Chemotherapy Of Tuberculosis and Leprosy Important Notes
1. Anti-tuberculous drugs
- First-line drugs are highly effective with low toxicity
- Second-line drugs have low efficacy with high toxicity
Chemotherapy of Tuberculosis Q&A
2. Drug regimen for tuberculosis
- INH 300 mg + Rifampicin 600 mg + Pyrazinamide 2 g or Ethambutol 15 mg/kg taken daily for 2 months
- Followed by INH 300 mg + Rifampicin 600 mg daily for 4 months
Read And Learn More: Pharmacology Question and Answers
Chemotherapy of Tuberculosis
3. Peripheral neuritis
- It is caused by isoniazid
- Can be prevented by taking pyridoxine 10 mg/day prophylactically
- Can be treated by taking pyridoxine 100 mg/day
- Drugs causing peripheral neuritis are:
- Griseofulvin
- Nitrofurantoin.
- Vincristine
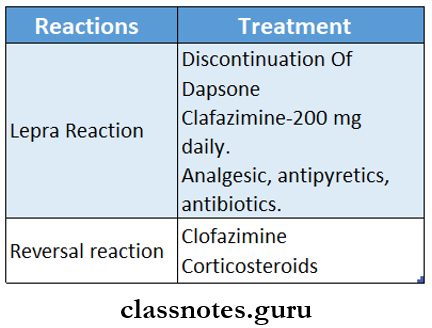
4. Lepra reaction
- It is seen in lepromatous chemotherapy
- Occurs due to the release of antigens from bacilli
- Drugs used to control it are:
- Clofazimine
- Chloroquine
- Thalidomide
Chemotherapy Of Tuberculosis and Leprosy Long Essays
Question 1. Classify drugs used in tuberculosis. Write the pharmacology of any two commonly used drugs.
Answer:
Tuberculosis:
- Tuberculosis is a chronic granulomatous disease.
Tuberculosis Anti-tubercular drugs:
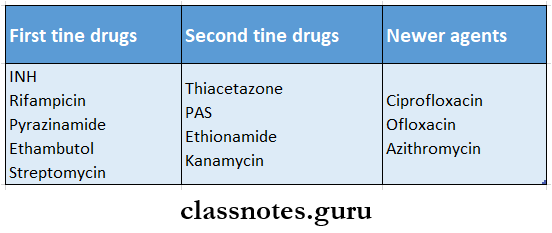
- According to their clinical utility, the anti-tuberculosis drugs are divided into.
1. First-line drugs.
- They have high antitubercular efficacy.
- Have low toxicity.
- They are:
- Isoniazid (H)
- Rifampicin (R)
- Pyrazinamide (Z)
- Ethambutol (E)
- Streptomycin (S)
2. Second-line drugs.
- They have low antitubercular efficacy.
- Have high toxicity.
- They are:
- Thiacetone (Tzn)
- Para-aminosalicylic acid (PAS)
- Ethionamide (Etm)
- Kanamycin (Kmc)
- Amikacin (Am)
- Newer drugs are:
- Ciprofloxacin, ofloxacin, clarithromycin, azithromycin.
Antitubercular drugs questions and answers
Chemotherapy of Tuberculosis
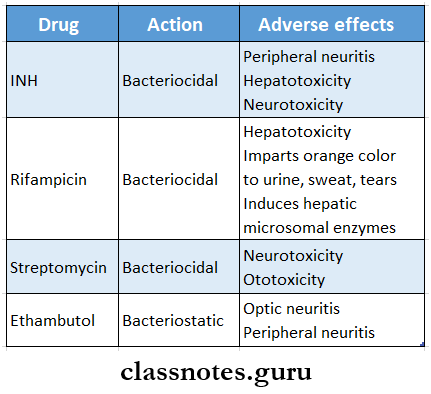
Isoniazid: (INH):
- It is the most effective and cheapest primary antitubercular drug.
