Fixed Partial Denture (FPD)
Fixed Partial Denture Definitions
Fixed Partial Denture: It is defined as a partial denture that is cemented to natural teeth or roots which furnish the primary support to the prosthesis
Pontic: An artificial tooth on a fixed partial denture that replaces a missing tooth restores its functions and usually fills the space previously filled by a natural crown
Abutment: A tooth, a portion of a tooth, or that portion of an implant used for the support of a fixed or removable prosthesis
Retainer: It is defined as the part of a fixed partial denture that unites the abutment to the remainder of the restoration
Connector: The portion of a fixed partial denture that unites the retainer and pontic
Ceramic: It is an inorganic compound with nonmetallic properties typically consisting of oxygen and one or more metallic or semi-metallic elements that is formulated to produce the whole or part of ceramic-based dental prosthesis
Structural Durability: The ability of the restoration to withstand destruction due to external forces is known as “structural durability”
Read And Learn More: Prosthodontics Question And Answers
Fixed Partial Denture Important Notes
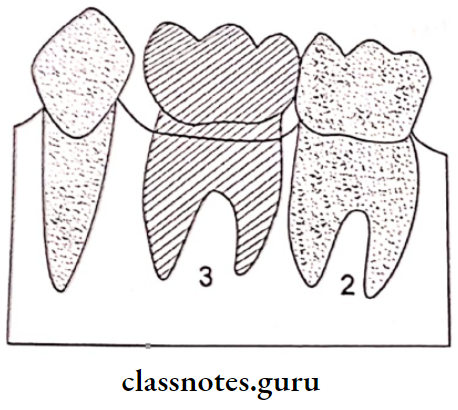
1. Ante’s Law:
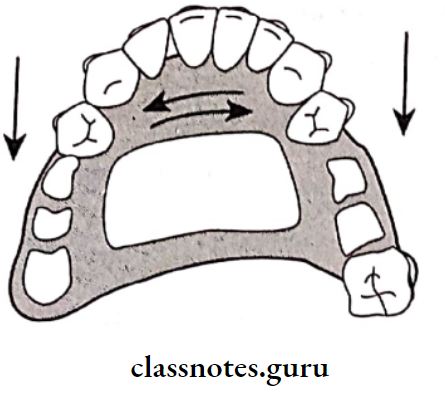
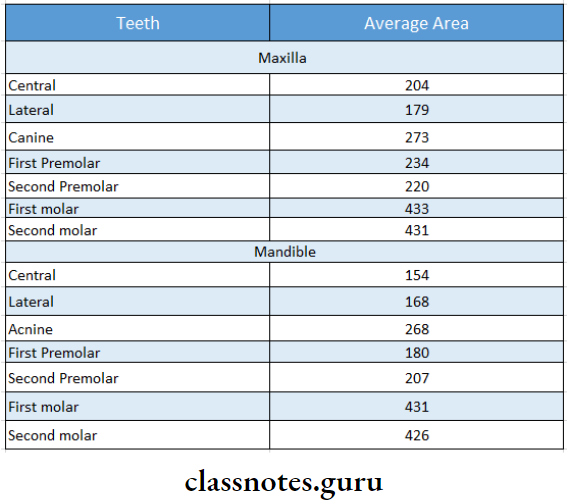
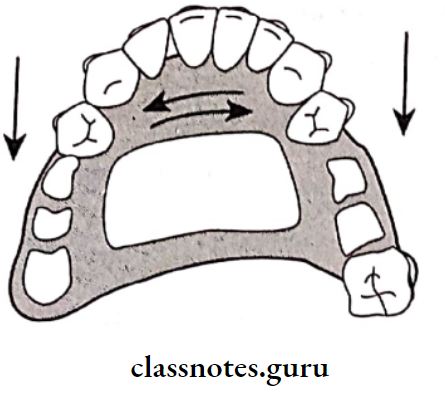
Ante’s Law states that “The combined pericemental area of all abutment teeth supporting a fixed partial denture should be equal to or greater in pericemental area than the tooth or teeth being replaced”
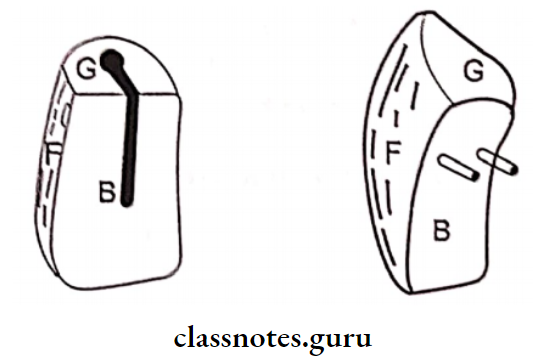
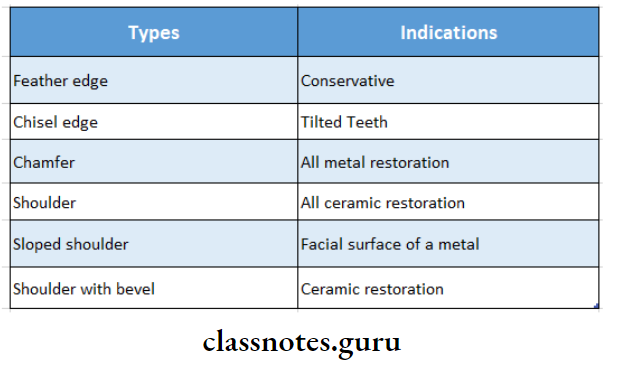
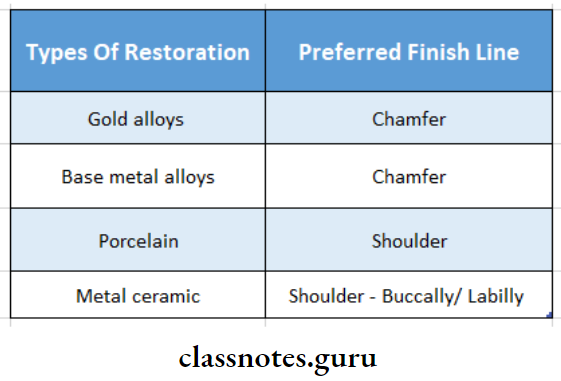
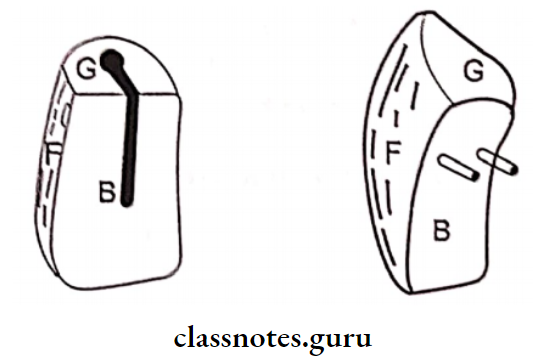
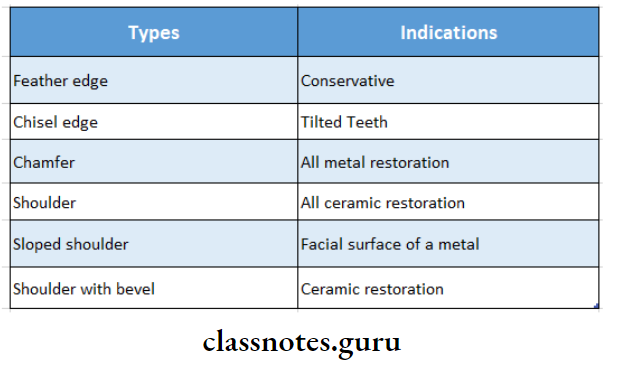
2. Finish Lines:
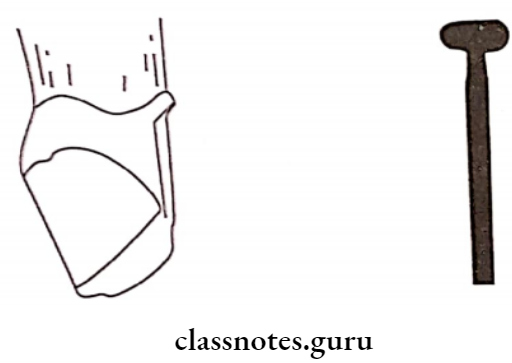
1. Shoulder Finish Line:
Indications Shoulder Finish line:
- All ceramic crown
- PFM crown
- Injectable porcelain
Fixed Partial Denture Definition
Advantages Of Shoulder Finish lines:
- Good crown contours
- Esthetics
- Less distortion
- Provides adequate bulk
Disadvantages Of Shoulder Finish lines:
- Least conservative
- Inferior marginal adaptation
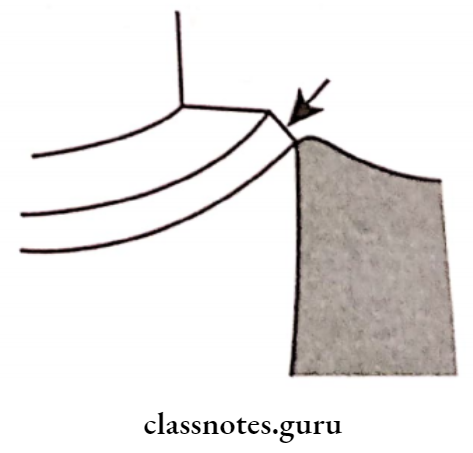
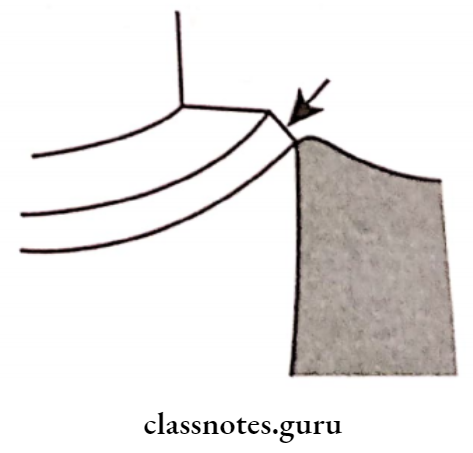
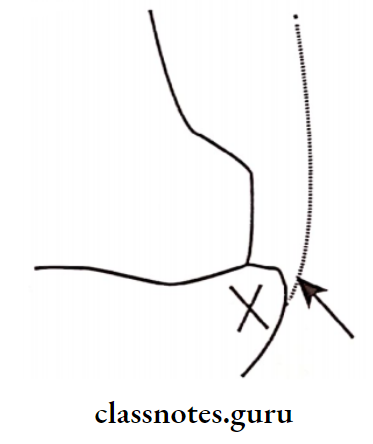
2. Shoulder With Bevel:
Indications Of Shoulder With Bevel:
- Proximal boxes of inlays and onlays Labial finish line of metal ceramics, Occlusal shoulder of onlays
Advantages Of Shoulder With Bevel:
- Superior marginal adaptation
- Resists distortion
- Facilitates removal of unsupported enamel rods
Disadvantages Of Shoulder With Bevel:
- Requires subgingival extension
- Detection of post-cementation caries is difficult
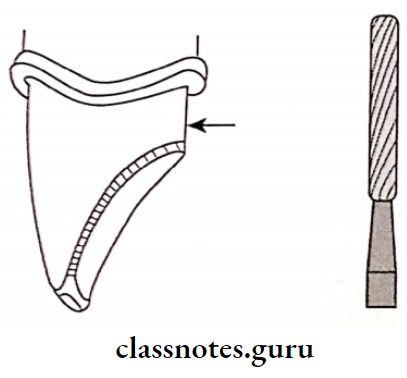
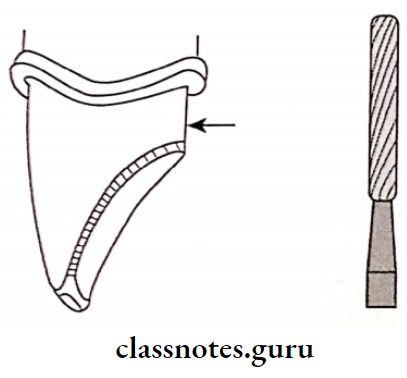
3. Chamfer:
Indications Of Chamfer:
- Cast metal restorations
- The lingual aspect of metal ceramics
- Advantages Of Chamfer:
- Conservative
- Good marginal adaptation
- Provides bulk

Disadvantages Of Chamfer :
- Improper fabrication may result in an unsupported tip
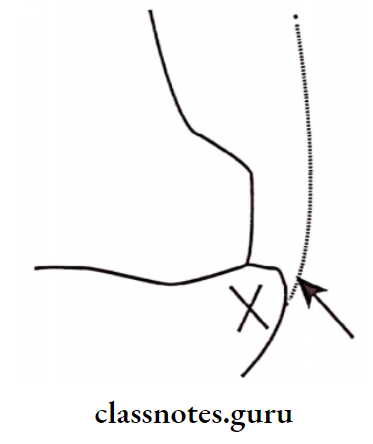
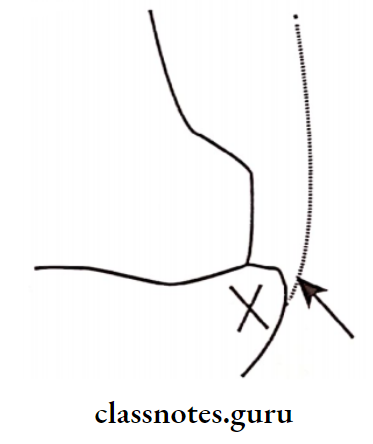
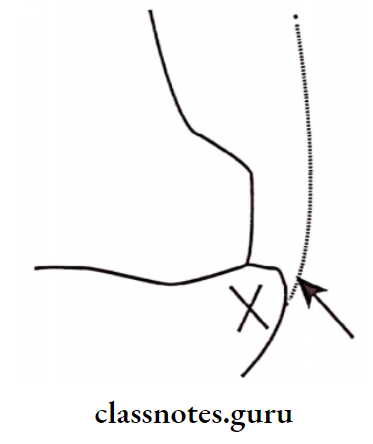
4. Knife Edge:
Indications Of Knife Edge:
- Young patients
- MOD onlay
- Inaccessible area
- Finish lines in cementum
Advantages Of Knife Edge:
- Conservative
- Ideal for marginal adaptation
What is a Fixed Partial Denture?
Disadvantages Of Knife Edge:
- Does not provide a distinct finish line
- Waxing, polishing and casting become critical
- Overcontoured restoration
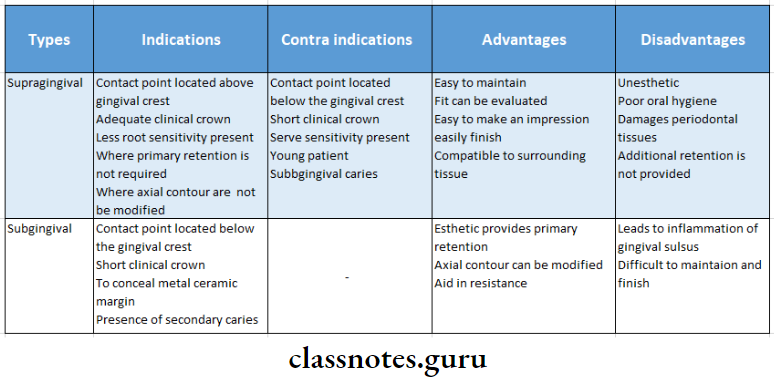
3. Gingival Finish Lines:
- Supragingival Finish Line:
- Better periodontal health
- Facilitates accurate impression-making
- Allows accurate assessment of the fit
- Subgingival Finish Line:
- Used when additional is needed
- Indicated in an anterior zone where esthetics is a prime consideration
- Used in cervical erosion and root hypersensitivity cases
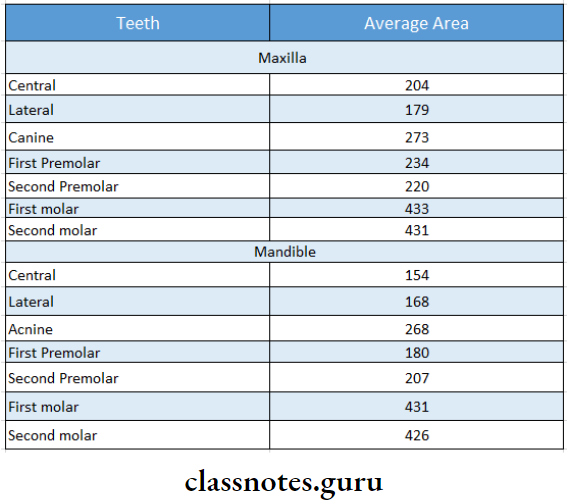
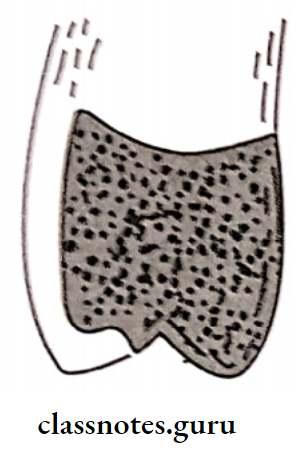
4. Surface Areas Of Different Tooth:
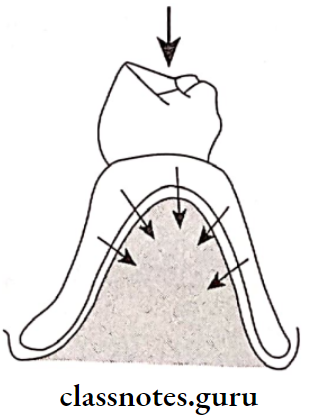
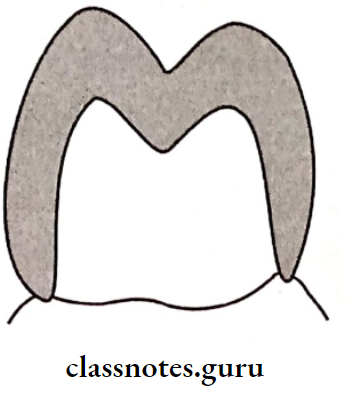
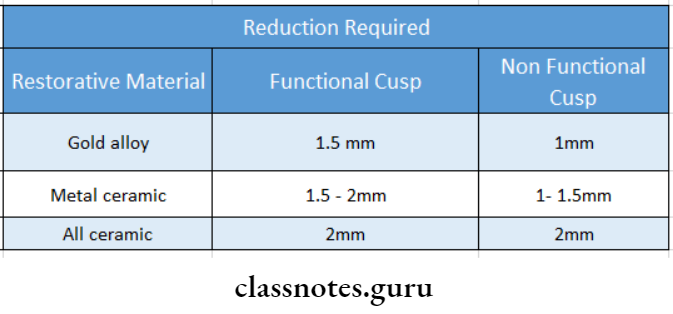
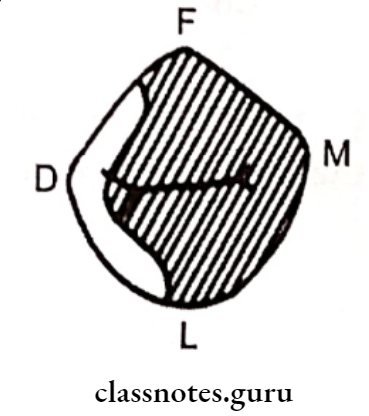
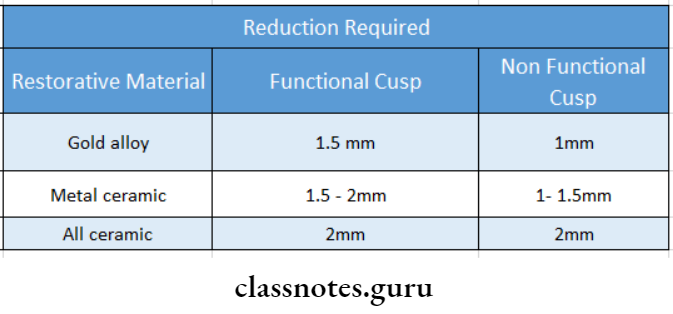
5. Structural Durability:
- Structural Durability is the resistance to deformity of a restoration
- Structural Durability is achieved by
- Reduction of 1.5 mm on the functional cusp and 1mm on the nonfunctional cusp
6. Principles Of Tooth Preparation:
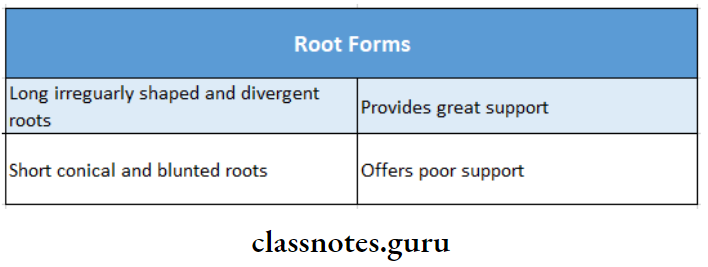
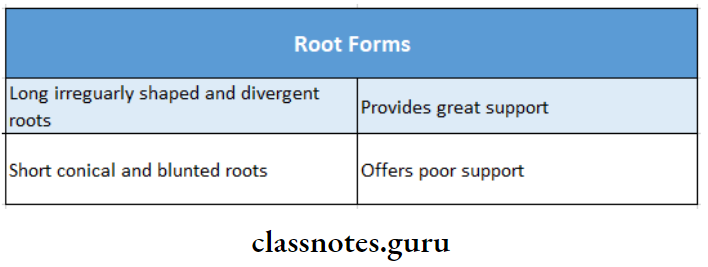
7. Root Forms:
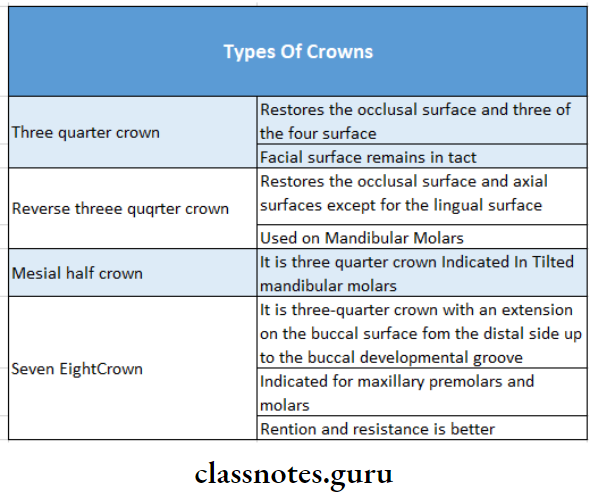
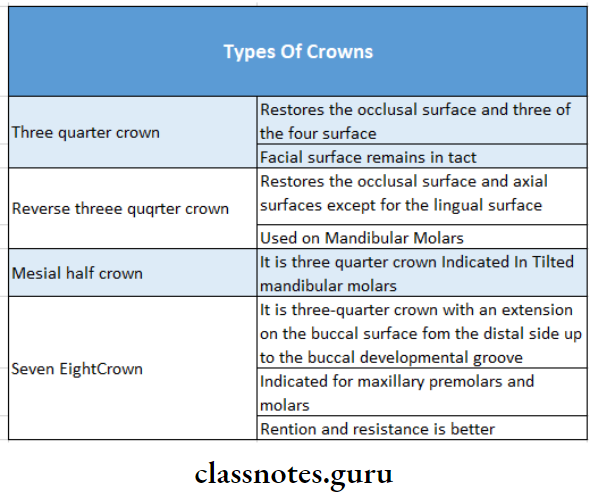
8. Types Of Crowns:
9. Indications Of Laminates:
- Diastema
- Stained restoration
- Fractures
- Malposition
- Attrition, erosion and abrasion
- Discolored teeth
Fixed Partial Denture Meaning
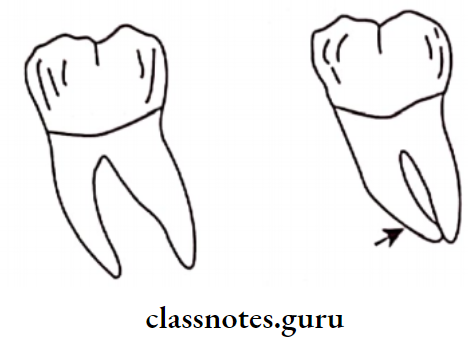
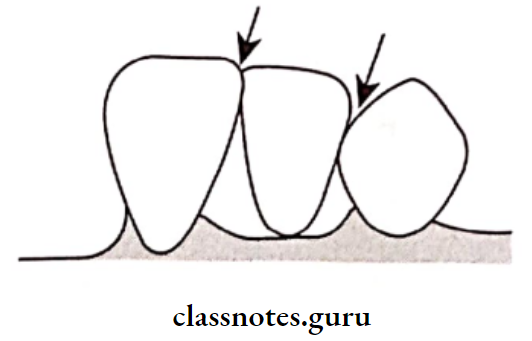
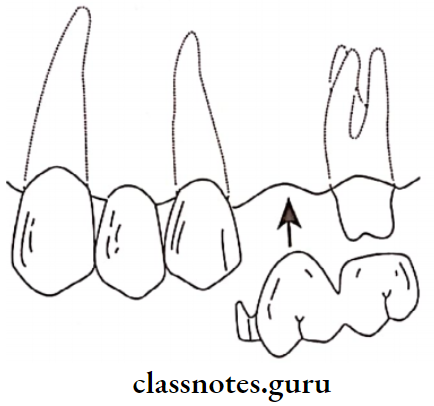
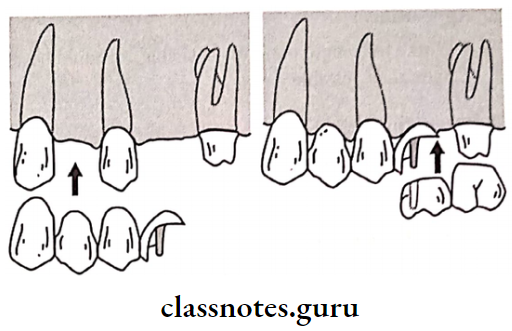
10. Types Of Abutment:
- Healthy or ideal abutment
- Cantilever abutment
- Tilted abutment
- Extensively damaged abutment
- Implant abutment
11. Disadvantages Of The telescopic Crown:
- Esthetically not acceptable
- Expensive
- Cannot be used in short crowns
12. Types Of Resin Bonded Retainers:
- Rochette bridges
- Maryland bridge
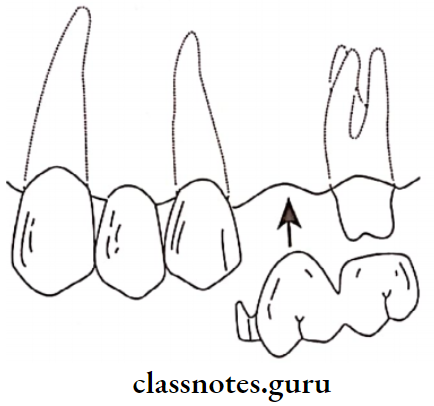
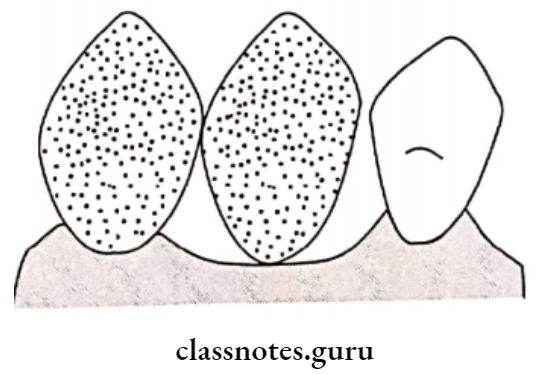
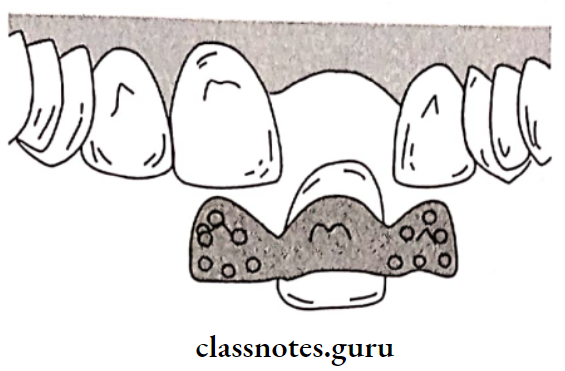
13. Classification Of Pontics:
- Based On Mucosal Contact
- With mucosal contact
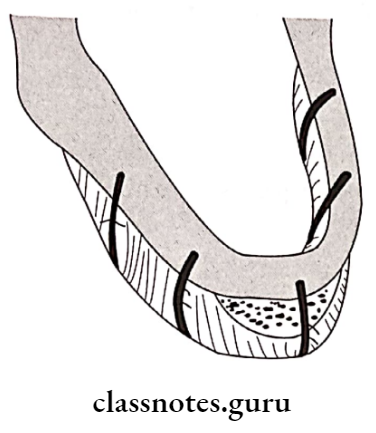
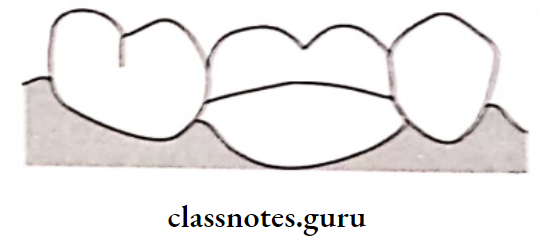
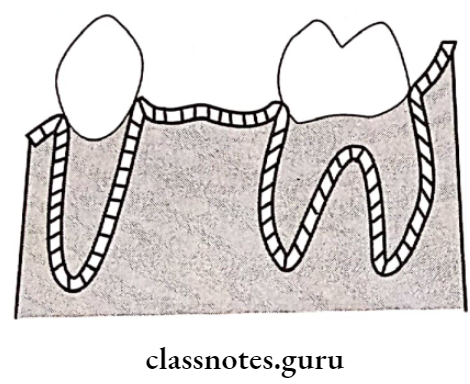
- Saddle pontic
- The concave gingival surface overlaps the ridge buccally and lingually
- The gingival surface will not have continuous contact with the ridge
- It is the least hygienic
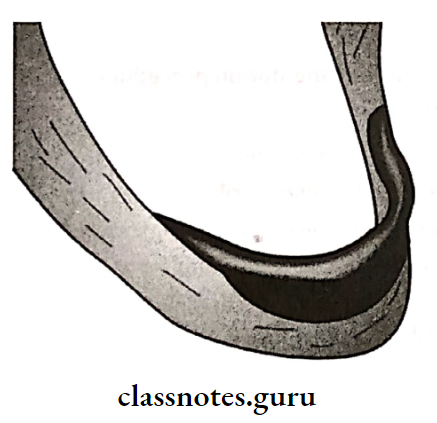
- Ridge Lap Pontic
