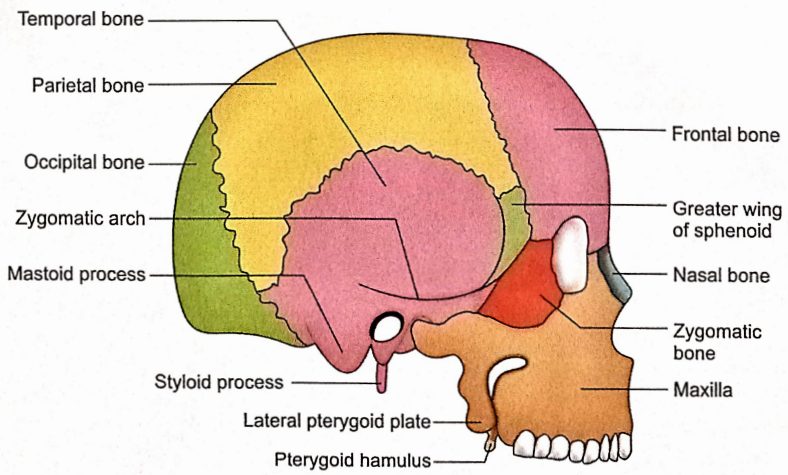
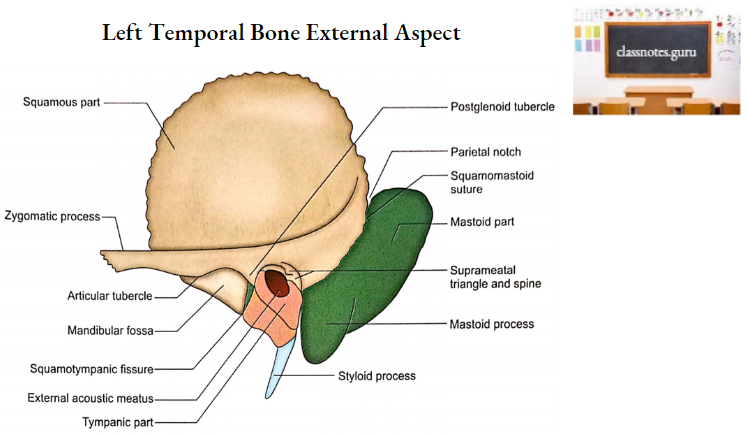
Temporal Bones
Temporal Bones Terminology
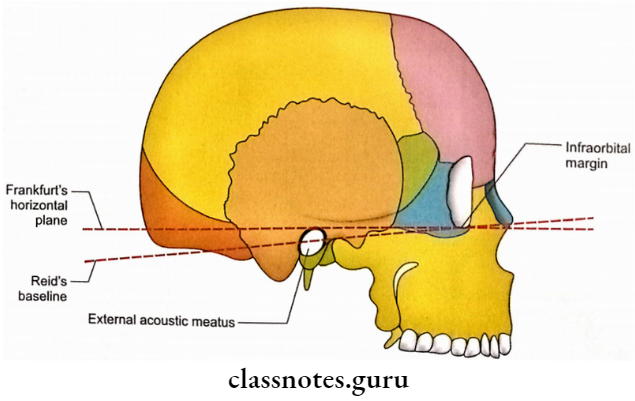
The temporal bone is so named because of its contribution to the temporal region.
Temporal Bones Side Determination
1. To distinguish superior and inferior, the following features are to be noted:
- A thin plate-like squamous part is directed upwards and lies in para- the sagittal plane.
- Styloid and mastoid processes occupy the lower part of the bone and are directed downwards.
2. To distinguish external and internal aspects, one should consider the following features:
- The outer surface of the squamous part is very smooth.
- The zygomatic process is directed forward.
- The zygomatic process is present on the external aspect of bone.
- External acoustic meatus (present below the posterior part of the zygomatic process) opens externally.
- The apex of the petrous temporal is directed medially and a little forward.
3. To distinguish anterior from posterior, the following criteria should be taken into account:
- The zygomatic process is directed forward.
- The mandibular fossa and external acoustic meatus are present below the posterior part of the zygomatic process. Relatively, the mandibular fossa is anterior to the external acoustic meatus.
Temporal Bones Features And Attachments
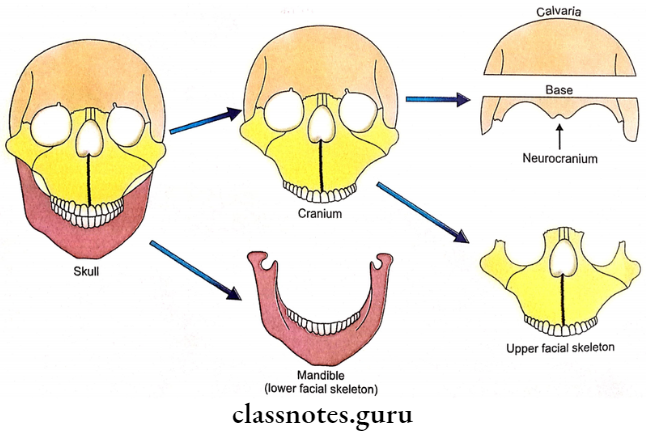
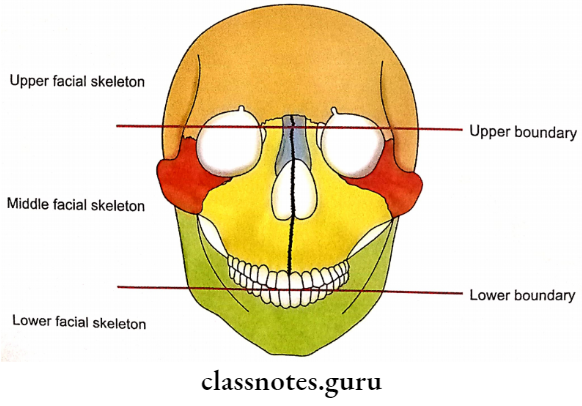
Morphologically temporal bone is divided into four parts.
- Squamous part.
- Petromastoid part.
- Tympanic part.
- Styloid process.
For descriptive purposes, the petromastoid part is further subdivided into the mastoid part and the petrous part.
Temporal Bones Squamous Part
It is thin and plate-like and occupies the anterior and superior parts of the temporal bone. It has two surfaces (temporal and cerebral) and two borders (superior and anteroinferior).
1. Surfaces
- Temporal Surface
- It is the outer surface.
- It is smooth and slightly convex.