- It is effective against both intra and extracellular organisms.
Isoniazid Mechanism of action:
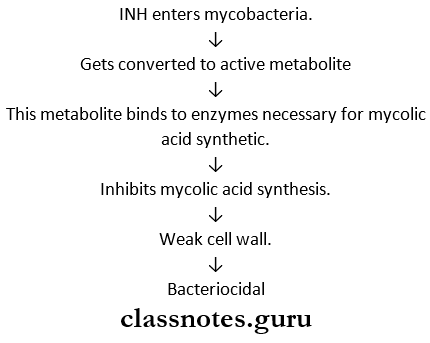
Isoniazid Pharmacokinetics:
- Completely absorbed orally.
- Penetrates all tissues.
- Metabolized by acetylation.
- Metabolites are excreted in the urine.
Isoniazid Adverse effects:
1. Peripheral neuritis.
- Occurs due to increased excretion of pyridoxine.
- Characterized by paraesthesia, numbness, mental disturbances, and convulsions.
- Avoided by prophylactic uses of pyridoxine with INH.
2. Hepatitis.
- Occurs due to dose-related damage to liver cells.
- More common in alcoholics and elders.
3. CNS effects – psychosis, seizures.
4. Hemolysis. In GePD deficiency patients.
5. Other effects.
- Anorexia, GIT disturbances, fever, rashes, acne, arthralgia.
Chemotherapy of Tuberculosis
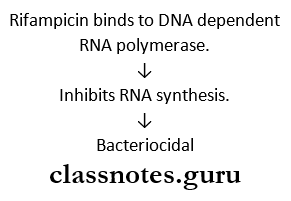
Rifampicin:
- It is a semisynthetic derivative of rifamycin B.
- It is highly effective.
- Acts on both intracellular and extracellular organisms.
Rifampicin Mechanism of action:
Rifampicin Pharmacokinetics:
- Well-absorbed orally.
- Has good tissue penetrability.
- Metabolized in the liver, excreted in bile.
- It is a microsomal enzyme inducer.
- Appears in saliva, tears, and sweat.
Rifampicin Adverse effects:
1. Hepatotoxicity.
- Causes hepatitis in patients With pre-existing liver disease.
2. Respiratory syndrome.
- Breathlessness, shock, collapse.
3. Purpura, hemolysis, renal failure.
4. GIT disturbances.
- Epigastric distress, nausea, Vomiting, Abdominal cramps, diarrhea.
5. Flu-hike synthesis drome.
- Fever, body ache, chills; hemolytic anemia.
6. CNS effects.
- Headache, drowsiness, dizziness ataxia.
7. Cutaneous syndrome.
- Flushing, pruritis, rash, redness, watering of eyes.
Rifampicin Other Uses:
- Leprosy.
- Prophylaxis Of H.influenza And Meningitis.
- Resistantstephylococcal infections.
- Brucellosis.
- To eradicate the nasal carrier state of meningitis.
Antileprosy drugs MCQs with answers
Chemotherapy Of Tuberculosis and Leprosy Short Essays
Question 1. DOTS chemotherapy in tuberculosis.
Answer:
- DOTS in directly observed treatment short course.
- It was recommended by WHO in 1995.
- It is found to be effective.
- It involves providing the most effective medicine and confirming that it is taken.
- Antitubercular drugs during the intensive phase are administered under the direct supervision of peripheral health staff or through voluntary workers.
- It ensures a high cure rate through its following components.
- Appropriate medical treatment.
- Supervision and Motivation by health and non-health workers.
- Monitoring of disease status by health services.
DOTS chemotherapy in tuberculosis Category:
- According to DOTS, patients are grouped into two categories
1. Category -1 – new patients
- New sputum smear positive.
- New sputum smear negative.
- New extrapulmonary.
- New others.
2. Category – II – previously treated patients.
- Smear positive relapse.
- Smear positive failure.
- SmeOr positive treatment after default.
