Complications:
- Hydrocephalous
- Focal deficits
- Cranial nerve palsies
Tubercular Meningitis Management:
- General management
- Maintenance of nutrition
- Electrolyte balance
- Care of bowel and bladder
- Drug therapy
- Anti-tubercular drugs
- Injection of streptomycin 1 g IM daily
- Tab icons 600-900 mg/ day
- Tab ethambutol
- Steroids
- 20-30 mg prednisolone daily for a few weeks
- Anti-tubercular drugs
Question 5. Discuss etiopathogenesis, and clinical features of Parkinsonian disease. Outline the drugs used in its treatment.
Answer:
Parkinsonian Disease:
- Parkinsonian Disease is a syndrome consisting of akinesia and brake- nesia, rigidity, and tremors
Etiopathogenesis:
- There is a loss of pigmented cells in the substantianigra
- Dopamine levels in the striatum get depleted
Parkinsonian Clinical Features:
- Both sexes are equally affected
- Age- The fifth decade and later age group are affected
- Muscle ache
- Depression
- Slow activity
- Tremors
- Rigidity
- Hypokinesia
Parkinsonian Treatment:
- Anticholinergics
- Trihexyphenidyl
- Benzhexol
- Phenadrine
- Amantadine
- I-dopa- it is administered orally
- Dopamine receptor agonists
- Bromocriptine
- Lisuride
- Pergolide
- Selegiline
- Catechol-o-methyltransferase inhibitors
Long descriptive answers on nervous system diseases
Question 6. Discuss various factors you consider in evaluating a patient for general anesthesia
Answer:
Preoperative Evaluation For General Anaesthesia:
- The patient’s history is asked
- Physical evaluation of the patient
- General examination of a patient
- Weight and height
- Pulse rate
- Rhythm
- Volume
- Blood pressure is measured
- Temperature is measured
- Movements of eyeballs
- Feel the carotid arteries
- Systems examined
- Cardiovascular
- Respiratory
- Nervous system
- GIT
- Genitourinary tract
Question 7. Mention causes of cerebral embolism. What are its manifestations? Describe the principles of management.
Answer:
Cerebral Embolism:
- The emboli travel to the brain and cause cerebral embolism
general anesthesia Causes:
- Atherosclerosis
- High cholesterol level
- High blood pressure
General Anesthesia Clinical Features:
- Focal motor deficit
- Changes in sensorium
- Visual and sensory deficits
- Respiratory arrest
- Seizures
- Severe headache
General Anesthesia Treatment:
- Use of anticoagulants like heparin and warfarin
- Use of thrombolytics like streptokinase to dissolve the clot
Neurology long essay questions with answers
Question 8. Describe the pathogenesis, differential diagnosis, and management of coma
Answer:
COMA
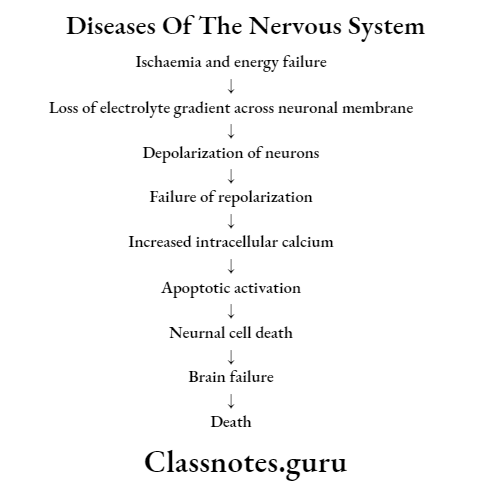
Pathogenesis:
Coma Differential Diagnosis:
- Cerebral anaemia
- Mechanical injury of the brain
- Convulsive attacks
- Cerebral vascular attacks
- Poisons
- Local infection of the brain and meninges
Coma Management:
- Treatment of the underlying cause
- Provide proper nutrition
- Maintain patient’s physical health
- Prevention of infection
- Physiotherapy to prevent bone, joint, and muscle deformities
Question 9. Describe the clinical features of intracerebral hemorrhage
Answer:
Clinical Features Of Intracerebral Haemorrhage:
- Hypertension
- Fever
- Cardiac arrhythmias
- Nuchal rigidity
- Subhyoid retinal haemorrhages
- Altered level of consciousness
- Focal neurological deficits
- Seizures
- Headache
- Nausea and vomiting
Nervous system pathology long answer questions
Question 9. Enumerate the causes of headaches. Discuss clinical features and management and prevention of migraine
Answer:
Causes Of Headache:
- Migraine headache
- Tension-type of headache
- Cluster headache
- Miscellaneous headache
- Traumatic headache
- Headache due to vascular causes- hematoma
- Headache due to nonvascular causes- due to increased pressure
- Headache due to substance abuse- alcohol
- Headache due to systemic infection
- Headache due to metabolic disorders
- Headache due to referred pain- from the ear, etc
- Cranial neuralgia- trigeminal neuralgia
- Unclassified headache
Migraine:
- Migraine is characterized by an episodic, hemicranial, or unilateral throbbing headache and is often associated with nausea, vomiting, and visual disturbances
Headache Clinical Features:
- Starts after puberty
- Common in females
- Headache occurs at regular intervals
- Each attack lasts for hours to days
- Prodromal symptoms
- Photophobia
- Visual disturbances
- Dysphagia
- Tinnitus
- Hemiparesis
- Hemianaesthesia
- Severe and throbbing headache
Long essay topics in nervous system disorders
Headache – Management:
- Removal of aggravating factors like alcohol, oral contraceptives, dietary factors
- Aspirin-600-900 mg/day.
- Paracetamol lg/day
- Anti-emetics like metoclopramide
- Ergotamine tartrate 0.5-1 mg sublingually orally or rectally
- Serotonin agonist sumatriptan 50-100 mg orally 2-3 times a day
Headache Prevention:
- Beta-blockers- propranolol- 80-120 mg/ day
- Pizotifen-1.5-3 mg at night
- Antidepressant- amitriptyline 50-100 mg at bedtime
- Flunarizine- 10 mg daily
- These all block 5-HT receptors