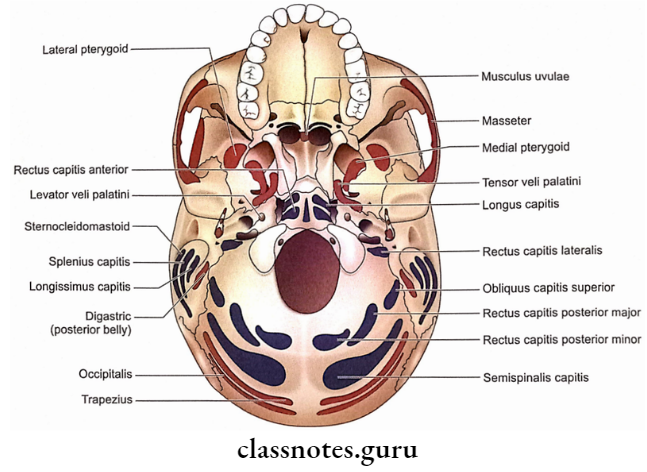
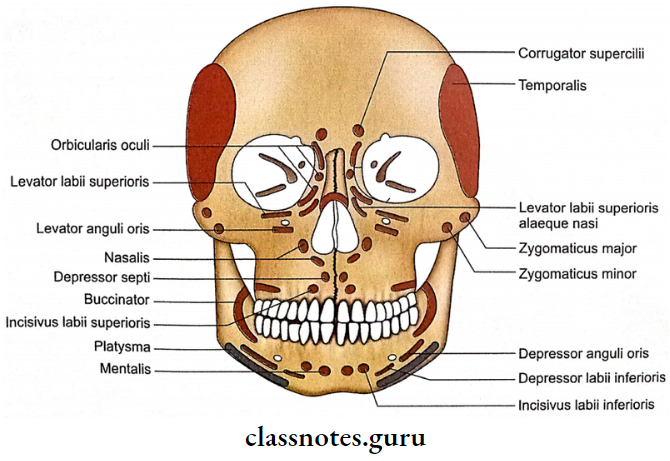
- It contributes to the temporal fossa, the origin of the temporalis muscle.
- The middle temporal artery grooves the surface, just above the external acoustic meatus.
- The supramastoid crest runs backwards and upwards across its posterior part. Temporal fascia is attached to this crest.
- Squamomastoid suture marks the junction between squamous and mastoid parts. It is situated 1.5 cm. below the supramastoid crest.
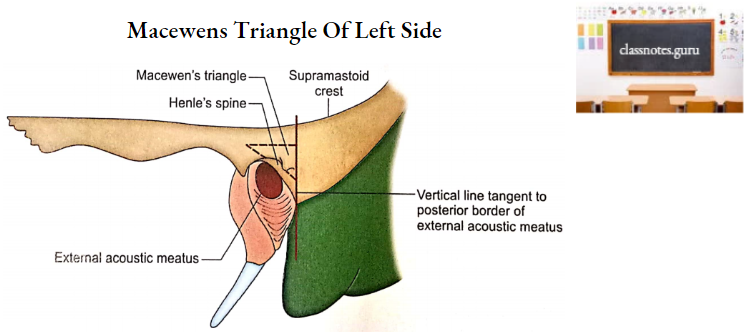
- Macewen’s Triangle (Suprameatal Triangle)
- It is a triangular depression posterosuperior to the external acoustic meatus.
- It is bounded by the posterosuperior margin of the external acoustic meatus, supramastoid crest and a vertical line tangent to the posterior border of the external acoustic meatus.
- The spine of Henle is a sharp, spur-like projection in the supramental triangle.
- The mastoid antrum is situated 12.5 mm deep to the surface of the supramental triangle in adults.
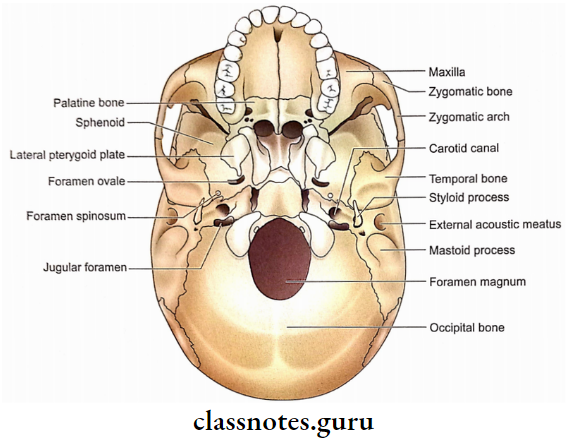
- Zygomatic Process
- It is a forward projection from the lower part of the temporal surface.
- Its anterior end articulates with the temporal process of zygomatic bone to complete the zygomatic arch or zygoma.
- The anterior part of the zygomatic process has two surfaces (lateral and medial) and two borders (superior and inferior). Masseter originates from its medial surface and inferior border. The temporal fascia is attached to its superior border. Its lateral surface is subcutaneous.
- Its posterior part is triangular having superior and inferior surfaces.
- The inferior surface of the posterior part of the zygomatic process is bounded by two roots (anterior and posterior) which converge at the tubercle of the root of the zygoma. The lateral ligament of the temporomandibular joint is attached to this tubercle.
- The anterior root extends medially from the tubercle of the root of the zygoma and is also called the articular tubercle.
- Mandibular Fossa
- It is situated behind the articular tubercle.
- Only the anterior part of the mandibular fossa is articular and contributed by the squamous part of the temporal bone.
- Articular tubercle and anterior part of mandibular fossa is related to the superior surface of articular disc of temporomandibular joint.
- The posterior part of the mandibular fossa is non-articular and contributed by the tympanic part of the temporal bone. This part is related to the parotid gland.
- Squamotympanic Fissure
- It is situated in the mandibular fossa and marks the junction of squamous and tympanic parts of the temporal bone.
- The medial part of this fissure is divided into petrosquamous and petrotympanic fissures by the projection of the tegmen tympani of the petrous part of the temporal bone.
- Three structures pass through petrotympanic fissure, i.e. chorda tympani nerve, anterior tympanic artery and anterior ligament of the malleus.
- Note: To remember the structures passing through petrotympanic fissure think of a ‘CAT’ in which the C-Chorda tympani nerve, A-Anterior ligament of malleus and T-Tympanic artery.
- A petrotympanic fissure leads into the middle ear.
- Cerebral Surface
- It is the inner surface.
- It is grooved by middle meningeal vessels.