Question 2. Mention six drugs for tuberculosis.
Answer:
1. First-line drugs.
- Isoniazid.
- Rifampicin
- Pyrazinamide
- Streptomycin.
2. Second-line drugs
- Thiacetazoue.
- Paia-aminosalicylic acid
- Ethionamide
- Cycloserine
- Kanamycin
- Amikacin
3. Newer Drugs.
- Ciprofloxacin.
- Ofloxacin.
- Clarithromycin.
- Azithromycin.
- Rifabutin.
Pharmacology of TB and leprosy notes
Question 3. Explain why multidrug therapy is used in the treatment of tuberculosis.
Answer:
Tuberculosis is one of the most difficult infections to curve.
- Its treatment is problematic due to
- Slow division of mycobacteria.
- Development of resistance.
- Ability to remain as persisters for years.
- Intracellular location of barley.
- Presence of caseous material.
- Long term therapy
- Expensive treatment
- Drug toxicity.
- Drug toxicity.
Tuberculosis Aim of treatment:
- Kill dividing bacilli – to make sputum negative
- To destroy persisters – to prevent relapse.
Tuberculosis Combination of Drugs:
- Drugs are combined to
- Delay development of resistance.
- Reduce toxicity.
- Shorten the course of treatment
Chemotherapy of Tuberculosis
Question 4. Dapsone (DDS).
Answer:
- Dapsone is diamino diphenyl sulfone (DDS)
- It is a simple, old, cheap, and active antileprotic drug.
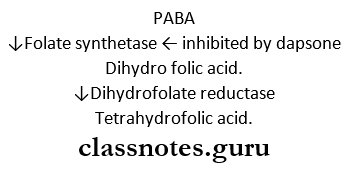
Dapsone Mechanism of action:
- Dapsone is chemically related to sulphonamide.
- It is a structural analog of PABA.
- It competitively inhibits bacterial folate synthetase.
- It also inhibits the union of PABA with pteridine residue to form dihydropetroic acid.
Dapsone Pharmacokinetics:
- Dapsone is completely absorbed orally.
- It is widely distributed.
- It is metabolized in the liver and excreted in bile.
- It is acetylated.
- It is leprostatic.
Dapsone Uses:
- Leprosy – a primary drug for leprosy.
- Used in combination with pyrimethamine for chloroquine-resistant malaria.
- Dermatitis is herpetiform.
- Used along with trimethoprim in P.jiroveci infections in patients with AIDS.
Question 5. Treatment schedule for leprosy.
Answer:
- Treated by multidrug therapy regime introduced by WHO in 1981.
- Drugs used are dapsone, rifampicin, and clofazime.
- All are administered orally.
Leprosy Duration:
- 2- years – for multibacillary/infectious leprosy.
- 6 months – for paucibacillary/non-infectious leprosy.
Leprosy Schedule:
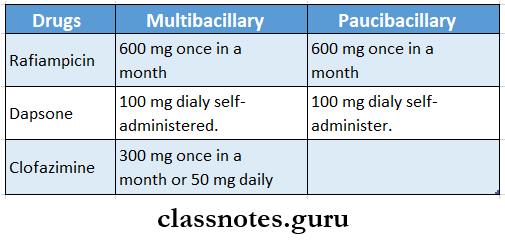
Leprosy Alternative regimen:
1. Clofazimine 50 mg with any two newer drugs daily for 6 months.
- Followed by clofazimine 50 mg with anyone new drug daily for 18 months.
2. In single lesion paucibacillary leprosy,
- Single dose of
- Rifampicin – 600mg.
- Ofloxacin-400 mg.
- Minocycline – 100 mg.
Chemotherapy of Tuberculosis
First-line TB drugs Q&A
Question 6. Lepra reactions.
Answer:
Lepra reactions are immunologically-mediated reactions that occur during the course of the disease.
Types:
1. Type I reaction – reversal reaction.
- Seen in tuberculoid leprosy.