- Evolved from saddle pontic
- Resembles natural tooth
- Satisfies esthetics
- Not hygienic
- Difficult to maintain
- Ovate pontic
- Without Mucosal Contact
- Bullet pontic
- Sanitary pontic
- Have zero tissue contact
- Easy to maintain
- Highly Unesthetic
- Recommended in mandibular posteriors
- Based On Type Of Material:
- Metal and porcelain veneered pontic
- Metal and resin veneered pontic
- All metal pontic
- All ceramic pontic
- Based On The Method Of Fabrication
- Custom made pontic
- Prefabricated pontic
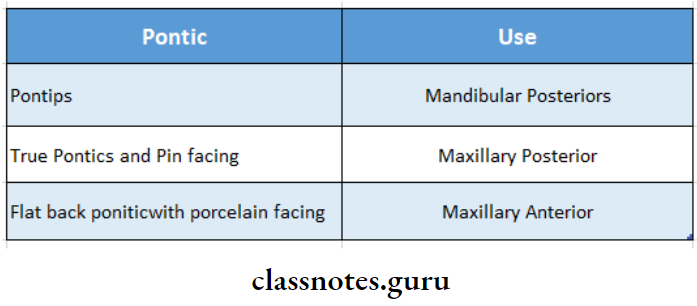
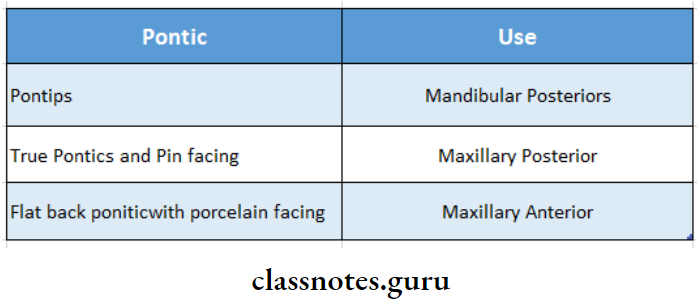
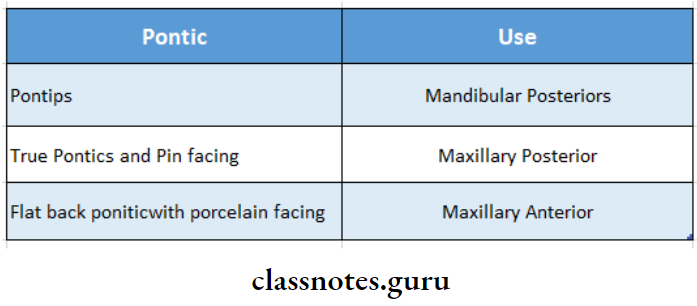
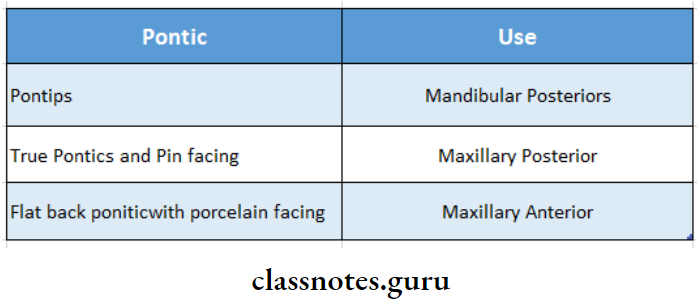
14. Preformed Pontics:
15. Classification Of Retainer:
- Based On Tooth Coverage
- Full veneer crowns
- Partial veneer crowns
- Conservative retainer
- Based On The Material Used
- Metal ceramic retainer
- All metal retainer
- All ceramic retainer
- All acrylic retainer
Fixed Partial Denture Long Essays
Question 1. Define and classify provisional restorations. Write in detail the various methods of fabricating a custom provisional restoration.
Answer:
Definition Of Provisional Restoration:
Provisional Restoration is a restoration that is established for the time being. until a permanent arrangement can be made
Classification Of Provisional Restoration:
- Based On The Method Of Fabrication
- Preformed: Anatomic form is prefabricated and readily available
- Custom Made: The anatomic form and shape of the tooth to be restored are fabricated by the dentist
- Based On Duration Of Use:
- Short-term used up to 2 weeks
- Long-term may be used for a few months
- Based On Material Used:
- Resins
- Metals
- Custom-made cast metal alloys
- Based On The Technique Of Fabrication:
- Direct technique – Restorations are fabricated intra-orally
- Indirect technique – Restoration is fabricated extraoral
- Direct/indirect technique
Custom Of Provisional Restoration:
The restoration is fabricated to reproduce the original contours of the tooth
- Technique Of Provisional Restoration:
- Tooth preparation is carried out
- An impression of the prepared tooth is made Cast is poured
- The prepared tooth over the cast is waxed up
- It is carved to reproduce the original contours
- Advantages Of Provisional Restoration:
- Minimum interference
- A wide variety of materials can be used
- Helpful in evaluating the adequacy of tooth reduction
- Disadvantages of Provisional Restoration:
- Additional lab procedure is involved
- Time-consuming
Question 2. Define FPD. Mention different types of retainer and criteria for selection of retainer. Add a note on the care of the prosthesis.
Or
Classify retainers used in fixed partial
Answer:
Fixed Partial Denture:
Fixed Partial Denture is defined as a partial denture that is cemented to natural teeth or roots that furnish the primary support to the prosthesis
Retainer Of Fixed Partial Denture:
Retainer Of Fixed Partial Denture is defined as the part of a fixed partial denture that unites the abutment to the remainder of the restoration
Classification Of Fixed Partial Denture:
- Based On Tooth Coverage:
- Full veneer crowns
- Partial veneer crowns
- Conservative retainer
- Based On Material Used:
- Metal ceramic retainer
- All metal retainer
- All ceramic retainer
- All acrylic retainer
Types of Fixed Partial Dentures
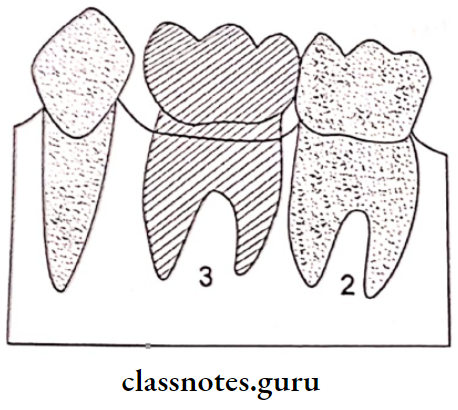
Question 3. Name parts of the bridge. Define and classify pontic. Add a note on the selection of pontic and its requirements and Pontic design and selection.
Answer:
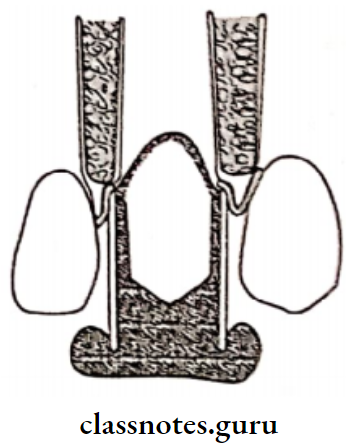
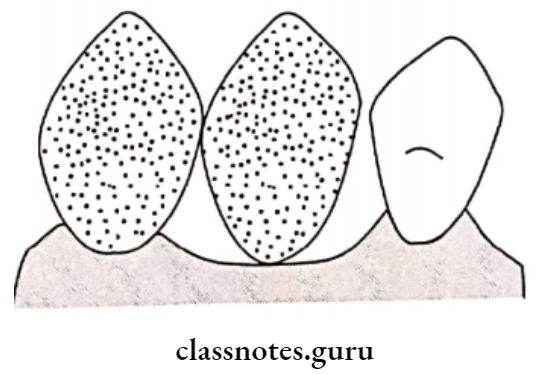
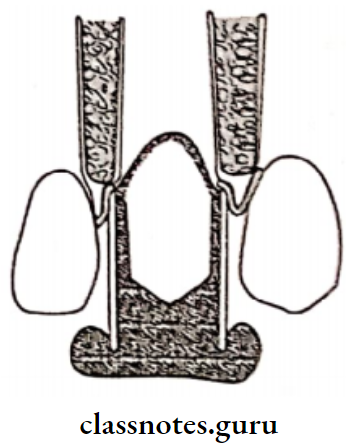
Parts Of Bridge:
- Retainer
- Pontic
- Connectors
Pontic Definition:
“An artificial tooth on a fixed partial denture that replaces a missing tooth restores its functions and usually fills the space previously filled by a natural crown”
Classification Of Pontic: Based On Mucosal Contact:
- With mucosal contact:
- Saddle pontic
- Ridge lap pontic
- Ovate pontic
- Without mucosal contact:
- Bullet pontic
- Sanitary pontic
- Based on the type of material:
- Metal and porcelain veneered pontic
- Metal and resin veneered pontic
- All metal pontic
- All ceramic pontic
- Based on the method of fabrication:
- Custom made pontic
- Prefabricated pontic
Requirements of Pontic:
- Pontic should restore the function of the tooth it replaces
- Pontic should provide good aesthetics
- Pontic should be comfortable for the patient
- Pontic should be biocompatible
- Pontic should have the color stability
- Pontic should permit effective oral hygiene
- Pontic should preserve underlying mucosa and bone
- Pontic should not overload the abutment
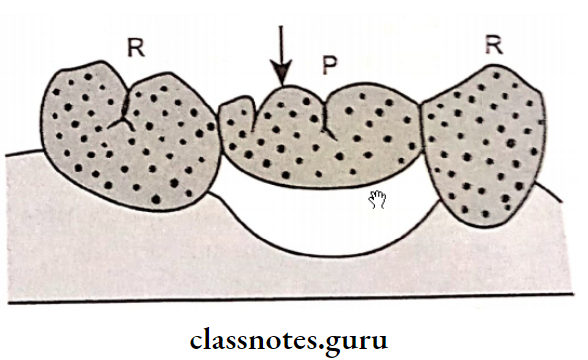
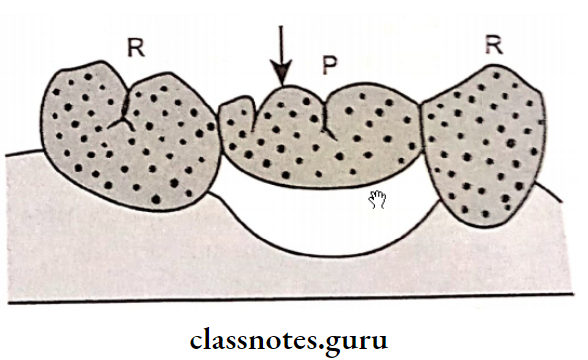
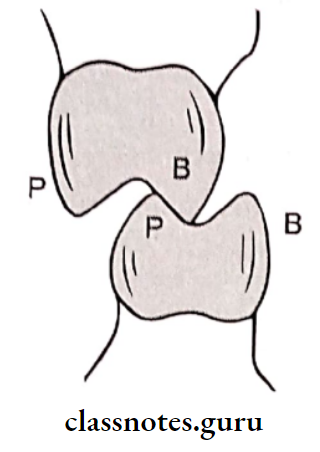
- Pontic – (P)
- Retainer – (R)
Pontic Selection: Various factors are considered for pontic selection. They are
- Cleanability:
- All surfaces of pontic should be made as cleansable as possible
- All surfaces should be smooth and highly polished
- It should not contain any junction between materials The embrasure and connector should be smooth and cleanable
- Appearance:
- Where full length of pontic is visible, it should be as natural as possible
- Strength:
- All pontic should be designed to withstand occlusal forces
- Age Of The Patient:
- Younger patients need pontic made up of stronger material like nickel-chromium.
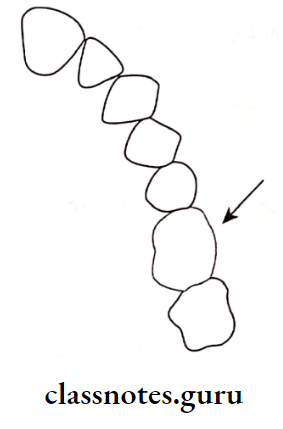
- Edentulous Space:
- The space created due to the loss of a tooth is usually sufficient for the fabrication of good pontic But due to long period of edentulousness teeth tend to be tilted or drifted
- In such cases the pontic should be modified
- Other Factors:
- DMFT score of the individual
- Oral hygiene status
- Periodontal support present
- Arch relation
- Skeletal relation
- Vitality of abutment
Question 4. Discuss various types of pontics in fixed partial dentures.