- It has impressions for the sulci and gyri of the temporal lobe of the cerebrum.
2. Borders
- Superior border
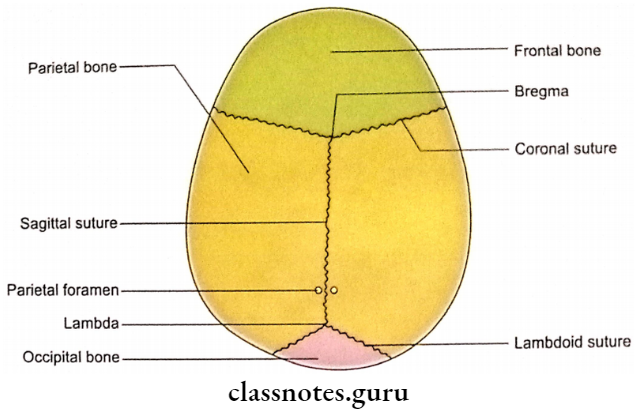
- It articulates with the parietal bone.
- Temporal Bones
- It articulates with the greater wing of the sphenoid bone.
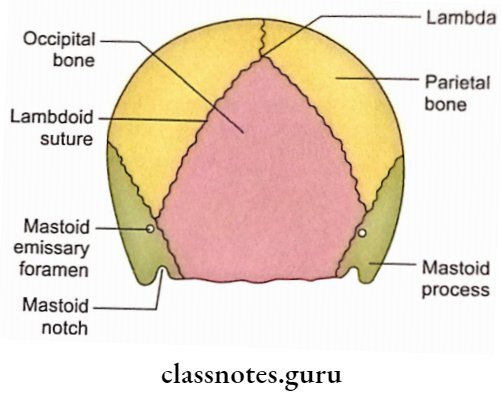
Temporal Bones Mastoid Part
It forms the posterior part of the temporal bone. It consists of two surfaces (outer and inner), two borders (superior and posterior) and a downward projecting part called the mastoid process.
1. Surfaces
- Outer Surface
- The auricularis posterior and occipital belly of occipitofrontalis are attached to this surface.
- The mastoid foramen is an infrequent opening near the posterior border. When present this foramen transmits an emissary vein from the sigmoid sinus and a branch from the occipital artery.
- Inner surface
- The sigmoid sulcus is a deep groove on the inner surface. It is meant for the sigmoid sinus.
- Mastoid foramen opens in the upper part of sigmoid sulcus.
2. Borders
- Superior Border
- It articulates with the occipital bone at occipitomastoid suture.
- Posterior Border
- It articulates with the occipital bone at occipitomastoid suture.
3. Mastoid process
It possesses a lateral and a medial surface.
- Lateral surface
- It gives insertions to the following three muscles from above downwards:
- Sternomastoid.
- Splenius capitis.
- Longissimus capitis.
- It gives insertions to the following three muscles from above downwards:
- Medial surface
- It is marked by a deep groove called a mastoid notch, from which originates the posterior belly of the digastric.
- The occipital groove is observed medial to mastoid notch. This groove lodges the occipital artery.
Temporal Bones Petrous Part
Petrous is a Latin word which means strong or rock-like. It is a strong part of the temporal bone and protects the internal ear within it.
The petrous part is comprised of a base, an apex, three surfaces (anterior, posterior and inferior) and three borders (superior, anterior and posterior).
1. Base
- It is directed laterally.
- It fuses with the squamous part at petrosquamosal suture which disappears soon after birth.
- The base also fuses with the mastoid part.
- The base is separated from the squamous and mastoid parts by an air-filled space called the mastoid antrum.
2. Apex
- It projects medially and slightly forward.
- It is situated between the greater wing of the sphenoid and the basilar part of the occipital bone.
- It forms the posterolateral boundary of the foramen lacerum.
- It possesses an anterior orifice of the carotid canal.
3. Surfaces
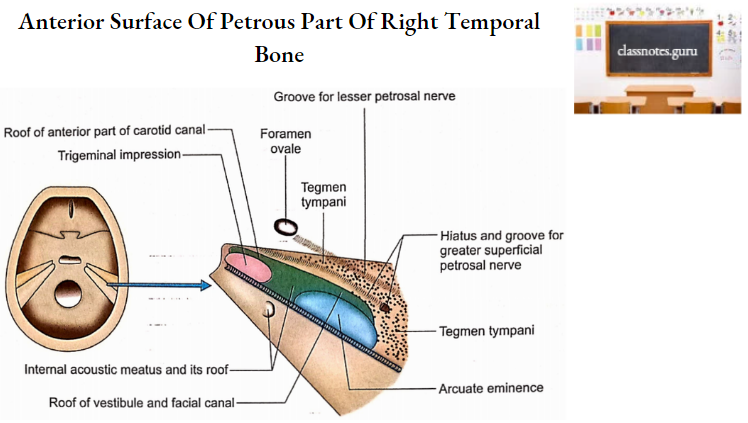
- Anterior surface
- It contributes to the middle cranial fossa.
- This surface shows the following features if one goes from apex to base:
- Trigeminal impression: It is a depression for the trigeminal ganglion adjacent to the apex.
- The roof of the internal acoustic meatus: Is another depressed area behind the ridge.
- Arcuate eminence: It is a prominent elevation produced by the superior semicircular canal. Its posterior sloping lies over lateral and posterior semicircular canals.
- Area anterolateral to trigeminal impression forms the roof of the anterior part of the carotid canal.
- Area anterolateral to arcuate eminence forms the roof of the vestibule and the beginning of the facial canal.
- A thin plate of bone between the squamous part (cerebral surface) of the temporal bone and the features described above is called tegmen tympani.
- It forms the roof of the mastoid antrum, middle ear and canal for tensor tympani from posterior to anterior.
- Tegmen tympani projects downwards to form lateral walls of the canal for tensor tympani and bony Eustachian tube and appears in the squamotympanic fissure.
- A hiatus (opening) lateral to arcuate eminence leads into a groove for greater superficial petrosal nerve which runs towards the foramen lacerum on the tegmen tympani.
- Lateral to the groove for the greater superficial petrosal nerve presents a groove for the lesser petrosal nerve which runs towards the foramen ovale.
- Posterior Surface
- It contributes to the posterior cranial fossa.
- Internal acoustic meatus is present in the centre of this surface. It transmits facial and vestibulocochlear nerves and labyrinthine vessels. It is about 1 cm in length.
