Diseases Of Cardiovascular System Long Essays
Question 1. What are the signs and symptoms of cardiac failure? How do you treat it? (or) Define heart failure. Describe its pathophysiology, etiology, clinical features, and management.
Answer:
Heart Failure:
- It denotes a pathophysiologic state when the heart is not able to maintain its cardiac output to meet the demands of metabolizing tissues.
Pathophysiology:
- Preload.
- It is maintained by venous return that fills the ventricle during diastole and raises their pressure.
- Afterload.
- It is the resistance offered by blood vessels to stroke output.
- Myocardial contractility.
- It depends on the adrenergic nervous activity and the levels of circulating catecholamine.
- It causes the emptying of the chambers of the heart.
- Over-stretching of the myocardium due to an increase in afterload leads to ventricular dilatation.
Etiology:
- Ventricular outflow obstruction.
- Hypertension
- Aortic stenosis
- Pulmonary hypertension.
- Pulmonary stenosis.
- Ventricular inflow obstruction.
- Mitral stenosis.
- Tricuspid stenosis.
- Ventricular volume overload.
- Mitral regurgitation.
- Aortic regurgitation.
- Atrial septal defect.
- Ventricular defect.
- Depressed ventricular contractility.
- Myocarditis.
- Cardiomyopathy
Read And Learn More: General Medicine Question and Answers
Pathophysiology Clinical Features:
- Due to low cardiac output.
- Fatigue
- Cold extremities
- Low BP
- Oliguria.
- Features due to left heart failure.
- Dyspnea
- Cough
- Orthopnoea.
- Paroxysmal nocturnal dyspnoea.
- Cardiac arrhythmia.
- Cardiomegaly.
- Features due to right heart failure.
- Raised jugular venous pressure
- Hepatic enlargement.
- Peripheral edema.
- Anorexia, nausea, vomiting.
- Jaundice.
- Features of chronic heart disease.
- Valvular defects.
- Congenital defects.
Cardiovascular system diseases
Pathophysiology Management:
- General measures.
- Bed rest
- Regular isotonic exercises.
- Low-calorie intake.
- Salt restriction.
- Drug therapy.
- Digitalis – digoxin – 0.25 – 0.5 mg/day.
- Sympathomimetic amine – dopamine, dobutamine.
- Diuretics – thiazides, loop diuretics, potassium sparing.
- Vasodilators – ACE inhibitors – captopril – 12.5 – 25 mg TID.
- Cardiac transplantation.
Question 2. Describe the etiology, clinical features, and management of acute ventricular failure.
Answer:
Left Ventricular Failure:
- It is defined as failure to maintain an effective left ventricular output for a given pulmonary venous or left atrial pressure.
Left Ventricular Failure Causes:
- Left ventricular outflow obstruction.
- Systemic hypertension.
- Coarctation of aorta.
- Aortic valvular stenosis.
- Left ventricular inflow obstruction.
- Mitral stenosis.
- Left ventricular volume overload,
- Mitral valve prolapsed.
- Mitral regurgitation.
- Aortic regurgitation
- Ventricular septal defect.
- Reduced left ventricular contractility.
- Cardiomyopathy.
- Anterior wall myocardial infarction.
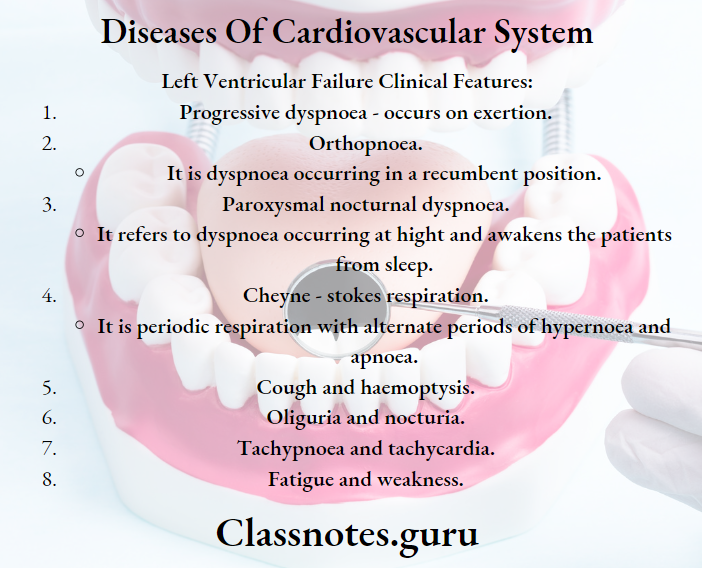
Left Ventricular Failure Clinical Features:
- Progressive dyspnoea – occurs on exertion.