Answer:
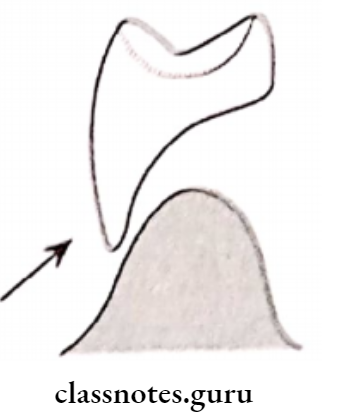
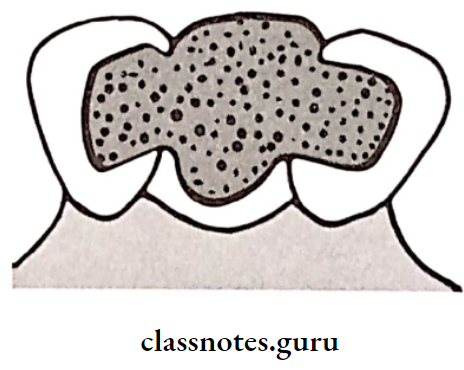
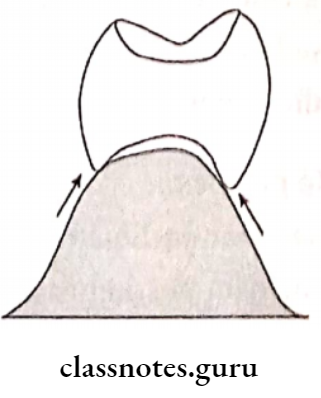
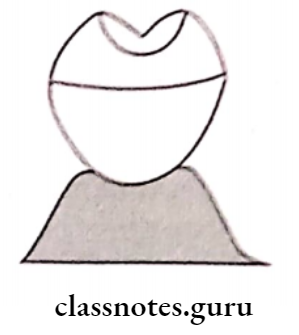
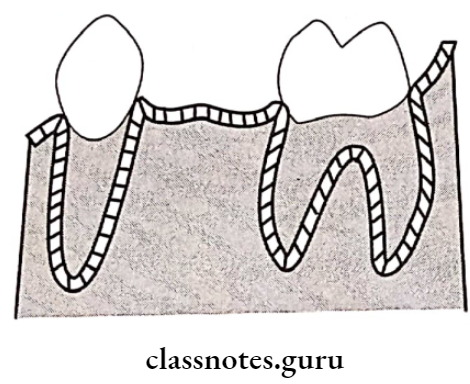
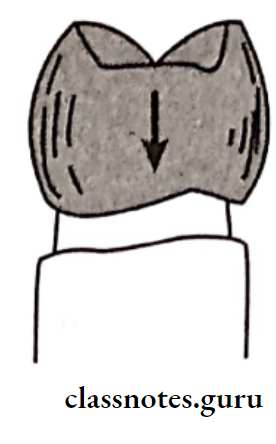
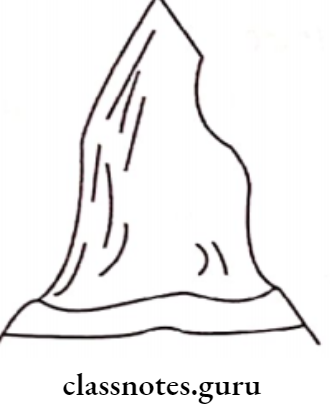
1. Saddle Pontic:
Saddle Pontic is a pontic that has a concave gingival surface overlapping the ridge buccally and lingually
Saddle Pontic Disadvantage:
- Saddle Pontic is difficult to maintain
- Saddle Pontic leads to food accumulation
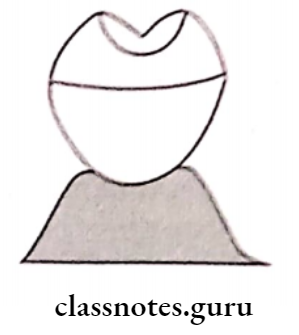
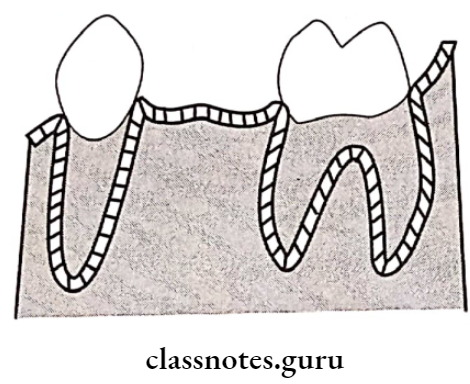
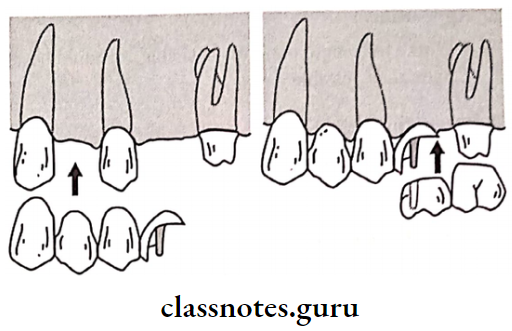
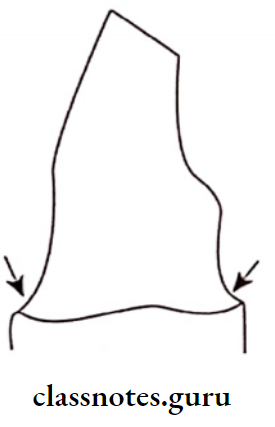
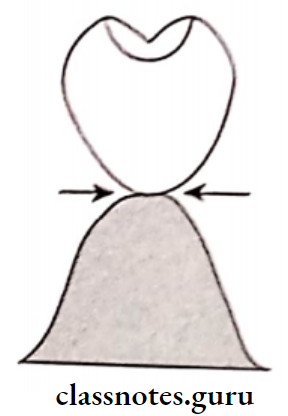
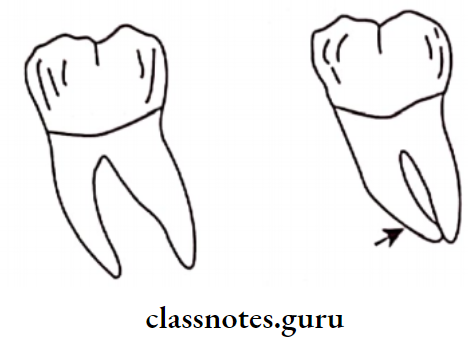
2. Ridge Lap Pontics:
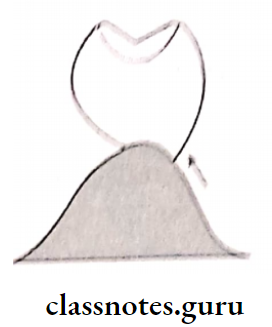
- Ridge Lap Pontics closely adapts to the ridge
- Ridge Lap Pontics resembles a natural tooth
- Ridge Lap Pontics leads to soft tissue inflammation
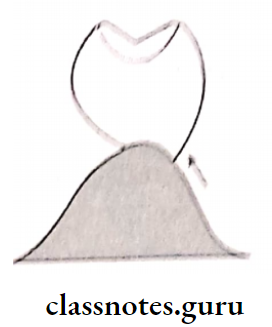
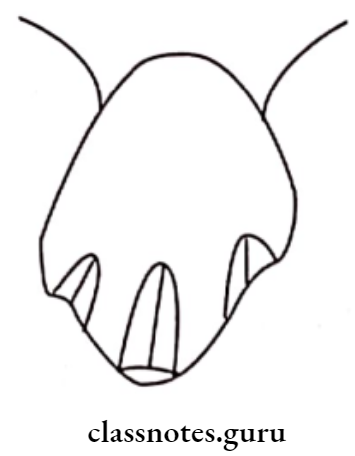
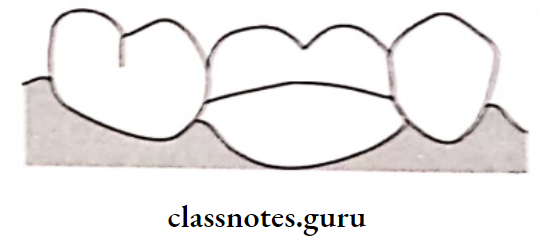
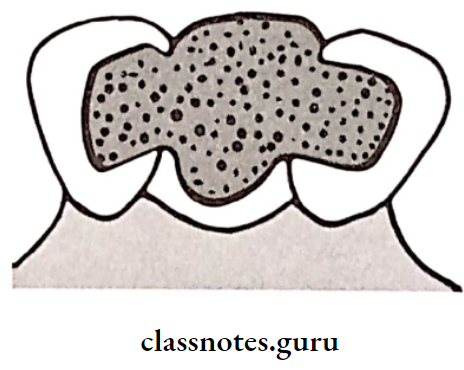
3. Modified Ridge Lap Pontic:
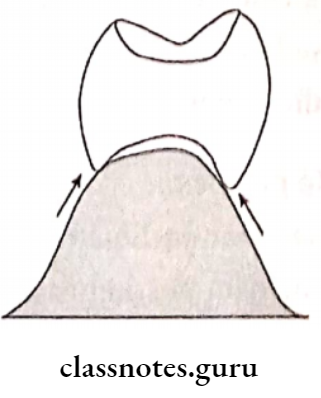
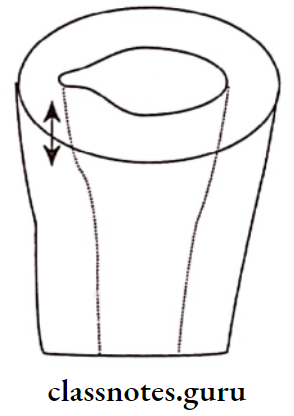
- In it, the tissue contact occurs only over the buccal surface of the ridge crest
- It has slight bucco lingual concavity and mesiodens tal convexity
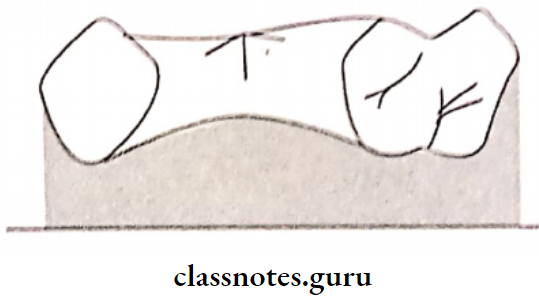
- The tissue surface of the pontic has a “T” shaped contact
- Vertical arm contacts crest of the ridge and the horizontal arm contacts the buccal surface

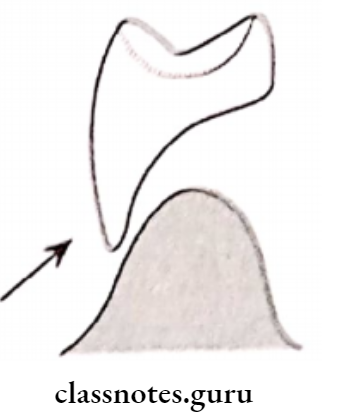
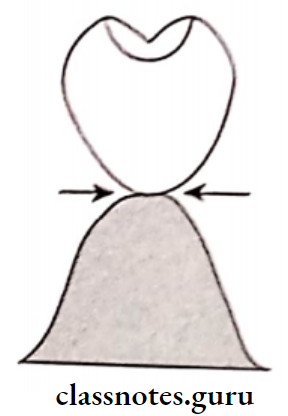
- Ovate Pontic:
- Ovate Pontic Indications:
- Defective ridge
- Broad and flat ridges
- The cervical end of the pontic extends into the ridge defect
- It is more esthetic
- Bullet Shaped: It has a convex tissue surface contacting at one single point
- Bullet Shaped Advantage: It is easy to clean and maintain
- Bullet Shaped Disadvantage: Poor esthetics
- Bullet Shaped Indication: Mandibular posteriors
- Spheroidal Pontic: It has tissue contact at the ridge
- Spheroidal Pontic Indications: Reduced inter-arch space
- Spheroidal Pontic Advantages: It develops adequate exaggerated occlusal-gingival dimension
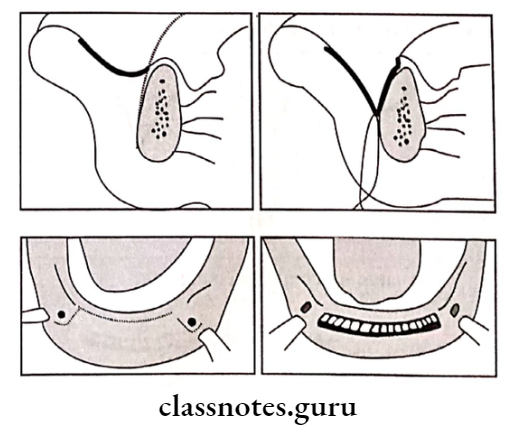
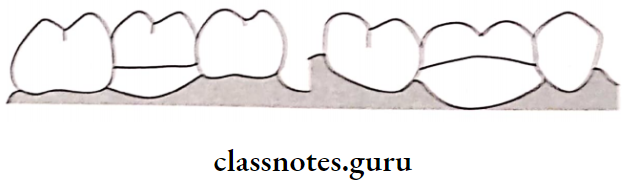
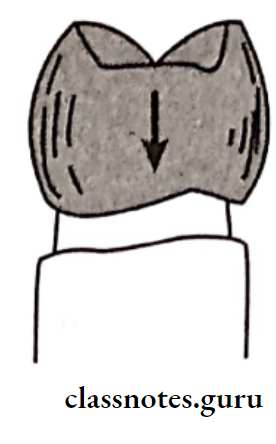
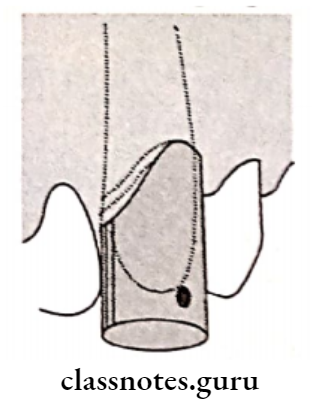
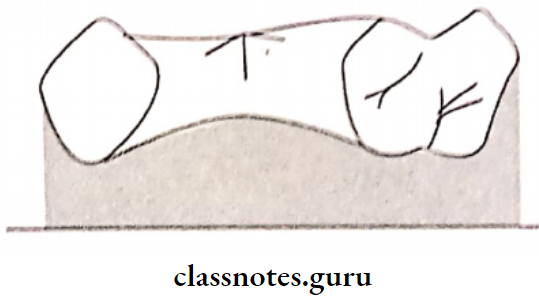
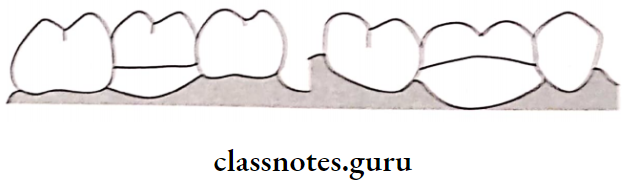
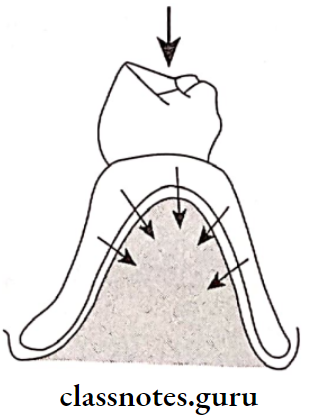
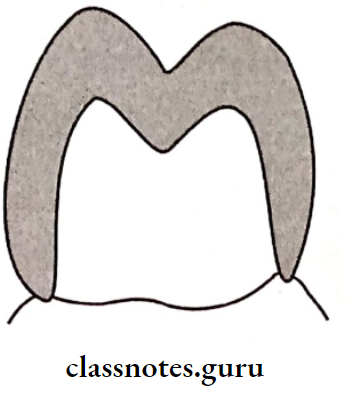
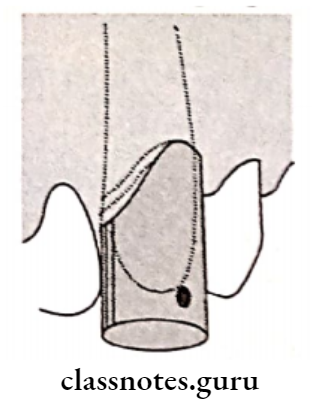
- Sanitary Pontic Or Hygienic Ponitic:
- They do not have any mucosal contact
- Sanitary Pontic Or Hygienic Ponitic is easy to maintain
- They are used only for the posterior due to poor esthetics
- Sanitary Pontic Or Hygienic Ponitic should have adequate tissue clearance by placing it 3 mm high occlusal-gingivally
Sanitary Pontic Or Hygienic Ponitic Common Designs Are Or Types:
- Bar Sanitary Pantic:
- Bar Sanitary Pantic has a flat gingival surface
- Bar Sanitary Pantic has sufficient gingival clearance to allow maintenance of it
Conventional Sanitary Or Fish Belly Pontic
- Sanitary Pontic has a convex gingival surface, both buccolingually and mesiodistally
- Sanitary Pontic resembles the belly of a fish
- Sanitary Pontic decreases the strength of the prosthesis by decreasing the size of the connector
Modified Sanitary Pontic:
- The gingival surface is concave mesiodistally and convex buccolingually
- Due to this, the arch shape obtained increases the size of the connector
- Metal Ceramic Pontics:
- Due to the use of ceramic, it gives an esthetic appearance
- Metal Ceramic Pontics is biocompatible
- Metal Ceramic Pontics fabrication is technique-sensitive
- Resin Veneered Pontic:
- Resin Veneered Pontic includes the straightforward procedure for fabrication
- Resin Veneered Pontic has poor esthetics
- Staining at the resin metal interface occurs
- All Metal Pontic:
- All Metal Pontic has good strength but poor aesthetics
- Thus it is used for mandibular molars
- Its use is indicated in bruxers
- Custom-Made Pontics:
- It is customized for each patient
- They offer superior aesthetics and flexibility
- A wax pattern is prepared and cast to prepare it
- Pre-Fabricated Pontic:
- Pre-fabricated Pontic are available as porcelain pontics
- These are adjusted according to the individual requirement
- Finally, they are reglazed and fit into a metal
- backing which is a custom-fabricated portion of the poetics
- The metal backing is designed to accept the prefabricated facing
Question 5. Define abutment. Explain the criteria for the selection of teeth for a fixed partial denture abutment.
Answer:
Definition Of Abutment:
“A tooth, a portion of a tooth or that portion of an implant used for the support of a fixed or removable prosthesis”
Abutment Selection Criteria:
- Location Of The Tooth:
- Teeth adjacent to the edentulous spaces are selected
- Condition Of The Tooth:
- Teeth should ideally be caries-free
- However, if the teeth are grossly decayed, it should be such that it can be restored with a full veneer crown
- Vital teeth are preferred
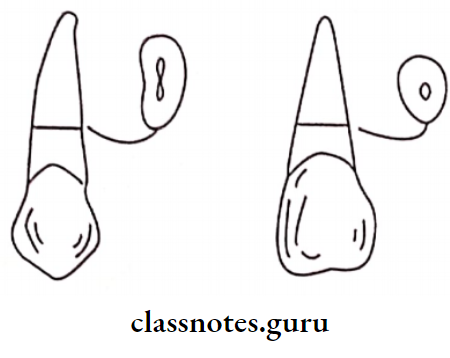
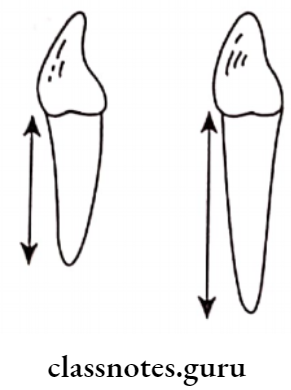
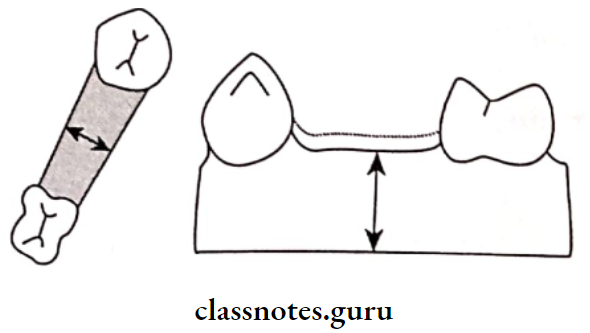
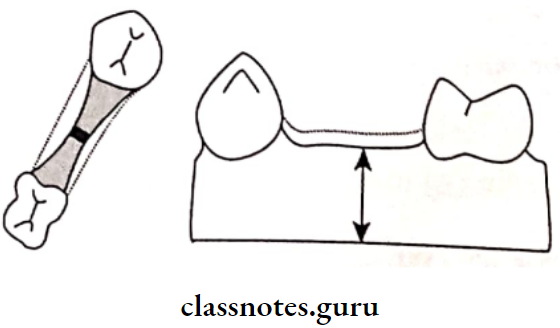
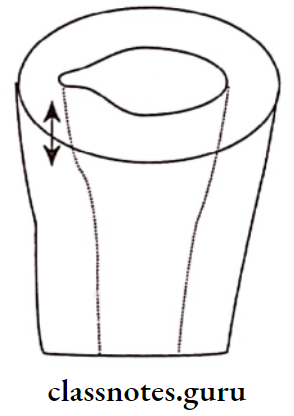
- Root Configuration/Shape:
- The root shape determines the ability of the abutment to withstand the masticatory load
- Some configurations are preferred for the abutment. They are
- Wide labiolingual roots
- Irregular curvature of roots
- Longer roots
- Conical roots
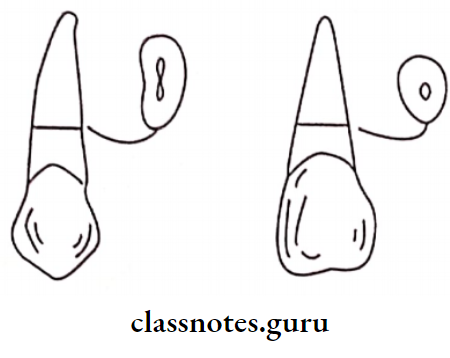
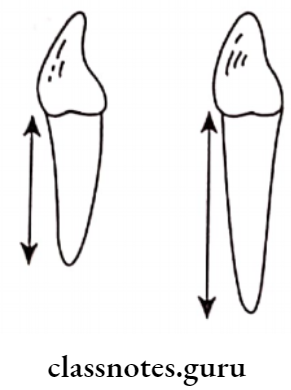
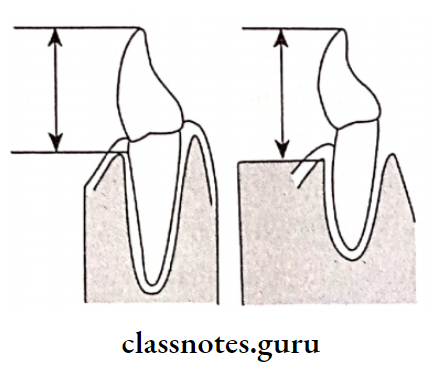
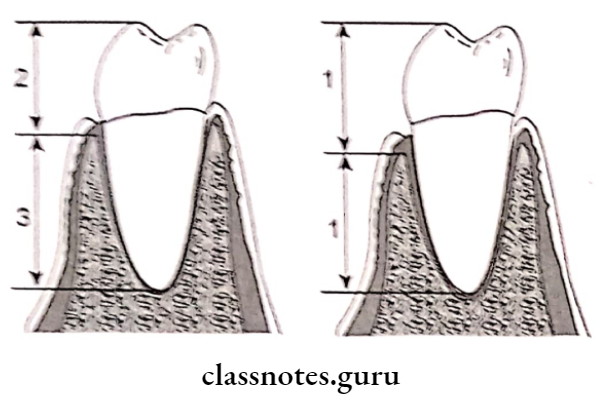
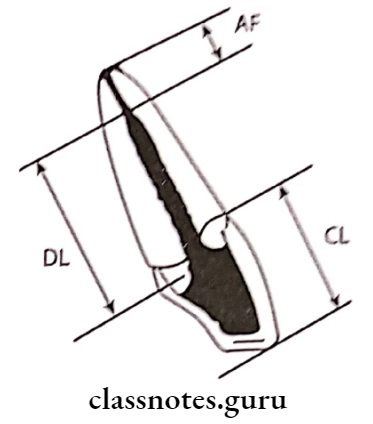
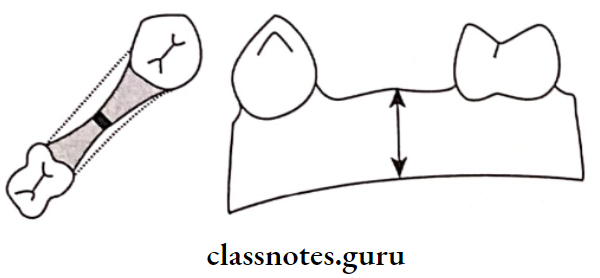
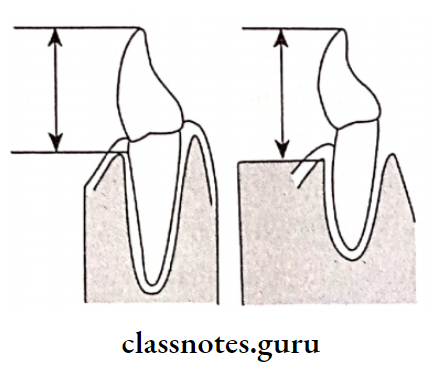
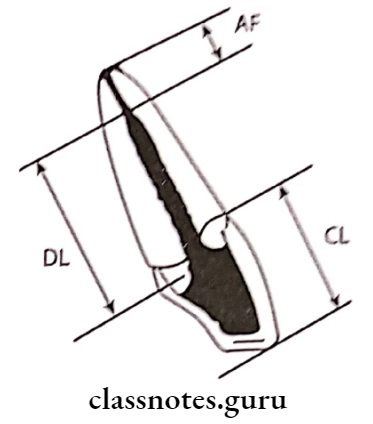
- Crown Root shape:
- Length of the crown
- It is the length of the tooth structure above the alveolar crest
- Length of the root
- It is the total length of the root
- The ratio of the above two gives the crown root ratio
- It is one of the important criteria for abutment selection
Abutment Ratio:
- 1:1 – Acceptable
- >1 – Unacceptable
- 2:3 – Ideal
1. Root Support:
- The tooth is supported if there is sufficient surrounding alveolar bone
- The alveolar should be
- Healthy
- Have normal trabecular pattern
- Have normal architecture
- If there is the presence of bone loss or bony defect, the abutment selected will lead to failure of the prosthesis

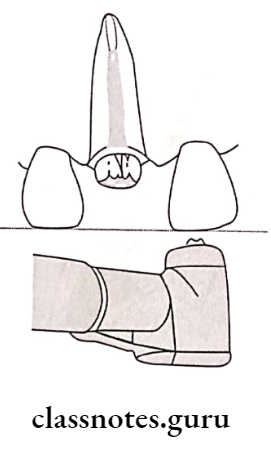
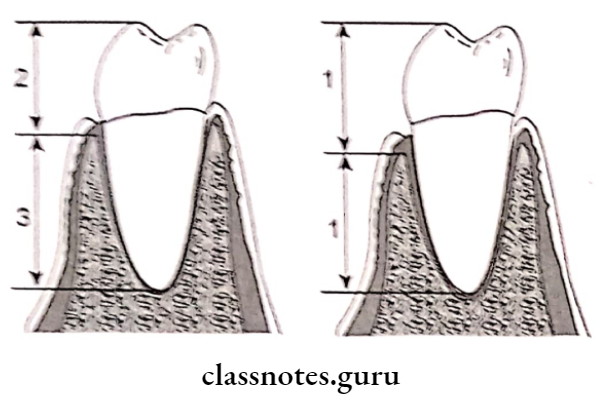
2. Periodontal Ligament Area:
- An increase in bone support results in an increase in the periodontal ligament area
- Periodontal Ligament Area is used to determine the potency of an abutment Periodontal diseased teeth are unsuitable to be used as an abutment
Ante’s Law:
- Ante’s Law states that “The combined pericemental area of all abutment teeth supporting a fixed partial denture should be equal to or greater in pericentral area than the tooth or teeth being replaced”
- The pericemental area is calculated
- If it is inadequate, then there is the addition of a secondary abutment
Assessment Of Pulpal Health:
- Unrestored abutments are preferred
- However, if the abutment tooth has a carious lesion with pulpal involvement then root canal treatment is advised.