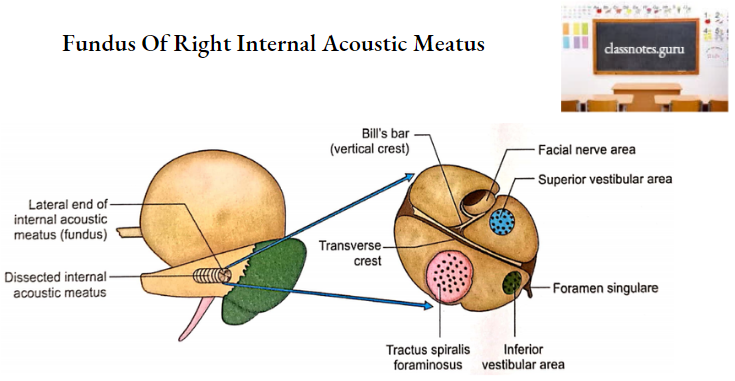
- The fundus of the internal acoustic meatus is a plate of bone at its lateral end. This plate is divided into upper and lower areas by a transverse ridge called crista falciformis.
- The upper area is further divided into anterior and posterior areas by a vertical crest called Bill’s bar. The anterior area shows a facial canal for the facial nerve.
- The posterior area is called the superior vestibular area which presents a number of small openings for the nerve fibres supplying the utricle and superior and lateral semicircular ducts.
- Below the transverse crest, anteriorly is the cochlear area (which possesses a number of foramina called tractus spiralis for aminosus) and posteriorly is the inferior vestibular area.
- Fibres of the cochlear nerve enter the cochlear area while nerve fibres supplying the saccule enter the inferior vestibular area.
- Below and behind the inferior vestibular area is the foramen singular for the passage of the nerve to the posterior semicircular duct.
- A slit behind the internal acoustic meatus leads into the aqueduct of the vestibule which contains the saccus and ductus endolymph phatic along with a small artery and vein.
- An irregular depression called the subarcuate fossa is located above and between the openings of the internal acoustic meatus and the aqueduct of the vestibule. It lodges a process of dura mater.
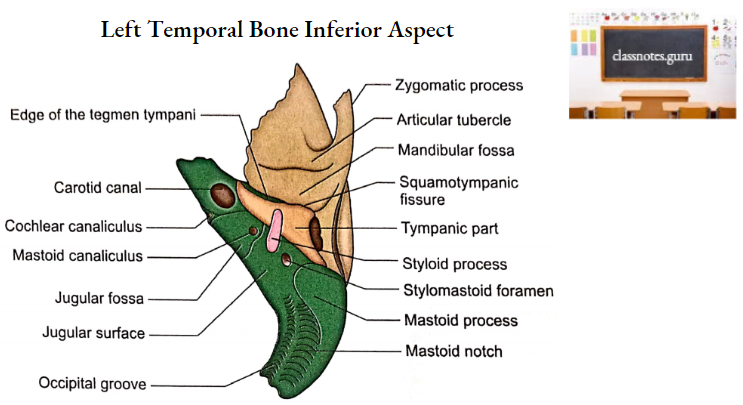
- Inferior Surface
- It is rough and triangular.
- It is divided into four areas from apex to base.
- The quadrilateral area near the apex provides attachment to the levator palate muscle.
- The Carotid canal (lower opening) is present behind the quadrilateral area. It transmits the internal carotid artery along with its sympathetic and venous plexuses.
- The jugular fossa is a depression behind the carotid canal. It lodges the superior bulb of the internal jugular vein.
- The jugular surface is a quadrilateral area behind the jugular fossa. It articulates with the jugular process of the occipital bone.
- A triangular depression in front of the medial part of the jugular fossa lodges the inferior ganglion of the glossopharyngeal nerve. The apex of this triangular depression is marked by an opening leading into the cochlear canaliculus which is traversed by:
- Perilymphatic duct
- Prolongation of dura mater
- A vein from the cochlea drains into the internal jugular vein.
- The canaliculus for the tympanic nerve (a branch of the glossopharyngeal nerve) is situated on the bony ridge between the carotid canal and the jugular fossa.
- The mastoid canaliculus is present in the lateral wall of the jugular fossa. It transmits the auricular branch of the vagus.
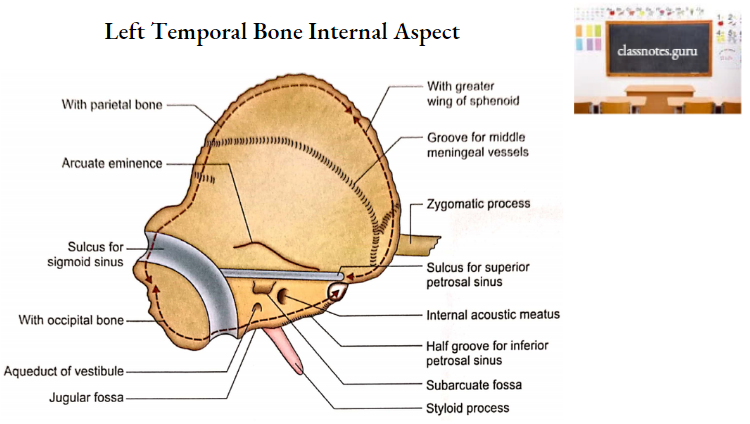
4. Borders
- Superior border
- It is grooved by the superior petrosal sinus.
- Margins of the groove provide attachment to tentorium cerebelli.
- Anterior border
- It is divided into medial and lateral parts.
- The medial part articulates with the greater wing of the sphenoid.
- The lateral part joins the squamous part at petrosquamosal suture which disappears soon after birth.
- Posterior border
- It can be divided into medial and lateral parts.
- The medial part has a sulcus which with a similar sulcus on the occipital bone forms a groove for the inferior petrosal sinus.
- The lateral part is occupied by a larger jugular fossa laterally and a smaller glossophary deal notch medially. The lateral part forms the anterior boundary of the jugular foramen whose posterior boundary is formed by the jugular notch of the occipital bone.
Temporal Bones Tympanic Part
It is a curved bony plate situated below the squamous part and in front of the mastoid part of the temporal bone.
- It joins the squamous part at squamotympanic fissure and mastoid part at tympanomastoid fissure. Auricular branch of vagus emerges through the tympanomastoid fissure.
- The tympanic part has two surfaces (anterior and posterior) and three borders (lateral, upper and lower).
1. Surfaces
- Anterior Surface
- It forms the posterior nonarticular part of the mandibular fossa.