- Orthopnoea.
- It is dyspnoea occurring in a recumbent position.
- Paroxysmal nocturnal dyspnoea.
- It refers to dyspnoea occurring at height and awakens the patients from sleep.
- Cheyne – stokes respiration.
- It is periodic respiration with alternate periods of hypernoea and apnoea.
- Cough and hemoptysis.
- Oliguria and nocturia.
- Tachypnoea and tachycardia.
- Fatigue and weakness.
Left Ventricular Failure Treatment:
- General measures.
- Removal of causative factors.
- Removal of precipitating factors.
- Maintain a sitting position with legs hanging alongside.
- Drugs.
- Sedative – morphine 5-10 mg IV.
- Antiemetic – Metaoclopramide – 10 mg IV
- Oxygen – 60 % through a face mask.
- Loop diuretics – frusemide – 400 -100 mg.
- Intravenous sodium nitroprusside – 20 – 30 μ/ min.
- Digoxin – 0.5 – 1 mg.
- Bronchodilator – aminophylline – 250 – 500 mg IV
- Inotropes – dopamine, dobutamine.
- Intra-aortic balloon counterpulsation.
Heart disease long essay
Question 3. Describe clinical features and treatment of ventricular septal defects.
Answer:
Ventricular Septal Defect:
- Ventricular Septal Defect implies a defect in the interventricular septum.
- The defect lies in the membraneous part or muscular part of the interventricular septum.
Ventricular Septal Defect Clinical Features:
- Common in pediatric age group.
- Remains asymptomatic for longer periods.
- Normal pulse, wide pulse pressure.
- Increased incidence of respiratory diseases.
- Systolic thrill.
- Pansystolic murmur.
- The apex beat is shifted down.
Ventricular Septal Defect Complication:
- Congestive cardiac failure.
- Pulmonary hypertension.
- Right ventricular outflow tract obstruction.
- Aortic regurgitation.
- Infective endocarditis.
Ventricular Septal Defect Treatment:
- Digoxin – 10 – 20 gg/ day.
- Frusemide – 1 – 3 mg/day.
- Small defects close spontaneously.
- Large defects require surgical repair.
Question 4. Describe etiology, clinical features, diagnosis, and treatment of rheumatic fever.
(or)
Rheumatic fever – etiology, pathology, clinical features, complications, and dental considerations.
(or)
Discuss in detail the clinical features, diagnosis, management, and prophylaxis of acute rheumatic fever.
Answer:
Acute Rheumatic Fever:
- It is an acute inflammatory disease that occurs as a sequel to infection caused by group A streptococci.
Etiology:
- Streptococcal infection.
Pathology:
- Gross appearance.
- Consists of small, uniformly sized thrombotic vegetations.
- Chronically scared, inflamed, and neovascular-sized valve.
- Microscopic appearance.
- Vegetations show.
- Surface thrombi.
- Lack of underlying valve destruction
- Mild edema.
- Chronic inflammation.
- Neo vascularisation.
- Mild calcification.
Acute Rheumatic Fever Clinical Features:
- Jones’ criteria.
- Major criteria.
- Carditis
- Polyarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules.
- Minor criteria.
- Fever
- Arthralgia.
- Raised ESR
- Previous history of rheumatic fever.
- Positive CRP.
Coronary artery disease
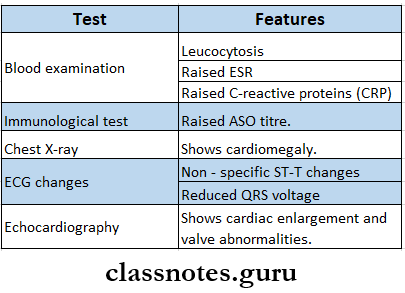
Acute Rheumatic Fever Diagnosis:
Acute Rheumatic Fever Treatment:
- Bed rest
- Drugs.
- Antibiotics.
- To treat the streptococcal infection.
- A single injection of benzathine penicillin 1.2 million IM.
- Daily injection of procaine penicillin 6,00,000 units IM for 10 days.
- Oral erythromycin – 20 40 mg/kg/day.
- Salicylates.
- For symptomatic relief in arthritis.
- Aspirin – 60 mg/kg/day 4 hourly.
- Corticosteroids.
- Prednisolone – 1 – 2 mg/kg per day.