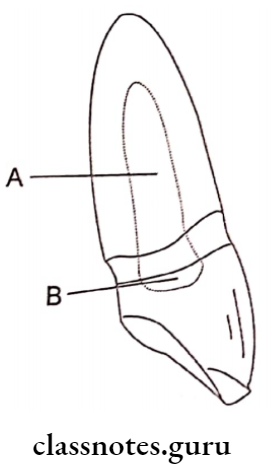
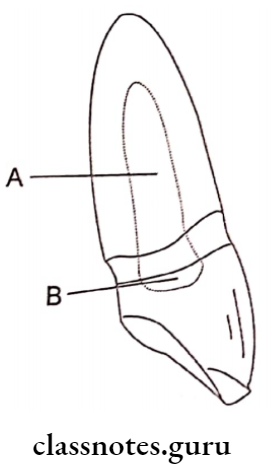
Question 6. Enumerate steps in preparation of full ceramic crown for 21. Add a note on the advantages and disadvantages of the same.
Answer:
Tooth Preparation:
- Step 1: Labial reduction
- Depth orientation grooves are prepared using a flat-end tapered diamond
- The grooves should be 1.2 – 1.4 mm deep on the labial surface and 2 mm on the incisal surface
- Two sets of grooves are made
- The first is parallel to the gingival third
- The second is parallel to incisal 2/3rd
- This provides a better aesthetic
- Next, the tooth structure between the grooves is removed
- The facial reduction should extend around the facio-proximal line angles
- Step 2: Incisal Reduction
- Depth orientation grooves are made across the incisal edge
- They are about 2.0 mm deep
- The tooth structure between the grooves is removed
- The incisal reduction should be perpendicular to the plane of the incisal half of the labial reduction
- Step 3: Lingual Reduction
- Cingulum should be reduced
- The reduction of the lingual axial surface is carried out with a flat-end tapered diamond
- The lingual wall should be parallel to the gingival portion of the labial wall.
- Step 4: Proximal Reduction
- A radial shoulder of at least 1.0 mm wide is made It should be in uniform contour along the line angles of the restoration
- The axial walls are smoothened with a radial fissure bur
- A biangle chisel is used to smoothen the shoulder
Advantages Of Tooth Preparation:
- Superior esthetics
- Good translucency
- Good biocompatibility
- Good selection of shade
Disadvantages of Tooth Preparation:
- Reduces strength of the restoration
- Less conservative
- An extensively damaged tooth cannot be restored
- Cannot be used as retainers
- This can lead to periodontal failure
- Wear on the functional surfaces of opposing natural teeth
Question 7. Describe the advantages, disadvantages, indications, and contraindications of FPD.
Answer:
Advantages Of Fixed Partial Denture:
- Movements for a fixed partial denture are less compared to a removable partial denture
- Psychologically better accepted than a removable partial denture
- Acts as a splint
- Less lateral forces are transmitted to the abutment
- Can use a weak abutment
- Aesthetically better
- Better functioning of the prosthesis
- Causes less bone resorption
Disadvantages Of Fixed Partial Denture:
- Fixed Partial Dentures can weaken, a strong abutment
- Fixed Partial Denture is an irreversible treatment
- Patient may not agree to carry out procedure over sound teeth
- Technique sensitive
- Fixed Partial Dentures can cause periodontal problems, if over-contoured
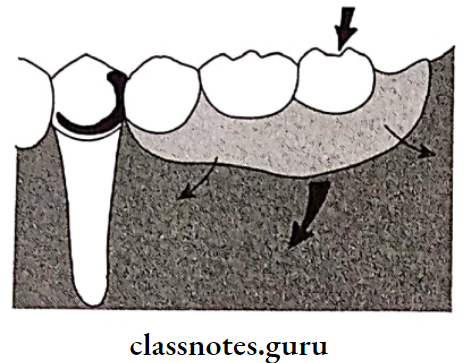
Indications Of Fixed Partial Denture
- Length Of The Edentulous Arch:
- Short-span edentulous arches are preferred for FPD
- This is due to the reason that a long-span FPD transfers excessive load to the abutment and also tends to flex to a greater extent
- To avoid it, short-span edentulous arches are preferred
- Condition Of The Abutment Tooth:
- FPD is used if there is the presence of a posterior tooth for support
- Such a tooth should have
- Ideal crown root ratio for support
- Adequate thickness of enamel and dentin for reduction
- Adequate bone support
- Absence of periodontal disease
- Proper gingival contour
- Condition Of The Residual Ridge:
- The contour of the ridge and texture of the soft tissues should be observed
- A smooth rounded ridge is best for the placement of FPD
- Patient’s Preference:
- The patient may not desire to frequently remove and insert the denture
- If in these patients removable partial denture is given, they may not maintain it
- This may further lead to post-insertion problems To avoid this, FPD is preferred
- Mentally Compromised And Physically Handicapped Patients:
- Such patients fail to maintain the removable prosthesis
- This may lead to soft tissue irritation
- To avoid it, FPD are preferred
Contraindications Of The Abutment Tooth:
- Excessive Bone Loss:
- When there is trauma or excessive residual ridge resorption, there is the absence of required support for the prosthesis.
- In such cases, it is difficult to place the artificial teeth of a fixed partial denture in an ideal buccolingual position
- Age Of The Patient:
- Patients under the age of 17 years, have large dental pulps
- They lack sufficient clinical crown height for tooth reduction
- Thus, a fixed partial denture is contraindicated
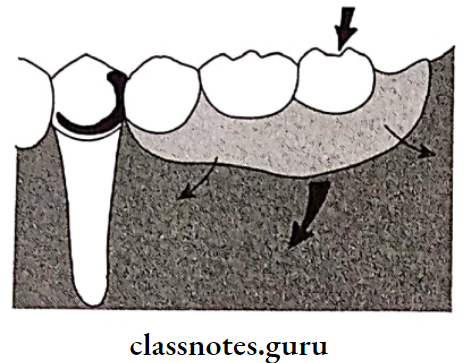
- Long Span Edentulous Space:
- In such cases, the entire occlusal load is directed to the abutment which in turn leads to damage to the abutment
- Periodontally Weak Teeth:
- The periodontal membrane is the structure that transfers all the load from the teeth to the underlying bone
- A periodontally weak tooth will not successfully transmit the forces to the alveolar bone
- Bilateral Edentulous Spaces, Which Require Cross-Arch Stabilization:
- When the remaining teeth have to be stabilized against lateral and anterior-posterior forces.
- A fixed partial denture is contraindicated as it will provide only anteroposterior stabilization and limited lateral or buccolingual stabilization.
- Congenitally Malformed Teeth:
- Such teeth do not have adequate tooth structure to offer support
- Mentally Sensitive Patients:
- Such patients are uncooperative
- Mentally Sensitive Patients do not allow tedious procedures to be carried out
- Medically Compromised Patients:
- Such patients may lead to certain post-treatment complications
- Very Old Patients:
- Such patients are contra-indicated due to
- The presence of generalized attrition leads to reduction in clinical crown height
- Presence of large edentulous spaces results in decreased/limited support
- Cannot tolerate operative procedures
- Presence of generalized periodontal weak teeth
Question 8. Discuss mouth preparation for fixed partial dentures.
Answer:
Mouth preparation is part of the treatment planning phase carried out to enhance the success of the fixed partial denture
Mouth Preparation Helps To
- Relieve symptoms
- Removes the etiologic factors
- Repairs the damages
- Maintains dental health
Procedures Of Mouth Preparation:
- Diagnosis and treatment planning
- Treatment to relieve the presenting symptoms
- Surgical procedures
- It involves
- Extraction Of:
- Hopeless abutment
- Residual root tips
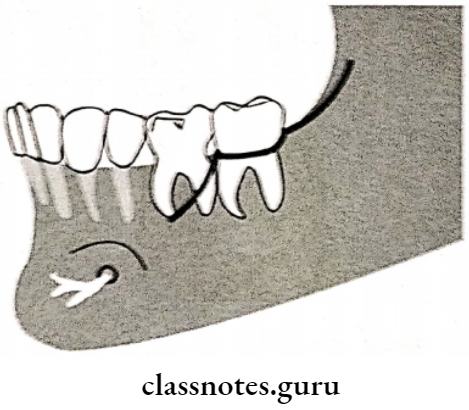
- Impacted/unerupted supernumerary teeth
- Malposed teeth, grossly extruded or drifted
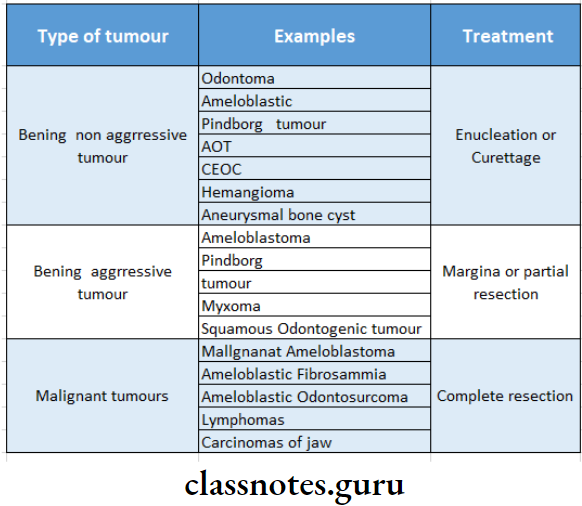
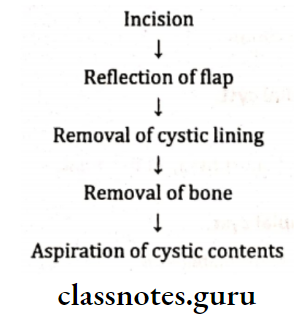
- Cyst And Tumors:
- Enucleation of cyst
- Excision of tumors
- Hyperplastic tissue – Surgical excision
- Bony spines and knife-edge ridges
- Al-veoloplasty to smoothen them
- Dentofacial deformity – Surgical correction
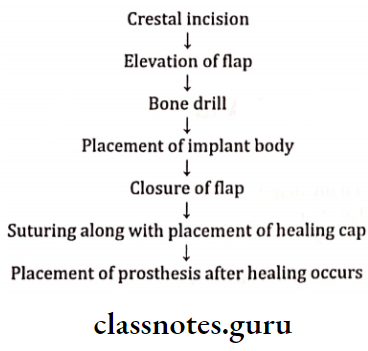
- Implant-supported fixed prosthesis
- These are placed under controlled oral surgical procedures
- Endodontic Procedures:
- Endodontically treated teeth are restored with crowns
- Caries tooth can be restored by amalgam, composite, GIC, pin retained restoration, or post and core
- Periodontal Procedures:
- Periodontal is carried out
- Removal of plaque and plaque retentive factors Elimination of pockets
- Crown lengthening procedures are carried out when clinical crown height is less and when retention will decrease due to it.
- Orthodontic Treatment:
- Minor orthodontic tooth movement can be done to upright a malpositioned abutment tooth
- Orthodontics can improve axial alignment
- Orthodontic will create pontic space and will improve embrasure form in the fixed prosthesis
- Orthodontics can direct occlusal forces along the long axis of the teeth
- Definitive occlusal treatment
- Orthodontic is done to make intercuspal position coincide with centric relation and to remove eccentric interferences
Contraindications of Mouth Preparation:
- Bruxers
- Angle class II and skeletal class III
- Excessive wear
- Temporomandibular pain
- Prosthetic rehabilitation and follow The patient needs to be recalled after prosthetic rehabilitation
Question 9. Discuss principles of bio-mechanical preparation in fixed partial dentures.
Answer:
1. Biological Considerations:
Prevention Of Damage During Tooth Preparation To:
- Adjacent Teeth:
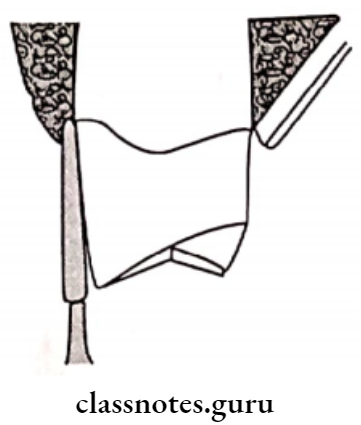
- Protect it by placing a matrix band during tooth preparation
- A thin taper diamond is used to break the
contact - If, however, the tooth gets damaged it has to be reshaped
- Soft Tissues:
- The tedious procedures can cause abrasion of soft tissues like lips, cheeks etc.
- It can be prevented by retracting it with the help of various types of retractors
- Pulpal protection
- Avoid excessive apical preparation
- Avoid excess removal of dentin
- Pulp may get damaged by the excessive heat generated, and chemical irritants used.
2. Conservation Of Tooth Structure:
- The tooth structure can be conserved by
- Use of partial veneer crowns
- Use of minimal taper of opposite axial walls
- Repositioning of tilted teeth before tooth preparation
- Use of conservative finish line
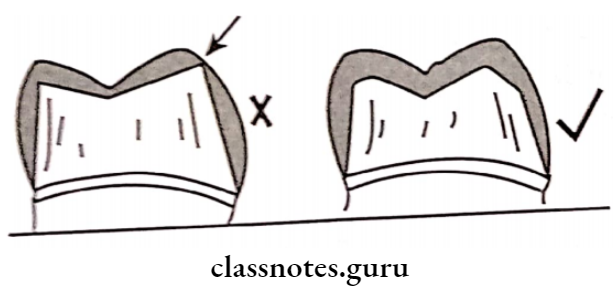
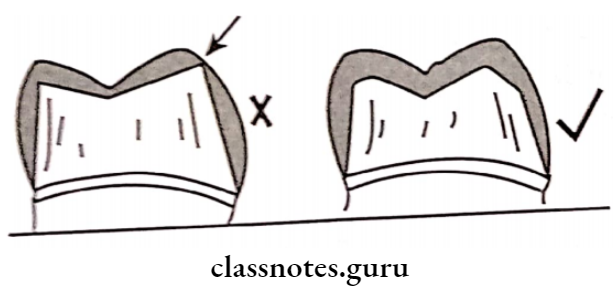
- Occlusal surface reduction should be such that
it follows the anatomical form
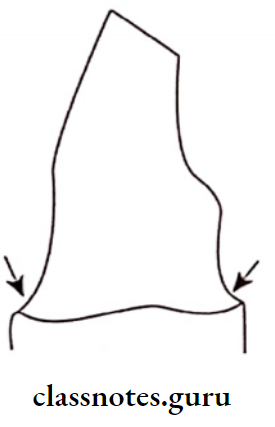
3. Margin Placement:
- The margin should be such that
- Margin is easy to prepare
- Margin is easy to identify in the impression and on the die
- Margin is easy to finish
- Margin should allow sufficient bulk of material
- Margin should preserve tooth structure
TypesOf Fixed Partial Denture:
- At The Crest Of The Gingival:
- Occlusal Consideration:
- Tooth preparation leads to the weakening of the tooth Thus, the occlusal reduction should be such that it maintains the anatomic form
- To obtain proper and conservative reduction, the tilted/supra-erupted teeth should be aligned prior to the preparation
- Mechanical considerations:
- Providing Retention Form:
- Retention is the quality of a preparation that prevents the restoration from becoming dislodged by forces acting parallel to the path of withdrawal
Factors Affecting Retention:
- The Magnitude Of The Dislodging Forces:
- It depends on the stickiness of the food, surface area, and texture of the restoration
- Geometry Of The Tooth Preparation:
- Taper Smaller degrees of taper have more retention
- The optimum taper is 6 degrees
- Surface area Crowns with long axial walls are more retentive
- Stress concentration – Round margins may reduce stress concentration and hence increase the retention
- Type of preparation – Addition of retentive grooves and boxes
- The Roughness Of The Surfaces:
- Materials Being Cemented:
- Base metal alloys – Better retained ‘
- Cement – Adheres better to amalgam
- Crowns – Adheres better to composite
- Type of luting agent: Adhesive resin cements are the more retentive
- Providing Resistance Form:
- Providing Resistance Form is the form that resists the lateral forces acting on the restoration and prevents its displacement
Factors Of Fixed Partial Denture:
- The magnitude and direction of the dislodging forces
- Geometry of the tooth preparation
- Increased taper-Decreases resistance
- Rounded axial angles
- Decreases resistance Short tooth preparation
- Physical properties of the luting agent zinc phosphate cements have a higher modulus of elasticity
1. Preventing Deformation Of The Restoration Factors:
- Alloy Selection:
- Type III or Type IV gold alloys
- High noble metal content ceramic alloys Nickel chromium alloys
- All these are harder alloys
- They resist the deformation and, hence preferred
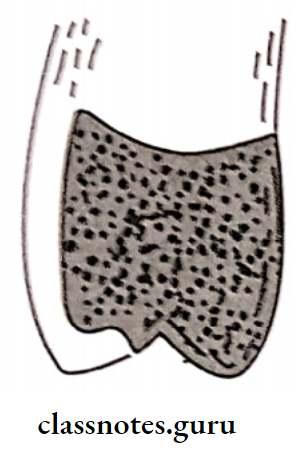
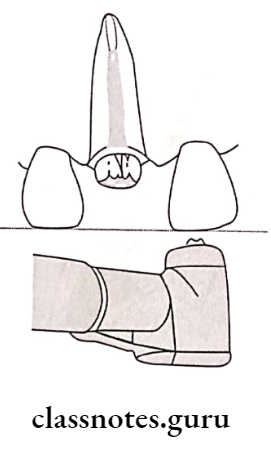
- Adequate Tooth Reduction:
- Tooth reduction should be 1.5 mm over functional cusps and 1 mm over non-functional cusps
- Margin Design:
- Margin Design depends on the type of restoration being used
- Example. Ceramic requires more reduction to obtain space for bulk material
2. Aesthetic Considerations:
- Aesthetic Considerations depends on the patient’s esthetic requirement
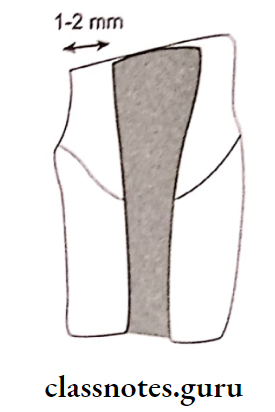
3. Partial Coverage Restoration:
- Proximal margin Place it buccal to the maximal contact area.
- Facial margin – It should be extended just beyond the occlusal-facial line angle
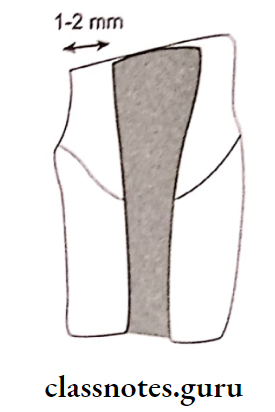
4. Metal Ceramic Restoration:
- Facial reduction – A minimal reduction of 1.5 mm is required
- Labial margin placement margins should be placed after observing the patient’s smiles
Fixed Partial Denture Short Essays
Question 1. Ridge lap and modified ridge lap pontic.
Answer:
- Ridge Lap Pontic:
- Evolved from saddle pontic
- Ridge Lap Pontic resembles a natural tooth
- Ridge Lap Pontic is designed to adapt closely to the ridge
- Satisfies esthetics
- Difficult to maintain
- Often leads to inflammation of the tissues in contact
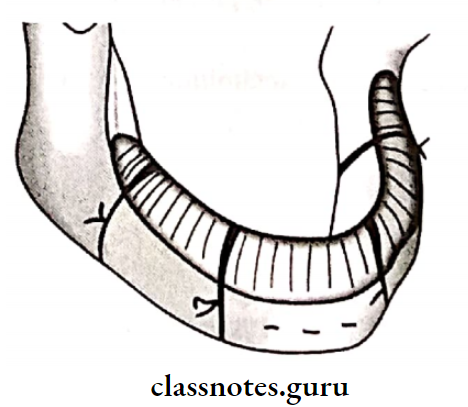
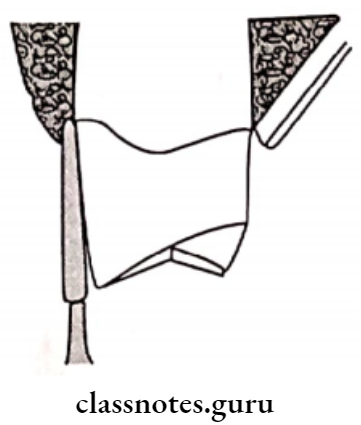
- Modified Ridge Lap Pontic:
- They are designed to reduce tissue contact
- Satisfies both esthetics and hygiene
- Tissue contact is limited to the buccal surface of the ridge crest
- Modified Ridge Lap Pontic has T T-shaped contact
- The vertical arm of the T ends at the crest of the ridge
- The horizontal arms form contact along the buccal surface of the ridge
- Recommended in maxillary anterior-posterior regions
- Modified ridge lap with no embrasure is recommended in mandibular anterior areas with extensive ridge resorption
Question 2. Sanitary pontic.
Answer:
Pontic Definition:
“An artificial tooth on a fixed partial denture that replaces a missing tooth restores its functions and usually fills the space previously filled by a natural crown”
Sanitary Pontic: These pontics have zero tissue contact
- Easy to maintain
- Highly unesthetic
- At least 3 mm of a vertical gap should be present between the pontic and the ridge
- Recommended in the mandibular posterior area
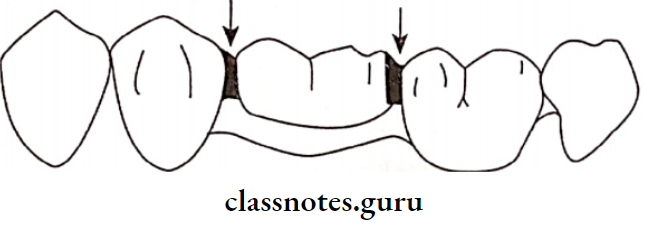
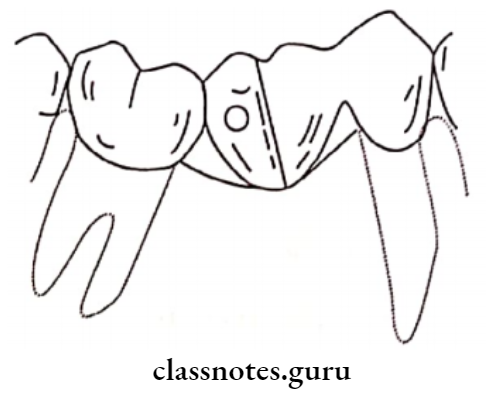
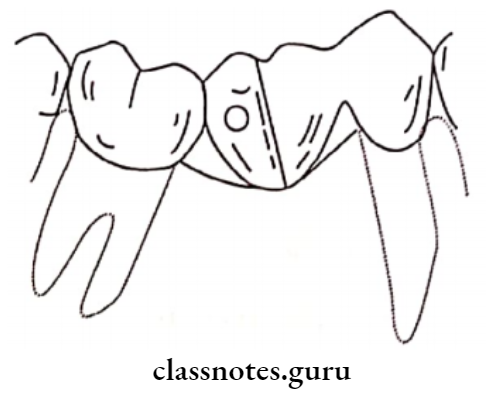
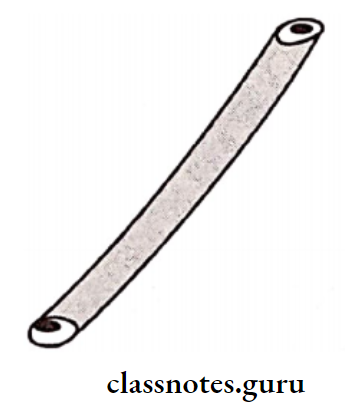
Question 3. Types of connectors in the fixed partial denture.
Answer:
Connector:
The connector is the portion of a fixed partial denture that unites the retainer and pontic
Types Of Connector:
1. Rigid Connectors: They are used to unite retainers and pontics in fixed partial denture
- Fabrication:
- The design of the connector is incorporated into a wax pattern
- The part of the connector to be soldered is sectioned
- The whole assembly is then cast
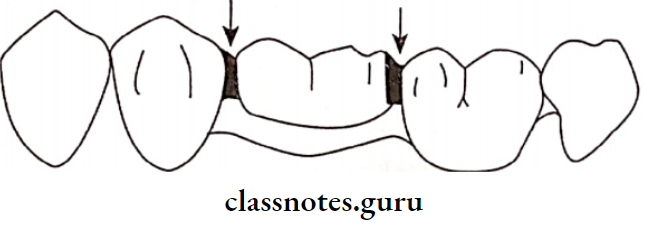
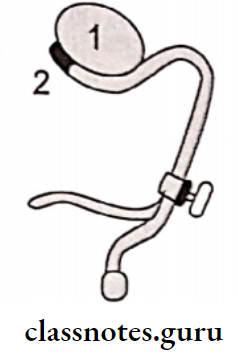
2. Non Rigid Connectors:
- These connectors are used in case of parallel abutments
- They allow limited movement between the retainer and pontics
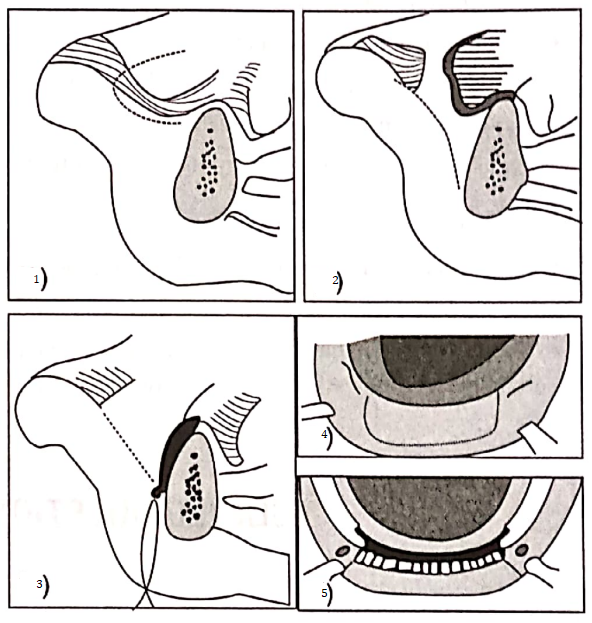
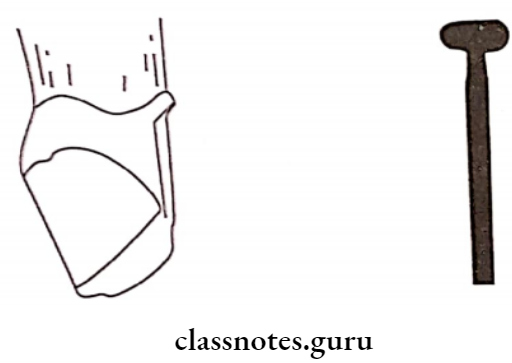
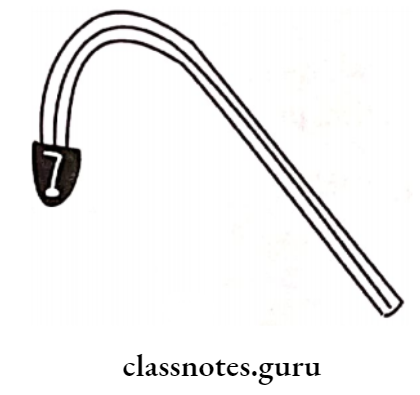
- Tenon Mortise pontic:
- It consists of Mortise as the female component and Tenon component as the male component
- The female component is prepared in the wax pattern within the contours of the retainer
- The male component is fabricated with auto-polymerizing resin and attached to the pontic
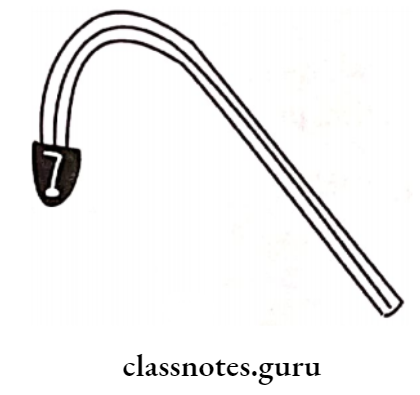
- Loop Connectors:
- Loop Connectors is used in diastema cases
- Loop Connectors consists of a loop on the lingual aspects of the prosthesis that connects adjacent pontic and retainer
- Split Pontic Connectors:
- Split Pontic is used with a pier abutment
- The pontic is split into mesial and distal segment
- Each segment is attached to retainer
- The mesial segment is fabricated with a key while the distal segment with a key way to fit over the key.
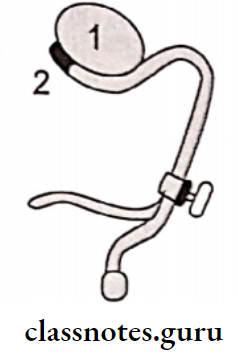
3. Cross Pin And Wing Connectors:
- Cross Pin And Wing is used for tilted abutments
- A wing is attached to the distal retainer called the retainer wing component
- The pontic is attached to the mesial retainer called the retainer pontic component
- These are fabricated and aligned on the working cast
- 0.7 mm pinhole is drilled across the wing The components are cemented
- Next, the pin is seated into the hole using a punch and mallet
Question 4. Veneering materials.
Answer:
Veneer is a layer of tooth-colored material that is applied to a tooth to restore localized/generalized defects and intrinsic discoloration
Materials Of Veneering:
1. Ceramic: It is most ideal veneering material when used with metal substructure or in all ceramic restoration
The Procedure Of Ceramic:
- Metal preparation:
- Clearing of casting defects
- Cleaning of casting by sandblasting and ultrasonic cleaning
- The gingival surface of the pontic is reduced
Porcelain Application Of Ceramic:
- An opaque layer of porcelain should be applied over the metal surface
- The gingival surface of porcelain is coated with cervical porcelain
- Next other part are build-up
- Next porcelain is fired
2. Acrylic:
- After firing the core porcelain, glaze porcelain is added and fired as usual
- Acrylic can be used with metallic restoration
- Has poor wear resistance
- So not used as a permanent restoration
The Procedure of Acrylic:
- Mechanical undercut are made over the entire metal surface
- The surface of cast metal can be roughened using aluminum oxide
- A small quantity of opaque resin is added to the metal surface
- Body surface resin is added over opaque resin
- Resin is polymerized
- Excess material is carved out Incisal shade resin is added
- Finally restoration is finished and polished
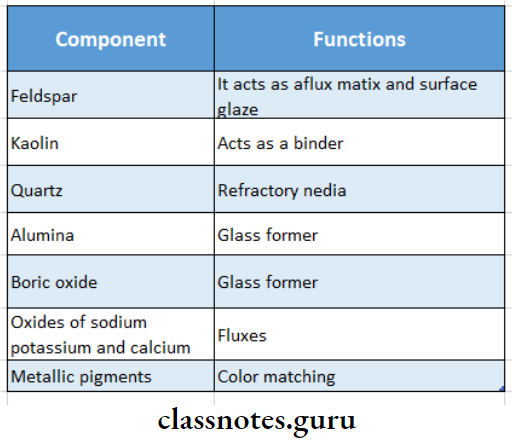
Question 5. Ceramics.
Answer:
Definition Of Ceramics:
Ceramics is an inorganic compound with nonmetallic properties typically consisting of oxygen and one or more metallic or semi-metallic elements that are formulated to produce the whole or part of ceramic-based dental prosthesis
Classification of Ceramics:
- According to the firing temperature
- High fusing
- Medium fusing
- Low fusing
- Ultra-low fusing
- According to the type
- Feldspathic porcelain
- Leucite-reinforced glass ceramic
- Alumina reinforced porcelain
- Zirconia reinforced ceramics
- According to the function of the restoration
- Core ceramics
- Opaque ceramic
- Veneering ceramic
- According to microstructure
- Glass ceramic
- Crystalline ceramic
- Crystal containing ceramic
- According to the fabrication process
- Condensable ceramics
- Heat pressed ceramic Castable ceramic
- Machinable ceramics
Ceramics Composition:
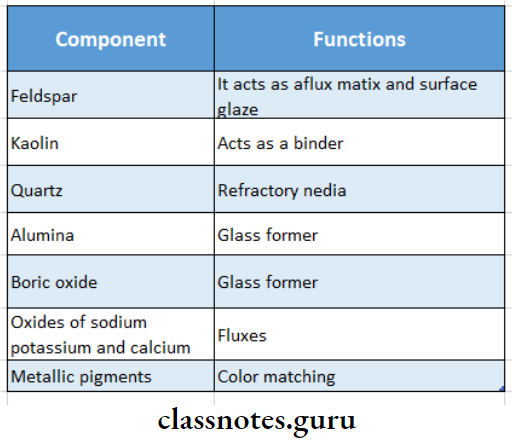
Uses Of Ceramics:
- Single unit crown
- Porcelain veneer for crown and bridges
- Artificial teeth
- Inlays and onlays
- Ceramic brackets used in orthodontics
- Implants, bioglasses
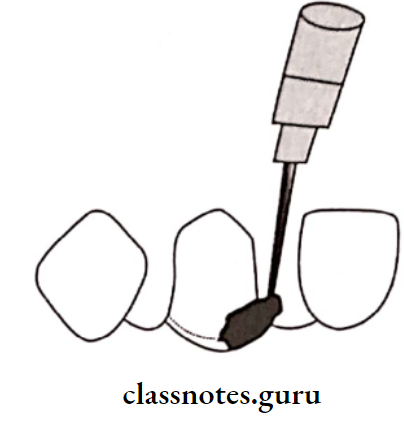
Question 6. Blockout procedure.
Answer:
- Blockout is defined as the elimination of undesirable undercut areas on the cast to be used in the fabrication of the removable partial denture
- Blockout is the process by which the undesirable undercuts on the master cast are eliminated using wax
- Since the undercuts are filled with wax, the refractory cast duplicated from the master cast will not have these undercuts
- Before blocking out, the master cast is coated with a sealer so that it forms a protective film over the cast
Types Of Blockout Procedure:
- Parallel Block Out:
- This is the procedure by which undercuts below the height of the contour of the existing teeth are eliminated in relation to that path of insertion
- Blockout wax is filled into the infra-bulge area of the tooth and trimmed such that its surface is parallel to the path of insertion
- Arbitrary Blockout:
- Arbitrary Blockout involves filling the soft tissues and other unwanted undercuts in the cast with block-out wax
- Formed Or Shaped Blockout:
- Formed Or Shaped is done in the undercut of the primary abutment along the lower border of the proposed retentive arm
Question 7. RPI system.
Answer:
- Rest, Proximal Plate and I-bar
- RPI system is a modified I-bar retainer system
1. Mesial Rest modification:
- Mesial rest extends into the triangular fossa in molar preparation
- Canine rests are circular, concave depressions prepared on the mesial marginal ridge
2. Proximal Plate Modification:
- Design Modification 1: The proximal plate is designed to extend from the marginal ridge to the junction between the middle and cervical third of the tooth
- Design modification 2: The proximal plate is designed to extend along the entire length of the proximal surface of the abutment with a minimum tissue relief
- Design modification 3: The proximal plate is designed to contact just about 1 mm of the gingival third of the guiding plane of the abutment tooth
3. 1-bar Modification:
- The tip of 1-bar is modified to have a pod-shaped in order to allow more tooth contact
- 1-bar is placed more mesially
Question 8. Rubber-based impression materials.
(or)
Impression materials in FPD.
Answer:
Properties of Rubber Base Impression Materials:
- Rubber Base Impression Materials are accurate impression materials they excellently reproduce the surface details
- Rubber Base Impression Materials are dimensionally stable
- Available in various viscosity
- The low viscosity is capable of reproducing even very fine details
- Rubber Base Impression Materials are generally hydrophobic
- Resilience
- Rubber Base Impression Materials are flexible with near complete elastic recovery the coefficient of thermal expansion is high
- Rubber Base Impression Materials cannot melt, before melting they pass into a gaseous state
- Rubber Base Impression Materials swell in the presence of certain solvents
- Rubber Base Impression materials are insoluble
- Rubber Base Impression Materials have lower creep resistance
- Tear strength is excellent
- Rubber Base Impression Materials can be electroplated
Uses Of Rubber Base Impression Materials:
- In FPD for impressions of prepared teeth
- In RPD for an impression of dentulous mouths
- On CD impression of the edentulous mouth
- Polyether is used for border molding
- For bite registration
- Silicon is used for making refractory casts
Materials Of Rubber Base Impression Materials:
- Polysulphide
- Condensation silicone
- Addition silicone
- Polyether
Question 9. Soldering-implication and procedures.
Answer:
Soldering involves joining two components of metal with an intermediate metal whose melting temperature is lower than the parent material
Implications Of Soldering :
- To cast multiple smaller units
- To rectify casting defects
Proedures Of Soldering:
- Soldering For Metal Ceramic Restoration:
- Soldering is done prior to ceramic application
- Done at a temperature of 1075 to 1120 degrees C
- Soldering Advantages:
- The metal framework can be soldered and tried prior to ceramic build-up
- Minor casting errors can be corrected
- Soldering Disadvantages:
- Difficult to build ceramic
- Oven Soldering:
- Performed under vacuum or in air
- Torch Soldering:
- Torch Soldering is done under direct flame
- Infrared Soldering:
- Used for low-fusing connectors
- Good accuracy is possible
- Laser welding:
- Infrared Soldering is done to join titanium components of dental crowns, bridges, and partial denture frameworks
- The maximum penetration depth of the laser welding unit is 2.5 mm
Question 10. Double impression technique.
Answer:
Double Impression Technique is one of the methods of impression-making for fixed partial dentures
- Technique of Double Impression:
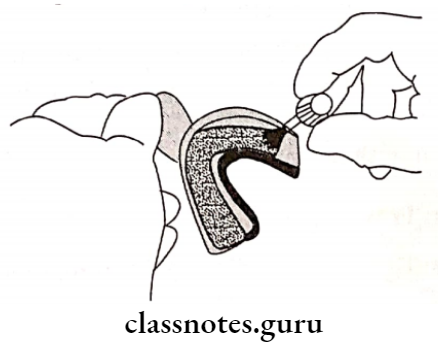
- A suitable stock tray is selected
- Tray adhesive is applied uniformly to the tray
- Putty impression material is mixed and made into a rope and loaded onto the tray
- A spacer for light body material should be placed over the loaded putty material
- The loaded tray along with the spacer is used to make a full mouth impression
- After making and removing the impression the polyethylene spacer is carefully peeled away
- The impression is additionally relieved by scraping the areas that recorded the tooth preparation
- The light body material is then syringed over the putty impression and also over the tooth preparation
- The final impression will contain the accurate details recorded by the light body impression material
Question 11. Full veneer crown.
Answer:
Full veneer crown covers all the tooth surfaces
Indications Of Full Veneer Crown:
- A full Veneer Crown is indicated when the Abutment tooth is small The edentulous span is long
- When the partial veneer crown lacks in retention, resistance, coverage, or esthetics
- When the abutment is extensively decayed or decalcified or previously restored
- For endodontically treated teeth
Contraindications Of Full Veneer Crown:
Full Veneer Crown is not given to patients with uncontrolled caries
The Procedure Of Full Veneer Crown:
- Occlusal reduction
- Axial reduction
- Buccal reduction
- Lingual reduction
- Proximal reduction
- Establishing the finish lines
Commonly Used Full Veneer Crowns:
- Full metal crowns
- Metal ceramic crowns
- All ceramic crowns
Question 12. Diagnostic aids in fixed partial dentures.
(or)
Radiographs in fixed partial denture.
Answer:
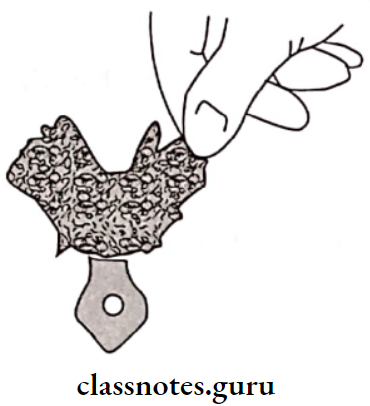
1. Diagnostic Cast:
- The impression for the diagnostic cast is made with alginate in a perforated stock tray and poured into a dental stone
- The diagnostic cast should be an accurate reproduction of the teeth and adjacent tissues
- A Diagnostic Cast is a life-size reproduction of a part or parts of the oral cavity or facial structures for the purpose of study and treatment planning
Importance Of Fixed Partial Denture:
- Fixed partial denture permits viewing the occlusion from both lingual and buccal aspect
- Fixed partial denture helps to analyze the existing occlusion
- Fixed partial denture helps to survey the dental arch
- Fixed partial denture helps to survey the cast
- Fixed partial denture aids in mouth preparation
- Fixed partial denture aids in patient’s education
- Fixed partial dentures aid in the selection of trays
- Fixed partial dentures may be used as a constant reference
- Fixed partial denture helps in mock surgery
Advantages Of Fixed Partial Denture:
- Fixed partial denture allows changing of the interocclusal relations
- Fixed partial denture helps to prepare and assess tooth preparation
- The path of withdrawal can be determined
2. Radiographs Types:
- Periapical:
- Periapical determines the extent of bone support, quality of supporting bone
- Periapical determines the root morphology of each abutment tooth
- Periapical evaluates the width of periodontal ligament space
- Periapical evaluate bone resorption
- Periapical determines
- Inclination of teeth
- Continuity of lamina dura
- Pulpal morphology Any periapical pathology
- Crown root ratio
- Root length, shape
- Periodontal status of abutment
- Bitewing:
- Evaluation of proximal caries
- Evaluate secondary caries on the previous restoration
- Panoramic Files: Aid in
- Evaluation of bone resorption, pattern of bone resorption, and quality of bone support
- To check for the presence of retained root tips, impacted tooth
- To determine the thickness of soft tissue on the ridge in an area of pontic placement
- In The Case Of TMJ Disorders:
- Transcranial exposure
- Serial tomography Arthrography
- CT scanning
- Magnetic resonance imaging
Question 13. Recording of jaw relation for crown and bridge.
Answer:
Types Of Jaw Relation:
- Centric registration:
- Centric occlusion
- Centric relation
- Eccentric registration:
- Lateral excursive records
- Protrusive records
Jaw Relation Centric Occlusion:
- Direct Intercuspation:
- An interocclusal record is placed over the prepared tooth
- The patient is asked to close to the normal interocclusal position
- After it is set, the record is trimmed and articulate
- Centric Relation:
- Bite wafer technique
- A bite wafer is made from base plate wax
It is used to record the relation - The indentations in the wax are brushed with zinc oxide eugenol, repeat the record
- Anterior Stop Technique:
- A wax wafer is pressed to the occlusal surface of the maxillary teeth with the anterior jig
- The wafer is refined and shaped to the patient arch form
- The patient is asked to close on posterior teeth until the lower teeth touch the anterior jig
- After recording it, a thin layer of ZOE is applied to the lower cusp indentation of the wafer, and the record is repeated
Eccentric Relation:
- Lateral Relation:
- Canine-Guided Occlusion: In lateral movement, the canine causes the separation of all the other teeth
- Group Function: In lateral movement contact is maintained between a group of teeth
Method Of Jaw Relation:
- Mount the patient’s cast on an articulator
- Manipulate the mandibular member such that the left mandibular canine is edge to edge with the left maxillary canine
- A wax wafer is placed on the lower cast
- The record is checked in the patient’s mouth
- Jaw is followed by the ZOE record
Protrusive Relation:
- Articulate the patient’s cast
- The upper cast is brought with the incisors in an end-to-end relation
- A warm wax is placed in the patient’s mouth
- Reline the indentation of wax with registration paste
- The resultant refined bite is placed on the mandibular cast and the maxillary cast is placed over it
Question 20. Questionable Abutment.
Answer:
Questionable Abutment are abutment teeth that can be retained after periodontal and endodontic treatment which otherwise is a hopeless tooth
Selection Of Questionable Abutment
- Periodontally weak tooth:
- A tooth with slight mobility
- Tooth with recession
- Tooth with furcation involvement
- A tooth with gingival and periodontal pathology
- Corrected By:
- Scaling and root planning
- Splinting of mobile teeth
- Flap surgeries for recession
- Ridge augmentation for osseous defects
- Abutment Tooth Requiring Endodontic Treatment:
- If pulpal vitality is doubtful endodontic treatment is carried out
- It is then treated with post and core
- Abutment With Large Restoration:
- Subgingival margin is used in it
- Abutments That Are Malaligned, And Tilted:
- Mesially drifted tooth leads to insufficient space for pontic
- Abutments That Cannot Withstand Forces:
- Certain modifications are carried out
- Implant-supported prostheses need to be used
- Pontics and connectors should be of adequate thickness
- A single incisor present is best removed
- Multiple edentulous spaces are best restored with a combination of fixed and removable partial dentures
- Abutments That Are Grossly Attrited:
- Crown lengthening procedures or a sub-gingival finish line should be done
- If chances of pulp exposure are present it should be endodontically treated
- Proximal boxes and additional grooves are added to the preparation
- Abutments With Reduced Bone Support:
- After periodontal disease root surface area is reduced
- Short conical roots give less support
- Divergent multiple roots give good support
- A single rooted tooth with an elliptical cross-section gives better support
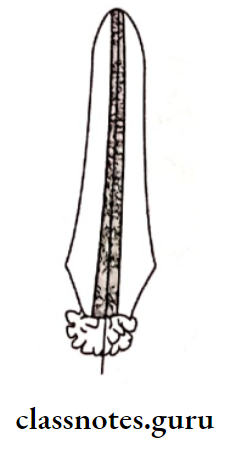
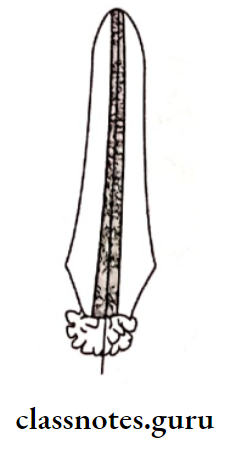
Question 21. Post and Core/radicular retainer.
Answer:
- When an endodontically treated tooth is used as an abutment, the post and core are used
- The post/dowel is the screw component that is inserted into the root canal
- The core is the retentive component, which acts as a prepared crown for the placement of a retainer
Types Of Post And Core:
- Prefabricated
- Custom made
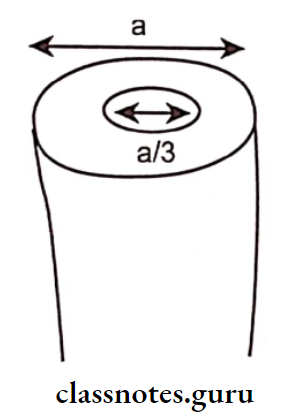
Post And Core Factors To Be Considered:
- The canal should be obturated only with gutta-percha
- For proper retention, the length of the dowel core inside the root should be at least 2/3rd of the root length
- The coronal portion of the dowel should be encircled at least by 1-2 mm of tooth structure to obtain a ferrule effect.
Tooth Preparation:
- Unsupported enamel is removed
- Any weak enamel wall or restoration should be removed
- Remove the gutta-percha and enlarge the canal using peesoreamer
- There should be at least 1 mm of tooth structure at the apical end
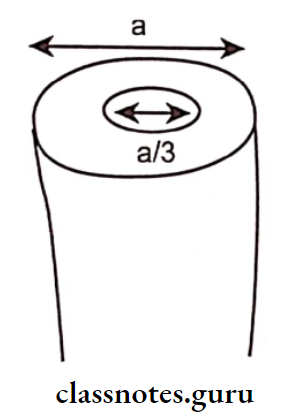
- The diameter of the canal should be at least 1/3rd the width of the tooth
- A contra bevel is placed around the occluso-axial line angle
- The canal and plastic sprue are coated with petrolatum jelly
- Impression is made with resin
- The pattern is cast and finished
Question 22. Bridge Retainer.
Answer:
Bridge Retainer:
“The part of a fixed partial denture which unites the abutment to the remainder of the restoration”.
Types Bridge Retainer:
1. Bridge Retainer Based On Tooth Coverage:
- Full Veneer Crown:
- A full veneer crown covers all the surfaces of the abutment
- Full veneer crowns are indicated for extensively damaged teeth
- Full veneer crowns are the most retentive
- Partial Veneer:
- Partial Veneer require less tooth reduction
- Partial Veneer is less retentive

Bridge Retainer Conservative:
- Bridge Retainer requires less tooth reduction
- Bridge Retainer is indicated for anterior teeth
- Bridge Retainer has small metallic extensions luted onto the lingual surface of the abutment using resin cement
2. Bridge Retainer Based On The Material Used:
- All Metal:
- Bridge Retainer can be partial/full veneer
- Bridge Retainer require minimal tooth reduction
- Bridge Retainer are strong enough
- Metal Ceramic Retainers:
- Metal Ceramic Retainers require more tooth reduction
- Metal Ceramic Retainers can be fabricated over an entire full veneer crown over the labial/buccal surface of full veneer or over partial veneer
- All Ceramic Retainers:
- Ceramic requires maximum tooth reduction because porcelain requires sufficient bulk for adequate strength
- All Acrylic Retainers:
- Acrylic are used for long-term temporary fixed partial dentures
Question 23. Structural Durability.
Answer:
- The ability of the restoration to withstand destruction due to external forces is known as “structural durability”
- Adequate reduction during tooth preparation is necessary to obtain adequate thickness of restoration
- The amount of reduction required depends on the type of restoration and the design of the restoration
Question 24. Supragingival Finish lines.
Answer:
Requirements of Supragingival Finish Lines:
- Shallow bevels nearly parallel to the cavosurface should be avoided
- The bevel should not produce a very acute margin
- The tooth should not be reduced to more than half of the width of the diamond.
Types of Supragingival Finish Lines:
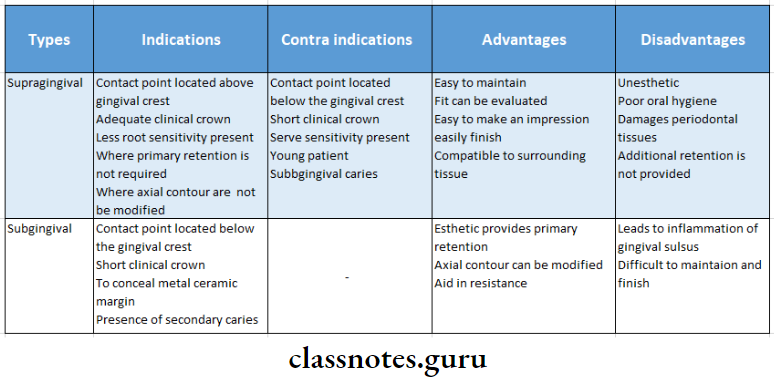
1. Chamfer of Supragingival Finish lines:
This possesses a curved slope from the axial wall to the margin
Indications Of Supragingival Finish Lines:
- Cast metal restorations
- Metal collars
- Lingual margins of metal-ceramic restoration
Contraindications Of Supragingival Finish Lines:
- Restoration where the finish line will be obvious
Disadvantages Of Supragingival Finish Lines:
- Marginal distortion
- Provide less room cervically
2. Shoulder:
Shoulder has a gingival finish wall perpendicular to the axial surfaces of the teeth
Indications of Shoulder:
- All anterior restoration
- All ceramic restoration
- Facial margins of metal-ceramic
Advantages Of Shoulder:
- Less marginal distortion
- Good marginal adaptation
- Esthetic
- Increased retention
- Better resistance to occlusal forces
- Sholuder accommodates the bulk of porcelain
Disadvantages of Shoulder:
- Requires more tooth reduction
- This leads to adverse pulpal involvement at 90°
3. Shoulder With A Bevel:
An external bevel is created on the gingival margin of the finish line
Indications of Shoulder With A Bevel:
- Facial finish line of metal-ceramic
- Presence of ledge
Advantages of Shoulder With A Bevel:
- Aids in contouring the restoration
- Improves burnish ability
- Minimizes the marginal discrepancy
- It prevents unsupported margins from chipping
4. Feather Edge And Knife Edge:
- Difficult to wax up and cast
- Difficult to produce smooth margin
- Susceptible to distortion
- Overcontoured restoration
Indications of Knife Edge:
- Lingual surface of mandibular posteriors
- The very convex axial surface
- For the undercut of tipped teeth
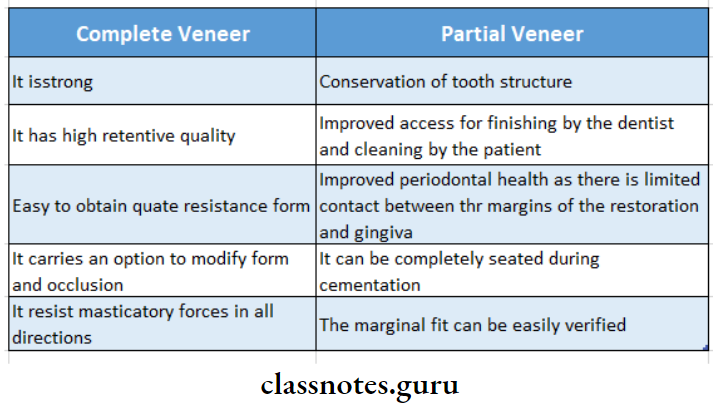
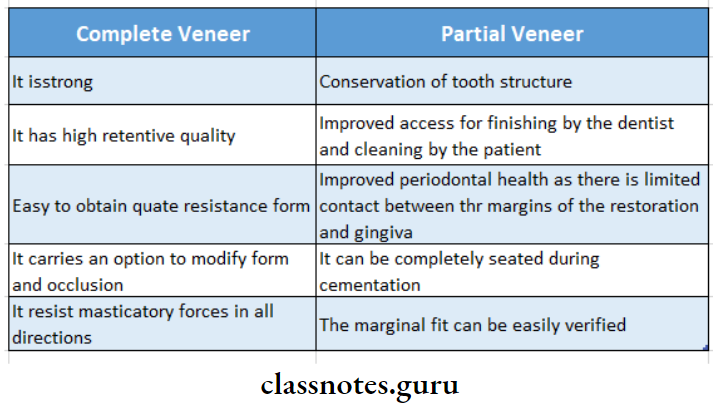
Question 25. Merits of complete veneer and partial veneer
Answer:
Question 23. All ceramic restoration/metal-free ceramics.
Answer:
Ceramic Restoration was introduced by Land in 1903
Ceramic Restoration is defined as man-made solid objects formed by baking raw materials at high temperatures
Classification Of Ceramic Restoration:
- Conventional powder- Slurry ceramics
- Castable ceramics – Dicor plus
- Machinable ceramics – Dicor MGC
- Pressable ceramics – IPS Empress
- Infiltrated ceramics – In cream
Advantages Of Ceramic Restoration:
- Superior aesthetics
- Excellent translucency
- Requires slightly more preparation of the facial surface ‘The appearance can be influenced and modified by selecting different colors of luting agent
Disadvantages Of Ceramic Restoration:
- Reduced strength
- Ceramic Restoration is very difficult to obtain a well-finished margin
- They cannot be used on extensively damaged teeth
- Due to porcelain’s brittle nature, large connectors have to be used
- This usually leads to impingement of the interdental papilla
- Wear of opposing natural teeth
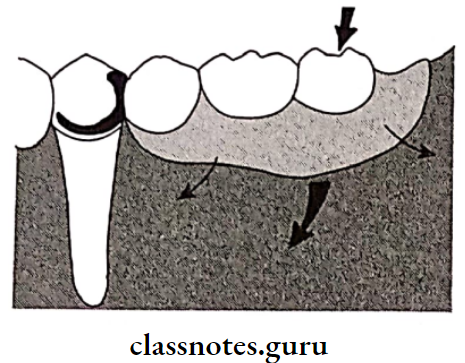
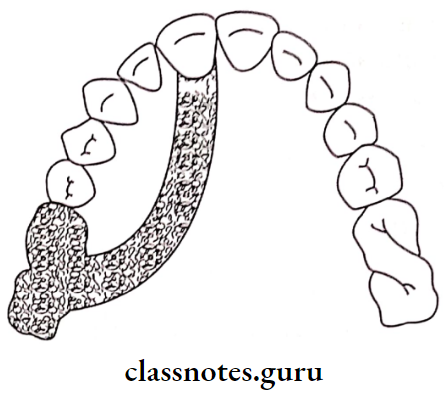
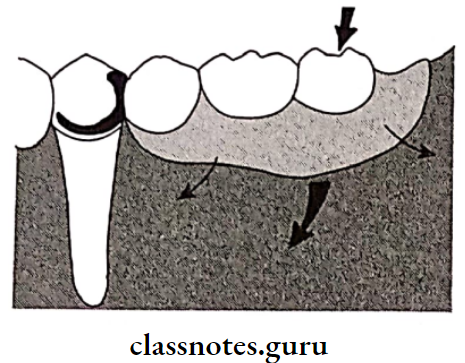
Question 26. Cantilever Fixed Partial Denture/Bridge.
Answer:
Cantilever is a fixed partial denture in which the pontic is retrained and supported only on one end by one or more abutments
Selection Of Cantilever Abutment:
- Good bone support should be present more than the average
- Adequate clinical crown height should be present
- Should be able to develop a harmonious occlusion
- Should have a good clinical crown height
Indications Of Cantilever Abutment:
- Replacement of lateral incisor
- Replacement of first premolar
Contraindications Of Cantilever Abutment:
- Extensively damaged teeth Maligned teeth.
- Mobile teeth
- Endodontically treated teeth
Advantages Of Cantilever Abutment:
- Conservative design with preservation of tooth structure
- Secondary abutments used can be prepared easily with parallelism
- Easy to fabricate
Disadvantages Of Cantilever Abutment:
- Produces torquing and lateral forces Cannot restore long-span edentulous space
- Lateral forces can tip, rotate, or drift the abutment tooth
Question 27. Gingival Retraction Techniques.
(or)
Gingival Retraction
Answer:
Gingival Retraction
1. Gingival Retraction Mechanical Methods:
- Rubber Dam:
- Punch holes are made in the area of the preparation site of the rubber dam and clamped in position.
- Cotton Rolls:
- In the maxillary arch, a single cotton roll is used in the buccal vestibule.
- While in the mandibular arch, cotton rolls are placed both in the buccal vestibule and lingual sulcus
- High Vaccum:
- High Vaccum can be used as a retractor as well as for clear-ing saliva and water during preparation
- It is also useful for removing small operatory debris
- Saliva Ejector:
- It is placed in the corner of the mouth opposite the quadrant being operated
- It is used for the evacuation of the maxillary arch
- Svedopter:
- Svedopter consist of a metal saliva ejector with a tongue deflector
- Effectively used in the mandibular arch
- Effective fluid control
Disadvantages Of Gingival Retraction :
- Access to the lingual surface of mandibular teeth is limited
- Gingival retraction may cause injury to the floor of the mouth due to metallic nature
- Presence of tori makes its use difficult
- Tongue deflector
- Suction tip
- Cellulose Wafers:
- Cellulose wafers is used along with cotton rolls to control saliva and retract the cheek laterally
- Oversized Copper bands:
- Oversized copper bands are placed on the prepared tooth and elastomeric impression material is used to make an impression of the prepared tooth which retracts the gingival
2. Chemical Methods:
- Agents:
- Anti-Sialogogues:
- These are group of drugs that can be effectively used to control salivary flow
- They inhibit the action of myoepithelial cells in the salivary glands
- Anti-Sialogogues Examples:
- Methantheline bromide 50 mg: 1 hour before the procedure
- Propantheline bromide 15 mg: 1 hour before the procedure
- Clonidine hydrochloride 0.2 mg: 1-hour procedure
- Local Anaesthetic:
- Contraindications:
- Hypersensitive patients
- Patients with glaucoma
- Asthmatic patients
- Obstructive conditions of congestive heart failure
3. Mechanico-Chemical Methods:
Mechanical is a method of combining a chemical with pressure packing which leads to the enlargement of the gingival sulcus
- Mechanical Chemical Used:
- 8% Racemic epinephrine
- Aluminium chloride
- Alum
- Ferrous sulphate
- Mechanical Technique:
- The operating area should be dry
- The retraction cord is drawn from the dispenser bottle
- The cord is dipped in 25% AIC13 solution in a dampened dish
- The retraction cord is looped around the tooth and packed into the gingival sulcus
- After 10 minutes, the cord should be removed slowly
4. Surgical Methods:
- Rotary Curettage: It is a troughing technique, wherein a portion of the epithelium within the sulcus is removed to expose the finish line
- Rotary Curettage Technique:
- The torpedo diamond point is extended into the gingival sulcus to remove a portion of sulcular epithelium
- Abundant water should be sprayed
- Electrosurgery:
- An electrosurgery unit is a high-frequency oscillator or radio transmitter that uses either a vacuum tube or a transmitter to deliver a high-frequency electric current of at least 1 MHz.
- Electrosurgery denotes the surgical reduction of sulcular epithelium using an electrode to produce gingival retraction.
Question 28. Impression Procedures for Fixed Partial Denture
Answer:
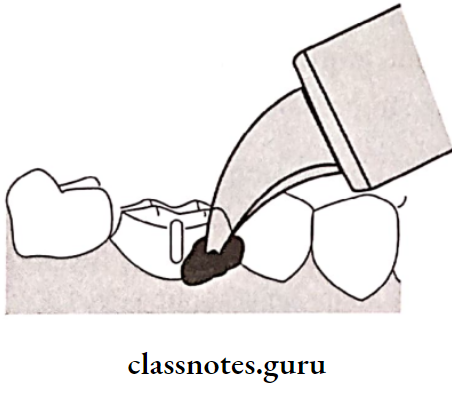
- Stock tray/Putty wash impression:
- Custom tray impression – Single Mix:
- Closed bite double arch method/triple tray technique.
- Copper tube impressions
- Post space impressions
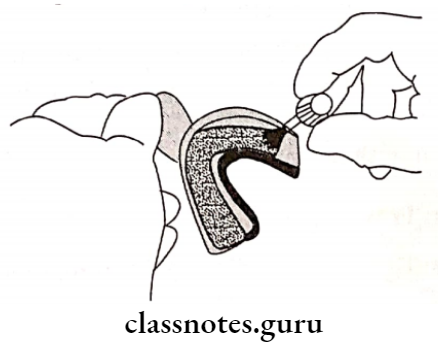
1. Putty Wash Impression:
- Double Mix Technique:
- An appropriate stock tray is selected
- Tray adhesive is applied over it
- Putty material is mixed and formed in the shape of rope and loaded onto the tray
- A spacer (polythene sheet) is placed over it • Impression is made
- Remove the impression Next, take out the spacer
- Light body material is syringed over the tray as well as the prepared tooth
- Repeat the impression
- Single Mix Technique:
- Putty material is loaded into the tray while light body material is syringed over the prepared tooth
- A full-mouth impression is made
2. Custom Tray Impression:
- Two sheets of tin foil spacer are applied over the primary cast
- An acrylic special tray is fabricated over it
- Tray adhesive is applied over it
- Medium-body elastomer is loaded into the tray and light body material is syringed over the prepared tooth
- Full mouth impression is made
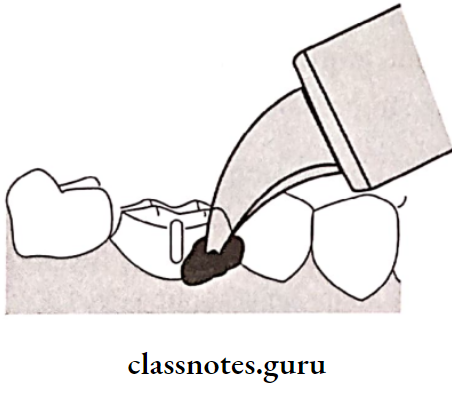
3. Triple Tray Impression:
- The tray consists of a plastic framework with a plastic sleeve and handle
- Light body material is injected into the prepared tooth
- High-viscosity material is placed in excess on both arches
- The tray is placed in between the arches
- The patient is asked to bite slowly
- After the material sets, the patient is asked to open the mouth due to which the tray adheres to one arch
- Bilateral pressure should be applied to remove it
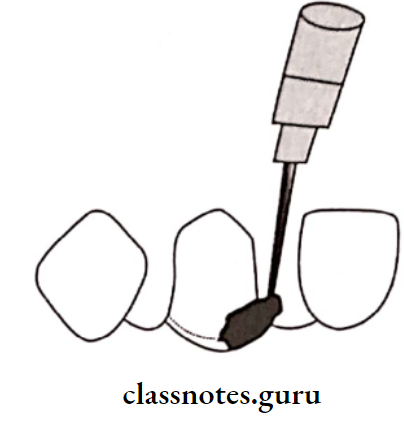
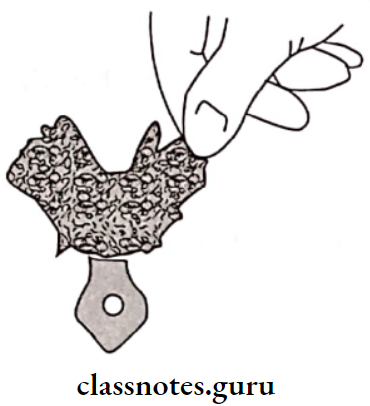
4. Copper Band Impression Technique:
- A softened impression compound is filled up to 1/3rd of the copper band
- It is placed onto the prepared tooth
- Light body material is syringed over the prepared
tooth
5. Post Space Impression:
- A separating medium is applied on the post space
- Light body material is syringed into it
- A lentil spiral, coated with tray adhesive is used to push the material into the post space
- Before it sets, medium/heavy-bodied impression. material is loaded over the tray and placed over it
- Both are removed together
Question 29. Temporization/Provisional Restoration.
Answer:
Temporization is a restoration that is established for the time being, until a permanent arrangement can be made
Requirements Of Temporization:
- Biological Requirement:
- Biological requirements should provide pulpal protection
- Biological requirements should maintain periodontal health
- Biological requirements should maintain occlusal harmony
- Mechanical Requirements:
- The restoration should be able to transmit the occlusal forces
- Mechanical requirements should closely adapt
- Mechanical requirements should not be damaged during the removal
- Material Requirements:
- Material requirements should be bio-compatible
- Material requirements should have sufficient working time
- Material requirements should be easy to fabricate
- Material requirements should be dimensionally stable
- Material requirements should have adequate strength
- Material requirements should be esthetic
- Material requirements should be compatible with the luting agents
Types of Temporization:
- Based on method of fabrication:
- Based on the type of material used:
- Based on duration of use:
- Based on technique for fabrication:
- Direct technique Indirect technique
- Direct-indirect technique
Disadvantages of Temporization:
- Provisional restoration tends to fracture They poorly adapt to the margins
- They wear off easily
- They have unpleasant odour
- They may cause tissue irritation
- It is difficult to remove it
- They have poor colour stability
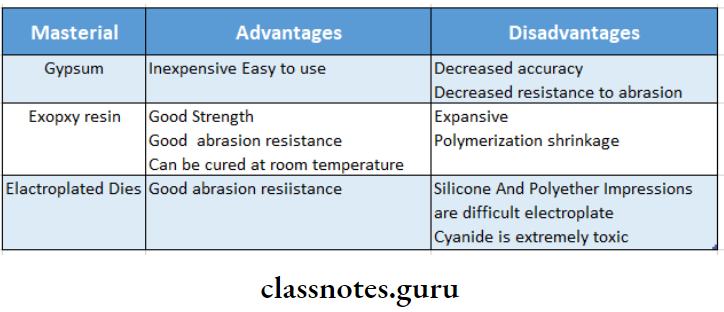
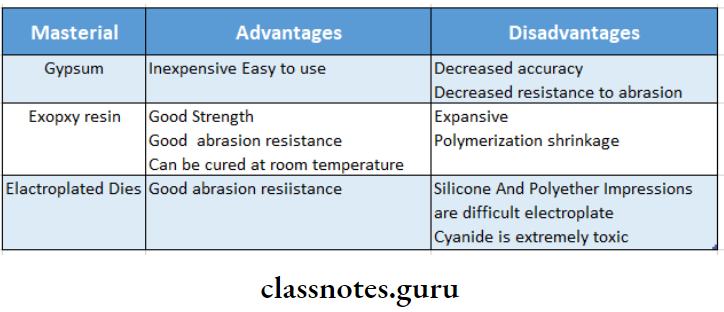
Question 30. Die Materials.
Answer:
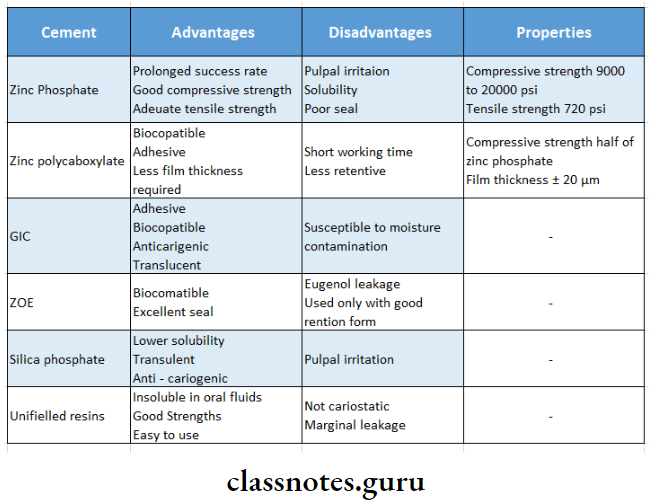
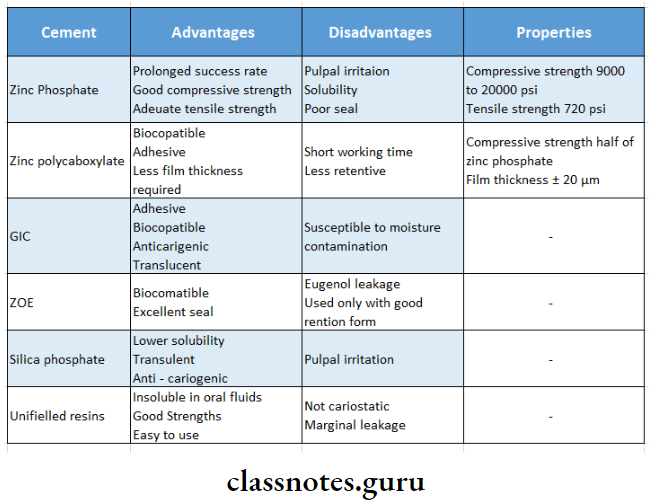
Question 31. Luting Cements for fixed Partial Denture.
Or
Properties of polycarboxylate and GIC
Or
Cement in FPD
Answer:
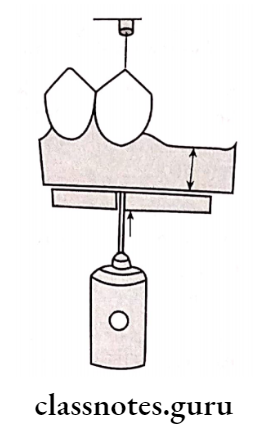
Question 32. Porosities.
Answer:
1. Solidification Defects:
- Solidification Shrinkage:
- Mainly occurs near sprue-cast junction
- Solidification Shrinkage Causes:
- Incomplete feeding of molten metal
- Premature solidification of the sprue
- Suck Back Porosities:
- Occurs near sprue
- Suck Back Porosities Cause:
- This occurs when a hot metal, impinging from a sprue channel onto a point on the mold wall, causes a hot spot
- This causes local regions to freeze last resulting in shrinkage
- Suck Back Porosities Prevention: Lowering casting temperature
2. Microporosities:
- Microporosities Cause: Too rapid solidification
- Microporosities Prevention: Lowering the temperature
3. Pinhole Porosity:
- Pinhole Porosity is spherical in shape
- During solidification absorbed gases are expelled leading to pinhole porosity
4. Sub-Surface Porosity:
Sub-Surface Porosity Cause:
- Simultaneous nucleation of solid grains and gas bubbles as the metal freezes at the mold walls
- This can be decreased by controlling the rate of molten metal entry
5. Residual Air In the Mold:
- Causes back pressure porosity
- Residual Air In the Mold occurs as a large concave depression due to the inability of air in the mold to escape
Residual Air In the Mold Causes:
- Dense investments
- Low mold temperature
Residual Air In the Mold Prevention:
- Adequate mold temperature
- Ideal casting pressure
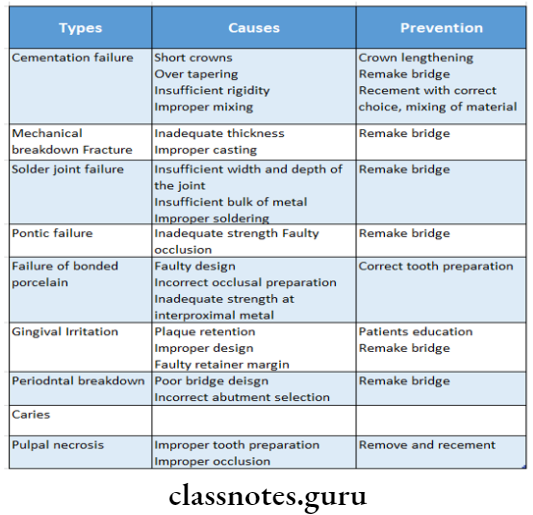
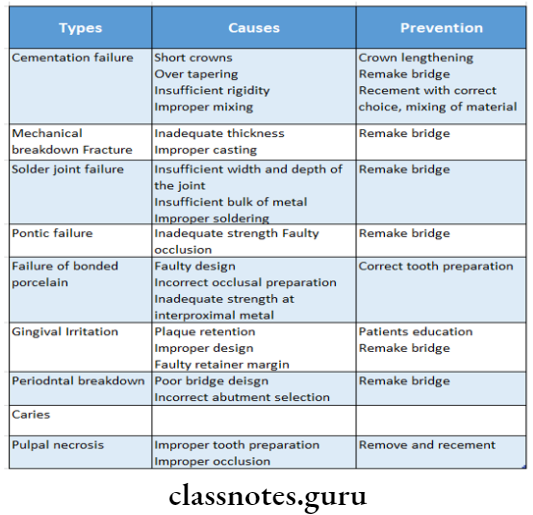
Question 31. Failures in fixed Partial Dentures
Answer:
Question 33. Abrasive and Polishing agents.
Answer:
- Diamond:
- Emery: Mixture of aluminum oxide and iron oxide bound to paper discs with glue or resins
- Aluminum Oxide
- Garment: For metal and porcelain
- Sandpaper discs: They are made from a dense crystalline form of quartz
- Tripoli: A fine siliceous polishing powder combined with a wax binder to form light brown cakes used with a cloth buff wheel or a soft bristle bursh
- Rouge:
- Composed of Iron Oxide
- Used for gold restorations applied with a soft bristle brush
- Electrochemical Finishing:
- One part nitric acid and three parts hydrochloric acid
- Electrochemical Milling:
- The casting is placed in cyanide solution which etches the casting by removing a layer of 40 microns from Type III alloy in one minute
Question 34. Nonprecious alloys used in fixed partial dentures
Answer:
1. Nickel-Chromium Alloys:
- Nickel-Chromium Alloys Composition:
- Nickel-70-80%
- Chromium-13-20%
- Beryllium – Small quantities
- Nickel-Chromium Alloys Advantages:
- Good strength
- Have superior physical properties
- Nickel-Chromium Alloys Disadvantages:
- High casting shrinkage
- Questionable biocompatible
- Requires modified casting techniques
2. Cobalt-Chromium Alloys:
- Cobalt-Chromium Alloys Composition:
- Cobalt-55-68%
- Chromium-25-27%
3. Cobalt-Chromium Nickel Alloys:
- Cobalt-Chromium Nickel Alloys Advantages:
- Cheaper
- Good strength
- Can be used along with metal ceramics
- Cobalt-Chromium Nickel Alloys Disadvantages:
- High fusion temperature
- Poor marginal fit
- Cannot be burnished
- Nickel-containing alloys can cause allergy
Question 35. Recent Advances in Fixed Partial Dentures.
Answer:
Recent Advances In Metal Ceramics:
- Pure titanium can be used as a coping and framework metal for metal-ceramic restoration.
- Copy milling is used to prepare duplicate dies of graphite and to machine the outer form of a titanium crown
- Titanium-based products are melted in a specialized casting machine and cast using the conventional lost wax technology
Recent Advances In Veneering Materials:
Reinforced Composites:
- Encore Bridge:
- The composite superstructure is bonded with porcelain veneers
- Encore Bridge is composed of 81% filled composite with a glass fiber reinforcement
- The framework has sufficient flexure to attain a class 1 mobility
- Encore Bridge Advantage:
- It requires minimal tooth preparation
- Castable Hydroxyapatite: Hydroxyapatite mixed with composite fibers is slip-cast by vibration
- Injectable Ceramics/Castable Ceramics:
- Dicor – It was used for FPDs, inlays, and on lays
- Indication – Laminates for periodontally compromised patients
- Contraindication – Short clinical crowns
- Injectable Ceramics/Castable Ceramics Advantages:
- Good strength
- Good marginal adaptation
- Bio-compatible
- Highly aesthetic
- Low thermal conductivity
- Injectable Ceramics/Castable Ceramics Disadvantage:
- Shrink-Free Ceramic System:
- Shrink-Free Ceramic System Indication: For periodontally compromised patients
- Shrink-Free Ceramic System Advantages:
- Good flexural strength
- Highly aesthetic
- Good marginal fit
Question 36. Splinting of abutment teeth
Answer:
A fixed partial denture usually requires the splinting of additional abutments to overcome the loss of bone support of an abutment
Purpose Of Abutment Teeth:
- Abutment Teeth distribute and direct the functional forces
- Abutment Teeth eliminate any mobility present Stabilize and reorient the forces
- Improves the function and form of teeth
- Modifies occlusal pattern
Classification Of Abutment Teeth:
- Based On The Extent Of The Prosthesis Across The Midline:
- Unilateral Splint:
- Unilateral Splint is the joining of two or more teeth in one plane of an arch segment
- They are very resistant to the mesiodistal forces
- Bilateral Or Cross-Arch Splints:
- Bilateral Or Cross-Arch Splints cross midline
- Resists forces that come from all directions
- Based On Duration Of Use:
- Temporary splints
- Used for a shorter span of time
- Permanent splints
- Help in the prevention of further progress of periodontal diseases
Question 37. Temporary crowns.
Answer:
- Polycarbonate Crown:
- These are performed crowns used for provisional restoration
- These are available in various sizes
- The operator can choose the size and material that would best suit the patient and place it as a provisional restoration
- Before cementing they are slightly altered and modified to fit the tooth
- Cast Metal Restorations:
- Cast Metal Restorations Indications:
- Patients with gross maxilla-mandibular discrepan- cies
- Medically compromised patients
- For maintenance of vertical dimension
- Aluminium Shell Crowns: Used for premolars and molars
- Nickel Chromium Metal Crowns:
- Used in children with extensively damaged primary teeth
- Used for long-term provisional restoration
- It is very hard
- Cellulose Acetate Crown: It is a thin, soft, and transparent material
- Heat-Polymerised Resin:
- A wax pattern with the desired shape is made on the mounted casts
- Wax patterns are flashed, dewaxed, and packed with heat-cure acrylic resin and cured
Question 38. Marginal integrity
Answer:
- Marginal adaptation and seating of restoration affect marginal integrity
- Poor marginal adaptation leads to percolation of oral fluids and secondary caries
- Margin of restoration should be preferably placed supragingival
Advantages Of The Supragingival Finish Line:
- Easy to maintain
- Fit can be evaluated
- Easy to make an impression
- Easily finish
- Compatible with surrounding tissue
Indications Of Subgingival Finish Line:
- The contact point is located below the gingival crest
- Short clinical crown
- To conceal the metal-ceramic margin
- Presence of secondary caries
Question 39. Anterior three-quarter crown.
Answer:
Advantages Of Anterior Three-Quarter Crown:
- Conservative tooth reduction Esthetics
- Electric pulp testing can be done
- Favorable periodontal response
- Ensures complete seating
Disadvantages of Anterior Three-Quarter Crown:
- Poor retention and resistance Critical preparation
- May cause discoloration of anterior teeth
Indications of Anterior Three-Quarter Crown:
- Intact or minimally restored teeth
- Teeth with adequate crown length
- Teeth with adequate labiolingual thickness
- Teeth having normal anatomic configuration
Contraindications of Anterior Three-Quarter Crown:
- High caries rate
- Short teeth
- Bell shaped teeth
- Thin teeth
Tooth Preparation Sequence:
- Occlusal reduction
- Lingual reduction
- Placing proximal grooves
- Placing occlusal grooves
- Placement of facial bevel
- Chamfer finish is preferred
Question 40. Partial crowns.
Answer:
- Three-Quarter Crown: Restores occlusal surface and three of the four axial surfaces not including the facial surface
- Reverse Three-Quarter Crowns:
- Restores all surfaces except lingual surface
- Indicated on mandibular molars with severe lingual inclination
- Seven-Eights Crown: Extension of the three-quarter crown to include a major portion of the facial surface
- One Half-Crown:
- It is a three-quarter crown rotated at 90 degrees preserving the distal surface
- Indicated on a tilted mandibular molar abutment
Question 41. Direct technique of provisionalization
Answer:
Bis-acryl composites exhibit less heat and shrinkage during polymerization and hence can be used to fabricate provisional restoration via direct technique
Technique of Direct :
- Overimpression is made using additional silicon Tooth preparation is carried out
- The prepared tooth is coated with petrolatum
- The base and catalyst of the composite are mixed and loaded into overexpression
- Before composite polymerises the over impression is reseated in the patient’s mouth
- The composite is allowed to be polymerized intraorally for 10 min
- The over impression is removed and the polymerized composite is teased out carefully
- Restoration is finally finished, polished, and cemented
Question 42. Mutually protected occlusion.
Answer:
- Proposed by Stalled and Stuart
- It states that the balancing contents during eccentric jaw movements were eliminated by making the canines on the working side disocclude the posterior teeth
- During lateral or protrusive excursions there is no posterior occlusal contacts
The rationale of Mutually protected:
- Anterior teeth have an advantage over posterior teeth when it comes to mechanical properties
- Forces generated by muscles of mastication are comparatively lesser when the tooth contact occurs more anteriorly
- The class 3 lever arm at the anterior teeth exerts lesser pressure
Features of Mutually protected:
- When condyles are in their most superior position uniform contact of all the teeth happens
- With functional jaw movement, the anterior tooth contact is harmonized
- At the lateral or protrusive movement, there is no contact of the posterior teeth
Question 43. Gingival finish lines.
Answer:
Requirements Of Gingival Finish Lines:
- Shallow bevels nearly parallel to the cavosurface should be avoided
- The bevel should not produce a very acute margin
- The tooth should not be reduced to more than half of the width of the diamond.
Question 44. Indications of fixed partial dentures
Answer:
Indications Of Fixed Partial Dentures:
1. Length Of The Edentulous Arch:
- Short-span edentulous arches are preferred for FPD
- This is due to the reason that a long-span FPD transfers excessive load to the abutment and also tends to flex to a greater extent
- To avoid it short span edentulous arches are preferred
2. Condition Of the Abutment Tooth:
- FPD is used if there is the presence of a posterior tooth for support
- Such a tooth should have
- Provides primary tion of gingival sulcus retention
- Axial contour can be difficult to maintain when modified
- Aid in resistance and finish
- Ideal crown root ratio for support
- Adequate thickness of enamel and dentin for reduction
- Adequate bone support
- Absence of periodontal disease
- Proper gingival contour
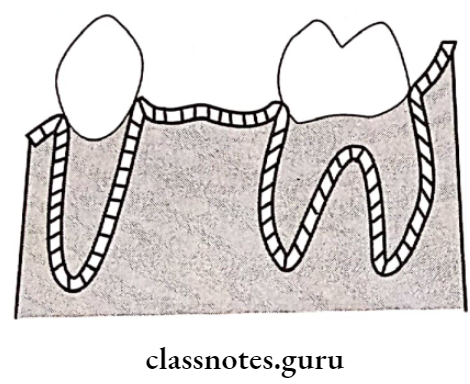
3. Condition Of The Residual Ridge:
- The contour of the ridge and texture of the soft tissues should be observed
- A smooth rounded ridge is best for the placement of FPD
4. Patient’s Preference:
- The patient may not desire to frequently remove and insert the denture
- If in these patients removable partial denture is given, they may not maintain it
- This may further lead to post-insertion problems
- To avoid this, FPD is preferred
Question 45. Virginia bridge.
Answer:
- Proposed by Moon and Hudgins
- Virginia bridge are resin-bonded fixed partial dentures that use particle roughed retainers
Method Of Fabrication:
- 150-250 μm salt crystals are sprinkled over the cast
- Retainer wax patterns are fabricated using resin
- The salt particles get incorporated onto the tissue surface of the resin pattern
- Salt particles get dissolved – Lost salt technique
- The resin pattern is invested and cast
- Dissolve crystals produce voids in the resin pattern
- These voids are reproduced in the cast metal retainer which helps in mechanical retention
Advantages of Virginia Bridge:
- Even noble metal alloys can be used
- Surface treatment of the retainer is not required
- Air abrasion with aluminium oxide is sufficient
Fixed Partial Denture Short Question And Answers
Question 1. Suck back porosity.
Answer:
- Back porosity is an external void seen inside of a crown opposite the sprue
- A hot spot is created by the hot metal impinging on the mold wall near the sprue
- The hot spot causes this region to freeze last
- Since the sprue has already solidified no more molten material is available and the resulting shrinkage causes a peculiar type of shrinkage called suck back porosity
Question 2. Maryland bridges.
Answer:
- Livaditis and Thompson from University of
- Maryland School of Dentistry used Dunn’s study and developed Maryland bridges
- In it mechanical retention was developed by the micro-porosities present on the tissue surface of the retainer
- Micro-porosities are created by etching the tissue surface of the retainer
Question 3. Solders.
Answer:
Requirements of Solders:
- Solders should fuse safely below the sag or creep temperature of the parent alloy
- Solders should resist tarnish and corrosion
- Solders should be non-pitting
- Solders should be free-flowing
- Solders should match the color of the parent metal
- The joint should be strong
Composition Of Solders:
Question 4. Types of occlusion in FPD.
Answer:
- Centric Occlusion: Centric Occlusion is the occlusion of opposing teeth when the mandible is at a centric relation
- Eccentric Occlusion: It is an occlusion other than centric occlusion
- Myocentric Occlusion:
- Proposed by Bernard Jankelson
- It produces relaxation of the mandibular muscles and then initiates controlled isotonic muscle contraction
- Pathologic Occlusion: It is defined as one in which sufficient disharmony exists between the teeth and the temporomandibular joint to result in symptoms that require intervention
Question 5. Casting defects.
Answer:
- Distortion
- Surface roughness Porosity
- Caused by solidification shrinkage
- Localized shrinkage porosity
- Suck back porosity
- Microporosity
- Caused by gas
- Pinhole porosity
- Gas inclusion
- Subsurface porosity
- Caused by air entrapment
- Back pressure porosity Incomplete casting
- Contamination of casting due to oxidation
Question 6. Disadvantages of partial veneer crown.
Answer:
- Less retentive than complete cast crown
- Limited adjustment of the path of withdrawal
- Some displays of metal
Question 7. Partial veneer crown.
Answer:
Indications of Partial Veneer Crown:
- Clinical crown of average length or longer
- The intact buccal surface that is not in need of contour or modification and that is well-supported
- No conflict between the axial relationship of the tooth and the proposed path of withdrawal of the FPD
Contra-Indications Of Partial Veneer Crown:
- Short teeth
- High caries index of tooth
- Extensive destruction
- Bulbous teeth
- Thin teeth
- Poor alignment
Question 8. Dicor.
Answer:
- Dicor is the first commercially available castable ceramic material for dental use
- Dicor was developed by Dentsply International
- Dicor is a castable glass that is formed into an inlay, facial veneer, or full crown restoration by a lost wax casting process
- Dicor is not used nowadays because of
- Very low tensile strength
- Tends to fracture easily
- More amount of tooth preparation is required
Question 9. Cerestore.
Answer:
- Cerestore is a shrink-free ceramic system
- Cerestore offsets conventional ceramic shrinkage by a combination of
- Chemical transformation- By oxidation of silicone
- Crystalline transformation- By formation of MgAl2O4
Question 10. Reversible hydrocolloid.
Answer:
Agar is a reversible hydrocolloid
Composition Of Reversible Hydrocolloid:
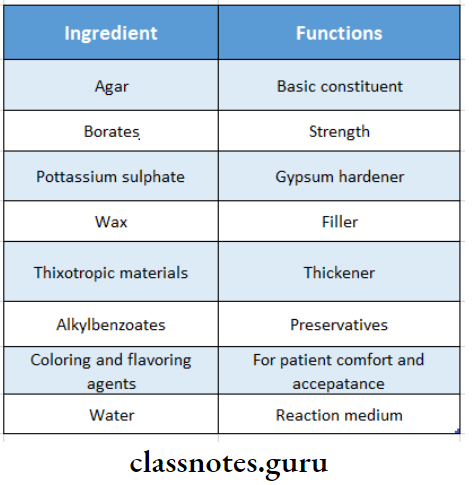
Question 11. Shade selection.
Answer:
- If natural teeth are present, the shade of the teeth adjacent to the edentulous space is taken as the index
- The artificial tooth should be moistened before matching it with a shade guide
- Natural light is better than artificial light for shade selection
- When operator stares at a tooth for a long time his/her eyes will undergo fatigue leading to the creation of shades
- Fatigue can be avoided by providing intermittent rest to the eyes
Question 12. Retraction cord.
Answer:
- Pressure packing the retraction cord into the gingival sulcus provides sufficient gingival retraction
- Retraction cord should be made of absorbent material like cotton
Technique Of Retraction Cord:
- Dry out the area
- Cut the desired length of cord from the dispenser bottle
- Twist the cord
- Dipped in 25% aluminium chloride solution Loop it around the tooth
- The cord is packed into the gingival sulcus Excess cord is cut off
- At least 2-3 mm of the cord is left protruding outside the sulcus
- After 10 minutes the cord is removed slowly to avoid bleeding
Question 13. Pain control in tooth preparation.
Answer:
Anesthesia is given to the tooth to be operated on and of adjacent soft tissues prior to tooth preparation
Pain Control Result:
- Pain elimination
- Reduces salivation
- Results in more pleasant procedure for patient and operator
Question 14. Axio-proximal grooves.
Answer:
- Axio-proximal grooves are indicated when the prepared tooth is short
- When properly positioned, grooves are in sound dentin close to DEJ
- The long axis of the bur must be held parallel to the line of draw
Question 15. Disadvantages of ridge lap pontic.
Answer:
- Ridge lap pontic is difficult to maintain
- Ridge lap pontic often leads to inflammation of the tissues in contact
Question 16. Disadvantages of subgingival finish lines.
Answer:
- Leads to inflammation of gingival sulcus
- Difficult to maintain and finish
Question 17. Importance of full mouth intra-oral radiographs.
Answer:
- Aids in:
- Evaluation of bone resorption, pattern of bone resorption, and quality of bone support
- To check for the presence of retained root tips, impacted tooth
- To determine the thickness of soft tissue on the ridge in an area of pontic placement
Question 18. Indications of fixed partial denture.
Answer:
- Short span edentulous arches
- Presence of a posterior tooth for support
- Presence of smooth rounded ridge Patient’s preference
- Mentally compromised and physically handicapped patients
Question 19. Articulating Paper.
Answer:
- Articulating paper is available in blue and red stripes
- Articulating paper is used to check the occlusion
Articulating Paper Method Of Use:
- Articulating paper is placed over the occlusal surface of mandibular teeth
- The patient is asked to bite over it
- The paper is gently pulled out
- The markings over the high points are observed and reduced accordingly
Question 20. Pier Abutment.
Answer:
A Pier Abutment is a natural tooth located between terminal abutments that serve to support a fixed or removable prosthesis
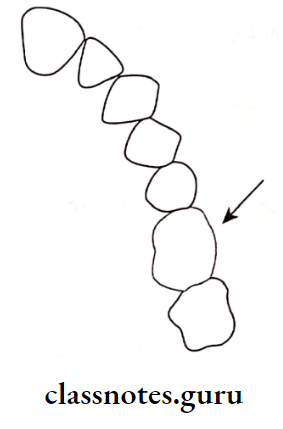
Disadvantages Of Placing A Rigid Connector In Pier Abutment:
- Intrusion of abutment teeth
- Tooth moves in a buccolingual direction
- Weakening of terminal retainers
- Microleakage and caries
- Trauma to the periodontum
Pier Abutment Prevention: To avoid adverse effects, stress breaker should be provided
Question 21. Relationship between pontic and soft tissue.
Answer:
- The contour of the soft tissue is surveyed on the diagnostic cast during treatment plan
- A smooth rounded ridge is best for pontic placement
- Siebert grouped residual ridges into 3 categories
- Class 1: It is a ridge with loss of faciolingual width with normal apicocoronal height
- It is corrected by ridge augmentation
- Class 2: It is the ridge with loss of ridge height with normal ridge width
- It is corrected by grafting
- Class 3: It is the ridge with loss of both height and width
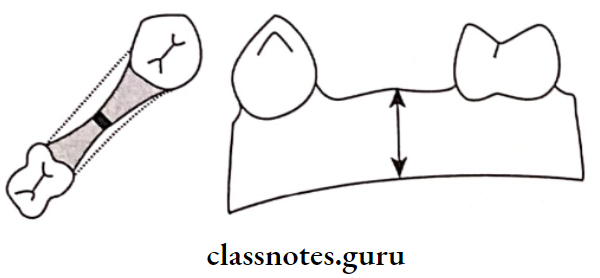
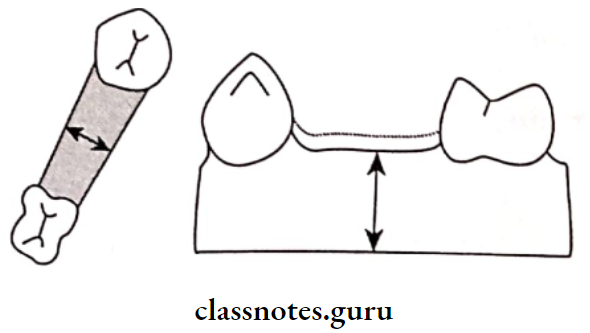
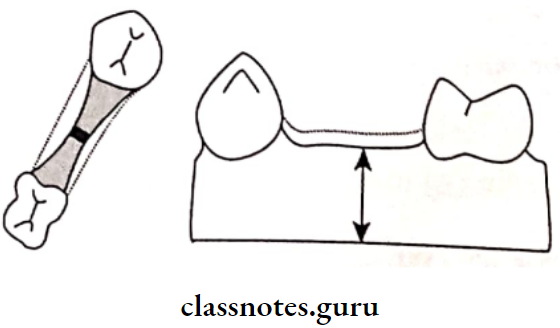
Question 22. Depth orientation Grooves.
Answer:
- Depth orientation grooves are made during tooth preparation Three depth orientation grooves, 1.0 mm deep are placed.
- One in the middle of the facial wall and one each in the mesio-facial and distofacial line angles in the incisal edge.
- Two more depth orientation grooves of 2.0 mm depth are placed on the incisal half/occlusal half – 2 mm deep grooves are placed on the incisal edge for incisal reduction.
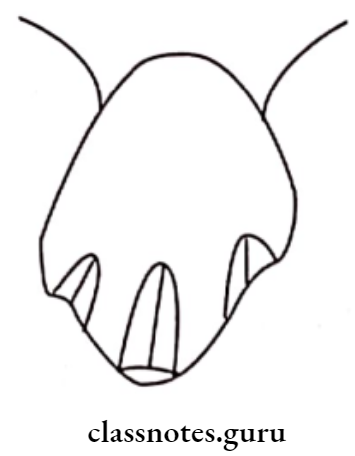
Question 23. Mesial Half crown/Proximal Half crown.
Answer:
A mesial half crown restores the occlusal and mesial surfaces as well as portions of the facial and lingual surfaces.
Indications of Mesial Half Crown:
- In mesially tilted molars
- Patients with good oral hygienc status and low incidence of caries
Contraindications of Mesial Half Crown:
- Distal caries present
- In caries prone mouth
- In poor oral hygiene maintenance
- If there is a severe marginal ridge height difference between the distal of the second molar and the mesial of the third molar.
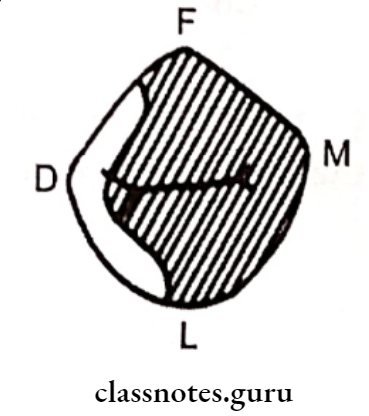
Question 24. All ceramic systems/Metal-free ceramics.
Answer:
Ceramic system are man-made solid objects formed by baking raw materials at high temperatures
Classification Of Ceramic Systems:
- Conventional powder-slurry ceramics
- Castable ceramics
- Machinable ceramics
- Pressable ceramics
- Infiltrated ceramics
Question 25. Dowel Pin.
Answer:
- Used when an endodonticaaly treated tooth is used as an abutment
- Dowel pin is the screw component that is inserted into the root canal
Types of Dowel Pin:
Dowel Pin Factors To Be Considered:
- The canal should be obturated only with gutta-percha
- For proper retention, the length of the dowel inside the root should be at least 2/3rd of the root length
- The coronal portion of the dowel should be encircled at least by 1-2 mm of tooth structure to obtain a ferrule effect
Question 26. Disadvantages of Porcelain veneer.
Answer:
- Reduced strength
- Technique sensitive
- Least conservative
- Brittle in nature
- Can be used as single restoration only
Question 27. Advantages of Porcelain fused to metal crowns/Metal ceramic crowns.
Answer:
- Good strength
- Good marginal fit
- Good aesthetic
- Can be used as a fixed partial denture retainer

Its Tooth Preparation Provides:
- Structural durability
- Preservation of periodontal health
- Provide retention
- Resistance
- Preservation of tooth structure
Question 28. Indications for Jacket Crown.
Answer:
- High esthetic requirement
- Considerable proximal caries
- The incisal edge reasonably intact
- Endodontically treated teeth
- Favorable occlusal distribution
Question 29. Advantages of Partial veneer.
Answer:
Advantages Of Partial Veneer:
- Conservation of tooth structure
- Improved access for finishing by the dentist and cleaning by the patient
- Improved periodontal health as there is limited contact between the margins of the restoration and gingiva
- Partial veneer can be completely seated during cementation
- The marginal fit can be easily verified
Question 30. Types Finish lines.
Answer:
Types Of Fish Lines:
- Supragingival
- Subgingival
- Chamfer
- Shoulder
- Shoulder with bevel
- Feather edge
- Knife edge
Question 31. The angle of Cervical Convergence.
Answer:
The Angle Of Cervical Convergence:
- The degree of taper is inversely proportional to the retention form
- Zero-degree taper is the most retentive
- The sum of the degree of taper is called as angle of cervical convergence
- 4-100 optimum retention
- Mandibular premolars No reduction as they are lingually tilted 60 needed for tooth preparation
- Bur used – tapering fissure diamond with 30
Question 32. Laminate Veneers.
Answer:
Laminate Veneers Synonym: Facial veneer
Features of Laminate Veneers:
- Laminate Veneers are prostheses that are used of ceramic
- Laminate Veneers are used as a thin layer over the facial surface of the tooth
- Its inner surface is etched with hydrofluoric acid and bonded to the tooth with composite resin cement
Advantages of Laminate Veneers:
- Good translucency
- Reduced plaque adherence
- Reduced chair time
- Wear resistant
- Bio-compatible
- Good bond strength
Disadvantages of Laminate Veneers:
- Fragile
- Loss of glaze while finishing
- Expensive
- Technique sensitive
Question 33. Polycarbonate Crown.
Answer:
- Polycarbonate crown are performed crowns used for provisional restoration
- Polycarbonate crown are available in various sizes
- The operator can choose the size and material that would best suit the patient and place it as a provisional restoration
- Before cementing they are slightly altered and modified to fit the tooth
Advantage of Polycarbonate Crown:
- Less time consuming
- Its shade can be altered by the shade of the luting agent
- Esthetic
Disadvantage of Polycarbonate Crown:
- Limited to single-tooth preparation
Indication of Polycarbonate Crown:
- For anterior teeth restoration
Question 34. Relationship of finish line and restoration.
Answer:
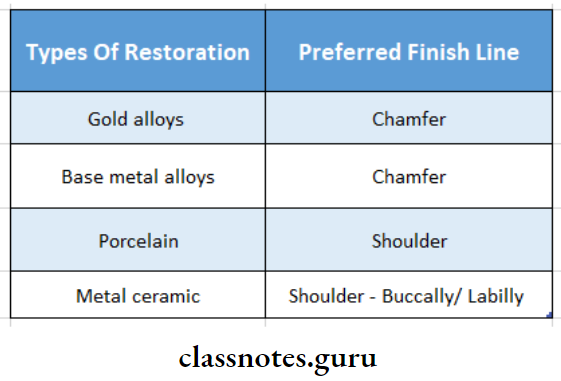
Question 35. Rochette Bridges-Design by Rochette in 1973.
Answer:
- Rochette bridge is a wing-like retainer with six perforations to provide mechanical undercut for resin cement
- Etched retainers are coated with pyrolyzed silane and bonded with resin cement
- Rochette bridge is funnel-shaped with a base towards the tooth surface
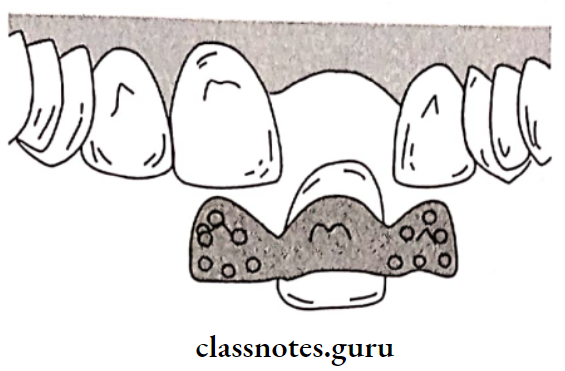
Disadvantage of Rochette Bridges:
- The resin is exposed through the perforation to oral fluids and external stress, which leads to abrasive and marginal leakage
Variation of Rochette Bridges:
Question 36. Spring Cantilever Bridge.
Answer:
Spring cantilever bridge is special cantilever bridge designed for the replacement of maxillary incisors
Design Considerations:
- A long resilient bar connector is used to connect the posterior retainer to the anterior pontic
- The bar adapts closely and extends over the soft tissues of the palate
- The bar should be thin and resilient enough to resist permanent deformation under masticatory load
Advantages of Spring Cantilever Bridge:
- Can be used for diastema cases
- Requires minimal tooth preparation
Disadvantages of Spring Cantilever Bridge:
- The bar may interfere with speech and mastication
- Spring cantilever bridge deformation may produce coronal displacement of the pontic
- This may lead to tissue hyperplasia due to food entrapment
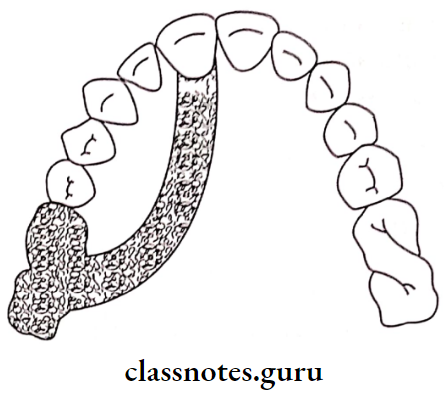
Question 37. Fixed partial denture.
Answer:
- Fixed partial denture consists of fixed partial dentures with rigid connectors
- Thus, there can be no movement between the connected components
Advantages of Fixed Partial Dentures:
- Easy to fabricate
- Easy to maintain
- Economical
- Strong
- Helps to splint mobile abutments
- Can be used along with periodontally weak abutments
Disadvantages of Fixed Partial Dentures:
- Unwanted forces are directed to the abutment Requires excessive tooth preparation
- Difficult to cement
- Cannot be used for pier abutments
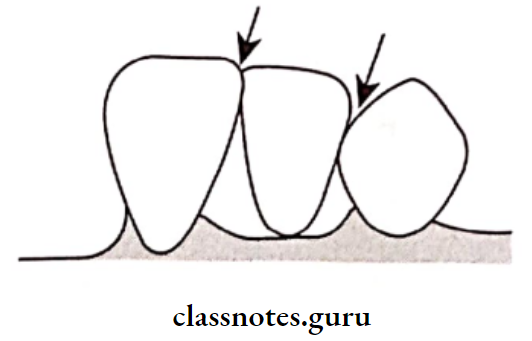
Question 38. Impression materials.
Answer:
Impression Materials Ideal Requirements:
- Impression Materials should be dimensionally stable
- Impression Materials should be accurate
- Impression Materials should be sufficiently elastic
- Impression Materials should be able to get the oral tissues
- Impression Materials should be compatible with the model and materials
- Impression Materials should be possible to electroplate them
Question 39. Removable Dies.
Answer:
In this system, a special type of working cast is prepared and the dies are carefully sectioned so that the individual dies can be removed and replaced in their original position in the cast
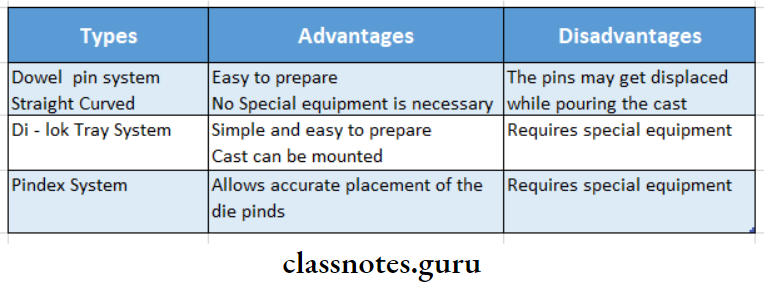
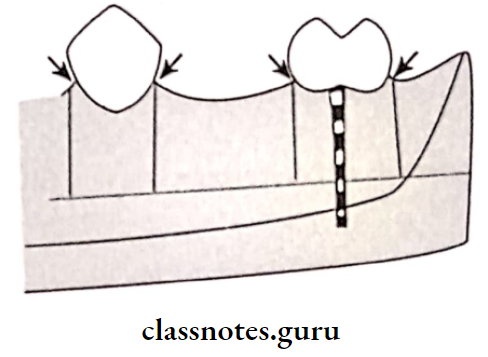
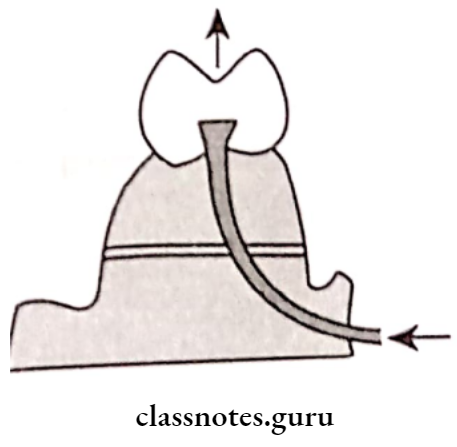
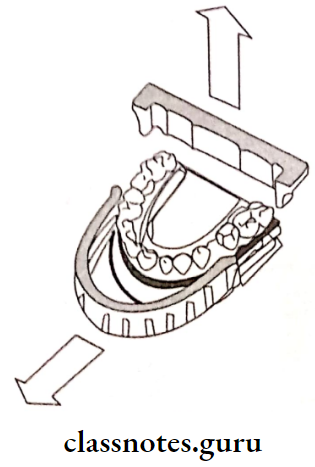
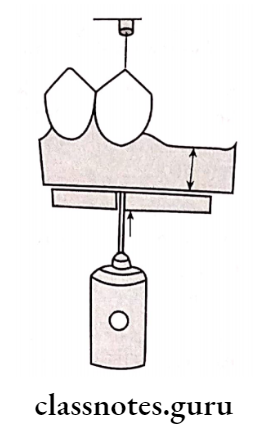
Question 40. Soldering Flux.
Answer:
Soldering Flux is a substance applied to surfaces to be soldered by joining, to increase fluidity and reduce oxidation of a molten metal
Significance of Soldering Flux:
- Removes oxides and prevents oxidation
- Allows solder to wet the metal surface
- Helps solder to adhere to metal surface
Composition of Soldering Flux:
- Borax glass 55 parts
- Boric acid-35 parts
- Silica – 10 parts
Question 41. Pressure Indicating Paste (PIP).
Answer:
Any substance applied to a prosthesis that when seated on a structure, demonstrates the adaptation of the prosthesis to the structure it opposes
Composition of Indicating Paste:
Equal parts of vegetable additives with Zinc Oxide or a mixture of Calcium Carbonate and Chloroform
Indicating Paste Method Of Use:
- The two paste are mix to a homogenous mix
- It is applied over the occlusal and denture-bearing area
- Pressure is applied by the patient/dentist
Indicating Paste Pressure Areas:
- In Maxilla:
- Palate
- Lateral sides of tuberosity
- In Mandible:
- Mylohyoid ridge
- Area buccal to the bicuspid
- Distolingual border of denture
- Retromylohyoid space
Question 42. Die spacer.
Answer:
To produce space for luting cement, a die spacer is used over a die
Materials Used for Die Spacer:
- Commonly resins
- Colored nail polish
- Thermoplastic polymers dissolved in volatile solvents
Technique of Die Spacer:
- Such spacers are applied in several coats to within 0.5 mm of the preparation finish line
Purpose of Die Spacer:
- Provide relief space for luting cement
- Ensures proper seating of the otherwise precisely fit- ting casting or coping
Question 43. Night Guards.
Answer:
Night guards acts as an occlusal protective device
Uses Of Night Guard:
- In bruxer
- In acute TMJ disorders cases
- To prevent abnormal mandibular closure
- In sports like boxing
Materials Used By Night Guard:
- Acrylic
- Latex rubber
- KVA Copolymer
- Polyurethane
- PVC
Advantages Of Night Guard:
- Night guard supports the edentulous spaces
- Reduces chances of jaw fracture and dislocation
- Protects occurrence of tooth fracture and dislocation
Question 44. The function of functional cusp bevel in fixed partial denture.
Answer:
- Functional cusp bevel is prepared on palatal cusps of maxillary molars and buccal cusps of mandibular posteriors
- The angulation of the functional cusp bevel should be at 45 degrees angle to the long axis of the tooth for partial veneer crown
- For a complete veneer crown, the angulation should be parallel to the inner inclines of the cusps of opposing tooth
- Provides adequate bulk in the areas of heavy occlusal contacts
- Lack of functional cusp bevel can cause a thin areas of perforation in the casting
- Fixed Partial Denture provides structural durability of restoration
Question 45. Classify fixed partial dentures.
Answer:
- Class – Identifies location of edentulous space
- Class 1- Posterior edentulous space
- Class 2 – Anterior edentulous space
- Class 3-anteroposterior edentulous space
- Division indicates teeth present adjacent to the edentulous space that is capable of taking support
- Division 1 – Cantilever FPD abutment present on one side of edentulous space
- Division 2 – Conventional FPD abutment present on both sides of edentulous space
- Division 3 – Pier abutment single tooth sur rounded by edentulous space on either side
- Subdivision – denotes the status of the tooth
- Sub-division 1- Ideal abutment
- Sub-division 2 -Tilted abutment
- Sub-division 3 – Periodontally weak abutment
- Sub-division 4 -Extensively damaged abutment
- Sub-division 5 -Implant abutment
Question 46. Di-lock system
Answer:
- Di-Lock System is a special tray used to pour the cast
- Di-Lock System has orientation grooves on the inner aspect
- In the di-lock system, the impression is poured using the pour technique
- The first pour is poured up to the level of the impression
- Next, the rim of the di-lock tray is positioned over the impression
- The second pour is poured over it
- The cast is allowed to set
- Di-lock tray is then dismantled
- Grooves formed on the base of the cast by the di-lock
- The tray is used as a guide for die-sectioning
Advantages of the Di-lock system:
- Simple and easy to prepare
Disadvantage of the Di-lock system:
- Requires special equipment
Question 47. Pickling
Answer:
- Pickling is the process of cleaning the casting with 50% warm HCI
- Used to remove surface oxides from casting
- Pickling is not a routine procedure
- Used only when indicated
Question 48. Flux and anti-flux
Answer:
Flux: Flux means flow
- Uses of Flux:
- Removal of oxide coating of solder
- Dissolves impurities
- Prevents oxidation
- Reduces melting point
- Composition of Flux:
- Borax glass- 55%
- Boric acid-35%
- Silica – 10%
Antiflux: It confines the flow of molten solder
Antiflux Example:
- Lead pencil markings
- Graphite lines
- Iron rouge
Question 49. Non-rigid connectors in fixed partial dentures
Answer:
- Used in case of non-parallel abutments. They are
- Tenon mortise connector
- Loop connector
- Split connector
- Cross pin and wing connector
Question 50. Indications and contraindications of porcelain jacket crown.
Answer:
Indications:
- Fractured incisal angles
- Hypoplastic, discolored, and malformed teeth
- Facial/ proximal caries that cannot be restored by composites
Contra-Indications:
- Young patients
- Short clinical crowns
- Sports persons
- Excessive overbite
- Least overjet
- High DMF rate
Question 51. Differences between direct and indirect spring.
Answer:
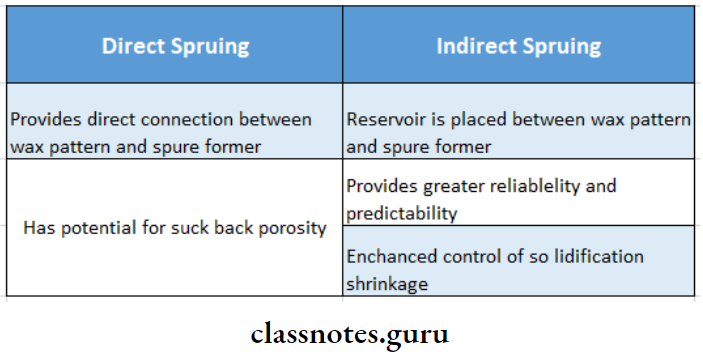
Question 52. Classification of posts
Answer:
Types Of Posts:
- Prefabricated
- Available with either amalgam or resin core
- Materials used are
- Stainless steel
- Titanium
- Nickel and chromium
- Molybdenum
- They can be parallel-sided or tapering
- Further classified into
- Passive/cemented type
- Active/threaded type
- Custom Made:
- Custom Made are cast from wax patterns fabricated in the canal
- A brass wire or a paper clip may be used to make the wax pattern within the canal
- Further classified into
- Prefabricated noble metal
- Resin pattern fabrication
- Wax pattern fabrication
- Fabrication Steps:
- Tooth preparation
- Canal preparation
- Canal pattern fabrication
- Casting
- Finishing and cementation
Question 53. Advantages of a fiber post.
Answer:
Advantages Of A Fiber Post:
- Biocompatibility
- More rapid treatment
- Esthetics
- Corrosion resistance
- Safe
- Easily removed
- Conserves tooth structure
- Tend to absorb and dissipate stress like natural dentin
- Prevents root fracture
Question 54. Tube impression
Answer:
Indications of Tube impression:
Advantages of Tube impression:
- Saves time
- An accurate finish line can be obtained
Disadvantages of Tube impression:
- Requires additional impressions
- Proper orientation of the die with the dies of adjacent/ opposing teeth is difficult
Method of Tube Impression:
- Copper tube is selected and customized according to the patient
- Fingers are coated with petroleum jelly
- Green stick compound is softened and filled up to one third of the tube
- This tube is then placed onto tooth preparation
- Light body material is then syringed over the prepared tooth
Question 55. Bull’s law.
Answer:
- For correction of occlusal errors selective grinding is done
- All contact areas are made visible by the markings of articulating paper
- On the non-working side, contacts occurs between maxillary buccal and mandibular lingual cusps
- Selective grinding on the working side is done following Bull law which is grinding of Buccal cusps of Up- per molar and Lingual cusps of Lower molar
- Selective grinding is verified and repeated is required
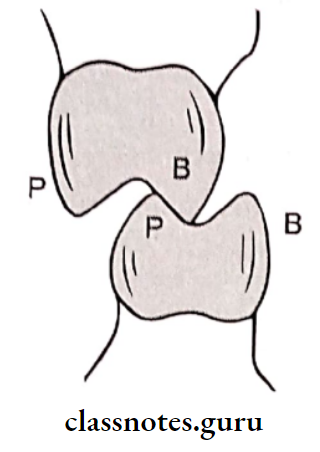
- B-buccal
- P-palatal
Fixed Partial Denture Viva Voce
- After removing from mouth, alginate impression should be poured within 15 minutes
- Average root surface area of maxillary permanent 1st molar is 433 mm3
- A molar with divergent roots provides better support in FPD
- Long span fixed partial denture should be fabricated by material having high strength and rigidity
- Shoulder gingival margin is less conservative
- Chisel edge gingival margin is indicated in tilted teeth
- Shoulder gingival margin is indicated on facial margins of metal-ceramic crowns
- Chamfer gingival margin is indicated for lingual margin of metal ceramic crown
- The functional cusp bevel is placed at 45 degrees to long axis of the tooth
- Incisal reduction for metal-ceramic crown 1.5-2mm
- Incisal reduction for porcelain crown – 1.5 mm
- Optimal cavosurface angle in all ceramic crown is 90 degrees
- The facial surface is more reduced in metal ceramic crown as compared to complete ceramic crown
- Hydrofluoric acid is etchant used in bonding of porcelain to tooth
- Polysulfide and hydrocolloid are not compatible with resin dies
- Bullet shaped pontic has only one point contact
- Modified ridge lap pontic is recommended in maxillary anterior region
- The sanitary pontic is the most hygienic
- All metal pontic is needed in situations of high stress
- Sprue is attached to the thickest part of the wax pattern
- Recommended soldering gap is 0.25 mm
- Loop connector is used to maintain a diastema in a planned fixed prosthesis
- Graphite is used as antireflux
- Rouge contains iron oxide
- Reducing zone of flame is used in torch soldering
- Modified zinc oxide eugenol cement is used as luting agent for provisional restoration
- RPI stands for – Rest, Plate, I bar clasp
- Cyanoacrylate is used as die hardener
- Modified ridge lap pontic is sued to replace missing canine