- It is related to the parotid gland.
- Posterior Surface
- It forms the anterior wall, floor and the lower part of the posterior wall of the external acoustic meatus.
- Its medial end is marked by a groove called the tympanic sulcus. This sulcus provides attachment to the circumferential of the tympanic membrane.
2. Borders
- Lateral Border
- It is free.
- It continues with the cartilaginous part of the external acoustic meatus.
- Upper border
- Laterally it fuses with the postglenoid tubercle.
- Medially it forms the posterior boundary of the petrotympanic fissure.
- Lower Border
- Medially it extends up to the carotid canal.
- Laterally it splits to form the veginal process which encloses the root of the styloid process.
Temporal Bones Styloid Process
- The styloid process is divisible into two parts:
- Proximal or tympanohyal part
- It is surrounded by a bony sheath derived from the lower border of the tympanic part of the temporal bone.
- Distal Or Stylohyal Part
- It is visible lower part. It is this part which is described below.
- Proximal or tympanohyal part
- The styloid process is a conical projection directed downwards, forwards and slightly medially.
- It provides attachments to five structures (3 muscles and 2 ligaments):
- Medially: Stylopharyngeus muscle.
- Anteriorly: Styloglossus muscle.
- Posteriorly: Stylohyoid muscle.
- Laterally: Stylomandibular ligament.
- At the tip: Stylohyoid ligament.
- Some important relations are as follows:
- It is interposed between two important structures, the parotid gland (laterally) and the internal jugular vein (medially).
- The external carotid artery crosses the tip of the styloid process superficially
- The facial nerve crosses the base of the styloid process laterally.
- Stylomastoid foramen is situated behind its base (between it and the mastoid process). The following structures pass through this foramen:
- Facial nerve.
- Stylomastoid artery.
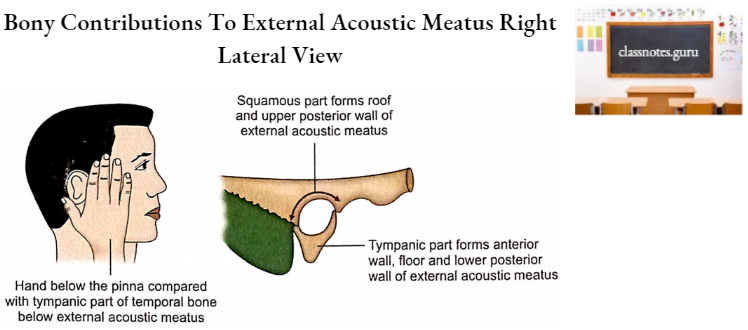
Temporal Bones Spaces And Canals External acoustic meatus
- The bony part of the external acoustic meatus is about 16 mm long. This contribution is about 2/3rd of the total length (24 mm).
- It is directed medially, downwards and slightly forward.
- The tympanic part of the temporal bone contributes to its anterior wall, floor and lower part of the posterior wall.
- The squamous part of the temporal bone forms its roof and the upper part of the posterior wall.
Middle Ear Space (Tympanic Cavity)
- Parts
- The tympanic cavity consists of three parts:
- Tympanic cavity proper (mesotympanum): Opposite the tympanic membrane.
- Epitympanic recess (epitympanum): Above the level of the tympanic membrane.
- Hypotympanum: Below the level of the tympanic membrane.
- Measurements
- Vertical diameter – 15 mm.
- Anteroposterior diameter – 15 mm.
- Transverse diameters:
- Upper part – 6 mm.
- Lower part – 4 mm.
- Opposite the centre of the tympanic membrane 2 mm.
- Boundaries
- Roof
- It is formed by tegmen tympani which separates the middle ear from the middle cranial fossa.
- Floor
- It is formed by a thin plate of bone which separates the cavity from the superior bulb of the internal jugular vein.
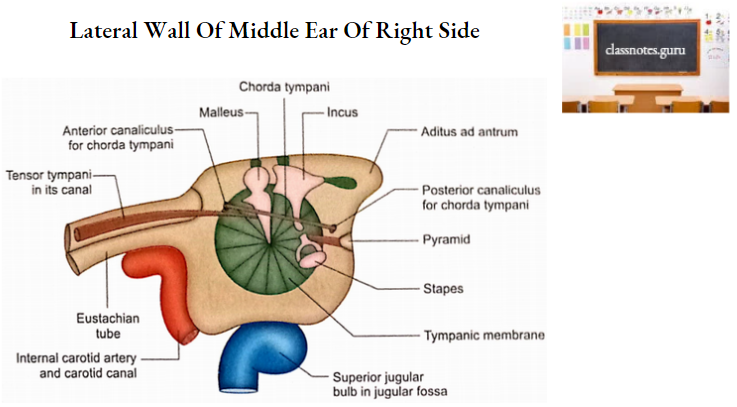
- Lateral wall
- It is formed mainly by the tympanic membrane.
- Close to the circumference of the tympanic membrane, there are three small apertures:
- Petrotympanic fissure: It is located. anteriorly.
- Anterior canaliculus for chorda tympani: It is located at the medial end of the petrotympanic fissure.
- Posterior canaliculus for chorda tympani It is located posteriorly.
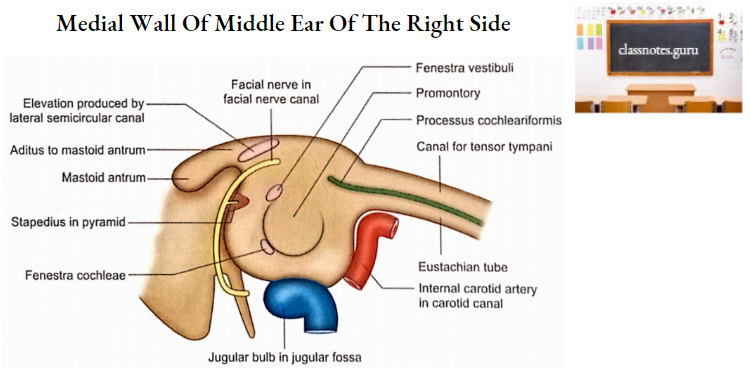
- Medial wall
- It is the lateral wall of the internal ear.
- It has a rounded elevation called promontory produced by the basal turn of the cochlea.
- Promontory is grooved by the nerves of tympanic plexus.
- A depression behind the promontory, the sinus tympani, indicates the position of the ampulla of the posterior semicircular canal.