- They are cell-mediated, delayed hypersensitivity reactions.
- Characterized by cutaneous ulceration, multiple nerve involvement with pain and tenderness.
Type I reaction – reversal reaction Treatment:
- Treated with corticosteroids or clofazimine.
2. Type II reactions – lepra reaction.
- Seen in lepromatous leprosy.
- It is Jarischherxheimertypeofireaction.
- It is a type III hypersensitivity reaction due to the release of antigens from killed bacilli.
- It is abrupt in onset.
- Old lesion – enlarges, becomes red, swollen, and painful.
- New lesions also appear.
- Fever, malaise, lymphadenitis, myositis, and neuralgia occur.
Type II reactions – lepra reaction Treatment:
- Temporary discontinuation of dapsone in severe cases.
- Administration of analgesics, antipyretics, and antibiotics.
- Clofazimine – 200 mg daily in most severe cases.
- Corticosteroids are used in severe cases.
Chemotherapy Of Tuberculosis And Leprosy Short Question And Answers
Question 1. Adverse effects of rifampicin.
Answer:
- Hepatitis.
- Respiratory syndrome.
- Purpura, hemolysis, shock, renal failure.
- Cutaneous syndrome.
- Flu-like syndrome.
- GIT disturbances.
- Staining of secretions.
- Hypersensitivity reactions.
Question 2. Pyridoxine should be administered with INH.
Answer:
- Isoniazid (INH) is anti-tubercular drug.
- It causes peripheral neuritis due to interference with utilization and increased excretion of pyridoxine.
- It is characterized by paresthesia, numbness, mental disturbances, and convulsions.
- It is avoided by prophylactic use of pyridoxine 10-50 mg.
- Hence, pyridoxine should be administered with INH to prevent peripheral neuritis.
Question 3. Streptomycin.
Answer:
- Streptomycin is an anti-tuberCuter drug.
- It is tuberculocidal.
- It acts only against extracellular organisms.
- It does not cross CSF.
- When used alone resistance develops rapidly.
Streptomycin Disadvantages:
- The rapid development of resistance.
- Has to be given IM.
- Causes ototoxicity and nephrotoxicity.
- Thus, streptomycin is the least preferred.
Tuberculosis pharmacology important questions
Chemotherapy of Tuberculosis
Question 4. Pyrazinamide.
Answer:
- Pyrazinamide is tuberculocidal.
- It is more active at acidic pH.
- Has good sterilizing activity.
- Highly effective during the first 2 months of therapy.
- It is well-absorbed orally.
- Metabolized in the liver, excreted in urine.
Pyrazinamide Adverse effects:
- Hepatotoxicity.
- Hyperuricaemia.
- Arthralgia.
- Anorexia, vomiting.
- Rashes.
- Fever, flushing.
- Loss of diabetes control.
Question 5. Isoniazid acetylation status in tuberculosis chemotherapy.
Answer:
- Isoniazid is metabolized by acetylation.
- Depending on the genetic variations, patients can be fast or slow acetylation.
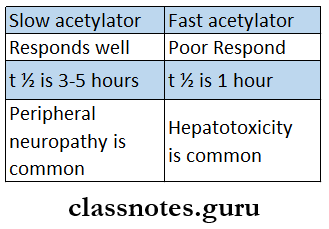
- metabolites are excreted in the urine.
Question 6. Drugs used in the treatment of leprosy.
Answer:
- Sulfone-dapsone.
- Phenazine derivative – clofazimine.
- Antitubercular drugs – rifampin, ethionamide.
- Other antibiotics-Oflaxacin, minocycline.
Leprosy treatment pharmacology questions
Question 7. Dapsone.
Answer:
- Dapsopne is diamino dlpheyl sulfone (DDS).
- It is a simple, cheap, old, and more active anti-leprotic drug.
Question 8. Treatment of lepra reactions.
Answer: