Clinical Features Of Gingivitis
Gingivitis Definitions
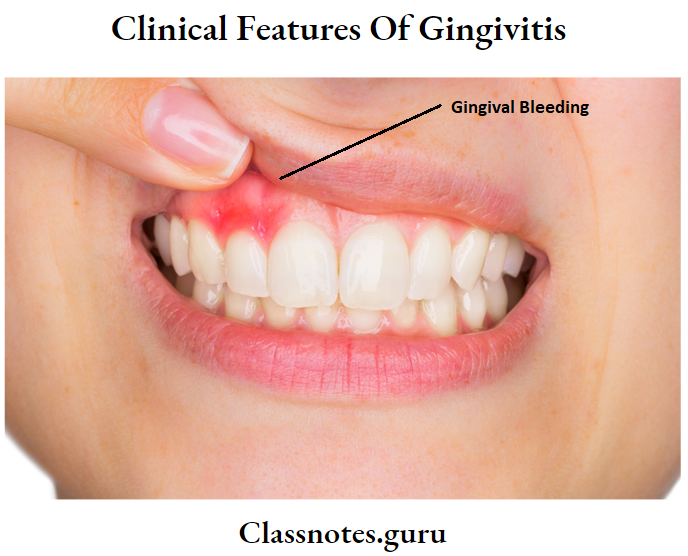
- Gingival bleeding
- It refers to bleeding from any part of the gingival
- Gingival recession
- The apical shift of the gingival margin to a position apical to the CEJ, with exposure of the root surface to the oral cavity
Clinical Features Of Gingivitis Important Notes
Gingival Recession
Gingival Recession Class 1:
- Includes marginal gingival only
- No loss of bone or soft tissue in the interdental area
- It can be narrow or wide
Gingival Recession Class 2:
- Extension of recession beyond mucogingival junction
- No loss of bone/soft tissue
- Can be wide and narrow
Read And Learn More: Periodontics Question and Answers
Gingival Recession Class 3:
- Extension of marginal recession beyond the mucogingival junction
- Loss of bone/soft tissue
- Malpositioning of teeth
Gingival Recession Class 4:
- Extension of marginal recession beyond the mucogingival junction
- Severe bone/soft tissue loss Severe
- malpositioning of teeth
1. Two earliest signs of gingival inflammation are
- Increased GCF production
- Bleeding on probing
2. Etiological factors for gingival recession
- Faulty tooth-brushing technique
- High renal attachment
- Gingival inflammation
- Tooth malposition
- Gingival ablation
Clinical Features Of Gingivitis Long Essays
Question 1. Define gingival bleeding. Describe its Suture around bleeding end causes and management.
Answer:
Gingival Bleeding:
Gingival Bleeding refers to bleeding from any part of the gingival
Gingival Bleeding Causes
1. Gingival Bleeding Local causes:
- Toothbrush trauma
- Food impaction
- Presence of plaque and calculus
- Biting into solid foods
- Acute necrotizing ulcerative gingivitis
- Gingival burns
2. Gingival Bleeding Systemic causes:
- Scurvy
- vitamin K deficiency
- Purpura
- Hemophilia
- Leukemia
- Drug-induced like salicylates, heparin
Gingival Bleeding Significance:
- It is the earliest sign of inflammation
- It gives clues for the stage where
- Active – readily bleeds
- Inactive-no bleeding
- Bleeding severity indicates the severity of inflammation
Gingival Bleeding Management:
- Consult physician
- Carry out blood tests to rule out bleeding disorders
- Treat the cause
- Operate gently and carefully
- Use of sharp instruments
- Application of pressure
- Application of moist gauze soaked in sterile ice water for several minutes
- Use of local anesthesia with vasoconstriction
- Use of hemostatic agents
- Gel foam
- Oxidized cellulose
- Surgical
Clinical Features Of Gingivitis Short Essays
Question 1. Clinical Features of Gingivitis.
Answer:
Changes Seen In Gingival:
- Color: From coral pink to bright red
- Contour: rolled margins
- Blunt papilla
- Consistency: Puffiness
- Pits on pressure
- Sloughing of gingival
- Vesicle formation
- Size: Increased
- Surface Texture: Loss of stippling
- Position: Apically displaced – In the recession
- Coronally displaced – In pseudo pockets
- Bleeding on probing: Present
Gingival Types:
- Acute: Sudden onset
- Short duration, painful
- Subacute: Less severe than acute
- Recurrent: Reappears after treatment
- Chronic: Slow in onset
- Longer duration
- Painless
Question 2. Gingival Bleeding.
Answer:
Gingival Bleeding Definition:
- Gingival Bleeding refers to bleeding from any part of the gingival
Gingival Bleeding Significance:
- The earliest sign of inflammation
- Clue for the stage where
- Active-readily bleeds
- Inactive – No bleeding
- Bleeding severity indicates the severity of inflammation
Gingival Bleeding Etiology:
- Local causes
- Toothbrush trauma
- Food impaction
- Presence of plaque and calculus
- Biting into solid foods
- Aug
- Gingival burns
- Systemic causes
- Scurvy
- vitamin K deficiency
- Purpura
- Hemophilia
- Leukemia
- Drug-induced like salicylates, heparin
Question 3. Gingival Recession.
Answer:
Gingival Recession Definition:
- The apical shift of the gingival margin to a position apical to the CEJ, with exposure of the root surface to the oral cavity
Gingival Recession Etiology:
1. Inflammatory:
- Plaque-induced periodontal diseases
- Toothbrush injury
2. Anatomic factors:
- Development anomalies
- Dehiscences
3. Iatrogenic factors:
- Clasps and bars of partial dentures
- Prolonged orthodontic treatment
- Overhanging restoration
Gingival Recession Classification: Miller’s classification
Class 1:
- Includes marginal gingival only
- No loss of bone or soft tissue in the interdental area
- It can be narrow or wide
Class 2:
- Extension of recession beyond mucogingival junction
- No loss of bone/soft tissue
- Can be wide and narrow
Class 3:
- Extension of marginal recession beyond the mucogingival junction
- Loss of bone/soft tissue
- Malpositioning of teeth
Class 4:
- Extension of marginal recession beyond the mucogingival junction
- Severe bone/soft tissue loss
- Severe malpositioning of teeth
Significance:
- Gingival recession predisposes to
- Accumulation of plaque
- Exposure of root surface
- Root caries
- Hyperemia of pulp Unesthetic appearance
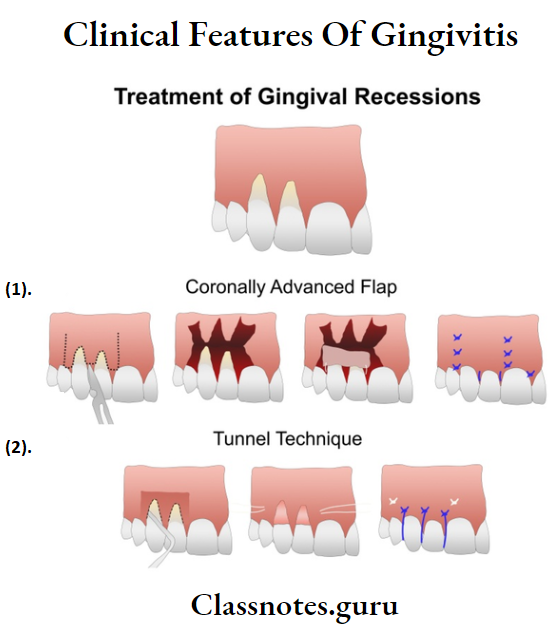
Gingival Recession Treatment:
Objectives:
- Widening of attached gingival
- Esthetic correction
Procedures:
- Colonially repositioned flap
- Guided tissue regeneration
Clinical Features Of Gingivitis Short Answers
Question 1. Classify gingival recession.
Answer:
Gingival Recession Classification:
- Miller’s classification
Gingival Recession Class1:
- Includes marginal gingival only
- No loss of bone or soft tissue in the interdental area
- It can be narrow or wide
Gingival Recession Class 2:
- Extension of recession beyond mucogingival junction No loss of bone/soft tissue
- Can be wide and narrow
Gingival Recession Class 3:
- Extension of marginal recession beyond the mucogingival junction
- Loss of bone/soft tissue
- Malpositioning of teeth
Gingival Recession Class 4:
- Extension of marginal recession beyond the mucogingival junction
- Severe bone/soft tissue loss
- Severe malpositioning of teeth
Question 2. Etiology of gingival recession.
Answer:
1. Inflammatory:
- Plaque-induced periodontal diseases
- Toothbrush injury
2. Anatomic factors:
- Developmental anomalies
- Dehiscences
3. Iatrogenic factors:
- Clasps and bars of partial dentures
- Prolonged orthodontic treatment
- Overhanging restoration
Clinical Features Of Gingivitis Viva Voce
- Bleeding on probing is a more objective sign that requires less subjective estimation by the examiner
- In gingivitis, there is no true pocket formation
- Bacteria found in gingivitis are localized in the gingival sulcus
- Inflammation of the gingival margin and a portion of con-contiguous attached Gingival is regarded as marginal gin-gives
- The earliest symptoms of gingival inflammation are increased gingival reticular fluid production and bleeding on probing
- Most common cause of abnormal gingival bleeding on probing is chronic inflammation
- The severity of the gingival recession is determined by the level of the epithelial attachment
- Recession tends to be more frequent and severe in patients with good oral hygiene
- Bleeding on probing is a best clinical indicator for gingival inflammation