- Fenestra vestibuli is a reniform opening posterosuperior to the promontory. It
connects the tympanic cavity to the vestibule of the internal ear. - Fenestra cochlea is a rounded opening in the posteroinferior part of the promontory. It connects the tympanic cavity with the scala tympani of the cochlea.
- Above and posterior to the fenestra vestibuli there is an elevation produced by the facial nerve canal.
- Posterior wall
- Aditus to the mastoid antrum is an opening in the upper part of the posterior wall. It connects the epitympanic recess with the mastoid antrum.
- The medial wall of the aditus to mastoid antrum shows an elevation produced by the lateral semicircular canal.
- The facial nerve canal lies vertically in the posterior wall anterior to which is a pyramidal eminence projecting into the middle ear cavity.
- Pyramidal eminence is occupied by the stapedius muscle.
- Fossa includes a small depression in the posteroinferior part of the epitympanic recess. It contains the short process of incus.
- Anterior wall
- Its lower part is formed by a thin plate of bone which separates the middle ear from the carotid canal.
- Its upper part is occupied by two openings. An upper opening leads into the canal for the tensor tympaní. The lower opening leads into the osseous part of the Eustachian tube. These two canals are visible from the apex side of the petrous temporal at petrosquamosal junction.
- The septum between the aforementioned canals runs on the medial wall and just above the fenestra vestibuli its posterior end curves laterally to form processus cochleariformis.
- Roof
Mastoid Antrum
- It is an air sinus in the petrous part of the temporal bone.
- It is well developed at birth and is almost of adult size.
- The mastoid antrum is a spherical sinus.
- In adults, the mastoid antrum has a capacity of about 1 ml.
- Aditus ad antrum is an opening in the upper part of the anterior wall of the mastoid antrum. It connects the antrum with the epitympanic recess of the middle ear.
- The roof of the antrum is formed by tegmen tympani.
- Posteriorly the antrum is closely related to the sigmoid sinus.
- The medial wall is related to the posterior semicircular canal.
- Anteroinferiorly the antrum is related to the canal for the facial nerve.
- The floor has multiple apertures which connect the mastoid antrum with mastoid air cells.
- The lateral wall of the antrum corresponds to the supramental triangle. This wall is 1 mm thick at birth and increases at a rate of 1 mm per year until it reaches the adult thickness of about 12.5 mm.
Mastoid Air Cells
- These are very small intercommunicating spaces in the temporal bone continuous
with mastoid antrum. - At birth neither mastoid air cells nor mastoid process are present. Only after birth do mastoid air cells grow out of the mastoid antrum into the mastoid process.
- The mastoid air cells are mainly seen in the mastoid process but may extend into the surrounding bones like petrous or squamous parts of the temporal bone or even zygomatic bone and the jugular process of the occipital bone.
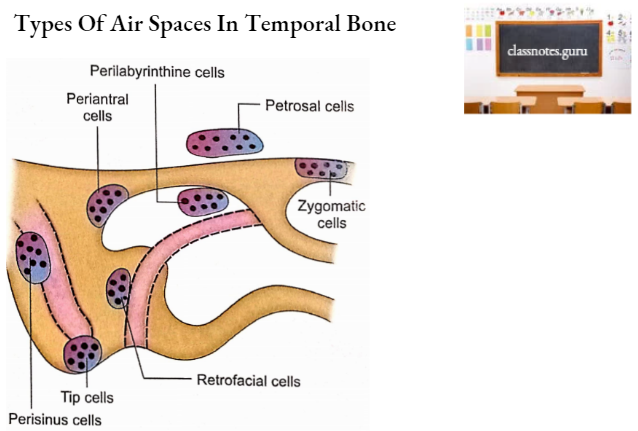
- Some common groups of air cells are as follows:
- Tip cells.
- Perisinus cells.
- Retrofacial cells.
- Periantral cells.
- Perilabyrinthine cells.
- Petrous cells.
- Zygomatic cells.
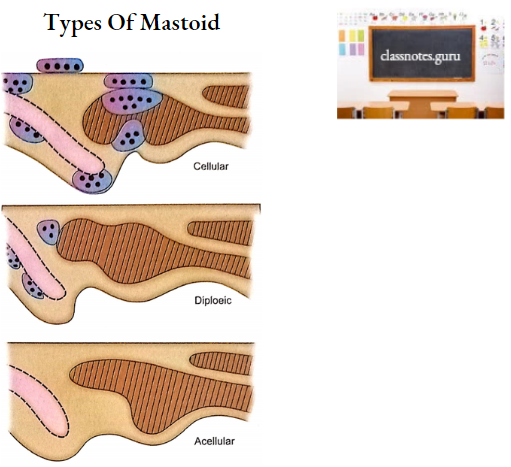
- Depending upon the pneumatization, the mastoid process may be of three types:
- Pneumatic or cellular.
- Sclerotic or acellular.
- Diploeic or mixed.
Bony Labyrinth (Osseous Labyrinth)
It consists of three parts, vestibule, semi-circular canals and cochlea.
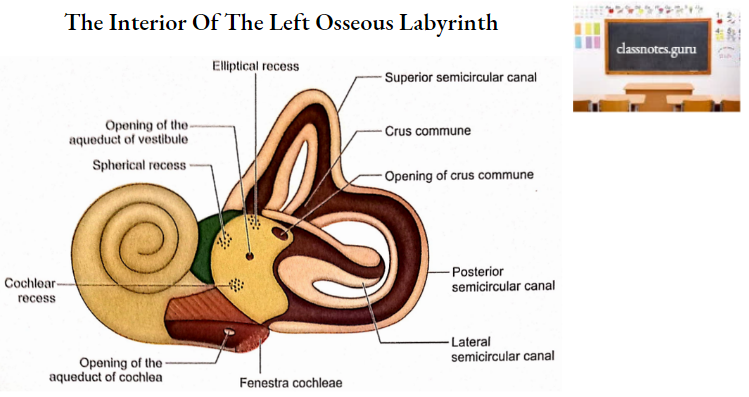
1. Vestibule
- It is the central part of the bony labyrinth.
- In its lateral wall, there is an opening of fenestra vestibuli (oval window) occupied by a foot plate of stapes in life.
- Its medial wall corresponds to the fundus of the internal acoustic meatus.
- The anterior part of the medial wall has a spherical recess for the saccule. This recess has multiple perforations which correspond to the openings in the inferior vestibular area of the fundus of the internal acoustic meatus.
- Posterosuperior to spherical recess is an elliptical recess which lodges the utricle. This recess also has a number of foramina which correspond to openings in the superior vestibular area of the fundus.
- Below the elliptical recess is the opening of the aqueduct of the vestibule which passes ductus endolymphaticus.
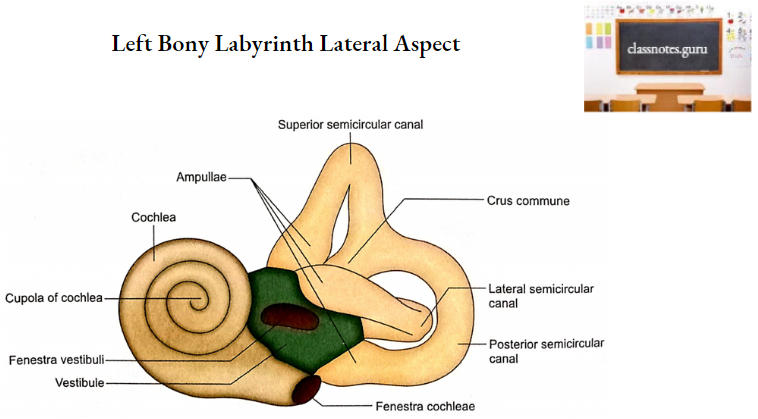
2. Semicircular Canals
- They lie posterosuperior to the vestibule.
- There are three semicircular canals.
- Anterior or superior.
- Lateral or horizontal.
- Posterior.
- Ipsilateral semicircular canals lie in three planes at right angles to each other.
- Each canal is about two-thirds of a circle.
- The superior semicircular canal is placed in a vertical plane perpendicular to the long axis of the petrous bone at about 45° with the sagittal plane.
- The posterior semicircular canal is placed in a vertical plane in the long axis of the petrous bone. This also makes an angle of 45° with the sagittal plane.
- The lateral semicircular canal makes an angle of 30° with the horizontal plane. This canal lies horizontally if the head is bent forward for 30°.
- One end of each canal is dilated called the ampulla.
- Both the ends of each canal open into the vestibule. Since non-ampullated ends of superior and posterior semicircular canals have a common opening in the vestibule, only five openings connect the three canals with the cavity of the vestibule.
3. Cochlea
- It is conical in shape and consists of two and three-quarter spiral turns of a tapering cylindrical canal.
- The axial bone around which the canal spirals is called modiolus.
- The basal turn of the cochlea produces promontory on the medial wall of the middle ear.
- From the modiolus a shelf of bone projects into the canal. Since the shelf follows the spiral path of the canal, this is called the spiral lamina.
- The spiral lamina forms a hook-like structure (called hamulus) at the apex of the modiolus.
- The basal turn of the cochlea shows two holes:
- The fenestra cochleae
- It is closed in life by a secondary tympanic membrane.
- The opening of the aqueduct of cochlea
- It leads downwards to reach the apex of the glossopharyngeal notch.
- The base of the modiolus is perforated by spirally arranged foramina. This area corresponds to the cochlear area of the fundus of the internal acoustic meatus.
Temporal Bones Ossification
- Temporal bone ossifies partly in cartilage and partly in membrane.
- Squamous and tympanic parts ossify in the membrane.
- The petromastoid part and the styloid process ossify in cartilage.
- Appearance of centres
- Squamous part
- The single centre appears near the root of the zygomatic process during the 8th week of intrauterine life.
- Petromastoid part
- As many as 14 centres may appear in the cartilaginous mass (otic capsule) around the developing internal ear during the 5th month of intrauterine life. These centres fuse by the 6th month of intrauterine life.
- Tympanic part
- Single centre appears during the 12th week of intrauterine life. At birth, a tympanic ring represents the tympanic part.
- Styloid process
- It develops from the cranial end of the 2nd arch cartilage. It ossifies from two centres. Centre for tympanohyal appears before birth and for stylohyal appears after birth.
- Fusion
- The squamous part fuses with the tympanic part just before birth.
- The petromastoid part fuses with the squamous part and tympanohyal during 1st year.
- Stylohyal fuses with the tympanohyal after puberty.
- Squamous part
Temporal Bones Applied Anatomy
- At birth, the tympanic cavity, tympanic membrane, mastoid antrum, ear ossicles and internal ear are all of adult size.
- At birth the mastoid process is absent and the facial nerve lies on the surface at its exit from the stylomastoid foramen. This makes the postauricular incision a risky procedure in newborns.
- A very long styloid process may lead to multiple complications and in such cases, it has to be removed by surgery.
- In the majority of people, the pneumatization of the temporal bone is adequate. In 20% of cases, the pneumatization may be arrested in childhood.
- This is easily pointed out in X-ray and is called sclerotic or acellular mastoid, a condition which is prone to inflammation.
- Infections of the middle ear (otitis media) invariably lead to infections of the mastoid antrum and mastoid air cells.
- The suprameatal triangle is clinically very important as it helps in localizing the mastoid antrum. The mastoid antrum is located 1.25 cm deep to the surface of this triangle.
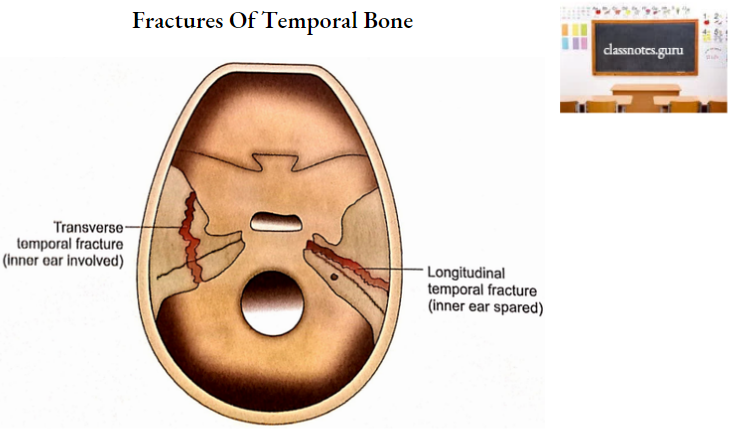
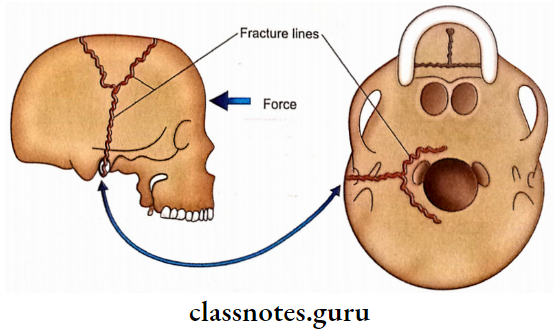
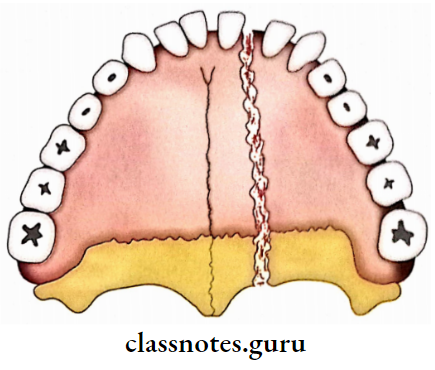
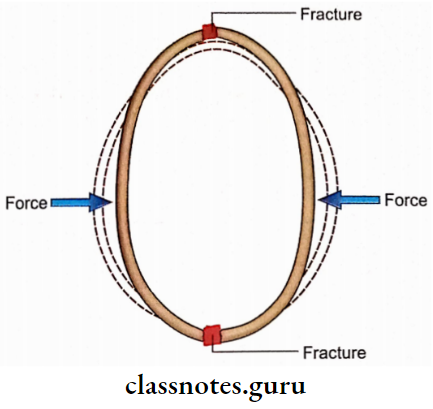
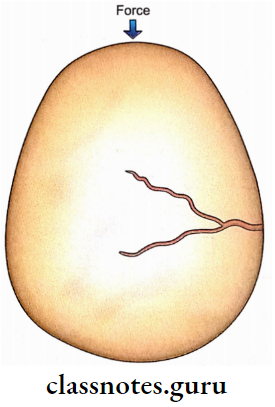
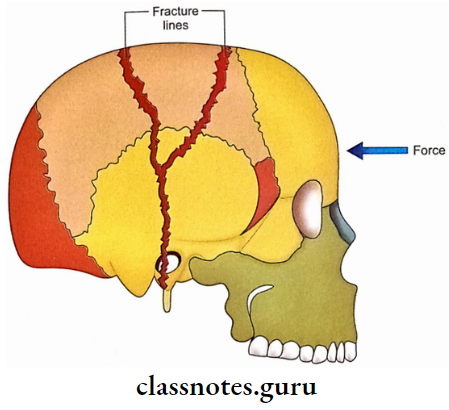
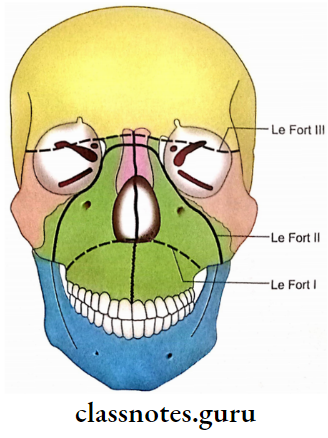
- Gross fractures of temporal bones are divided into longitudinal and transverse in relation to the long axis of the petrous temporal bone.
- Longitudinal fractures are common and are due to blows to the temporal or parietal areas. Transverse fractures are less common and are due to blows in the occipital region.
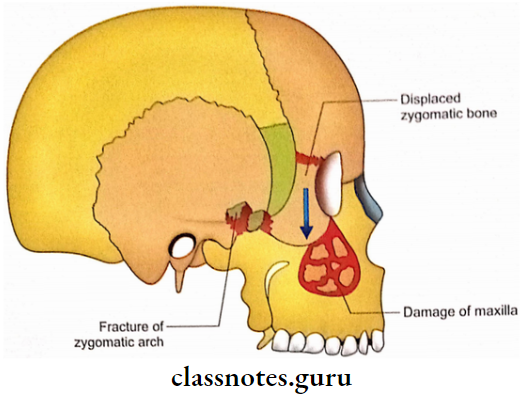
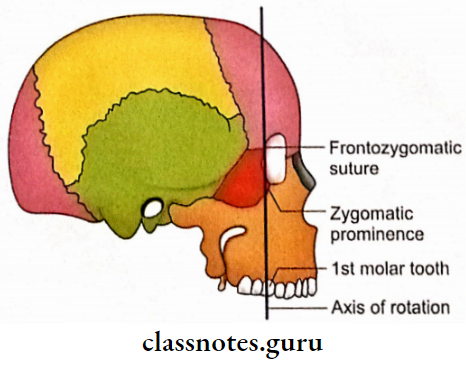
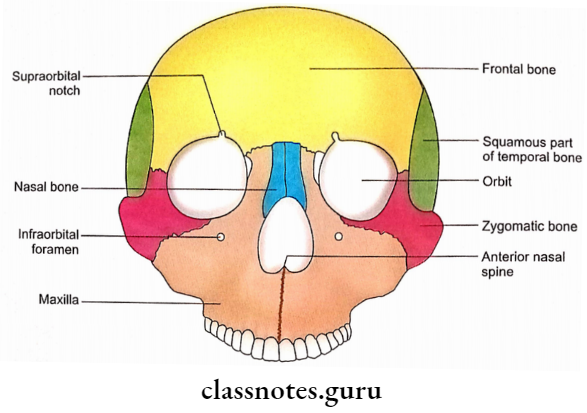
- Zygomatic arches form the prominences of the face and, therefore, are prone to facial injuries.
- Fractures of the zygomatic process of the temporal bone may involve the lateral wall of the orbit and injure the eye.
- The squamous part of the temporal bone contributes to the vault and, therefore, is prone to both fissured and depressed fractures. The petrous part contributes to the base of the skull and thus invariably shows a linear fracture.
- Fracture of the tegmen tympani might connect the subarachnoid space with the middle ear leading to CSF leakage into the middle ear.
- If the tympanic membrane is also damaged then the CSF will appear as a discharge through the external acoustic meatus. This condition is called CSF otorrhoea. The passage may also act as a portal for sepsis of the meninges and brain.
- Since the petrous part of the temporal bone is very strong, most fracture lines end here without making a tear in it.
- The indications of the fracture of the petrous part of the temporal bone are as follows:
- CSF otorrhoea.
- Tear of tympanic membrane.
- Collection of blood in the middle ear.
- Discolouration and oedema of the tissue over the mastoid process (Battle’s sign) is an indication of sigmoid sinus damage.
- Fracture of the petrous temporal may damage the facial nerve and result in facial paralysis.
- Involvement of vestibulocochlear nerve in petrous fracture will lead to hearing loss, vertigo and nystagmus.