- Antibiotics.
Prophylaxis:
- Primary prevention.
- Done by mass penicillin prophylaxis
- Established cases treated by benzathine penicillin oral penicillin or erythromycin.
- Secondary prevention.
- IM injection of 1.2 million units of benzathine penciling G every 3 weeks.
- Oral penicillin V- 250 mg twice daily.
- Sulphadiazine – lg/ day orally as a single dose.
- Erythromycin – 250 mg twice daily orally.
- Dental Consideration:
- Acute rheumatic fever is caused by group A streptococcus.
- This causes pharyngitis and sore throat.
- Good oral hygiene should be maintained as oral bacteria entering the bloodstream can increase the risk of complications.
- Antibiotics are given before some dental procedures to prevent bacterial infection of the damaged areas of the heart.
- Patients with rheumatic fever have an increased risk of developing bacterial endocarditis after a dental procedure.
Question 5. Describe clinical features, complications, diagnosis, and management of rheumatic mitral stenosis.
(or)
Describe the etiology, clinical features, investigations, and management of mitral stenosis.
Answer:
Mitral Stenosis:
- Mitral stenosis is chronic rheumatic heart disease.
Etiology:
- Rheumatic
- Congenital
- Atrial fibrillation.
- Lack of coordinated contractions of atria.
Mitral Stenosis Clinical Features:
- Symptoms due to low cardiac output.
- Fatigue
- Lethargy
- Weakness.
- Symptoms of pulmonary congestion.
- Dyspnoea.
- Orthopnoea
- Paroxysmal nocturnal dyspnoea.
- Symptoms of right heart failure.
- Puffiness of face
- Oedema of legs
- Hepatomegaly.
- Symptoms due to embolization.
- Hemoptysis.
- Chest pain
- Hemiplegia.
- Abdominal pain.
- Loss of peripheral pulses.
- Gangrenes.
- Others.
- Mitral facies
- Low pulse pressure.
- Raised jugular venous pressure.
- Cold extremities.
- Pitting edema.
Mitral Stenosis Complications:
- Pulmonary hypertension a Heart failure
- Cardiomyopathy
- Atrial fibrillation
- Pulmonary edema.
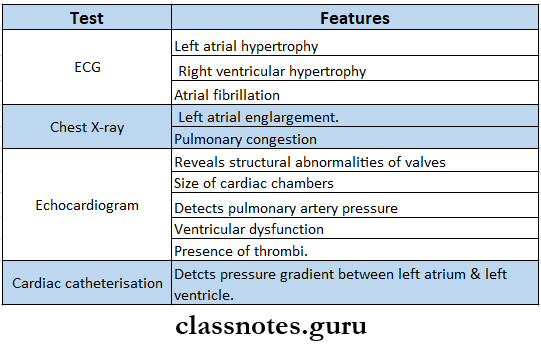
Mitral Stenosis Investigations:
Congestive heart failure essay
Mitral Stenosis Management:
- Salt restriction.
- Medical treatment.
- Digoxin – 0.25 – 0.25 mg/day
- Diuretics – to reduce pulmonary congestion.
- Anticoagulants – to prevent systemic embolization.
- Antibiotic prophylaxis.
- Surgical treatment.
- Mitral balloon valvuloplasty.
- Mitral valve replacement.
Question 6. Discuss the etiology, clinical features, diagnosis, and management of infective endocarditis.
(or)
Discuss the etiology, pathogenesis, and management of subacute bacterial endocarditis. Add a note on its prophylaxis.
(or)
Mention causative factors, clinical features, and management of bacterial endocarditis. Add on the note on dental considerations.
Answer:
Infective Endocarditis:
- Infective endocarditis is a microbial infection of the mural endocardium, heart valve, or lining of the blood vessel.
Etiology:
- Causative organisms are:
- Staphylococcus aureus.
- Streptococcus pneumonia.
- Neisseria gonococci.
Pathogenesis:
Persons with pre-existing heart disease.
↓
Transient bacteremia following dental procedures.
↓
Bacteria in circulation get deposited on the endocardium at sites of high blood flow.
↓
Develops sterile vegetation consisting of platelets and fibrin.
↓
Infective endocarditis
Infective Endocarditis Clinical Features:
- General
- Fever, weight loss, night sweats, weakness.
- GIT disturbances.
- Nausea, vomiting, anorexia.
- CVS disturbances.
- Tachycardia, conduction defects, cardiac failure.
- CNS.
- Headache, toxic encephalopathy, hemiplegia.
- Lungs.
- Hemoptysis, pleuritic pain.
- Nails.
- Clubbing, OsleTs nodes.
- Skin – petechiae, purpuric spots.
- Eyes.
- Roth’s spot, subconjunctival hemorrhage, petechial hemorrhage.
- Kidneys – hematuria.
- Spleen – spleenomegaly.
Infective Endocarditis Diagnosis:
- Duke’s criteria.
- Major criteria.
- Positive blood culture.
- Typical organisms from two cultures.
- Persistent positive blood cultures taken more than 12 hours apart.
- 3 or more positive cultures taken over more than 1 hour.
- Endocardial involvement.
- Positive ECG findings.
- New valvular regurgitation.
- Positive blood culture.
- Minor criteria.
- Predisposing heart conditions
- Fever ≥ 38° C
- Intravenous drug misuse.
- Vascular phenomena.
- Immunologic phenomena
- Microbiologic evidence.
- Treatment:
- Antibiotics.
- Penicillin G – 2 – 4 million units IV 4 – hourly.
- Gentamicin -1 mg/kg TV or IM 8 hourly.
- Ceftriaxone – 2 g IV OD.
- Ampicillin- 2 gIV4 hourly.
- Cefazolin – 2g IV 8 hourly.
- Vancomycin-15 mg/kg IV12 hourly.
- Surgery.
- Valve replacement.
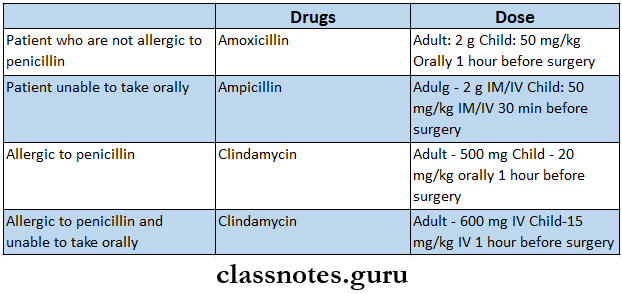
Prophylaxis:
Rheumatic heart disease
Dental, Considerations:
- Bacteria in the mouth may trigger endocarditis in people at higher risk.
- Bacteria found in tooth plaque may multiply and cause gingivitis.
- Gingiva becomes inflamed and often bleeds during tooth brushing or dental procedures.
- When gingiva bleeds, the bacteria can enter the bloodstream and infect other parts of the body.
- Antibiotic prophylaxis is required before any surgical procedures.
Question 7. Describe the signs and symptoms of angina and how would you manage the case.
(or)
Describe clinical features, investigations, management, and prevention of angina pectoris.
Answer:
Angina Pectoris:
- It is a clinical syndrome of episodic chest discomfort due to transient myocardial ischemia.
Angina Pectoris Clinical Features:
- Common in 40 – 60 years males.
- Retrosternal pain.
- It radiates to the left arm or the right arm, throat, back, chin, and epigastrium.
- It gets precipitated by exertion and relieved by rest.
- The patient feels heaviness, pressure, squeezing, or choking sensation.
- Nocturnal angina – characterized by.
- Nightmares.
- Dyspnoea.
- Palpitation.
- Skin flushing.
- Profuse sweating.
- Wide pulse pressure.
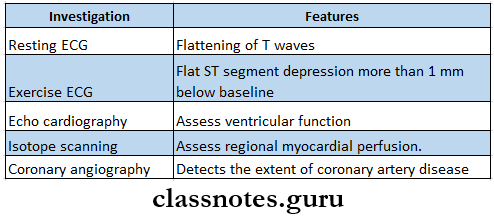
Angina Pectoris Investigations:
Angina Pectoris Management:
- General measures.
- Proper explanation of the disease.
- Avoid walking after meals.
- Avoid smoking and alcohol.
- Avoid strenuous exercise
- Reduction of risk factors.
- Control of BP and diabetes
- Treatment of co-existing diseases.
- Drug therapy.
- Aspirin – 75 – 150 mg, reduces the risk of infarction.
- Sublingual glyceryl trinitrate – 500 pg relieves angina pain within 2-3 min.
- Beta-blockers – atenolol – 50 – 100 mg orally/day.
- Calcium channel blockers – nifedipine – 5 – 30 mg orally 8 hourly.
- Surgical treatment.
- Coronary angioplasty.
- Coronary artery bypass grafting.
Angina Pectoris Prevention:
- Acute prevention
- Sublingual nitroglycerin given 15 min before exertion can prevent the attack.
- Its effect lasts for 30 min.
- Chronic prevention.
- Long-acting nitrates, beta-blockers, or calcium channel blockers are used.
Question 8. Describe the etiology, clinical features, complications diagnosis, and management of acute myocardial infarction.
(or)
What are the risk factors for coronary artery disease? Describe clinical features, investigations, and management of acute myocardial infarction.
Answer:
Risk Factors For Coronary Artery Disease:
- Old age
- More prone in males
- Family history
- Smoking, alcohol.
- Hypertension
- Mental stress.
- Sedentary habits.
- Diabetes mellitus.
- Obesity
Coronary Artery Disease Myocardial Infarction:
- Myocardial infarction is myocardial necrosis, occurring as a result of a critical balance between coronary blood supply and myocardial demand.
Etiology:
- Formation of occlusive thrombus.
- Erosion of an atheromatous plaque in a coronary artery.
Coronary Artery Disease Clinical Features:
- Prolonged and severe chest pain.
- Anxiety
- Dyspnoea
- Nausea, vomiting
- Sweating
- Syncope
- Pallor
- Tachycardia
- Cold extremities
- Oliguria.
- Low pulse pressure
- Fever
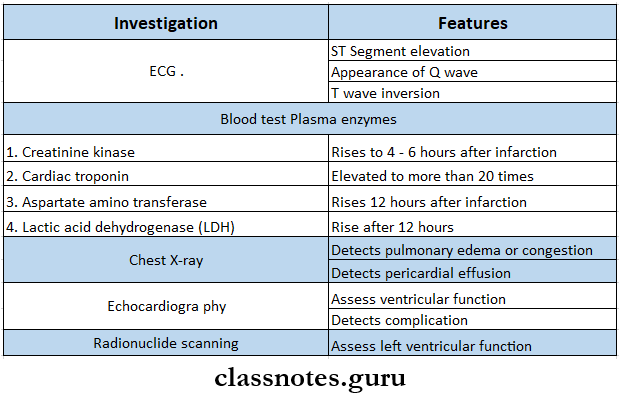
Coronary Artery Disease Investigation:
Coronary Artery Disease Management:
- Early treatment.
- Aspirin treatment.
- Sublingual glyceryl trinitrate – 0.4 – 1 mg.
- Oxygen administration – 2 – 4 L/min.
- Analgesic – 4 morphine 5 mg + antimetic metaclopramide 10gm.
- Beta-blockers – 4 metoprolol 5 mg every 2 – 5 min for 3 doses.
- Thrombolysis.
- Late treatment.
- Bed rest
- 4 morphine sulphate 10 mg + 4 prochlorperazine. 12.5 mg
- Aspirin – 75 – 150 mg.
- Inhalation of oxygen.
- Streptokinase – 1.5 million units in 100 ml of saline given in an intravenous infusion over 1 hour.
- Alteplase.
- Bolus dose 15 mg.
- 50 mg over 30 min.
- 35 mg over the next 60 min.
- Angioplasty.
- Anticoagulant – subcutaneous heparin – 7500 units twice a day for 7-10 days.
- Beta-blockers – 4 atenolol – 5 – 10 mg over 5 min.
- Nitrates – sublingual glyceryl trinitrate – 0.4 mg.
- Sedative – diazepam – 5 mg – 3-4 times a day.
Coronary Artery Disease Complications:
- Immediate:
- Arrhythmia and conduction disturbances.
- Sinus bradycardia.
- Ventricular tachycardia.
- Ventricular fibrillation.
- Atrial fibrillation
- Heart block.
- Post-myocardial angina.
- Acute circulatory failure.
- Pericarditis.
- Mechanical complications.
- Papillary muscle dysfunction.
- Rupture of the interventricular septum.
- Rupture of the ventricle.
- Mural thrombosis and embolism.
- Sudden death.
- Arrhythmia and conduction disturbances.
- Late Complication
- Post myocardial infarction syndrome.
- Ventricular aneurysm.
Cardiovascular disorders in adults
Question 9. Describe the etiology, clinical features, complications, and management of systemic hypertension.
Answer:
It is defined as a level of blood pressure at which there is an increased risk for target organ damage.
Etiology:
- Primary hypertension.
- Idiopathic.
- Secondary hypertension.
- Renal diseases
- Chronic pyelonephritis.
- Acute and chronic glomerulonephritis.
- Renal artery stenosis.
- Endocrine disorders
- Cushing syndrome
- Hyperparathyroidism.
- Pheochromocytoma.
- Acromegaly.
- Drug-induced
- Oral contraceptives
- Anabolic steroids
- Corticosteroids
- NSAIDs
- Pregnancy.
- collagen vascular disorders.
- SALE
- Miscellaneous.
- Coarctation of aorta.
- Renal diseases
Etiology Clinical Features:
- General
- Headache
- Dizziness
- Palpitation
- Fatigue.
- Primary hypertension
- Epistaxis.
- Blurring of vision.
- Hematuria.
- Angina pectoris
- Dyspnoea.
- Secondary hypertension
- Polyuria, polydipsia.
- Weakness.
- Weight gain.
- Truncal obesity.
- Episodic headache
- Palpitation
- Sweating.
Etiology Complication:
- Central nervous system.
- Cerebral, atheroma.
- Transient cerebral ischaemic attacks.
- Stroke
- Hypertensive encephalopathy.
- Subarachnoid hemorrhage.
- Retinopathy.
- Heart
- Left ventricular hypertrophy.
- Coronary artery disease.
- Cardiac failure.
- Kidneys.
- Proteinuria.
- Uraemia.
Etiology Management:
- General measures.
- Avoid unnecessary stress
- Salt restriction
- Obesity correction.
- Regular exercise
- Avoid smoking.
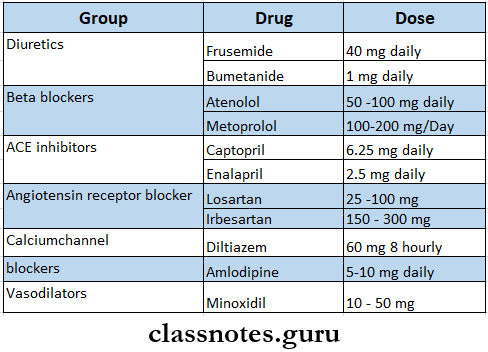
- Drug therapy.
Hypertension and heart disease
Question 10. What is hypertension? Classify hypertensive drugs. Describe complications of hypertension.
Answer:
Hypertension: Hypertension is defined as a level of blood pressure at which there is an increased risk for target organ damage.
Hypertension Classification:
- Diuretics.
- Thiazide s- hydrochlorothiazide, chlorthiali- done.
- Loop diuretics – Frusemide, bumetanide.
- Potassium-sparing diuretics – Spironolactone, amiloride.
- Drugs acting on renin – angiotensin system.
- ACE inhibitors – captopril, enalapril, lisinopril.
- Angiotensin 2 receptor antagonists – losar- tan, candesartan.
- Renin inhibitor – Aliskiren.
- Sympatholytics.
- Centrally blockers – trimethaphan.
- Adrenergic neuron blockers – reserpine.
- Adrenergic receptor blocers.
- α blockers – prazosin, phenoxybenzamine.
- β blockers – propranolol, atenolo.
- α and β blockers – labetalol.
- Calcium channel blockers.
- Verapamil, nifedipine, amlodipine.
- Vasodilators.
- Arteriolar dilators – hydralazine, minoxidil.
- Arteriolar and venular dilators – sodium ni- troprusside.
Atherosclerosis pathophysiology
Question 11. Describe etiopathogenesis, clinical features, and treatment of chronic corpulmonale.
Answer:
Definition: Chronic corpulmonale is defined as a combination of hypertrophy and dilatation of the right ventricle secondary to pulmonary hypertension.
Etiology:
- Diseases of the lung.
- Chronic obstructive pulmonary disease, COPD.
- Chronic bronchial asthma.
- Pulmonary tuberculosis.
- Cystic fibrosis.
- Pleural fibrosis.
- Diseases of pulmonary circulation.
- Recurrent pulmonary thromboembolism.
- Primary pulmonary hypertension.
- Chronic liver disease.
- Diseases of the thorax.
- Neuromuscular disease.
- Obesity.
Pathogenesis:
Increased pulmonary vascular resistance.
↓
Pulmonary hypertension
↓
Chronic corpulmonale.
Chronic Corpulmonale Clinical Features:
- Dyspnoea.
- Dry cough.
- Peripheral cyanosis, Anterior chest pain,
- Tachypnoea.
- Ankle oedema,
- Right heart failure.
- Respiratory failure.
Chronic Corpulmonale Treatment:
- Treat the cause
- Avoid smoking.
- Avoid strenuous exercise
- Avoid traveling to high altitudes.
- Oxygen therapy
- Use of anti-coagulants.
- Lung transplant.
